36 Vertebral Body Stenting
KEY POINTS
Introduction
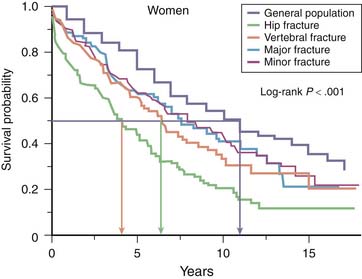
Vertebral body compression fractures (VBCFs) are the hallmark of osteoporosis, and their incidence increases exponentially with increasing age. VBCFs are related to important morbidity and loss of quality of life comparable to that in hip fractures (Figure 36-1).1,2
The treatment of painful VBCFs with percutaneous cement reinforcement has a long history and appears very effective in a very high percentage of patients treated. There are many case series published that support this treatment, with the most recent publication also providing encouraging long-term results.3–5 Furthermore, there is class A evidence based on a large multicenter Randomized Clinical Trial (RCT) comparing percutaneous cement reinforcement after cavity creation with a balloon against conservative treatment. This study clearly shows a superiority of cement reinforcement for pain, activity level, and pain medication in the first year of treatment.6 Although the study is comparing kyphoplasty as a specific technique of reinforcement against conservative treatment, based on several review articles, there is no clinical advantage of kyphoplasty over vertebroplasty.7,8 Most recently, two studies were published comparing vertebroplasty with a sham procedure showing no difference in early outcome. Although the studies show a randomized design with independent assessment, there seems to be a selection bias because the inclusion of patients took several years even though a multicenter study design was used.9,10
Although cement reinforcement can stabilize a fracture and therefore decrease pain, height restoration remains an issue, that is not solved yet. Kyphoplasty was introduced initially with the idea to restore vertebral body height. However, the amount of height gain remained very modest, and its clinical impact remains obscure. With the inflation of the balloon, excellent height reduction can be achieved, but after deflation a major amount of the reduction gets lost.11
The consequences of vertebral height loss and increased kyphosis are reported in several epidemiological studies: impaired quality of life and even an increased mortality are documented (see Figure 36-1).2,12,13
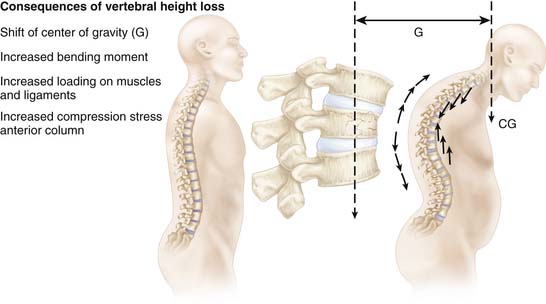
The kyphotic deformity leads to a shift of center of gravity and consecutively to an increased load on the anterior column. Consequently, there is an increased risk for new fractures.14,15 Furthermore the increased kyphosis raises the load of the back muscles enormously (Figure 36-2).16,17
Vertebral Body Stent
In Vitro Testing
Extensive cadaver testing allowed proof of the feasibility of the concept, and in a sophisticated in vitro setup, one could clearly demonstrate the superior potential for height maintenance in comparison to the balloon insertion only with sound significance (Figure 36-3).18
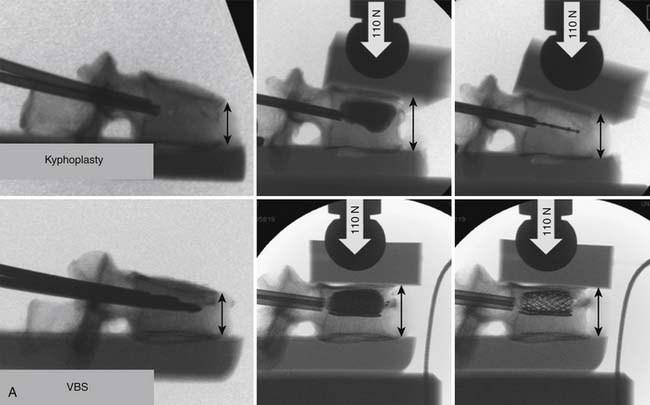
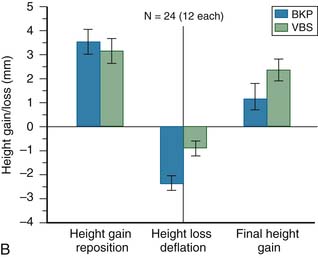
FIGURE 36-3 A, Comparison of a kyphoplasty procedure and a vertebral body stenting system as assessed in a cadaver model with a preload of 110 N.21,22 Initial reduction can be achieved equally well with both systems. After deflation of the balloon there is a significant loss of reduction with the kyphoplasty system (∗), whereas the height can be maintained with the VBS (∗∗). B, Summary of twelve pairs of vertebrae tested. Initial height gain is similar in both techniques. Loss of height is observed with both systems, but significantly less with VBS (p = .024), and consequently the overall height restoration is superior with the VBS system (p = .035). (From Wilke HJ, Neef P, Caimi M, Hoogland T, Claes LE. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine 1999;24-8:755-762; and Sato K, Kikuchi S, Yonezawa T. In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine 1999;24-23:2468-2474.)
Clinical Application
Indications
The use of the vertebral body stent (VBS) is indicated in acute and subacute painful VBCFs with at least 15% of height loss and kyphotic deformity with the potential of reducibility. In consolidated and fixed fractures, the use of a stent is no longer indicated.
Surgical Technique
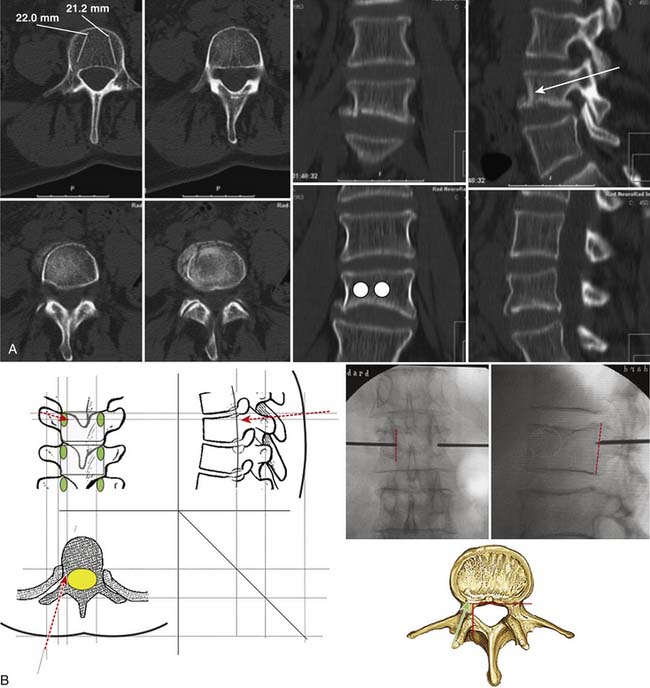
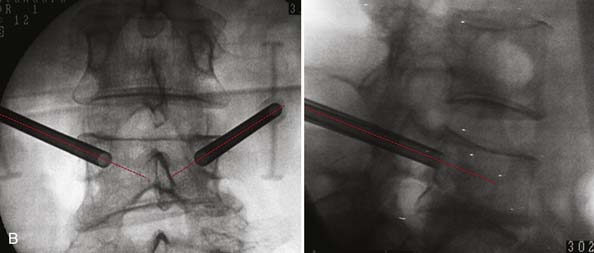
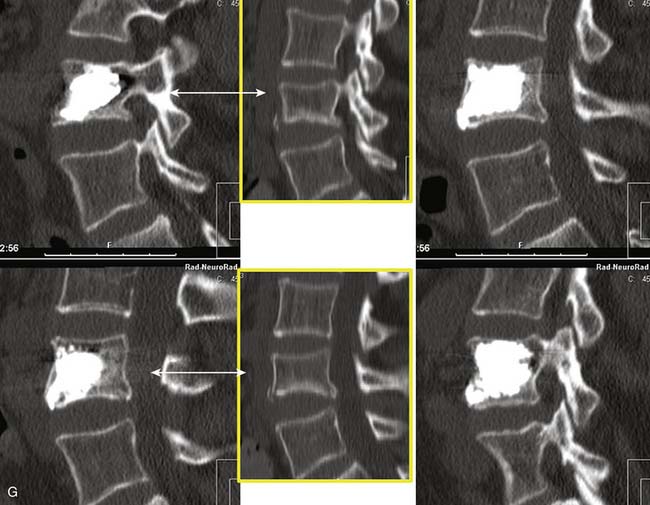
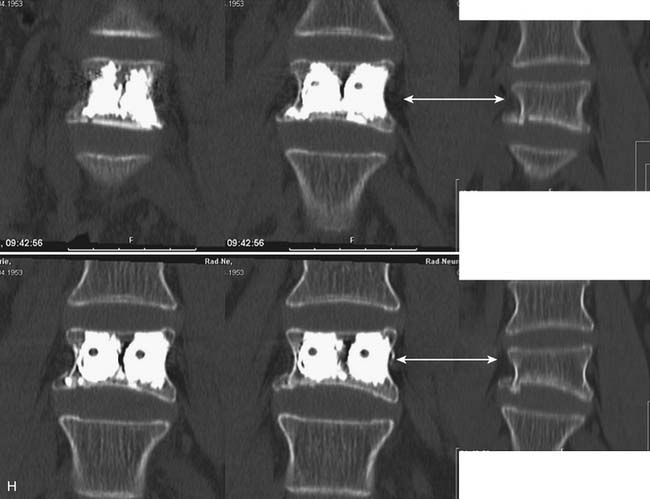
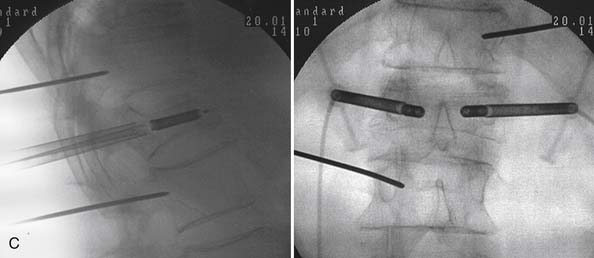
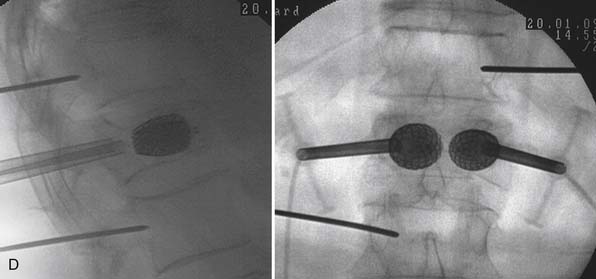
Preferably the procedure is performed under general anesthesia, with the patient placed in hyperextension. Based on the preoperative imaging (either CT scan or MRI and conventional x-rays), the placement of the working cannula and the stent is planned in order to achieve an optimal effect for the fracture reduction (Figure 36-4, A). Intraoperatively this placement is navigated by biplanar C-arm control. The crucial landmarks to be respected are the medial border of the pedicle and the posterior wall of the vertebral body. Depending on the individual anatomical situation, the working cannula is placed transpedicular or parapedicular (Figure 36-4, B).
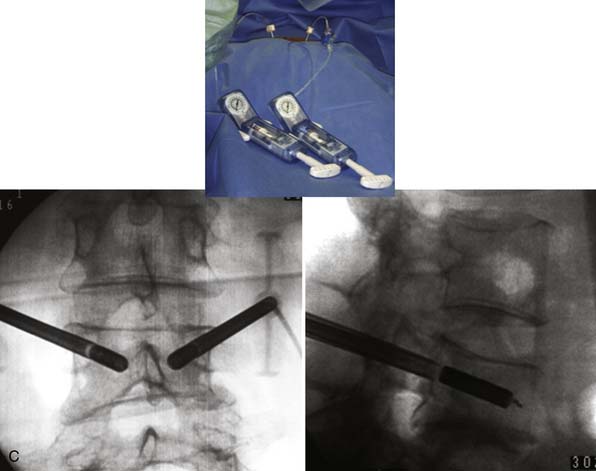
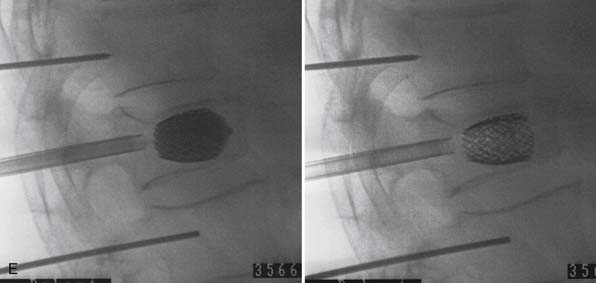
Once the working cannula is positioned, the space for the stent is prepared and its size determined and confirmed with the reamer. Then the stents are placed and the appropriate position is monitored in both planes. Make sure that the stents are outside the working cannula but fully inside the vertebral body and that they do not interfere at the tip. Do not start expansion before this check. Then a stepwise symmetrical filling of the balloon stent is performed under pressure, volume, and visual control by imaging. Once the maximal filling or height restoration is achieved, the balloons are deflated and removed. The filling is performed with high viscosity polymethylmethacrylate (PMMA). The cement should fill the void of the stent and infiltrate the surrounding bone. If there is any leakage, cement injections must be stopped immediately, wait for at least 45 seconds and then cautiously continue with the injection (Figure 36-5). Once the cement is cured remove the filling cannulas.
Results
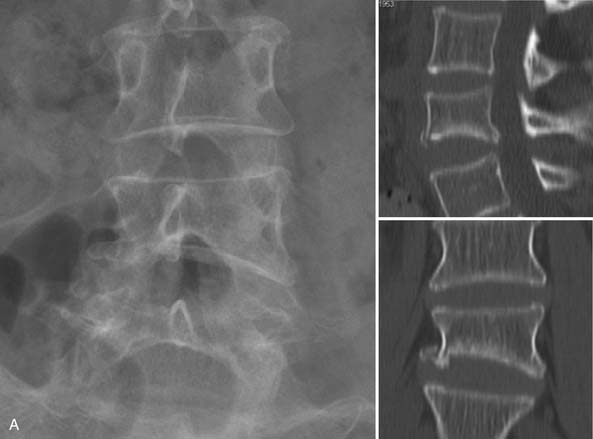
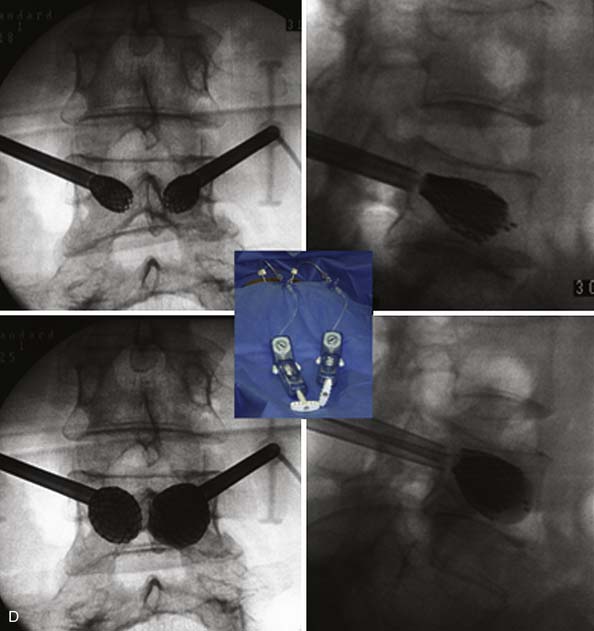
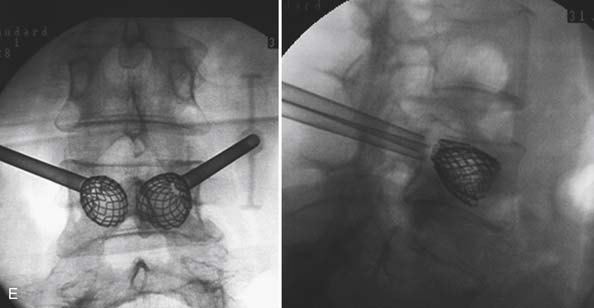
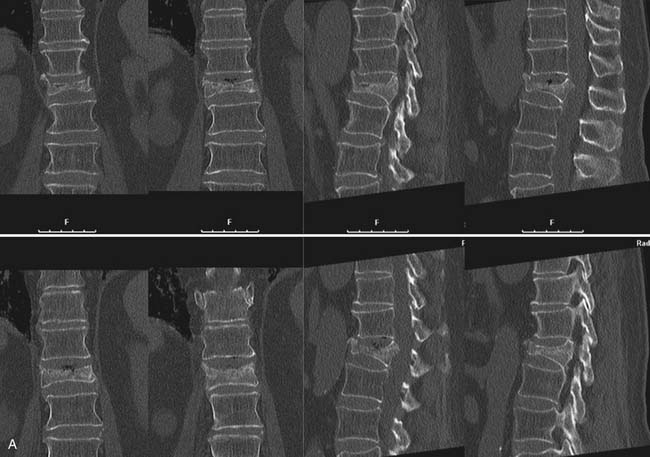
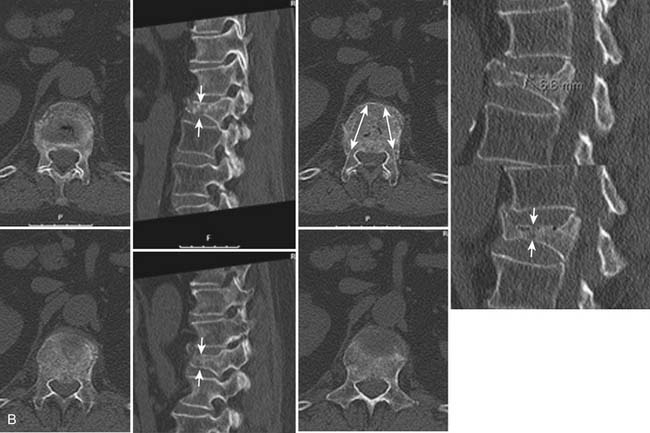
The amount of reduction that was achieved in the cases with still mobile fractures (n = 40) was measured by the segmental kyphosis (Figure 36-6, C). The average kyphosis angle preoperatively was 23 degrees (13 to 32 degrees) and could be corrected to 12 degrees (0 to 16 degrees) postoperatively. Height restoration was assessed semiquantitatively in the cases where the deformity was not mainly the kyphosis. The amount was graded from 0 to 3, where 0 meant no reduction possible and 3 meant complete restoration. There were 9 cases with grade 0. We have seen 18 cases with a reduction of grade 1, which means 50% height gain (see Figure 36-5); 15 cases with grade 2, which is 75% of height gain (Figure 36-7); and 7 cases with complete height restoration (Figure 36-8).
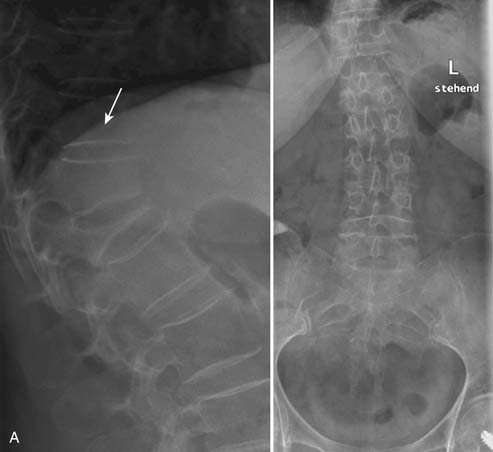
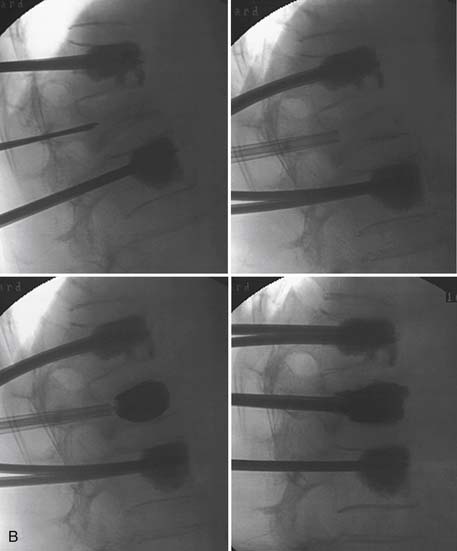
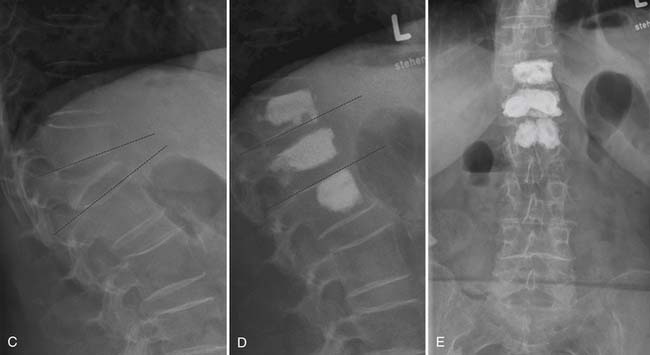
FIGURE 36-6 A, A 72-year-old woman with pain history of 8 weeks. The first x-rays show a complete collapse of L1 with severe kyphosis. B, Combining the closed reduction techniques of lordoplasty23 and VBS allows a nearly complete height restoration. (From Orler R, Frauchiger LH, Lange U, Heini PF. Lordoplasty: report on early results with a new technique for the treatment of vertebral compression fractures to restore the lordosis. Eur Spine J, 15(2) 1769-1775, 2006.) C, Comparison of preoperative standing film and follow-up x-ray after 6 months. The vertebral height is well restored and maintained and the kyphosis nearly completely corrected (D and E).


FIGURE 36-8 A, Male patient, 41 years old, presents after a skiing accident with a burst split fracture of L1 (AO 3.2). B, The stent restored L1 to its former height. Ligamentotaxis provides realignment of the fragments, the cement then provides stability that allows immediate weight bearing. Reservations against using PMMA in young people are justified; however, alternative material is lacking and histologic workup of a postmortem specimen depicts no adverse effects around the cement, as demonstrated in the MRI taken 1 month after the intervention.24 (From Braunstein V, Sprecher CM, Gisep A, Benneker L, Yen K, Schneider E, Heini P, Milz S. Long-term reaction to bone cement in osteoporotic bone: new bone formation in vertebral bodies after vertebroplasty. J Anat 2008;212-5:697-701.)
Discussion
The clinical impact of height restoration needs to be demonstrated. Based on clinical comparison the impact of the fracture kyphosis seems to be more important than the overall kyphosis regarding balance problems of the spine.19 Biomechanical calculations suggest that the increase of kyphosis is related to an increase of the pressure on the anterior column on one hand, and, more importantly, a massive increase on the muscle load posteriorly.14,20 This may be the cause of a vicious circle that ends up in this so-called sagittal plane decompensation.17 Therefore there is a rationale for height restoration and maintenance of spinal alignment. Further clinical studies are needed to demonstrate how vertebral body stenting is able to contribute to this.
1. Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS). J. Bone Miner. Res.. 2002;17–4:716-724.
2. Bliuc D., Nguyen N.D., Milch V.E., Nguyen T.V., Eisman J.A., Center J.R. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301–5:513-521.
3. Alvarez L., Alcaraz M., Perez-Higueras A., Granizo J.J., de Miguel I., Rossi R.E., Quinones D. Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine. 2006;31–10:1113-1118.
4. Muijs S.P., Nieuwenhuijse M.J., Van Erkel A.R., Dijkstra P.D. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: evaluation after 36 months. J. Bone Joint Surg. Br.. 2009;91–3:379-384.
5. Heini P.F., Walchli B., Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur. Spine J.. 2000;9–5:445-450.
6. Wardlaw D., Cummings S.R., Van Meirhaeghe J., Bastian L., Tillman J.B., Ranstam J., Eastell R., Shabe P., Talmadge K., Boonen S. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373–9668:1016-1024.
7. Hulme P.A., Boyd S.K., Heini P.F., Ferguson S.J. Differences in endplate deformation of the adjacent and augmented vertebra following cement augmentation. Eur. Spine J.. 2009.
8. Eck J.C., Nachtigall D., Humphreys S.C., Hodges S.D. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J.. 2008;8–3:488-497.
9. Kallmes D.F., Comstock B.A., Heagerty P.J., Turner J.A., Wilson D.J., Diamond T.H., Edwards R., Gray L.A., Stout L., Owen S., Hollingworth W., Ghdoke B., Annesley-Williams D.J., Ralston S.H., Jarvik J.G. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N. Engl. J. Med.. 2009;361–6:569-579.
10. Buchbinder R., Osborne R.H., Ebeling P.R., Wark J.D., Mitchell P., Wriedt C., Graves S., Staples M.P., Murphy B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N. Engl. J. Med.. 2009;361–6:557-568.
11. Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30–24:2806-2812.
12. Ryan P.J., Blake G., Herd R., Fogelman I. A clinical profile of back pain and disability in patients with spinal osteoporosis. Bone. 1994;15–1:27-30.
13. Cooper C., Atkinson E.J., O’Fallon W.M., Melton L.J.3rd. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J. Bone Miner. Res.. 1992;7-2:221-227.
14. Huang M.H., Barrett-Connor E., Greendale G.A., Kado D.M. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J. Bone Miner. Res.. 2006;21–3:419-423.
15. Heaney R.P., Zizic T.M., Fogelman I., Olszynski W.P., Geusens P., Kasibhatla C., Alsayed N., Isaia G., Davie M.W., Chesnut C.H.3rd. Risedronate reduces the risk of first vertebral fracture in osteoporotic women. Osteoporos. Int.. 2002;13–6:501-505.
16. Briggs A.M., Greig A.M., Bennell K.L., Hodges P.W. Paraspinal muscle control in people with osteoporotic vertebral fracture. Eur. Spine J.. 2007;16–8:1137-1144.
17. Briggs A.M., Greig A.M., Wark J.D. The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos. Int.. 2007;18–5:575-584.
18. Rotter R., Fürderer S., Heini P. Vertebral stenting, a new device for vertebral height restoration. Eur. Spine J.. 2008;17:1551.
19. Greig A.M., Bennell K.L., Briggs A.M., Wark J.D., Hodges P.W. Balance impairment is related to vertebral fracture rather than thoracic kyphosis in individuals with osteoporosis. Osteoporos. Int.. 2007;18–4:543-551.
20. Briggs A.M., van Dieen J.H., Wrigley T.V., Greig A.M., Phillips B., Lo S.K., Bennell K.L. Thoracic kyphosis affects spinal loads and trunk muscle force. Phys. Ther.. 2007;87–5:595-607.
21. Wilke H.J., Neef P., Caimi M., Hoogland T., Claes L.E. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine. 1999;24–8:755-762.
22. Sato K., Kikuchi S., Yonezawa T. In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine. 1999;24–23:2468-2474.
23. Orler R., Frauchiger L.H., Lange U., Heini P.F. Lordoplasty: report on early results with a new technique for the treatment of vertebral compression fractures to restore the lordosis. Eur. Spine J.. 2006;15 (2):1769-1775.
24. Braunstein V., Sprecher C.M., Gisep A., Benneker L., Yen K., Schneider E., Heini P., Milz S. Long-term reaction to bone cement in osteoporotic bone: new bone formation in vertebral bodies after vertebroplasty. J. Anat.. 2008;212–5:697-701.