Chapter 36 Virus-Associated Lymphoma
Table 36-1 Epstein-Barr Virus-Associated Lymphoma
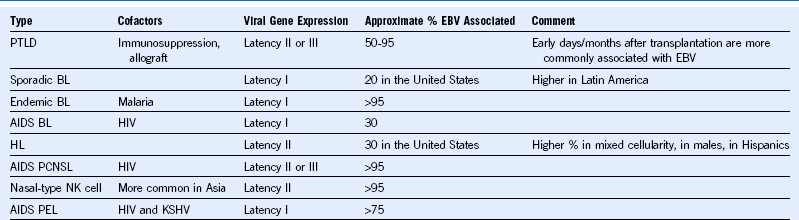
AIDS, Acquired immunodeficiency syndrome; BL, Burkitt lymphoma; EBV, Epstein-Barr virus; HIV, human immunodeficiency virus; HL, Hodgkin lymphoma; KSHV, Kaposi sarcoma—associated herpesvirus; NK, natural killer; PCNSL, primary central nervous system lymphoma; PEL, primary effusion lymphoma; PTLD, posttransplantation lymphoproliferative disorder.
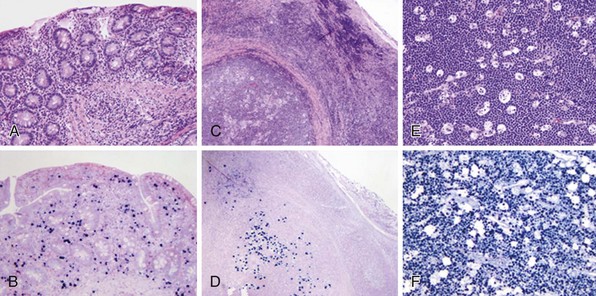
Epstein-Barr Virus-Associated Positive Posttransplant Lymphoproliferative Disorder
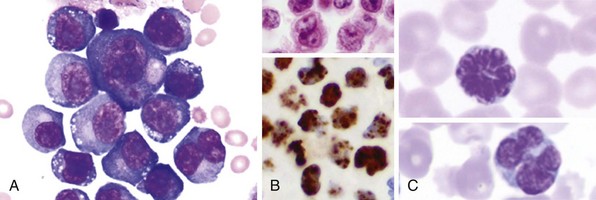
Figure 36-2 EXAMPLES OF KSHV- AND HTLV-1-ASSOCIATED LYMPHOPROLIFERATIVE DISEASE.
(A and B courtesy Dr. Elizabeth Hyjek, University of Chicago.)
Table 36-2 HIV-Associated Lymphoma
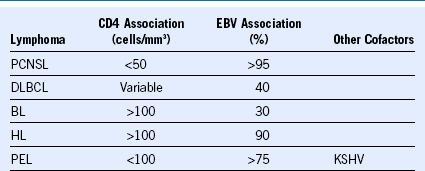
BL, Burkitt lymphoma; DLBCL, diffuse large B-cell lymphoma; EBV, Epstein-Barr virus; HIV, human immunodeficiency virus; HL, Hodgkin lymphoma; KSHV, Kaposi sarcoma—associated herpesvirus; PCNSL, primary central nervous system lymphoma; PEL, primary effusion lymphoma.