CHAPTER 65 Ultrasound assisted liposuction
Liposuction has become the most popular cosmetic procedure performed by board-certified plastic surgeons in the United States. Although liposuction is not a technically difficult procedure, it requires thoughtful planning and an artistic eye to achieve aesthetically pleasing postoperative results. The goal of the liposuction surgeon is to remove “target” fat, leaving the desired body contour and smooth transitions between suctioned and non-suctioned areas. Careful selection of patients and proper surgical technique will help avoid contour irregularity, and diligent perioperative care of the patient will help avoid postoperative complications.
Physical evaluation
• What is your current weight?
• How long have you been at this weight?
• Have you had any significant weight gains or losses?
• What is your current diet and exercise regimen?
• For how long have you maintained this regimen?
• Have you taken any diet pills to assist with weight reduction?
Anatomy
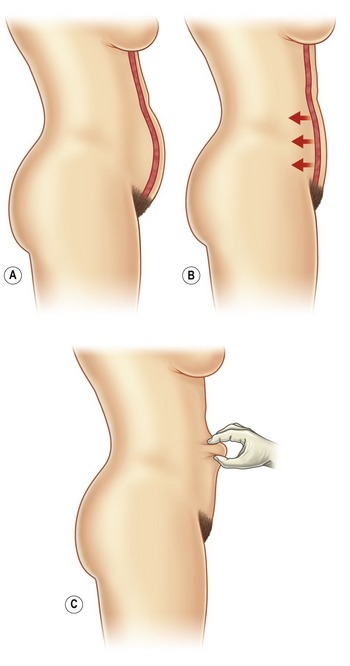
One of the most important factors to consider when evaluating a patient’s candidacy for liposuction is their patient’s skin tone, or dermal quality. It is important to pinch and palpate the skin, assessing for the degree of laxity and dermal thickness (Fig. 65.1). Young thick undamaged dermis is more likely to retract after liposuction and give a desirable result. Thin, stretched skin with striae is unlikely to retract and may look worse after liposuction. If it is determined that the skin quality is not suitable for liposuction, alternative procedures, such as skin excision, may be indicated. Liposuction does not improve cellulite, thus one should not make promises to this effect.
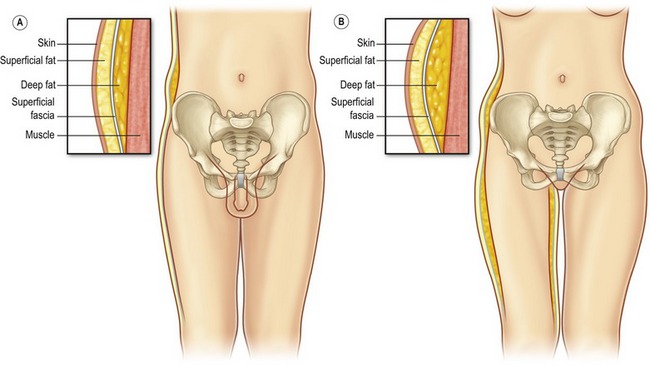
The anatomy of the subcutaneous adipose tissue varies through the body. Some areas of the body have both a deep adipose compartment and a superficial adipose compartment, which are separated by the discrete subcutaneous fascia. The superficial fat in the trunk and thigh consists of smaller lobules, tightly organized within the vertically oriented thin, fibrous septa and the zones of adherence differ between males and females (Fig. 65.2). The deep fat consists of larger lobules arranged more loosely within deeply spaced and more irregularity arranged septa. In these areas, the deep layer of fat is the target for liposuction. The overlying superficial fat is relatively thin and will act as a protective layer to hide small contour deformities, especially for the in experienced liposuction surgeon. In contrast, other areas of the body that are commonly suctioned (arms, lower legs) have only one layer of fat. Suctioning these areas with smaller cannulas will help to avoid contour irregularities.
Technical steps
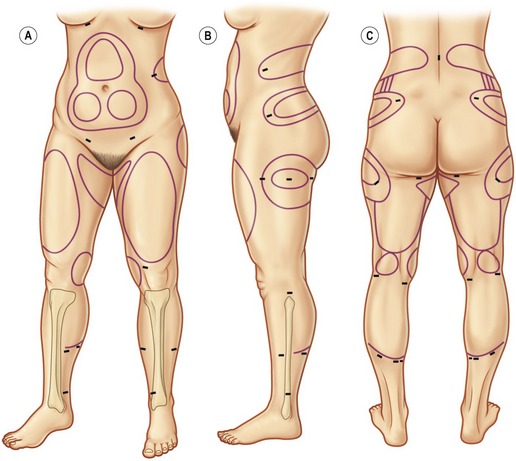
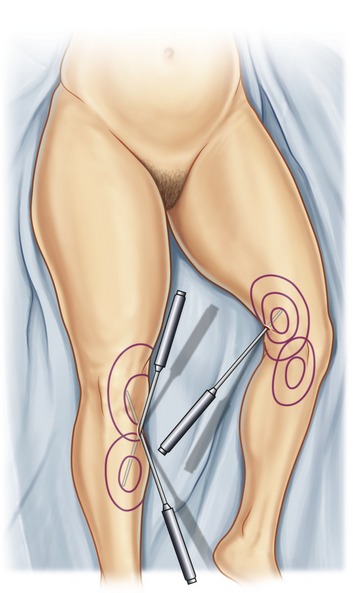
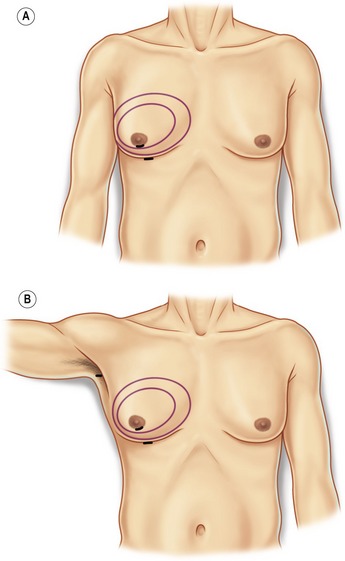
Marking and positioning markings provide a necessary “topographic map” that allows the surgeon to visualize the targeted convexities, to avoid concavities, and to address asymmetries when the patient is lying on the operating table. Markings should be done immediately before surgery with the patient in a standing position (Fig. 65.3). A permanent marking pen is recommended so the markings will not wash off when the patient is prepared. Asymmetries should be carefully marked and brought to the attention of the patient. Depressions and indentations are marked with a different color marker so these areas can be avoided or fat grafts can be planned.
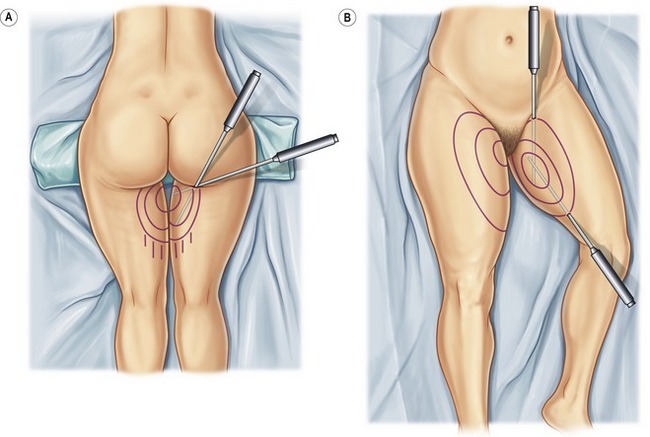
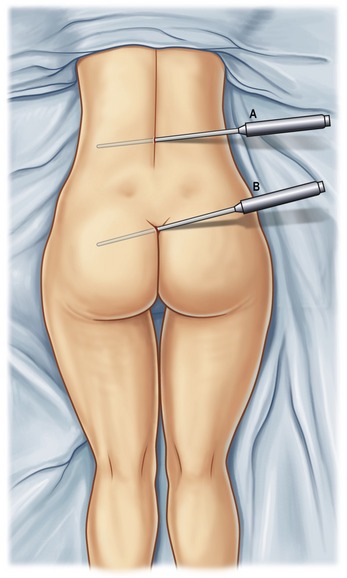
A large soft hip roll placed under the slightly flexed hip facilitates excellent exposure of the back, posterior hips, lateral, posterior and medial thighs. (Figs 65.4, 65.5) Abdomen, breast, arms, anterior and medial thighs, knees, calves and ankles are all best addressed from the supine position. (Figs 65.4, 65.6, 65.7) Patients are prepared with a 3-minute povidone-iodine (Betadine™) scrub, followed by povidone-iodine paint. Bair Hugger™ warming blankets are recommended on unexposed body parts. A Foley catheter should be placed when aspirations of more than 5 liters or multiple procedures are planned. When liposuction is combined with an open surgical procedure or when large-volume liposuction is performed, compression hose and sequential compression boots for prophylaxis of deep venous thrombosis are recommended.
Infiltration of tumescent solution: Standard wetting solution recipes are used for UAL. If large volume removals are planned, the amount of xylocaine is decreased so as not to exceed the recommend 35 mg/kg maximum subcutaneous dose. Our experience and research support the use of room temperature tumescent fluid to minimize the risk of ultrasound induced subcutaneous tissue elevation while maintaining stable core body temperature. The authors recommend infiltration of wetting solution at a 1 : 1 ratio, i.e. Superwet Technique. Accurate record-keeping of the amount infiltrated into each area is recommended.
Evacuation Phase: Even when a hollow ultrasonic cannula is used for application of ultrasonic energy there will still be some fatty emulsion left in the SQ space. (The internal diameter of a standard 5 mm hollow titanium cannula is 1.8 mm). The evacuation phase is performed using traditional liposuction cannulas of the surgeon’s choice. When using a solid probe, the entire volume of fat and fluid will be removed during the evacuation phase. When using a hollow cannula, it is common to remove 50–60% of the total volume during application of energy and the remaining 40–50% during the evacuation phase. Again, careful record-keeping of volumes removed from each area is important. Once all the fatty emulsion is removed one must evaluate the adequacy of treatment based on contour above all other data. Final contouring may be done at this point with small diameter cannulas, using traditional SAL technique. Once the final contouring is performed, the incisions are closed. Drains are recommended in the male breast, and when greater than 2 liters are suctioned from the abdominal area. The patient is dressed in a compression garment that covers the areas that have been suctioned. The author favors the use of compression foam (TopiFoam™) under the garment which seems to decrease bruising and swelling in the early postoperative period.
Postoperative care
Proponents of UAL contend that it is a safe method of body contouring with a number of advantages over traditional liposuction techniques. In addition to being less physically demanding for the surgeon, it is reported to allow greater suction volumes per patient with significantly less blood loss and better control of surface contour. Most long time users of UAL agree that it is not a replacement of traditional SAL techniques but an adjunct to be used in certain areas of the body. The authors feel that UAL is particularly useful in the male breast, the back, the posterior hip (flank) and the lateral thigh because these areas tend to have firmer, more fibrous fat (see Anatomy) and UAL offers the advantage of less surgeon fatigue and better control of surface contour. In areas like the abdomen, arms and anterior thighs, the main advantage of UAL is better control of surface contour, since these areas tend to have soft, loose fat. The authors prefer not to use UAL in the medial thighs, knees, calves and ankles, and neck. The reason for this is that UAL offers little advantage over SAL in these areas, may increase risk or may prevent disadvantages (e.g. ultrasonic probes don’t bend which is a disadvantage in calves and ankles).
Complications
Pearls & pitfalls
Pearls
• Identify and mark asymmetries preoperatively
• Keep accurate intra-operative data of volumes infused and aspirated
• Apply ultrasonic energy only in a wet environment & always keep the ultrasound probe moving
• It’s not what you take out, but what you leave in
• Perform pinch test at beginning, during and at completion of procedure
Summary of steps
1. Markings should be done immediately before surgery with the patient in a standing position.
2. Positioning should be planned before the patient enters the operating room and depends on which areas are being suctioned.
3. Patients are prepared with a 3-minute povidone-iodine (Betadine) scrub, followed by povidone-iodine paint.
4. A Foley catheter should be placed when aspirations of more than 5 liters are planned.
6. Application of energy by continuous hand motion
7. Evacuation and final contouring with small cannulae
Ablaza VJ, Gingrass MK, Perry LC, et al. Tissue temperatures during ultrasound-assisted lipoplasty. Plast Reconstr Surg. 1998;102:534.
Commons G, Halperin B. Ultrasound-assisted lipoplasty: a clinical study of 250 consecutive patients [discussion]. Plast Reconstr Surg. 1998;101:203.
Gamboa-Bobadilla GM. Implant breast reconstruction using acellular dermal matrix. Ann Plast Surg. 2006;56(1):22–25.
Gingrass MK, Kenkel JM. Comparing ultrasound-assisted lipoplasty with suction-assisted lipoplasty. Clin Plastic Surg. 1999;26(2):283–288.
Gingrass MK, Kenkel JM. Comparing ultrasound-assisted lipoplasty with suction-assisted lipoplasty. Clin Plastic Surg. 1999;26(2):283–288.
Goes JC, The use of UAL in breast surgery, Algarve, Portugal. Inaugural meeting of the International Society of Ultrasonic Surgery, 1995.
Manual Lymphatic Drainage (MLD), www.drvodderschool.com.
Rohrich RJ, Beran SJ, Kenkel JM. Ultrasound-assisted liposuction. St. Louis: Quality Medical Publishing; 1998.
Zocchi M. Ultrasonic liposculpturing. Aesthet Plast Surg. 1992;16(4):287–298.
Zocchi ML. Basic physics for ultrasound-assisted lipoplasty. Clin Plastic Surg. 1999;26(2):209–220.
Zocchi ML. Ultrasonic assisted lipoplasty. Technical refinements and clinical evaluations. Clin Plastic Surg. 1996;23(4):575–598.