CHAPTER 18 Use of the T-Pin in the Treatment of Extra-articular Distal Radius Fractures
Distal radius fractures are among the most common fractures treated by orthopaedic surgeons. Numerous techniques and implants have been devised to stabilize these fractures. The T-Pin (Union Surgical, LLC, Philadelphia, PA) is a novel instrument designed to stabilize extra-articular distal radius fractures utilizing minimal surgical dissection. The T-Pin allows for early active wrist range of motion, thus promoting earlier return to functional activities. Here we discuss the instrumentation, the techniques of insertion and extraction, and the postoperative care required for the use of the T-Pin in the treatment of extra-articular distal radius fractures.
Historical Perspective
Fractures of the distal radius are one of the most common fractures treated by orthopaedic surgeons. Owen stated that distal radius fractures represent one in six fractures in patients older than 50 years of age.1 Various procedures and fixation techniques have evolved to treat this common fracture based on many factors, which include the patient’s age, bone quality, and ability to tolerate the procedure and the type of fracture. Treatment modalities have included immobilization as originally described by Colles,2 pins in plaster, external fixation, percutaneous pinning with casting, and open reduction with internal fixation with a number of different implants.
Since Abraham Colles described the comminuted and displaced distal radius fracture in 1814, orthopaedic surgeons have sought to stabilize the fracture after reduction.3 Many fractures treated in plaster have a tendency to redisplace.4 For this reason, percutaneous pinning evolved as a relatively simple fixation method for extra-articular fractures prone to redisplacement with cast treatment alone. Various methods of pinning have been developed. The described techniques include two pins placed through the radial styloid5; two crossed pins, one inserted at the radial styloid just dorsal to the first extensor compartment and the second inserted on the dorsal ulnar aspect of the distal radius between the fourth and fifth extensor compartments3,6; three to four intrafocal pins within the fracture site7; transulnar oblique pinning in which a threaded wire is inserted in the distal ulna and passed obliquely through the distal ulna to the distal radius so that it engages the radial styloid fragment8; one radial styloid pin and a second across the distal radioulnar joint9; and multiple transulnar to radius pins, including the distal radioulnar joint.10 Despite improved maintenance of reduction with pinning, many of these series report 25% to 33% of patients having a significant loss of reduction.
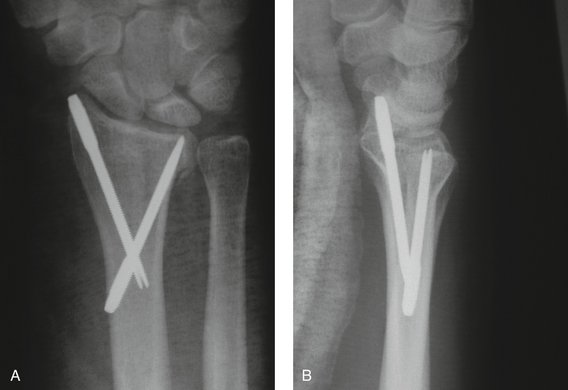
The T-Pin is a threaded pin designed specifically to treat acute distal radius fractures. The T-Pin technique has the advantages of (1) a short operative time, (2) being relatively inexpensive, (3) having utility for patients with medical conditions for whom general anesthesia poses a greater risk, and (4) allowing early active wrist motion. The T-Pin is threaded and affords better purchase of the fracture fragments than commonly used smooth pins (Fig. 18-1). Currently, we are undergoing a prospective multicenter study to further evaluate the efficacy of the procedure.
Indications and Contraindications
The main indication for use of the T-Pin is an unstable extra-articular dorsally displaced distal radius fracture (Fig. 18-2). This technique is useful for active patients because it is a relatively brief procedure and allows for a quick return of function. The brief nature of the procedure, especially the limited incisions (1 to 2 cm) required to insert the pins, makes this procedure useful in the elderly and medically unstable populations because it can be performed under local anesthesia with intravenous sedation.
Surgical Technique
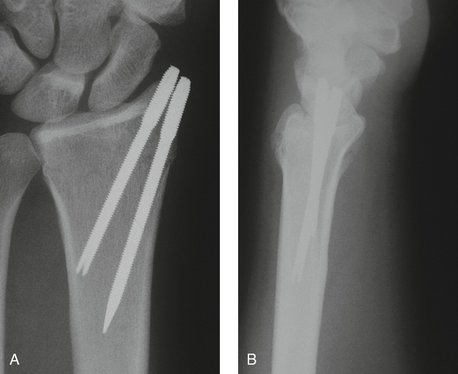
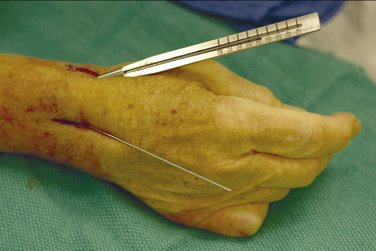
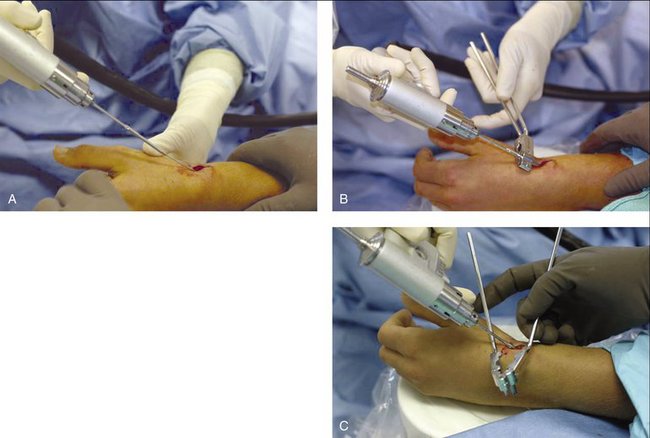
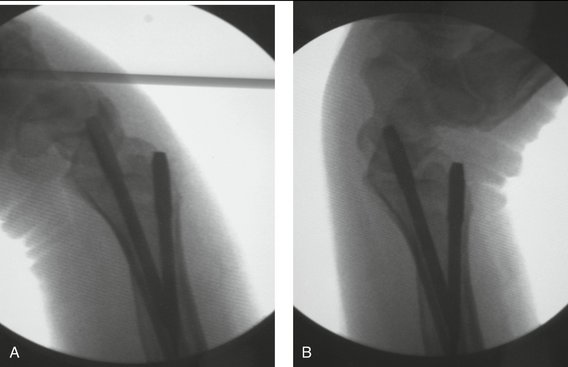
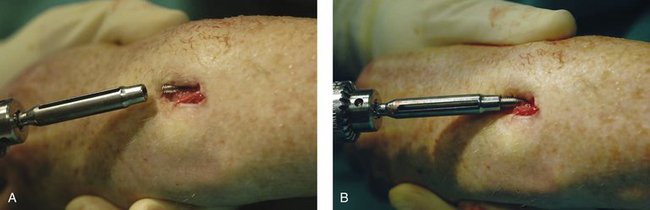
Under fluoroscopic guidance, closed reduction of the fracture is performed. A 0.620-inch Kirschner wire (K-wire) can be placed percutaneously into the distal fragment to use as a joystick to regain the normal anatomical volar tilt. Typically two 1- to 2-cm longitudinal incisions are made (1) at the distal aspect of the radial styloid between the first and second dorsal extensor compartment, dorsal to the abductor pollicis longus/extensor pollicis brevis tendons and (2) proximal to the fracture site on the radius (Fig. 18-3). Alternatively, for the younger patient with good bone stock, two pins can be placed at the radial styloid alone through a single incision (Fig. 18-4). The soft tissues are bluntly dissected to bone for safe placement of guidewires. Dissection is carried down to visualize the pin insertion site, and adjacent extensor tendons are protected by retraction or by use of the tissue protection guide provided on the tray. The fracture is initially stabilized with smooth 1-mm guidewires at the aforementioned insertion sites, and placement is adjusted under fluoroscopic guidance. A technical point to note is that the guidewire will deflect off the inner cortices and bend, whereas the more rigid T-Pin will not; therefore, guidewire insertion should stop when cortical contact is made (Fig. 18-5). A measuring guide is then applied along each guidewire indicating the length of the T-Pin required (Fig. 18-6). The pin tray supplies pin lengths from 40 to 70 mm in 5-mm increments. To avoid having the guide pin kink and bend near the tip, we back out the guide pin 10 mm after measuring its depth.

FIGURE 18-5 Fluoroscopic view of guidewires making cortical contact, with the radial styloid pin bowing slightly.
The cannulated T-Pin is secured onto the power driver and inserted over the guidewire (Fig. 18-7). The T-Pin is driven along the guidewire until the trailing threads are nearly flush with the bone. The split tissue protector opens to allow removal for final seating of the pin without having to disengage the driver. The surgeon disengages the power driver and removes the guidewire, leaving only the T-Pin in place. The break-off driving mechanism of the pin is easily removed by bending the smooth shaft by hand.
Stability of the fixation is checked under fluoroscopy (Fig. 18-8). The tourniquet is deflated and the skin closed with nylon sutures. The postoperative dressing includes sterile gauze and a volar splint.
Rehabilitation
The postoperative dressing is a plaster volar short arm splint that allows for unrestricted finger range of motion. The patient is given the usual instructions of elevation of the extremity, use of ice, and splint care and told to return for a follow-up visit on postoperative day 1 to 3. At this first postoperative visit the patient is fitted with a custom-molded, forearm-based static wrist splint, which can be removed for bathing and exercises. Therapy is initiated under the guidance of a hand therapist for active and passive digital range of motion, edema control, and gentle wrist active range of motion (Fig. 18-9). For severely osteoporotic bone, wrist range of motion is deferred until 2 to 3 weeks postoperatively. By initiating wrist range of motion on or before the third postoperative day, we believe it is possible to restore a greater degree of motion and quicker restoration of function compared with results achieved from delayed initiation of range of motion.
After 6 weeks, a decision is made whether to remove the pins. Our current practice is to remove the pins in active adults younger than 60 years of age. We tend to leave the pins in place in those patients with a sedentary lifestyle or those older than 60 years of age. Pins are removed with a removal tool designed to fit the flutes in the distal threads of the T-Pin, which is included in the pinning tray (Fig. 18-10). A 4.0-mm hollow mill is useful for cleaning scar tissue or bone from the distal threads of the T-Pin to allow easy placement of the removal tool. Once full fracture healing has occurred after the pin has been removed, as assessed by no tenderness from palpation at the fracture site, an unrestricted program of range of motion and strengthening can begin. The protective splint is discontinued at this time.
1. Owen RA, Melton LJ3rd, Johnson KA, et al. Incidence of Colles’ fracture in a North American community. Am J Public Health. 1982;72:605-607.
2. Colles A. On the fracture of the carpal extremity of the radius. Edinb Med Surg J. 1814;10:182.
3. Stein H, Katz S. Stabilization of comminuted fractures of the distal inch of the radius: percutaneous pinning. Clin Orthop Relat Res. 1975;108:174-181.
4. Fernandez D, Palmer AK. Fractures of the distal radius. In: Green D, Hotchkiss R, Pederson W, editors. Green’s Operative Hand Surgery. New York: Churchill Livingstone, 1999.
5. Lenoble E, Dumontier C, Goutallier D, et al. Fracture of the distal radius: a prospective comparison between trans-styloid and Kapandji fixations. J Bone Joint Surg Am. 1995;77:562-567.
6. Clancey G. Percutaneous Kirschner-wire fixation of Colles fractures. J Bone Joint Surg Am. 1984;66:1008-1014.
7. Kapandij A. Treatment of non-articular distal radius fractures by intrafocal pinning with pins. In: Saffer P, Cooney WP, editors. Fractures of the Distal Radius. Philadelphia: Lippincott Williams & Wilkins, 1995.
8. DePalma A. Comminuted fractures of the distal end of the radius treated by ulnar pinning. J Bone Joint Surg Am. 1952;34:651-662.
9. Mortier JP, Kuhlmann JN, Richet C, Baux S. Horizontal cubito-radial pinning in fractures of the distal radius including a postero-internal fragment. Rev Chir Orthop Reparatrice Appar Mot. 1986;72:567-572.
10. Rayhack JM, Langworthy JN, Belsole RJ. Transulnar percutaneous pinning of displaced distal radial fractures: a preliminary report. J Orthop Trauma. 1989;3:107-114.