8 Uveitis
Pathophysiology
Inflammatory reaction
Anterior uveitis
Inflammation of iris (iritis) and ciliary body (cyclitis)
Most common cause of anterior uveitis in adults is idiopathic (followed by HLA-B27 associated)
Most common cause of acute, noninfectious, hypopyon iritis is HLA-B27-associated iritis
Etiology
Classification
Findings
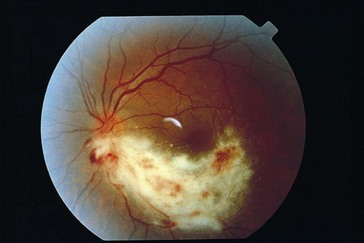
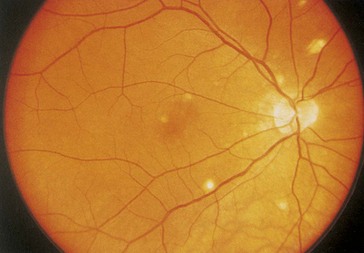
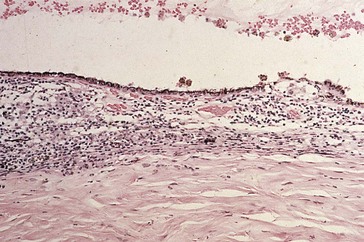
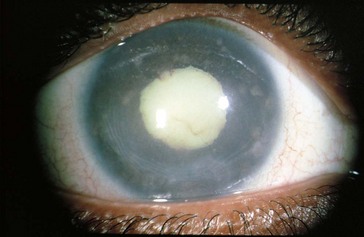
conjunctival and episcleral injection, ciliary injection (circumcorneal flush from branches of anterior ciliary arteries), miosis (iris sphincter spasm), AC reaction; may have hypopyon, keratic precipitates, iris nodules, dilated iris vessels (occasionally, rubeosis), synechiae (posterior [iris adhesions to lens; seclusio pupillae is a complete adhesion that can result in iris bombe] or anterior [iris adhesions to cornea and angle]) (Figure 8-1)

Figure 8-1 Severe idiopathic anterior uveitis with fibrinoid reaction.
(From Hooper PL: Idiopathic and other anterior uveitis. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
Diagnosis
Reiter’s Syndrome
Triad of conjunctivitis, urethritis, and arthritis
Associated with infections: Chlamydia, Ureaplasma urealyticum, Yersinia, Shigella, Salmonella
Inflammatory Bowel Disease (IBD)
Uveitis occurs in ulcerative colitis (10%) and Crohn’s disease (3%)
Fuchs’ Heterochromic Iridocyclitis
Occurs in young adults; unilateral
Associated with chorioretinal scars (toxo)
Findings
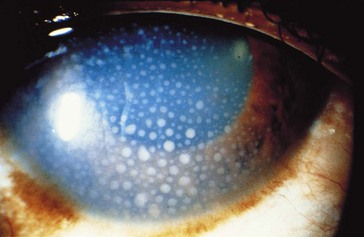
diffuse small white stellate KP, minimal AC reaction, no posterior synechiae, iris heterochromia (diffuse atrophy of stroma, loss of iris crypts; involved iris is paler; 15% bilateral), fine-angle vessels (may bleed during gonioscopy, cataract surgery, or paracentesis) (Figure 8-4)
Lyme Disease
Due to Borrelia burgdorferi (spirochete)
Ocular involvement is usually bilateral
Affected organ systems: skin, CNS, cardiovascular, musculoskeletal
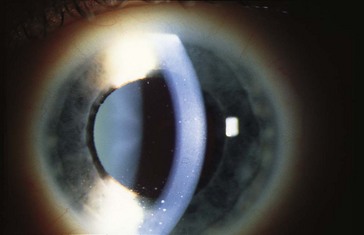
Posner-Schlossman Syndrome (Glaucomatocyclitic Crisis)
Recurrent anterior uveitis and increased IOP; episodes are typically self-limited
Intermediate uveitis
Pars Planitis
Most common cause of intermediate uveitis (85–90%)
Usually young adults; females > males; 75% bilateral
Accounts for 25% of uveitis in children
Associated with HLA-DR15 and MS
Findings
light flare with a few KP, anterior vitritis, snowballs (white vitreous cellular aggregates near ora serrata; may coalesce to form peripheral fibrovascular accumulation [snowbank] over inferior pars plana and vitreous base), peripheral retinal periphlebitis, hyperemic disc, no chorioretinitis, no synechiae (Figure 8-5)
Posterior uveitis
Most common cause of posterior uveitis in adults is toxoplasmosis (followed by retinal vasculitis)
Infections
Cytomegalovirus (CMV)
Progressive hemorrhagic necrotizing retinitis involving all retinal layers
Occurs in 15–46% of AIDS patients; usually when CD4 count <50 cells/mm3
Rare syndrome of neonatal cytomegalic inclusion disease
Findings
well-circumscribed necrotizing retinitis (2 appearances), mild AC and vitreous reaction
Treatment
antiviral therapy (induction during first 2 weeks)
Acute Retinal Necrosis (ARN)
Usually occurs in immunocompetent individuals; 33% bilateral (BARN), commonly in immunosuppressed
Association with HLA-DQw7 (50%)
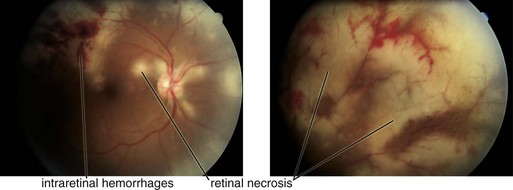
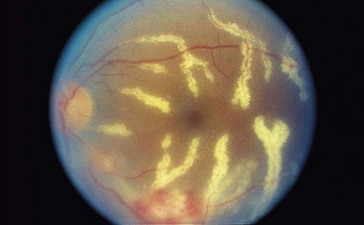
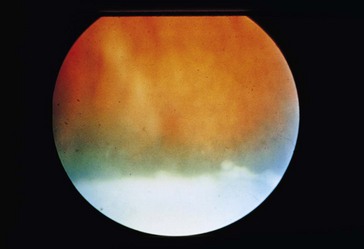
Findings
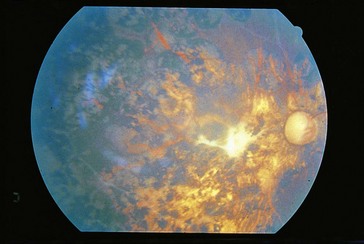
diffuse episcleral injection, mild iritis with granulomatous KP, vitritis; ‘thumbprint’ nummular infiltrates posterior to equator with isolated peripheral patches of necrotizing retinitis that becomes confluent; sawtooth demarcation line between necrotic and healthy retina, generalized obliterative retinal arteritis (with peripheral vaso-occlusion), pale disc edema (Figure 8-7); within 2 months, retinitis gradually resolves and necrotic retina sloughs; coarse salt and pepper pigmentation
Progressive Outer Retinal Necrosis (PORN)
Variant of ARN in AIDS but painless with minimal intraocular inflammation
Often have history of cutaneous zoster
74% unilateral at presentation, 70% become bilateral
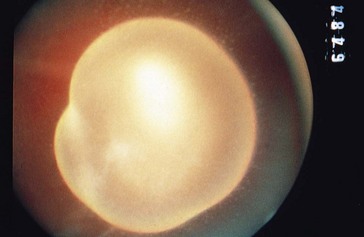
Findings: multiple discrete peripheral or central areas of retinal opacification/infiltrates (deep with very rapid progression), ‘cracked mud’ appearance after resolution; vasculitis is not prominent (Figure 8-8)
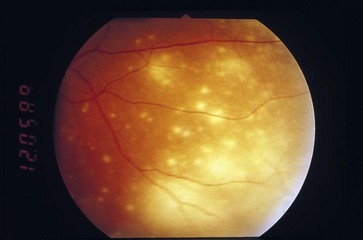
Figure 8-8 Progressive outer retinal necrosis, early stage.
(From Hudson HL, Boyer DS, Martin DF, et al: Viral posterior uveitis. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
Treatment: combination of foscarnet and ganciclovir; poor response to antivirals
Herpes Zoster
Uveitis typically develops during convalescence from acute Varicella infection
Reactivated uveitis (anterior and/or posterior), may have keratitis (epithelial or stromal)
May require chronic topical steroid treatment to prevent recurrence
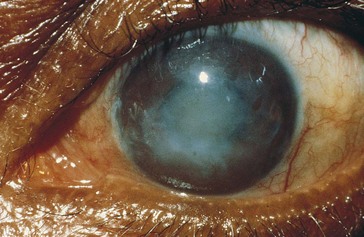
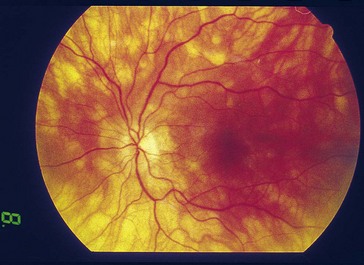
Rubella
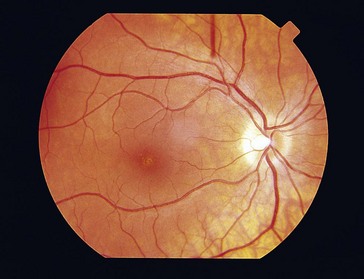
Sensorineural hearing loss, salt and pepper retinopathy; may develop cataract or glaucoma (rare to have both) (Figure 8-9)

Figure 8-9 Rubella retinopathy.
(Courtesy of George S. Novalis, MD. From Hudson HL, Boyer DS, Martin DF, et al: Viral posterior uveitis. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
Measles
Pigmentary retinopathy due to infection acquired in utero
Candidiasis
Yeast-like form (blastoconidia), or pseudohyphae or elongated branching structures (pseudomycelia)
Occurs in debilitated patients on hyperalimentation and in IV drug abusers
Most cases occur without positive blood cultures or ongoing fungemia
Pneumocystis Choroiditis
Choroiditis with multifocal orange nummular lesions; lesions contain cysts of Pneumocystis carinii (Figure 8-10)
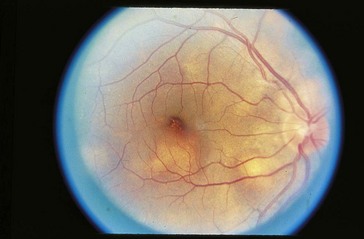
Figure 8-10 Multiple choroidal lesions in Pneumocystis choroiditis.
(From Cowan CL: Sarcoidosis. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
Associated with use of inhaled pentamidine (which is prophylaxis for pulmonary Pneumocystis only)
Leprosy
Onchocerciasis (River Blindness)
Second leading cause of corneal blindness in world (trachoma is first)
Findings
intraocular microfilariae (in AC), anterior uveitis, SPK, sclerosing keratitis, scleritis, chorioretinitis, optic neuritis and atrophy; may develop cataract, PAS, and glaucoma (Figure 8-12)
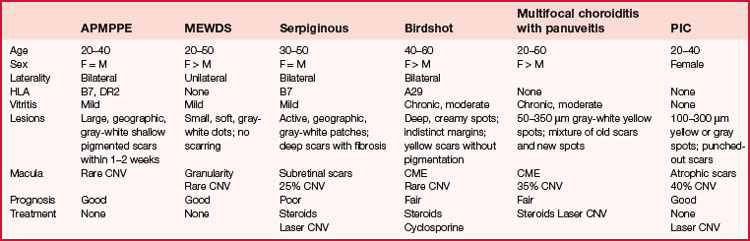
Inflammations ( Table 8-1)
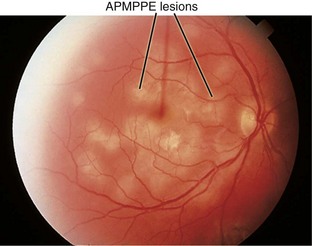
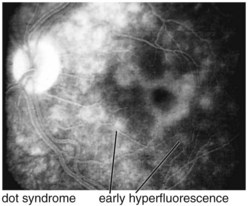
Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE)
Occurs in young, healthy adults; female = male; usually bilateral
Acute, self-limited; may be nonspecific choroidal hypersensitivity reaction
Associated with cerebral vasculitis
Flu-like prodrome (33%) followed by decreased vision
Findings
multiple creamy yellow-white plaque-like lesions (usually <1 DD) at level of RPE or choriocapillaris (possibly due to choroidal hypoperfusion); lesions fade over 2–6 weeks, leaving geographically shaped RPE changes (hypopigmentation and hyperpigmentation); may have vitreous cells, mild AC reaction; rarely vascular sheathing, disc edema, CNV (Figures 8-13)
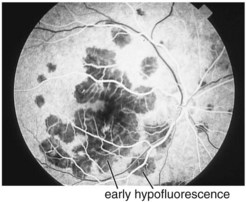
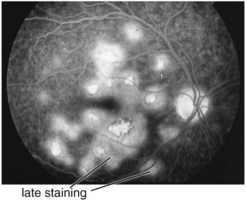
FA
initial blockage with late hyperfluorescence; window defects in old cases (Figures 8-14, 8-15)
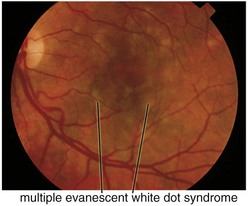
Multiple Evanescent White Dot Syndrome (MEWDS)
Onset between age 14 and 50; female > male; unilateral > bilateral
Findings
granular retinal appearance with small (100–200 µm) white spots in posterior pole at level of RPE; may have vitreous cells, positive RAPD, mild optic disc swelling (Figure 8-16)
Serpiginous Choroidopathy
Chronic, recurrent, indolent disease of unknown etiology
Onset between age 40–60; female = male; usually bilateral
Affects inner chorioretinal pigment epithelium
Findings
geographic (map-like) pattern of scars with active edges (yellow-gray, edematous), usually beginning in posterior pole (often extending from disc); active areas become atrophic over weeks to months; new lesions occur contiguously or elsewhere (often in snake-like pattern); may have mild AC reaction, vitritis, vascular sheathing, RPE detachment, NVD, CNV (rare) (Figure 8-18)
Birdshot Choroidopathy (Vitiliginous Chorioretinitis)
Occurs after 4th decade of life; female > male; usually bilateral
Multifocal Choroiditis with Panuveitis
Onset between age 20–50; female > male
Findings
multiple gray-white to yellow lesions (50–350 µm) at level of choroid or RPE; vitreous and AC cells; chronic lesions become atrophic with punched-out margins, variable amounts of pigmentation, and occasionally fibrosis (Figure 8-20)
Punctate Inner Choroidopathy (PIC)
Onset between age 20 and 40; healthy, moderately myopic women
Acute Retinal Pigment Epitheliitis (Krill’s Disease)
Rare, occurs in young adults; usually unilateral
Findings
clusters of hyperpigmented spots (300–400 µm) in macula surrounded by yellow-white halos; with resolution, the spots lighten or darken, but halos remain; no vitritis (Figure 8-22)
Frosted Branch Angiitis
Endophthalmitis
Inflammation involving 1 or more coats of the eye and adjacent ocular cavities
Classification
Treatment
rule out infection (AC and vitreous taps)
Panuveitis
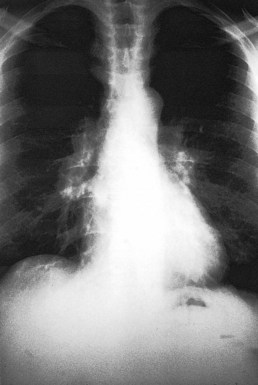
Sarcoidosis
Multisystem granulomatous disease characterized by noncaseating granulomas; unknown etiology
Females > males; more common among African Americans (10 : 1)
25–50% have systemic sarcoidosis
Ocular disease: 30% unilateral, 70% bilateral; 40% acute, 60% chronic
Other findings
pulmonary (50%), constitutional (40%; malaise, fever, weight loss), skin (15%), lymphadenopathy (20%) (Box 8-1)
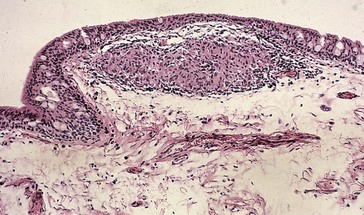
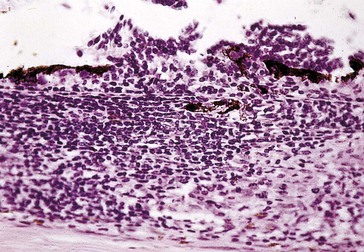
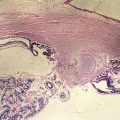
Pathology
noncaseating granulomas (caseating granulomas occur in TB) with Langhans’ multinucleated giant cells (Figure 8-24)
Diagnosis
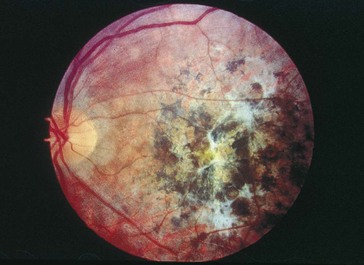
Behçet’s Disease
Triad of oral ulcers, genital ulcers, and inflammatory eye disease
Findings (75%)
recurrent, explosive inflammatory episodes with active episodes lasting 2–4 weeks
Uveitis (posterior more common than anterior); can present with nongranulomatous anterior uveitis (usually bilateral; may have transient hypopyon); occasionally, conjunctivitis, episcleritis, or keratitis can occur; posterior involvement with recurrent vascular occlusions, retinal hemorrhages, exudates, CME, vitritis, traction RD, ischemic optic neuropathy; may develop glaucoma and cataract (Figure 8-26)
Diagnosis
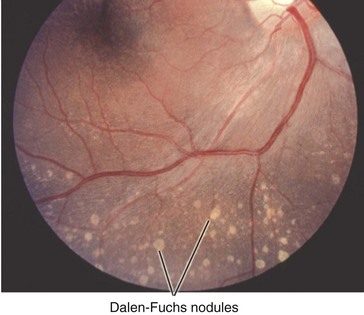
Vogt-Koyanagi-Harada Syndrome (VKH)
Symptoms
decreased vision, pain, redness, photophobia, stiff neck, headache, deafness, tinnitus, vertigo
Clinical course
Pathology
inflammation of choriocapillaris and retina; Dalen-Fuchs nodules (epithelioid cells between Bruch’s membrane and RPE) (Figure 8-27)
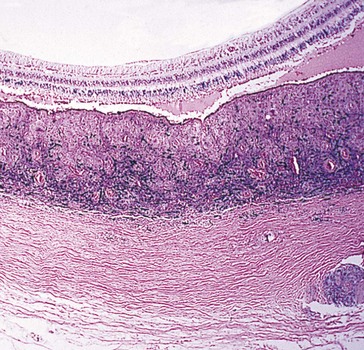
Sympathetic Ophthalmia
Bilateral granulomatous panuveitis following penetrating eye trauma
Incidence: 0.1–0.3% of penetrating injuries; 0.015% of intraocular surgery
Findings
Koeppe nodules, mutton fat KP, retinal edema, Dalen-Fuchs nodules; may have disc edema (Figure 8-28)
Pathology
diffuse lymphocytic infiltration of choroid with ill-defined patchy accumulations of epithelioid (giant) cells that contain phagocytosed uveal pigment; inflammation can extend into optic nerve, causing granulomatous optic neuritis; Dalen-Fuchs nodules (epithelioid giant cells between Bruch’s membrane and RPE that appear as small, round, yellow depigmented spots in peripheral retina [also seen in VKH, sarcoidosis, TB]); no involvement of choriocapillaris (Figure 8-29, 8-30)
Syphilis
Panuveitis (‘great mimic’) due to infection with spirochete Treponema pallidum
Acquired
Masquerade syndromes
Leukemia
Retina is most common ocular tissue affected clinically
Choroid is most common ocular tissue affected histopathologically
Primary Intraocular Lymphoma (Reticulum Cell Sarcoma)
Differential diagnosis of uveitis and associated signs
Surgery and uveitis
Usually wait at least 3 months for cataract surgery, 6 months for corneal transplant
Review Questions (Answers start on page 366)
American Academy of Ophthalmology. Intraocular Inflammation and Uveitis, vol 9. San Francisco: AAO; 2012.
Foster CS, Vitale AT. Diagnosis and Treatment of Uveitis. Philadelphia: WB Saunders; 2002.
Jones NP. Uveitis: An Illustrated Manual. Philadelphia: Butterworth-Heinemann; 1998.
Michelson JB. Color Atlas of Uveitis, 2nd edn. St Louis: Mosby; 1992.
Nussenblatt RB, Whitcup SM. Uveitis: Fundamentals and Clinical Practice, 4th edn. Philadelphia: Mosby; 2010.
Tabbara KF, Nussenblatt RB. Posterior Uveitis Diagnosis and Management. Philadelphia: Butterworth-Heinemann; 1994.

 with exacerbations)
with exacerbations)