1. Gao, H, et al. Definitive diagnosis of hepatic sinusoidal obstruction syndrome induced by pyrrolizidine alkaloids. J Dig Dis. 2012; 13(1):33–39.
2. Jevtic, D, et al. Veno-occlusive disease in pediatric patients after hematopoietic stem cell transplantation: relevance of activated coagulation and fibrinolysis markers and natural anticoagulants. J Pediatr Hematol Oncol. 2011; 33(3):227–234.
3. Lin, G, et al. Hepatic sinusoidal obstruction syndrome associated with consumption of Gynura segetum. J Hepatol. 2011; 54(4):666–673.
4. Mahgerefteh, SY, et al. Radiologic imaging and intervention for gastrointestinal and hepatic complications of hematopoietic stem cell transplantation. Radiology. 2011; 258(3):660–671.
5. Menke, J. Education and imaging. Hepatobiliary and pancreatic: sinusoidal obstruction syndrome during chemotherapy. J Gastroenterol Hepatol. 2011; 26(6):1083.
6. Sanei, MH, et al. Acute cellular rejection resulting in sinusoidal obstruction syndrome and ascites postliver transplantation. Transplantation. 2011; 92(10):1152–1158.
7. Sebagh, M, et al. Significance of isolated hepatic veno-occlusive disease/sinusoidal obstruction syndrome after liver transplantation. Liver Transpl. 2011; 17(7):798–808.
8. Rubbia-Brandt, L. Sinusoidal obstruction syndrome. Clin Liver Dis. 2010; 14(4):651–668.
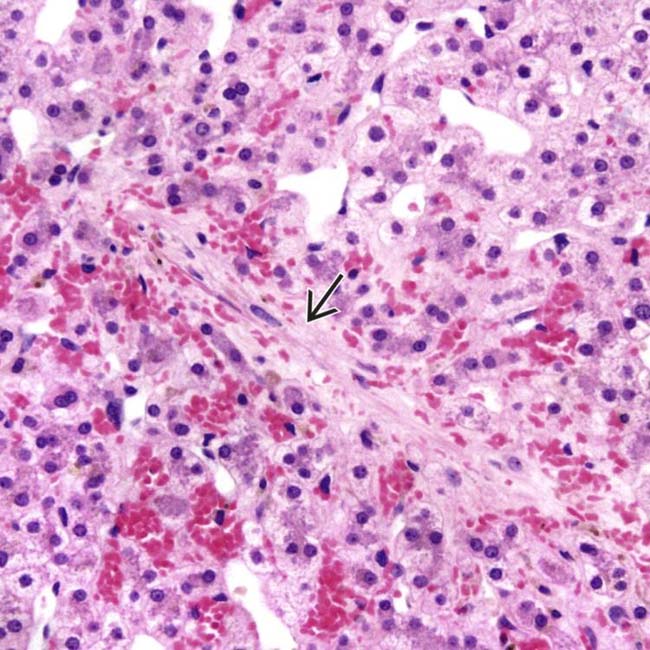
 accompanied by centrizonal sinusoidal congestion is seen in venoocclusive disease (VOD). (Courtesy S. Kakar, MD.)
accompanied by centrizonal sinusoidal congestion is seen in venoocclusive disease (VOD). (Courtesy S. Kakar, MD.)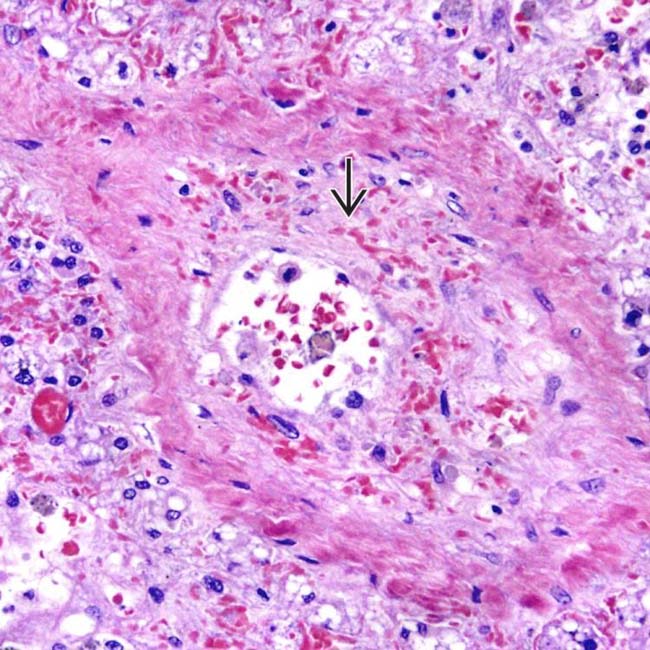
 led to partial occlusion of the lumen of a small hepatic vein in venoocclusive disease. (Courtesy S. Kakar, MD.)
led to partial occlusion of the lumen of a small hepatic vein in venoocclusive disease. (Courtesy S. Kakar, MD.)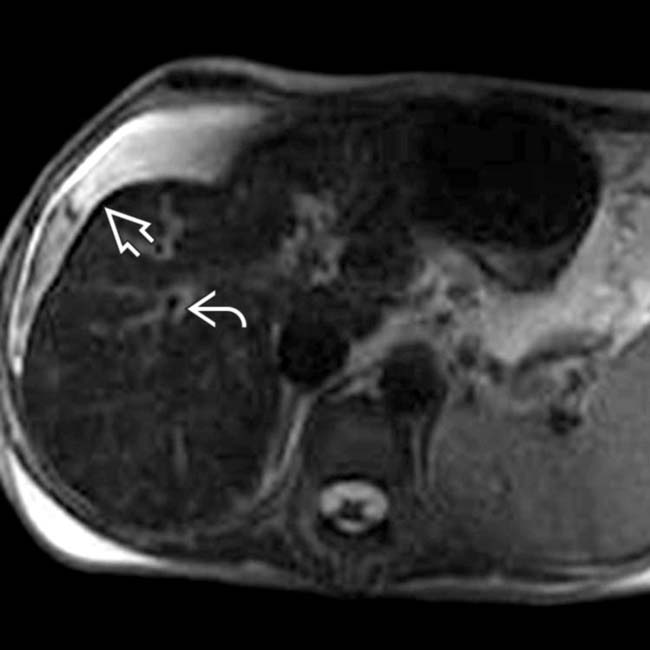
 and periportal edema
and periportal edema  , which are nonspecific findings. Liver biopsy showed sinusoidal congestion and fibrotic venules.
, which are nonspecific findings. Liver biopsy showed sinusoidal congestion and fibrotic venules.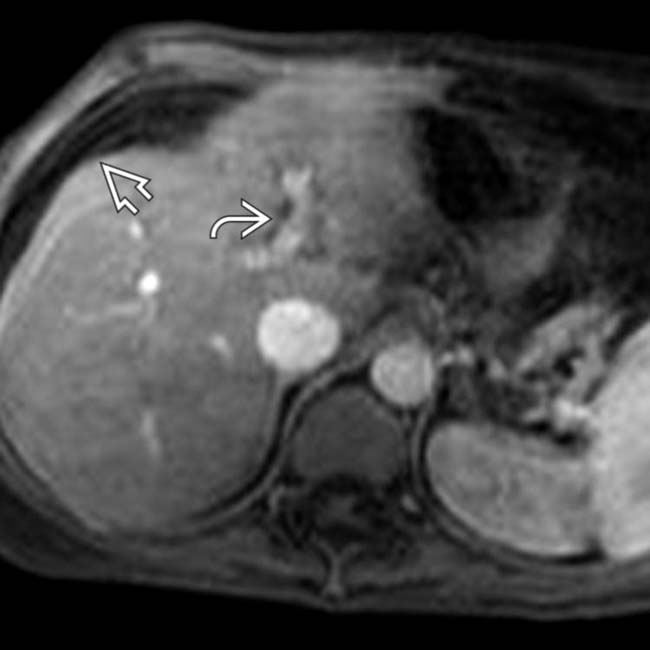
 and periportal edema
and periportal edema  .
.








































