Chapter 77 Vascular Complications After Anterior Cruciate Ligament Reconstruction
Vascular complications after anterior cruciate ligament (ACL) reconstructions cause serious morbidity and potential mortality. Fortunately, their incidence is low. Only a few peer-reviewed case reports provide information,1–5 and even a specific review article on complications after ACL surgery does not mention these rare complications.6
Arterial Complications
Knee arthroscopy is generally a safe procedure with a low incidence of complications. The two largest studies to date report complication rates of 0.54% and 0.8%.7,8 Penetrating popliteal artery injuries were described by DeLee in 6 of 118,540 arthroscopies.7 Small noted 9 cases (of 375,000 arthroscopic procedures) of penetrating trauma to the popliteal artery.8 A subsequent study of 8741 cases done by experienced arthroscopists showed no vascular complications.9 Pseudoaneurysm is the most frequently published popliteal artery lesion after arthroscopy of the knee. It is associated with direct violation of the posterior capsule or previous (open) knee surgery. However, it is still rare and published in case reports only.10–23
Roth and Bray1 described an occlusion of the popliteal artery 7 cm proximal to the knee joint line. A composite graft, consisting of a polypropylene ligament augmentation and the middle third of the quadriceps patellar tendon, was used as ACL reconstruction and fixed to the lateral femur with a single staple in an over-the-top position. The patient had a burning pain in the foot 6 hours after surgery. Doppler signals of the pedal arteries were intact. The symptoms subsided. Dull aching at the posterior calf occurred at 3 weeks. Pain and dysesthesia in the foot recurred at 6 weeks. Angiography revealed the occlusion. The artery was trapped between the composite graft and the femur at surgical exploration. A saphenous bypass was performed.
Spalding et al2 reported a case of unilateral claudication 8 years after ACL reconstruction with use of a GoreTex polytetrafluoroethylene braided ligament. Computed tomography (CT) analysis demonstrated a cyst had formed around the femoral insertion of the ruptured GoreTex ligament. The cyst was excised without the need for vascular repair.
Evans et al3 reported a pseudoaneurysm of the medial inferior genicular artery following ACL reconstruction with a central third patellar tendon graft fixed with interference screws into the tibia and femur. It was detected at 5 weeks postsurgery with a 10-day history of pulsating swelling on the medial side of the knee with normal femoral, popliteal, and distal pulses. Diagnosis was made by contrast angiography. Ligation of the artery and removal of the thrombus from the pseudoaneurysm led to an excellent recovery. The cause of the lesion was elevation of the periosteum on the medial side of the tibia for tibial tunnel preparation.
Aldridge et al4 described an avulsion of the middle genicular artery after arthroscopic ACL reconstruction with a bone–patellar tendon–bone (BPTB) autograft fixed with interference screws in both the tibia and femur. After tourniquet release, serious hemorrhage was detected with absent dorsal pedal pulse and a cold foot. The patient had a history of intravenous contrast dye allergy; therefore a CO2 arteriogram was performed with no evidence of vascular injury. The symptoms resolved overnight. At 2 weeks, the patient experienced difficulty with knee extension and felt a mass in the popliteal fossa. No mass was felt at examination, and pedal pulses were normal. Ultrasound examination showed no sign of venous thrombosis. At 4 weeks, a palpable mass in the fossa with 30-degree flexion contracture of the knee led to hospital readmission. Contrast angiography showed the vascular lesion. Surgical exploration revealed a tear in the popliteal artery, which was repaired with a short running stitch after removal of the hematoma. There was no rupture of the posterior capsule, and the avulsion of the middle genicular artery was hypothesized to have occurred during débridement of the femoral ACL stump.
Our first case was a 44-year-old male with a previous history of open medial and lateral ligament repair of the same knee 15 years previously (motor vehicle accident). The hospital recovery was uneventful after ACL reconstruction. On day 17 postsurgery, he experienced pain and swelling in the popliteal fossa of the knee. The complaints partially resolved with physiotherapy. Two days later, the fossa pain returned with alterations of skin color, sensory loss, and an increasingly cold foot. Adequate dorsal pedal and posterior tibial pulses were noted. Duplex ultrasound examination showed no sign of venous thrombosis. Angiography revealed a subtotal occlusion of the popliteal artery at the level of the superior genicular artery (Fig. 77-1). An embolectomy was performed using a Fogarty catheter inserted in the femoral artery. The pedal pulses were diminished after embolectomy, and a second angiography was performed. The occlusion at the level of the popliteal artery was no longer detected. No further emboli were noted; however, the peripheral flow qualified as too slow and suggestive of small distal occlusions. Anticoagulant therapy with intravenous heparin as well an epidural analgesia were administered until complete recovery of peripheral circulation was attained. The patient developed a superficial infection of the groin wound, which was treated by antibiotics. He was mobilized and discharged after 8 days. Sensory loss of the foot slowly recovered after 4 months. Vascular analysis in rest and strenuous activity was performed at 4 months. He had no more complaints, a symmetrical ankle-brachial index in both legs, and intact pulses at the foot and ankle. Our hypothesis of the cause was the traumatic knee dislocation 15 years previously. Precursors could have been preexistent intimal vascular damage or adhesions of the artery at the level of the superior genicular artery in combination with the use of the tourniquet.
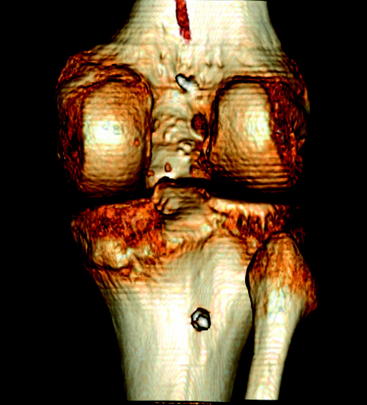
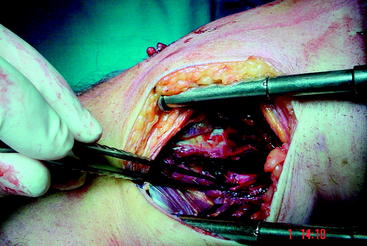
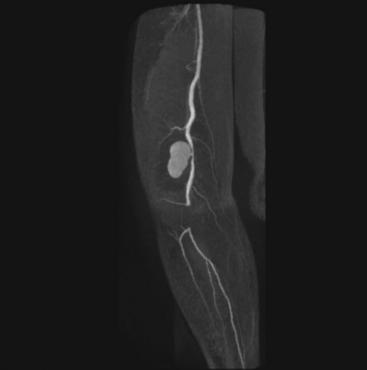
We have previously published our second case of pseudoaneurysm of the popliteal artery due to damage by the bicortical tibial drill.5 A 24-year-old man had an ACL reconstruction using a quadruple hamstring graft. The patient was allowed full weight bearing, and an aggressive rehabilitation was started the day after surgery. The hospital stay was uneventful. Twelve days after surgery, the patient complained of progressive pain in the popliteal fossa that had started on day 5 postsurgery. On physical examination, a pulsating mass was felt in the popliteal fossa and there was a sensory loss of the medial foot as well as the plantar heel. The dorsal pedal and posterior tibial pulses were intact. Duplex analysis and CT angiography demonstrated a pseudoaneurysm of the infragenicular popliteal artery near the site of the bicortical tibial screw (Fig. 77-2). The pseudoaneurysm measured 3.5 × 1.5 cm on the sagittal view and 3.5 × 4 cm in the frontal aspect (Figs. 77-3 and 77-4). Surgical exploration was immediately performed. A vascular defect (3 mm) of the infragenicular popliteal artery was found just proximal to the origin of the anterior tibial artery (Fig. 77-5). However, the tip of the bicortical screw was not in direct contact with the arterial lesion. Apparently the 3.2-mm drill used for the bicortical screw had caused perforation of the popliteal artery. An arteriotomy was performed, and an intimal lesion was repaired. A venous patch was used to close the arterial defect. A Fogarty catheter was inserted to remove small clots present in the tibioperoneal trunk. Aspirin was prescribed for 3 months. No complications occurred after the vascular repair. Functional treatment using continuous passive motion (CPM) was started the day after surgery. The muscular and proprioceptive rehabilitation was initiated after wound healing occurred. At 4-month follow-up, there was full range of motion of the knee. Lachman and anterior drawer test were 0 to 2 mm (according to International Knee Documentation Committee [IKDC]) with an absent pivot-shift test. Neurological evaluation by a neurologist showed a sensory loss of the saphenous and medial plantar nerves and, to a lesser degree, sensory loss of the superficial peroneal nerve of the right leg. There was no loss of motor function. The dorsal pedal and posterior tibial pulses were intact.
Our most recent case was a 50-year-old woman with a pseudoaneurysm of the popliteal artery after ACL reconstruction. She was seen 1 week postsurgery with pain in the popliteal fossa, absent foot pulses and sensory loss in the foot. Doppler examination showed weak signals in the foot. MRI angiography revealed a pseudoaneurysm of the supragenicular popliteal artery and a 4-cm occlusion proximal to the tibioperoneal trunk (Fig. 77-6). Surgical exploration on postsurgery day 9 showed damage to the artery in line with the tibial bicortical screw. Just as in our previous case, the tip of the bicortical screw was not in direct contact with the artery. The drill used for the bicortical screw had caused perforation of the popliteal artery. There was no hematoma around the pseudoaneurysm, nor was it in line with the Bone Mulch Screw fixation of the femur. The vascular surgeon thought this lesion to be preexistent and not related to the ACL surgery. The pseudoaneurysm was ligated and a saphenous bypass performed. A 5-day course of intravenous heparin was administered in combination with aspirin. Aspirin was continued after discharge. Follow-up is now 3 months; sensory loss of the plantar foot and decreased motor function of the flexor hallucis longus muscle are still present.
Post et al24 studied the relative position of the neurovascular structures at risk when drilling bicortical screws for tibial fixation in ACL reconstruction. Arthroscopic tibial tunnels were placed in cadaver human knees using lateral roentgen graphs for accurate positioning. A 4.5-mm bicortical drill hole was placed perpendicular to the tibial surface, 1 cm distal to the tibial tunnel. The distances from the posterior tibial drill exit point to the nearby neurovascular structures were measured with a caliper. The closest structure to the exit point was the bifurcation of the popliteal artery/vein (11.4 ± 0.6 mm). The next closest was the anterior tibial vein (11.7 ± 1.6 mm). The closest any individual hole came to a neurovascular structure was 3.5 mm from the anterior tibial vein. The researchers concluded that bicortical screw and spiked washer fixation of soft tissue ACL grafts appears to be relatively safe.24 Variations in anatomy and surgical technique are possible, and care should be taken in drilling through the posterior cortex.
Possible recommendations to prevent neurovascular damage in drilling bicortical tibia screws are the use of a drill stop5 or directing the screw toward the fibular head instead of the posterior cortex.25 A single cortex fixation on the tibia is another possible safeguard without compromising stability of fixation.26
All cases show a certain delay in diagnosis (2–6 weeks postsurgery to 8 years). Damage to the popliteal artery can occur even with an all-inside technique of arthroscopic ACL reconstruction and fixation as well as with any type of graft. Other than the GoreTex rupture ligament case,2 all patients maintained adequate ACL stability after vascular surgery. The neurological deficits, however, may be permanent.
Venous Complications
The incidence of deep vein thrombosis (DVT) in orthopaedic surgery is amongst the highest in clinical practice. DVT is complicated by pulmonary embolism (PE) and the postthrombotic syndrome. The former may be fatal in its immediate course and may result in pulmonary hypertension in the long term. The latter affects 23% of limbs 2 years after DVT, 35% to 69% at 3 years, and 49% to 100% at 5 to 10 years.27 A recent meta-analysis of DVT after knee arthroscopy without thromboprophylaxis showed an overall DVT rate of 9.9% (3.1% to 17.9%) when routine screening using ultrasound or contrast venography is used. The proximal DVT rate is 2.1% (0% to 4.9%).28 The range of incidence among different studies is mainly related to two factors: (1) heterogenous groups of variable age, risk factors, and types of surgery and (2) variable experience of ultrasound technologists in detecting DVT in comparable populations.27
Delis et al27 found 50% of the DVT patients to be completely asymptomatic. Lohman sign and thigh circumference measurements were unreliable. They also examined the history of DVT if treated (aspirin in calf DVT, heparin-warfarin in proximal DVT). Following early diagnosis, total clot lysis was documented in 50% and partial clot lysis in the remaining 50% within 118 days median follow-up. Segmental venous reflux developed in at least 75% of the legs sustaining thrombosis. A previous thrombosis or the presence of two or more risk factors for thromboembolism significantly increased the incidence of DVT. No symptoms or signs of PE were documented.27 Geerts et al reviewed the evidence-based literature for thromboprophylaxis. They suggest not using thromboprophylaxis in knee arthroscopy, other than early mobilization. For patients undergoing arthroscopic knee surgery who are at higher than usual risk based on preexisting venous thromboembolic risk factors or following a prolonged or complicated procedure, they suggest thromboprophylaxis with low-molecular-weight heparin (Grade 2B level of evidence).29 The authors do not present further definitions of their suggestions or specific guidelines for thromboprophylaxis after ACL reconstructions.
The incidence of DVT in ACL reconstruction has been prospectively analyzed with duplex ultrasound by Cullison et al.30 They found an incidence of DVT of 1.5% without thromboprophylaxis. However, one must note their selected population: all male (no previous surgery) with an average age of 26.5 years (the oldest patient is 39 years old). Their data cannot be extrapolated to a female population or patients with DVT risk factors or previous surgery.
Hirota et al31 quantified pulmonary emboli after tourniquet release in patients undergoing ACL reconstruction (extramedullary procedure) versus total knee arthroplasty (intramedullary procedure). They chose these two groups to have more than 60 minutes of tourniquet time. This period was found to significantly increase the risk for DVT according to Demers et al.32 Hirota et al detected pulmonary emboli in all patients after release of the tourniquet using transesophageal echocardiography with a peak at 30 to 40 seconds postrelease. The amount of emboli formed was defined as %Ae (percentage of total emboli formed to the right atrial area). The atrial emboli percentage returned to baseline levels 2 minutes after tourniquet release in the ACL group. They found a significant linear correlation between the atrial emboli percentage and the duration of tourniquet inflation in the ACL group. In comparison, the total knee arthroplasty group had a significant larger atrial emboli percentage (four- to fivefold) with no return to baseline levels during the assessment period. No patient in either group showed signs of PE.31
Pulmonary emboli occur in all patients with ACL reconstructions after tourniquet release. In addition, PE may occur as a result of proximal DVT.33 No incidence is known for PE after ACL reconstruction.
1 Roth JH, Bray RC. Popliteal artery injury during anterior cruciate ligament reconstruction: brief report. J Bone Joint Surg. 1988;70B:840.
2 Spalding TJW, Botsford DJ, Ford M, et al. Popliteal artery compression: a complication of Gore-tex anterior cruciate ligament reconstruction. J Bone Joint Surg. 1996;78B:151-152.
3 Evans JD, Boer de MT, Mayor P, et al. Pseudoaneurysm of the medial inferior genicular artery following anterior cruciate ligament reconstruction. Ann R Coll Surg Engl. 2000;82:182-184.
4 Aldridge JMIII, Weaver JP, Mallon WJ. Avulsion of the middle genicular artery: a previously unreported complication of anterior cruciate ligament repair. A case report. Am J Sports Med. 2002;30:748-750.
5 Janssen RPA, Scheltinga MRM, Sala HAGM. Pseudoaneurysm of the popliteal artery after anterior cruciate ligament reconstruction with bicortical tibial screw fixation. Arthroscopy. 2004;20:E4-E6.
6 Allum R. Aspects of current management. Complications of arthroscopic reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 2003;85B:12-16.
7 DeLee JC. Complications of arthroscopy and arthroscopic surgery: results of a national survey. Arthroscopy. 1985;1:214-220.
8 Small NC. Complications in arthroscopic surgery: the knee and other joints. Arthroscopy. 1986;2:253-258.
9 Small NC. Complication in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy. 1988;4:216-221.
10 Beck DE, Robinson JG, Hallet JW. Popliteal artery pseudoaneurysm following arthroscopy. J Trauma. 1986;26:87-89.
11 Manning MP, Marshall JH. Aneurysm after arthroscopy. J Bone Joint Surg. 1987;69:151.
12 Vincent GM, Stanish WD. False aneurysm after arthroscopic meniscectomy. A report of two cases. J Bone Joint Surg. 1990;72:770-772.
13 Armato DP, Czamecki D. Geniculate artery pseudoaneurysm: a rare complication of arthroscopic surgery. Am J Roentgenol. 1990;155:659. (letter)
14 Guy RJ, Spalding TJ, Jarvis LJ. Pseudoaneurysm after arthroscopy of the knee. A case report. Clin Orthop Rel Res. 1993;295:214-217.
15 Ritt MJ, Te Slaa RL, Koning J, et al. Popliteal pseudoaneurysm after arthroscopic meniscectomy. A report of two cases. Clin Orthop Relat Res. 1993;295:198-200.
16 Hilborn M, Munk PL, Miniaci A, et al. Pseudoaneurysm after therapeutic knee arthroscopy: imaging findings. Am J Roentgenol. 1994;163:637-639.
17 Aldrich D, Anschuetz R, Lopresti C, et al. Pseudoaneurysm complicating knee arthroscopy. Arthroscopy. 1995;11:229-230.
18 Potter D, Morris-Jones W. Popliteal artery injury complicating arthroscopic meniscectomy. Arthroscopy. 1995;11:123-126.
19 Sarrosa EA, Ogilvie-Harris DJ. Pseudoaneurysm as complication of knee arthroscopy. Arthroscopy. 1997;13:644-645.
20 Carlin RE, Papenhausen M, Farber MA, et al. Sural artery pseudoaneurysms after knee arthroscopy: treatment with transcatheter embolization. J Vasc Surg. 2001;33:170-173.
21 Mullen DJ, Jabaji GJ. Popliteal pseudoaneurysm and arteriovenous fistula after arthroscopic meniscectomy. Arthroscopy. 2001;17:E1.
22 Kiss H, Drekonja T, Grethen C, et al. Postoperative aneurysm of the popliteal artery after arthroscopic meniscectomy. Arthroscopy. 2001;17:203-205.
23 Audenaert E, Vuylsteke M, Lissens P, et al. Pseudoaneurysm complicating knee arthroscopy. A case report. Acta Orthop Belg. 2003;69:382-384.
24 Post WR, King SS. Neurovascular risk of bicortical drilling for screw and spiked washer fixation of soft-tissue anterior cruciate ligament graft. Arthroscopy. 2001;17:244-247.
25 Howell SM. Personal correspondence. 2005.
26 Prodromos CC, Han YS, Keller BL, et al. Stability results of hamstring anterior cruciate ligament reconstruction at 2- to 8-year follow-up. Arthroscopy. 2005;21:138-146.
27 Delis KT, Hunt N, Strachan RK, et al. Incidence, natural history and risk factors of deep vein thrombosis in elective knee arthroscopy. Thromb Haemost. 2001;86:817-821.
28 Ilahi OA, Reddy J, Ahmad I. Deep venous thrombosis after arthroscopy: a meta-analysis. Arthroscopy. 2005;21:727-730.
29 Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism. The seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126:338S-400S.
30 Cullison TR, Muldoon MP, Gorman JD, et al. The incidence of deep venous thrombosis in anterior cruciate ligament reconstruction. Arthroscopy. 1996;12:657-659.
31 Hirota K, Hashimoto H, Tsubo T, et al. Quantification and comparison of pulmonary emboli formation after pneumatic tourniquet release in patients undergoing reconstruction of anterior cruciate ligament and total knee arthroplasty. Anest Analg. 2002;94:1633-1638.
32 Demers C, Marcoux S, Ginsberg JS, et al. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med. 1998;158:47-50.
33 Williams JS, Hulstyn MJ, Fadale PD, et al. Incidence of deep vein thrombosis after arthroscopic knee surgery: a prospective study. Arthroscopy. 1995;11:701-705.