Chapter 32 Valgus Malalignment
Diagnosis, Osteotomy Techniques, and Clinical Outcomes
INDICATIONS
CONTRAINDICATIONS
Relative contraindications include severe angular deformity (consideration in these cases should be given to a double osteotomy of the distal femur and proximal tibia), limited knee range of motion (>15° flexion contracture or <90° of flexion), poor motivation, or poor rehabilitation potential. Rehabilitation issues would include the inability to follow postoperative weight-bearing restrictions and the use of drugs or substances such as nicotine that may interfere with bone healing. The extent of lateral joint arthrosis (as defined by amount of cartilage loss on femoral and tibial surfaces) has, to our knowledge, not been shown to have a demonstrable effect on outcome. Therefore, we do not use the amount of radiographic or clinical joint space loss as a criterion or contraindication. The presence of patellofemoral arthrosis as a relative contraindication is controversial. Some studies have shown that arthrosis of the patellofemoral joint has no bearing on the outcome, whereas others have even shown improvement in patellofemoral symptoms with DFO.14
CLINICAL BIOMECHANICS
The weight-bearing line (WBL) of the lower extremity is defined as the line drawn from the center of the femoral head through the center of the ankle mortise. Based on where this line crosses the knee joint, overall limb alignment is considered varus (medial to the center of the knee), valgus (lateral to the center of the knee), or neutral relative to the center of the knee. Based on morphologic studies of normal subjects with neutral overall alignment, Hsu and coworkers8 determined that 75% of weight-bearing forces are transmitted through the medial compartment of the knee in a one-legged simulated weight-bearing stance. Other studies have determined that 60% of the load is passed through the medial compartment during weight-bearing.1,11 Alterations in the overall alignment will change these forces and create an unfavorable mechanical environment, potentially leading to injury and degeneration of the overstressed compartment that may be stopped or slowed by timely correction of the malalignment.13
Osseous deformities should be understood in the context of “normal” anatomy and “physiologic” valgus. Kapandji9 illustrated that the average distal femoral angle is 7% to 9% of valgus, and the average proximal tibial angle is 0% to 3% of varus, producing the overall tibiofemoral angle of 5% to 7% of valgus, which, after accounting for hip offset, leads to a mechanical limb axis through the center of the knee. Osseous deformities in the valgus knee are usually limited to the lateral femoral condyle, which is typically hypoplastic, thus leading to excessive distal femoral valgus. Conversely, the lateral tibial plateau is usually well preserved, except in the case of fracture.
The important distinction is that for the majority of valgus knees, the deformity lies in the distal femur and not in the tibia. In some cases, this excessive distal femoral valgus may be minimal, but in other more severe cases, the distal femoral angle can approach 15% to 20% of valgus. Whereas the exact prevalence of valgus deformity of the knee is unknown, it is generally considered less common than varus deformity about the knee. Cooke and associates3 examined full-length radiographs of 167 white patients with osteoarthritis. Valgus alignment was seen in 24% and varus in 76%. In addition, valgus deformity has been noted to be more common in females, patients with inflammatory arthritis, post-traumatic arthritis, and those with metabolic abnormalities such as rickets or renal osteodystrophy.
The rationale of the DFO is to correct the excessive tibiofemoral valgus by shifting the mechanical axis line from the lateral compartment to a more median or even medial position. Historically, this correction has been performed both above and below the level of the joint line. Initial reports of correction of painful valgus deformity described a proximal tibial varus-producing osteotomy. However, Coventry4 recommended that deformity of greater than 12% of tibiofemoral valgus should be corrected above the joint line in order to avoid excessive joint line obliquity, which leads to increased shear stresses across the joint, ligamentous and capsular attenuation, and subsequent joint subluxation. A general rule is that the osteotomy should be performed at the site of the primary deformity, which in most patients with valgus deformity lies in the distal femur.
CLINICAL EVALUATION
Radiographic Evaluation
Critical Points RADIOGRAPHIC EVALUATION
PREOPERATIVE PLANNING
The radiographic studies are essential in the preoperative planning of the intended corrections. These are determined by calculating the tibiofemoral angle and the proximal tibial and distal femoral angles (Fig. 32-1). The goal is to shift the mechanical axis so that it falls through the center or just medial to the center of the knee. Overcorrection of the deformity, as for example in high tibial osteotomy (HTO), will place extreme loads through the medial compartment. The authors recommend instead aiming for the 0% to 4% of valgus that the literature suggests as acceptable. When performing an osteotomy as an ancillary procedure to cartilage repair in young patients, the goal of correction is to restore the WBL through the center of the knee, because overcorrection may be detrimental to long-term joint health. When used to treat cases of arthritis, in which undercorrection can lead to poor outcome, the minimum correction should result in neutral alignment with the maximum correction resulting in the WBL falling through the medial tibial spine. These corrections result in various degrees of tibiofemoral valgus alignment depending on other parameters such as hip offset. This is most easily determined preoperatively using tracing paper cutouts of the proposed osteotomy on standing long-alignment films.
OPERATIVE TECHNIQUE
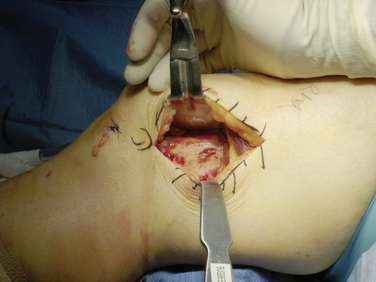
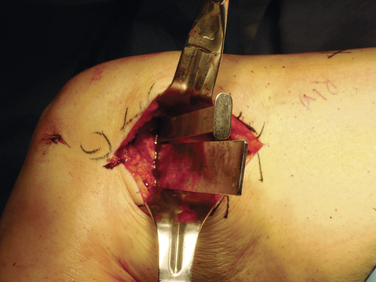
The operated limb including the ipsilateral hip is prepared free, and a small bump is placed under the hip to align the extremity in the coronal plane. For reasons described previously, a lateral opening wedge osteotomy fixed with an osteotomy plate and filled with either allograft or iliac crest bone graft is preferred. A sterile tourniquet is placed, but used only if necessary. An 8- to 10-cm incision is made over the lateral aspect of the distal femur. The iliotibial band is incised in line with the incision, and the vastus lateralis is dissected posteriorly off the lateral intermuscular septum to expose the femoral shaft and the metaphyseal flare (Fig. 32-2). The joint can be entered, if necessary.
Critical Points SURGICAL TECHNIQUE
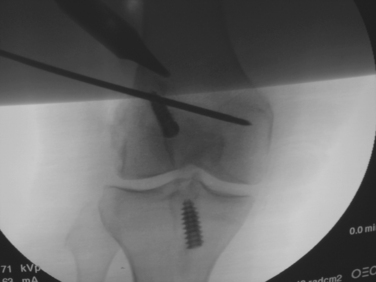
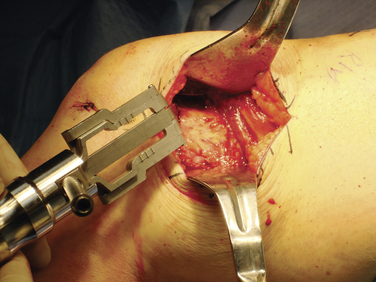
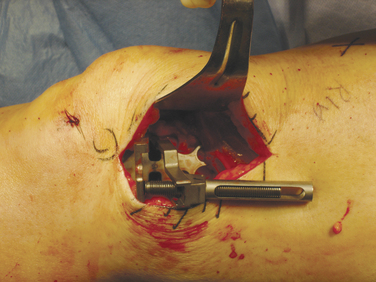
Using fluoroscopy, the starting point for the osteotomy is located, which is approximately 3 cm above the lateral femoral epicondyle. The guide pin is angled medially and distally so that it exits the cortex at the level of the medial epicondyle (Fig. 32-3). The goal is to create the osteotomy in the metaphyseal bone, which has excellent healing potential without violating the patellofemoral joint. The superiormost aspect of the trochlea should be palpated to ensure that the guide pin is not too distal. If this is the case, the superior aspect of the joint will be violated during the osteotomy. In these instances, the guide pin should be removed and placed more proximally.
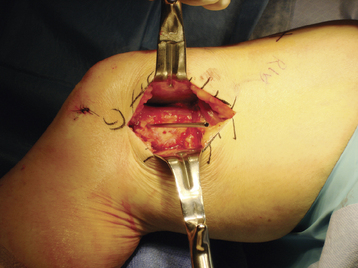
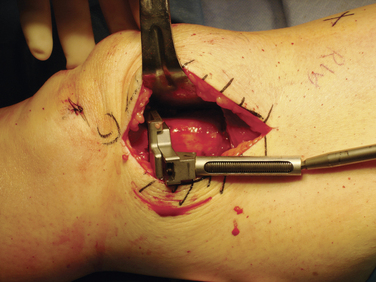
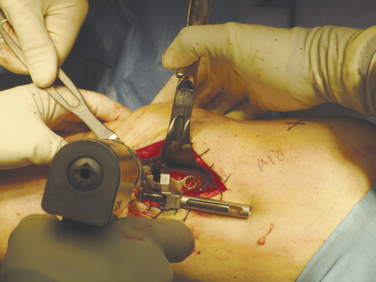
Once the first guide pin is accurately placed, a second guide pin should be placed either directly anterior or directly posterior to that pin in the same plane, so that both pins completely overlap on an AP view of the distal femur. This ensures that an osteotomy created parallel to the plane of both guide pins will be perpendicular to the long axis of the femur in the lateral plane. After the guide pins have been placed in the appropriate position on the AP view (Fig. 32-4), the osteotomy may then be performed using both pins as a guide. An oscillating saw with a 1-inch saw blade is used to start the osteotomy, either just above or just below the guide pins, to create the proper plane (Fig. 32-5). Once this has been done, wide osteotomes are used to complete the osteotomy (Fig. 32-6). The goal is not to create a complete fracture, but instead to keep the medial cortex intact to act as a hinge. Occasionally, the medial cortex is perforated to allow for opening of the osteotomy, which may be done with a small K-wire.
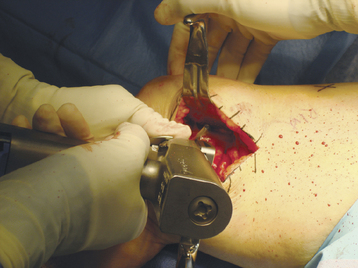
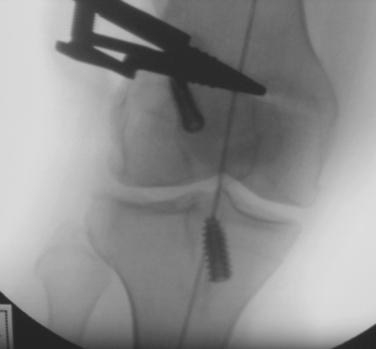
Once the majority of the cortex has been freed, the distraction device is placed in the osteotomy site (Fig. 32-7) and slowly distracted (Fig. 32-8). The goal is for the mechanical axis to pass through the medial tibial spine. The amount of distraction required to attain this goal correlates with the amount of correction attained. For small osteotomies, this is usually 5 to 8 mm, and for large osteotomies, 10 to 15 mm. Once the desired amount of correction is obtained, fluoroscopy is used to evaluate the WBL. An electrocautery cord is stretched from the center of the femoral head to the center of the ankle and the overall mechanical axis is assessed (Fig. 32-9). Undercorrection is associated with a higher rate of failure, whereas overcorrection places extreme loads on the medial side. If the mechanical axis is over- or undercorrected, it can be adjusted at this time using the distraction device. Once the correction is believed to be appropriate, a plate is used to secure the osteotomy (Fig. 32- 10). The plate is fixed using three unicortical cancellous screws distally and three bicortical cortical screws proximally (Figs. 32-11 to 32-13). Depending on the patient, either autologous iliac crest bone graft and/or allograft bone is used (Fig. 32-14). For younger, female patients and those concerned with cosmesis, allograft is preferred, but both methods of bone grafting have been equally successful. In the authors’ clinical experience since 2005 (encompassing 44 cases), no instance of delayed union or nonunion occurred. Of these 44 cases, 13 were performed using only autograft, 7 received only allograft, and 23 received a combination of both. This was supplemented with demineralized bone matrix (DBM) in 21 cases, and platelet-rich plasma (PRP) in 4 cases. One osteotomy was secured using only DBM putty. Although studies to date show no clear superiority of either method, our experience suggests that more rapid healing occurs when autograft is used in some fashion, but patient characteristics and the size of correction also play an important role in the healing process of opening wedge osteotomies.
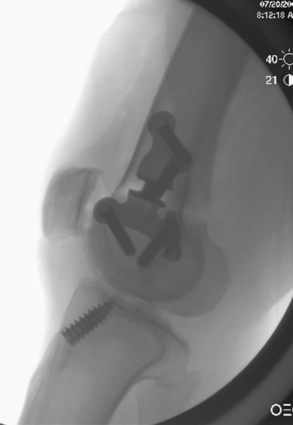
FIGURE 32-13 Intraoperative lateral fluoroscopic view shows plate and screw fixation of the osteotomy.
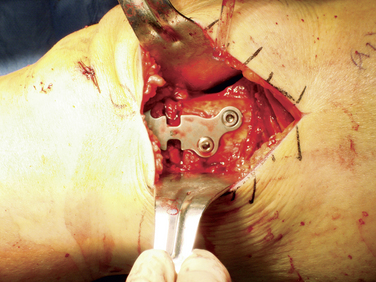
FIGURE 32-14 Intraoperative view of fixed osteotomy plate after placement of the autologous bone graft and bone matrix.
Postoperatively, the patient is placed in a knee immobilizer overnight for pain control. If osteochondral allografting has also been performed concomitantly, a range of motion brace is placed on postoperative day 1. Patients are started on range of motion exercises immediately, and isometric strengthening is initiated when pain and swelling subside. Patients are kept touch-down weight-bearing for 8 to 12 weeks or until radiographic evidence of healing is confirmed. At 4 weeks, patients are started on a low-resistance exercise bike; resistance training is initiated when the osteotomy is healed (Fig. 32-15). Regular activities are usually resumed at approximately 6 months postoperatively, with continued improvement up to a year.
CLINICAL OUTCOMES FROM OTHER AUTHORS
Compared with HTO, very few reports have been published in the orthopaedic literature on the results of distal femoral varus-producing osteotomy for painful lateral compartment gonarthrosis. The first study for lateral compartment gonarthrosis was published by Coventry in 1987,4 who described the results of 31 knees that underwent a varus-producing proximal tibial osteotomy. In this report, 77% of cases were considered successful. Failures occurred in patients with a large valgus deformity or in whom the results of the surgery produced a tilt of the articular surface greater than 10%. For these patients, Coventry4 recommended a distal femoral varus-producing osteotomy.
The first report of varus-producing DFO was by Healy and colleagues in 1988.7 The series included 23 patients (average age, 56 yr) with painful valgus deformity of the knee with lateral joint space narrowing. Diagnoses included osteoarthritis in 15, post-traumatic osteoarthritis in 3, rheumatoid arthritis in 3, and renal osteodystrophy in 2. The technique used in this series included a medial closing wedge osteotomy in all patients, fixed with a blade plate. Results an average of 4 years postoperatively were good or excellent in 83% (19 of 23). In the osteoarthritis subgroup, 93% had good or excellent outcomes. The authors of this study concluded that 86% of the patients were satisfied with their outcome; however, they did not recommend the procedure in patients with rheumatoid arthritis or decreased range of motion.
McDermott and coworkers10 reported their experience with distal femoral varus-producing osteotomy in 24 patients with painful valgus deformity of the knee. The average age at the time of operation was 53 years. The goal of the procedure was to obtain a final tibiofemoral angle of 0%. A medial closing wedge osteotomy technique was used, fixed with a blade plate in all patients. At follow-up 4 years postoperatively, 22 patients (92%) had a successful result and were satisfied. The greatest improvement was in the category of pain. There was 1 fixation failure, and 1 patient developed medial compartment gonarthrosis and converted to TKR.
Edgerton and associates5 followed 24 knees for 5 to 11 years (average, 8.3 yr) after DFO for painful valgus deformity of the knee. At follow-up, 71% of patients had good or excellent results, with no differences in those followed for longer periods. Complications occurred in 63% of the cases, including nonunion (25%), and loss of correction (21%). Both of these complications were associated exclusively with staple fixation, which the authors subsequently abandoned. Thirteen percent of the cases converted to TKR. The authors concluded that with current indications and techniques, a DFO is effective in up to 80% at long-term evaluation if the fixation is rigid, the correction is adequate, and the procedure is done relatively early in the course of the disease.
Finkelstein and colleagues6 reported on 21 knees that underwent DFO for painful valgus deformity and were followed long term (mean, 133 mo; range, 97–240 mo) or until failure. A medial-based closing wedge osteotomy fixed with a blade plate was performed. The study reported that 13 osteotomies survived, 7 failed, and 1 patient died. The probability of survival at 10 years was 64%. The authors concluded that this is an effective procedure for relieving pain in patients with symptomatic valgus deformity of the knee.
Wang and Hsu14 reported on 30 knees in 30 patients that were managed with distal femoral varus osteotomy (DFVO) for the treatment of noninflammatory lateral compartment arthritis of the knee associated with a valgus deformity. Twelve knees had isolated lateral compartment arthritis, 10 had mild to moderate degenerative changes in the other two compartments, and 8 knees had severe patellofemoral arthritis in addition to lateral compartment disease. The osteotomy site was fixed with a 90° blade plate. At an average follow-up of 99 months, 25 patients (83%) had a satisfactory result and 2 had a fair result according to the Hospital for Special Surgery rating system. The remaining 3 patients converted to a TKR. With conversion to TKR as the endpoint, the cumulative 10-year survival rate for all patients was 87% (95% confidence interval [CI], 69%–100%). Improvement in patellar tracking, which persisted at the time of the latest follow-up, was observed in 7 of 8 knees with associated severe patellofemoral arthritis. The authors concluded that DFVO with blade plate fixation is a reliable procedure for the treatment of lateral compartment osteoarthritis of the valgus knee and that the result of the osteotomy does not appear to be affected by the presence of severe patellofemoral arthritis.
Backstein and coworkers2 reported on 40 DFOs followed a mean of 123 months. At the most recent follow-up, 24 knees (60%) had good or excellent results, 3 (7.5%) had fair results, and 3 (7.5%) had poor results. Four in the fair or poor categories were awaiting TKR and 8 (20%) had been converted to TKR. The mean Knee Society objective score improved from 18 points (range, 0–74) to 87.2 points (range, 50–100). The mean Knee Society function score improved from 54 points (range, 0–100) to 85.6 points (range, 40–100). The 10-year survival rate of the DFO was 82% (95% CI, 75%–89%) and the 15-year survival rate was 45% (95% CI, 33%–57%).
COMPLICATIONS
One concern after DFO is the potential difficulty in performing a subsequent knee replacement, if necessary. Nelson and associates12 retrospectively evaluated the results of TKR performed after varus osteotomy of the distal part of the femur. The study group included nine patients (11 knees) with an average age of 44 years. The mean interval from osteotomy to TKR was 14 years, and the average time to follow-up after TKR was 5 years. The Knee Society score increased from 35 points before TKR to 84 points after TKR. Of note, a constrained prosthesis was required in 5 of the 11 knees. Two knees reported excellent results, 5 had a good result, and 4 had a fair result. The authors concluded that whereas TKR is effective for pain relief and improvement of function after DFO, it is technically more challenging and the results are inferior when compared with the results of primary arthroplasty performed without prior osteotomy of the knee.
In contrast to the previous report, Finklestein and colleagues6 reported on seven knees that converted to TKR after DFVO. The authors believed that at the time of conversion, there was little or no scarring and no difficulty with exposure. Similarly, there was no difficulty gaining correct femoral alignment. The authors believed that in some patients in whom there is difficulty with soft-tissue balancing and patellar tracking because of severe valgus deformity, a varus osteotomy of the distal part of the femur could make a future TKR technically easier. It should be noted that these studies involved conversion of closing wedge osteotomies rather than of opening wedge osteotomies. This scarce and somewhat conflicting data reflect the limited experience with conversion of lateral opening wedge osteotomies to TKR.
1 Andriacchi T.P. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25:395-403.
2 Backstein D., Morag G., Hanna S., et al. Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty. 2007;22(4 suppl 1):2-6.
3 Cooke T.D., Li J., Scudamore R.A. Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am. 1994;25:387-393.
4 Coventry M.B. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69:32-38.
5 Edgerton B.C., Mariani E.M., Morrey B.F. Distal femoral varus osteotomy for painful genu valgum. A five- to 11-year follow-up study. Clin Orthop Relat Res. 1993;288:263-269.
6 Finkelstein J.A., Gross A.E., Davis A. Varus osteotomy of the distal part of the femur. A survivorship analysis. J Bone Joint Surg Am. 1996;78:1348-1352.
7 Healy W.L., Anglen J.O., Wasilewski S.A., Krackow K.A. Distal femoral varus osteotomy. J Bone Joint Surg Am. 1988;70:102-109.
8 Hsu R.W., Himeno S., Coventry M.B., Chao E.Y. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215-227.
9 Kapandji A. The Physiology of the Joints. II. The Lower Extremity. Philadelphia: Churchill Livingstone, 1988;68.
10 McDermott A.G., Finklestein J.A., Farine I., et al. Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am. 1988;70:110-116.
11 Morrey B.F., Edgerton B.C. Distal femoral osteotomy for lateral gonarthrosis. Instr Course Lect. 1992;41:77-85.
12 Nelson C.L., Saleh K.J., Kassim R.A., et al. Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg Am. 2003;85:1062-1065.
13 Phillips M.J., Krackow K.A. High tibial osteotomy and distal femoral osteotomy for valgus or varus deformity around the knee. Instr Course Lect. 1998;47:429-436.
14 Wang J.W., Hsu C.C. Distal femoral varus osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am. 2005;87:127-133.