Ultrasound in animals
Overview
In 2004, in the first historical translational study of focused assessment with sonography for trauma (FAST) from humans to small animals, 101 dogs with severe blunt trauma after being hit by cars were evaluated.1 The authors reported that intraabdominal injury, specifically, hemoperitoneum, was more common than previously identified (pre-FAST rate of 12% to 23% versus a post-FAST rate of 45%).2 By imaging the thorax via the subxiphoid site, intrathoracic injury was detected, as well as pleural and pericardial effusions; moreover, proficiency by nonradiologists was documented.1 Since 2004, the abdominal FAST examination (AFAST) has been modified by naming sites based on target organs rather than external sites and by developing an abdominal fluid score (AFS) as a semiquantitative measure of the volume of effusions. In hemoperitoneum, the AFS was found to predict the anticipated degree of anemia and the need for blood transfusion and emergency laparotomy in dogs.3 Accordingly, a thoracic FAST examination (TFAST) and a lung survey (Vet BLUE Lung Scan) have been developed. These thoracic and lung ultrasound techniques appeared to be effective in the evaluation of blunt and penetrating trauma inasmuch as nonradiologist veterinarians were able to diagnose thoracic trauma (median time, <3 minutes), including pneumothorax, hemothorax, thoracic wall trauma, pulmonary contusions, and cardiac trauma, and discrimination among various causes of respiratory distress in nontrauma cases was facilitated as well.2,4
Abdominal focused assessment with sonography for trauma and abdominal fluid score
The initial veterinary FAST scan has been refined, including naming the original four sites by target organ and incorporating a fluid scoring system for initial and serial examinations (Figure 55-1)3. By emphasizing the target organ approach, veterinarians could appreciate the animal’s internal anatomy and enrich their ultrasound skills. Development of the AFS enabled progressive assessment of animals’ hemodynamic status (e.g., occult hemorrhage [negative AFS turned positive], continued hemorrhage [increasing AFS], resolving hemorrhage [decreasing AFS]).2,3
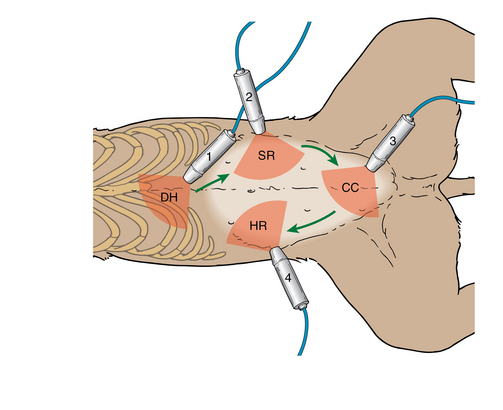
Figure 55-1 Abdominal focused assessment with sonography for trauma examination. Key: DH, diaphragmatico-hepatic view; SR, spleno-renal view; CC, cysto-colic view;HR, hepato-renal view. (Used with permission from Lisciandro GR, Lagutchik MS, Mann KA, et al: Evaluation of an abdominal fluid scoring system determined using abdominal focused assessment with sonography for trauma in 101 dogs with motor vehicle trauma, J Vet Emerg Crit Care 19[5]:426-437, 2009.)
The semiquantitative AFS (AFS 0, negative at all sites; AFS 1 to 4, score of 1 with a maximum of 4 for each positive site) correlated with the degree of anemia when dogs were placed in lateral recumbency (unequal gravity-dependent sites, in contrast to human hemorrhage scoring systems in the supine position, in which all sites are equally gravity-dependent), and such positioning served as an inherent depth gauge (Figure 55-2).3
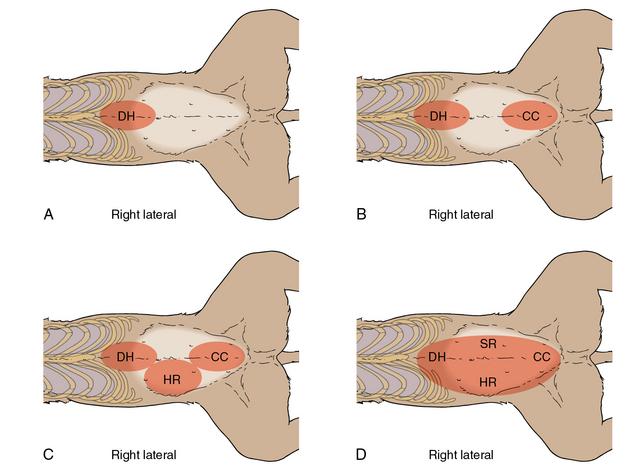
Figure 55-2 Abdominal focused assessment with sonography for trauma–applied abdominal fluid scoring system. DH, diaphragmatico-hepatic view; SR, spleno-renal view; CC, cysto-colic view; HR, hepato-renal view. (Used with permission from Lisciandro GR, Lagutchik MS, Mann KA, et al: Evaluation of an abdominal fluid scoring system determined using abdominal focused assessment with sonography for trauma in 101 dogs with motor vehicle trauma, J Vet Emerg Crit Care 19[5]:426-437, 2009.)
In previously healthy dogs, anemia uncommonly developed in lower-scoring dogs (AFS 1, 2 = small bleeders), as opposed to higher-scoring dogs (AFS 3, 4 = big bleeders), which as expected became anemic. Big bleeders predictably incurred a minimal decrease of 20% from their baseline packed cell volume (PCV), and approximately 20% became severely anemic (PCV <25%).3 AFS evaluations facilitated clinical management by anticipating the need for transfusion products or emergency laparotomy.3 Small bleeders that result in anemia should alert the clinician to look for other sites of hemorrhage such as the thorax (hemothorax), retroperitoneal space, or fracture sites.2,3 Serial AFS assessments enable monitoring of the evolution of anemia. However, the AFS has not proved to be effective in cats hit by cars (lack of case numbers, big bleeders, or both) because most bleeding cats, intolerant of blood loss, probably expire before reaching a veterinarian.5,6
The AFS is also used for nontraumatic causes of hemoperitoneum. The latter are usually caused by bleeding tumors and warfarin-based rodenticide toxicosis. Postoperative (e.g., ovariohysterectomy, splenectomy, liver lobectomy) and postinterventional (e.g., percutaneous biopsy, laparoscopy) cases at risk for hemorrhage could be monitored with the AFS since the latter could guide decisions on blood transfusion and definitive care (e.g., interventional radiology, exploratory laparotomy).2
In the AFAST study,3 all dogs exhibited normal PCV and were evaluated with AFAST soon after their trauma (median time, 60 minutes from trauma to AFAST) and following admission (median time from initial evaluation to AFAST, <5 minutes). Prompt AFAST examination aids in modifying resuscitative efforts accordingly and can guide management toward more conservative therapeutic end points and thus lower transfusion rates.2,3 Initial and serial AFAST and AFS should be integrated into veterinary trauma algorithms because of their potential to affect the clinical course as shown in human medicine.7,8 Past studies comparing abdominal radiographic (AXR) findings with AFAST-positive and AFAST-negative dogs reported that 24% of dogs with decreased AXR serosal detail (suggesting the presence of free abdominal fluid) were in fact AFS negative whereas 34% of dogs with normal AXR serosal detail (suggesting the absence of free abdominal fluid) were AFS positive. Hence, AXR findings are rather unreliable in comparison to AFAST, which is in accordance with human studies.3,9
The use of AFAST for penetrating trauma such as bite wounds was hypothesized to be helpful. However, it was found that AFAST performed in many of the 145 dogs in the TFAST study often missed serious intraabdominal injury. This discrepancy probably resulted from the nature of each type of trauma (e.g., blunt versus penetrating) since blood is rapidly “defibrinated” in blunt trauma and appears anechoic and conspicuously as free fluid. In penetrating trauma there is a different initiation event in the coagulation cascade because the crushed and torn tissue results in clotted blood, and thus AFAST misses isoechoic (shades of gray) areas (similar to soft tissue). No extensive data on the role of AFAST for penetrating trauma2,3 are available. Its ability to detect injury probably has low sensitivity but high specificity in such cases.10,11
The thoracic focused assessment with sonography for trauma examination
In veterinary medicine, a four-point thoracic scan (TFAST) has been introduced for the rapid detection of pneumothorax (PTX) and other thoracic injuries such as lung blast, hemothorax, pericardial effusion, diaphragmatic herniation, and thoracic wall trauma. The original TFAST has evolved into a 5-point scan through addition of the diaphragmatico-hepatic (DH) view (also part of the AFAST examination).2,3 In Figure 55-3 TFAST is depicted in lateral recumbency for ease of illustration, but is performed in sternal recumbency or standing in respiratorily compromised or distressed animals. Dorsal recumbency should never be used because it is dangerous to compromised animals. The chest tube site (CTS) refers to a stationary, horizontally held transducer (parallel to the spine) at the highest lateral point (lateral recumbency) and highest dorsal point ventral to the hypaxial muscles (sternal recumbency) of the thorax that is used to evaluate for PTX. The pericardial site (PCS) and DH views are dynamic, with cardiac transverse-axis (transducer marker toward the elbow) and longitudinal-axis (transducer marker toward the spine) views and broad fanning through the liver into the thorax, respectively. The sage axiom “one view is no view” should be used to help distinguish pleural from pericardial effusions; moreover, by zooming away from the area of interest (increasing depth), misinterpretation of effusions for normal heart chambers is less likely.2
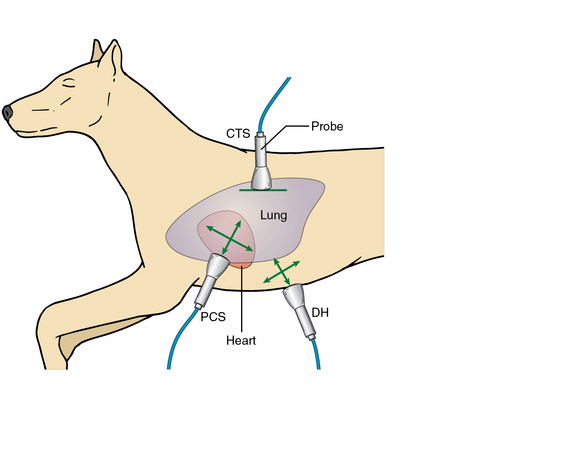
Figure 55-3 Thoracic focused assessment with sonography for trauma examination. (Used with permission from Lisciandro GR: Abdominal and thoracic focused assessment with sonography for trauma, triage, and monitoring in small animals, J Vet Emerg Crit Care 12[2]:104-122, 2011.)
The basic ultrasound findings on bilaterally applied CTS views include “dry” lungs (A-lines with a glide), PTX (A-lines with no glide and a lung point with partial PTX and absence of a lung point with massive PTX), “wet” lungs (ultrasound lung rockets or B-lines), and the step sign (deviations from the normal expected continuity of the glide sign along the pulmonary-pleural line).2,3 The Vet BLUE Lung Scan corresponds to a regionally applied lung ultrasound evaluation extending beyond the CTS. The “wet” versus “dry” lung concept is easily appreciated. “Dry” lungs are depicted as an A-line pattern (equidistant parallel lines called A-lines, which represent reverberation artifacts) with a glide sign (without a glide sign, PTX is present). “Wet” lungs are characterized by lung rockets (B-lines), which are defined as hyperechoic lines that do not fade, extend from the pleural line through the far field and obliterate the A-lines, and swing to and fro with inspiration and expiration.12 “Wet” lungs may reflect several forms of interstitial edema (e.g., cardiogenic pulmonary edema, noncardiogenic pulmonary edema [NCPE]; and pulmonary contusions in trauma).12,13 B-lines are infrequent in nonrespiratory dogs and cats.14 Notably, parenchymal abnormalities located in the central lung areas may be missed by sonography.14 In cases of suspected PTX, operators search for the lung point to determine the degree of PTX (partial vs. massive, Figure 55-4). The lung point refers to the location at which the lung recontacts the thoracic wall as evidenced by either resumption of the glide sign or the finding of B-lines.2,16
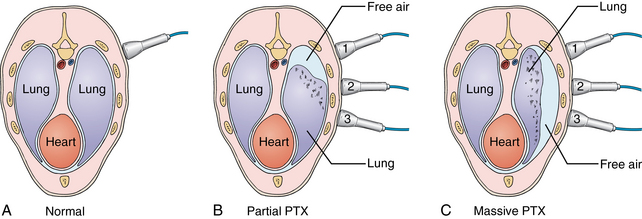
Figure 55-4 Search for the lung point. (Used with permission from Lisciandro GR: Abdominal and thoracic focused assessment with sonography for trauma, triage, and monitoring in small animals, J Vet Emerg Crit Care 12[2]:104-122, 2011.)
Ultrasound was suggested to be superior to physical examination and radiography in detecting pleural and pericardial fluid.11 PCS views are gravity-dependent and used for detecting either type of effusion. The DH view is useful because of the acoustic window that it provides for direct visualization into the pleural and pericardial spaces. The latter is considered a most sensitive view in human protocols.11 Multiple and repeated views improve the probability of accurate assessment and decrease the probability of pitfalls.
Vet blue lung scan
The Vet BLUE Lung Scan, referred to as Vet BLUE, is performed with the same technique as previously described for TFAST (CTS views). In addition, the transducer is moved as follows: from the CTS or caudodorsal lung region to the perihilar, middle lung, and finally the cranial lung lobe regions. Operators search for “wet” versus “dry” lungs, for the shred and tissue signs (lung consolidation), and for the nodule sign (neoplastic or granulomatous processes).12,17,18
Patient instability or lack of immediate technical support delays radiographic imaging, the historical diagnostic mainstay for veterinarians. Clinical decisions were based on insensitive information.19 However, the availability of computed tomography, which is considered the “gold standard” for many lung conditions, is gradually changing practices. Ultrasound is a reliable alternative bedside imaging modality. By applying the simple principles of “wet” lung (e.g., cardiogenic pulmonary edema, NCPE, pneumonia, lung contusions) versus “dry” lung (e.g., upper airway disease, pulmonary thromboembolism, asthma, severe acidosis, fever), combined with other findings such as nodules and consolidated lung (e.g., neoplasia, pneumonia), the probability of an accurate diagnosis exceeds traditional means. From a monitoring standpoint, interstitial edema, which precedes alveolar edema, is easily recognized by ultrasound well before physical examination and radiography can detect it. Many acute conditions have classic distribution patterns of “wet” versus “dry” lung. Dogs with left-sided heart failure (other than Doberman pinschers) would have B-lines at the caudodorsal and perihilar lung regions and “dry” lungs ventrally at the middle and cranial lung lobe regions (as would dogs with volume overload). The same pattern may be observed with acute NCPE from neurogenic causes (a dog that has seizures), electrocution (a dog that bites an electric cord), choking, or other causes (e.g., drowning, acute respiratory distress syndrome [ARDS]). Conversely, ventral patterns would be more suggestive of pneumonia (especially in dogs that have acutely aspirated). The Vet BLUE becomes even more valuable in sorting out the cause of respiratory distress in a choking dog, which could be due to NCPE, aspiration pneumonia, a combination of both or neither. If this dog has B-lines only at the right middle lung lobe region, the major cause of its respiratory distress is more likely to be acute aspiration than NCPE. Another major conundrum with respiratory distress in dogs and cats (the latter commonly have asthmatic crises) is determining the cause of their distress. “Dry” lungs in all fields would rapidly rule out left-sided cardiac failure. In veterinary medicine, ultrasound may be used for cardiac assessment during resuscitation and for monitoring fluid therapy (subjectively) by looking at the left ventricular transverse-axis (volume and contractility),20 whereas the caudodorsal and perihilar lung regions are scanned to detect “wet” versus “dry” lungs (left-sided cardiac status); moreover, scanning may be extended caudally for vena cava analysis and evaluation of hepatic vein distention (right-sided cardiac status).2,21
By combining AFAST, TFAST, and the Vet BLUE, veterinarians can arrive at a solid working diagnosis expediently by surveillance of four spaces (peritoneal, retroperitoneal, pleural, and pericardial) and the lung.2,14 Point-of-care ultrasound aids veterinarians in positively directing therapy with evidence-based information.
Pearls and highlights
• The AFAST-derived AFS predicts the degree of anemia anticipated in traumatized and nontraumatized bleeding dogs and thus guides clinical management.
• The TFAST examination detects the presence of PXT, hemothorax, and pericardial effusion in traumatized and nontraumatized small animals, whereas the Vet BLUE is used to assess for various lung parenchymal abnormalities.
• By combining AFAST, TFAST, and the Vet BLUE, veterinarians can rapidly and expediently arrive at a solid working diagnosis.
References
1. Boysen, SR, Rozanski, EA, Tidwell, AS, et al. Evaluation of focused assessment with sonography for trauma protocol to detect abdominal fluid in dogs involved in motor vehicle accidents. J Am Vet Med Assoc. 2004; 225(8):1198–1204.
2. Lisciandro, GR. Abdominal and thoracic focused assessment with sonography for trauma, triage, and monitoring in small animals. J Vet Emerg Crit Care. 2011; 12(2):104–122.
3. Lisciandro, GR, Lagutchik, MS, Mann, KA, et al. Evaluation of an abdominal fluid scoring system determined using abdominal focused assessment with sonography for trauma in 101 dogs with motor vehicle trauma. J Vet Emerg Crit Care. 2009; 19(5):426–437.
4. Lisciandro, GR, Lagutchik, MS, Mann, KA, et al. Evaluation of a thoracic focused assessment with sonography for trauma (TFAST) protocol to detect pneumothorax and concurrent thoracic injury in 145 traumatized dogs. J Vet Emerg Crit Care. 2008; 18(3):258–269.
5. Mandell, DC, Drobatz, K, Feline hemoperitoneum: 16 cases (1986-1993). J Vet Emerg Crit Care. 1995;5(2):93–97.
6. Lisciandro, GR. Evaluation of initial and serial combination focused assessment with sonography for trauma (CFAST) examination of the thorax (TFAST) and abdomen (AFAST) with the application of an abdominal fluid scoring system in 49 traumatized cats [abstract]. J Vet Emerg Crit Care. 2012; 22(2):S11.
7. Ollerton, JE, Sugrue, M, Balogh, Z, et al. Prospective study to evaluate the influence of FAST on trauma patient management. J Trauma. 2006; 60(4):785–791.
8. Blackbourne, LH, Soffer, D, McKenney, M, et al. Secondary ultrasound examination increases the sensitivity of the FAST exam in blunt trauma. J Trauma. 2004; 57(5):934–938.
9. Soderstrom, CA, DuPriest, RW, Jr., Crowley, RA. Pitfalls of peritoneal lavage in blunt abdominal trauma. Surg Gynecol Obstet. 1980; 151(4):513–518.
10. Udobi, KF, Rodriguez, A, Chiu, WC, Scalea, TM, Role of ultrasonography in penetrating abdominal trauma: a prospective study. J Trauma. 2001;50(3):475–479.
11. Matsushima, K, Frankel, H, Beyond focused assessment with sonography for trauma: ultrasound creep in the trauma resuscitation area and beyond. Curr Opin Crit Care. 2011;17(6):606–612.
12. Lichtenstein, DA, Meziere, GA, Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134(1):117–125.
13. Soldati, G, Testa, A, Silva, FR, et al, Chest ultrasonography in lung contusion. Chest. 2006;130(2):533–538.
14. Lisciandro, GR, Fosgate, GT, Fulton, RM. The frequency and number of ultrasound lung rockets (B-lines) using a regionally-based lung ultrasound examination named Vet BLUE (Veterinary Bedside Lung Ultrasound Exam) in dogs with radiographically normal lung findings. Vet Radiol and Ultrasound; accepted 2013.
15. Soldati, G, Sher, S, Testa, A, Lung and ultrasound: time to “reflect,”. Eur Rev Med Pharmacol Sci. 2011;15(2):223–227.
16. Lichtenstein, D, Meziere, G, Biderman, P, Gepner, A, The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26(10):1434–1440.
17. Hecht, S. Thorax. In: Penninck D, D’anjou MA, eds. Atlas of small animal ultrasonography. Ames, IA: Blackwell; 2008:119–150.
18. Reef, VB, Thoracic ultrasonography: non-cardiac imagingReef V, ed.. Equine diagnostic ultrasound. Saunders: Philadelphia, 1998; 187–214.
19. Sigrist, NE, Adamik, KN, Doherr, MG, et al. Evaluation of respiratory parameters at presentation as clinical indicators of the respiratory localization in dogs and cats with respiratory distress. J Vet Emerg Crit Care. 2011; 21(1):13–23.
20. Durkan, SD, Rush, JE, Rozanski, EA, et al. Echocardiographic findings in dogs with hypovolemia. J Vet Emerg Crit Care. 2005; 15:S4.
21. Kirkpatrick, AW. Clinician-performed focused sonography for the resuscitation of trauma. Crit Care Med. 2007; 35(S5):S162–S172.