CHAPTER 28 Ulnar Head and Styloid Fractures
Fractures of the distal ulna have potentially important functional implications for the wrist. Fractures of the ulnar head can disrupt the congruency and/or stability of the distal radioulnar joint (DRUJ) and limit pain-free forearm rotation and hand positioning. Similarly, fractures of the ulnar styloid process, seen more frequently, can on occasion produce secondary instability of either the ulnocarpal joint or the DRUJ if left untreated. It is not necessary to actively treat all fractures of the distal ulna. Those situations in which treatment is necessary to restore function, limit complications, and provide an optimal outcome for these injuries are discussed in this chapter.
Anatomy and Functional Biomechanics
The meticulous histological analysis of the radioulnar ligaments by Nakamura and colleagues1 reveals two predominant attachments to the distal ulna: the fovea and the base of the ulnar styloid process. The foveal attachment—just radial to the base of the ulnar styloid—is over a broad area and gives rise to near-vertical fibers. The styloid base attachment is over a smaller area, and its fibers are orientated horizontally. Both attachments are dense in Sharpey’s fibers. The foveal and styloid base fibers coalesce and then divide to embrace the palmar and dorsal edges of the proximal portion of the articular disc.
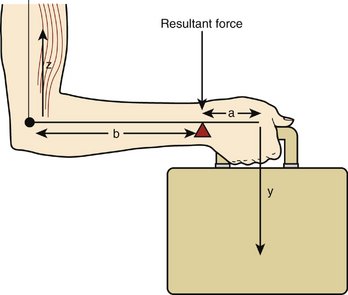
Isolated sectioning studies of the ulnar insertions of these structures have shown that each part plays an equal role in stability when no load is applied across the wrist. One of the primary functions of the distal ulna, however, is as a weight-bearing joint (Fig. 28-1); and when these sectioning studies are repeated under load, the foveal attachment of the radioulnar ligament is found to contribute significantly greater stability to the DRUJ than the styloid attachment.2 This view would be supported by the proximity of the fovea to the rotation axis of the forearm, making it more likely that this is the critical part of the radioulnar ligament’s bony anchorage under dynamic conditions.
Ulnar Head Fractures
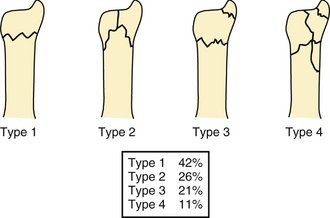
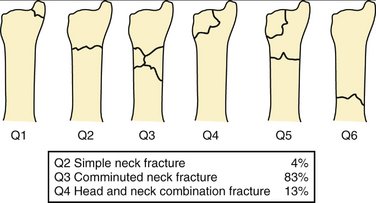
Ulnar head fractures are rare, occurring in only 6% of all wrist fractures.3 The frequency of each fracture configuration is shown in Figure 28-2. More recently, distal ulnar fractures have been classified according to the Comprehensive Classification of Fractures with an associated Q modifier (Fig. 28-3).4
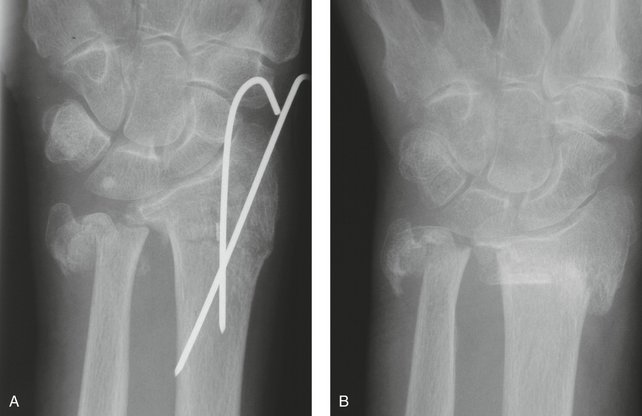
The risk of disabling complications in this injury is unlikely to be DRUJ instability. The attachments of the triangular fibrocartilage complex (TFCC) usually remain undisturbed. These articular fractures will give rise to the usual risks of this group of injuries. Coexistent fractures of the distal radius and ulna significantly increase the incidence of radial nonunion.5 Indeed, this is the most likely circumstance in which the unusual complication of radial nonunion will be seen (Fig. 28-4). In spite of this knowledge, combined distal radius and ulna fractures continue to be managed by treating the radius alone.
Indications
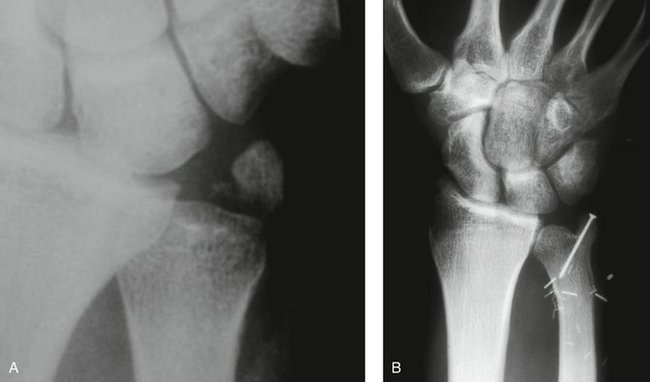
Standard radiographs will provide most of the information about the fracture pattern (Fig. 28-5). Computed tomography (CT) may be necessary on occasion to fully evaluate the injury.
Surgical Technique
General or regional anesthesia is required. Contrary to previous reports,6 regional anesthesia is a safe and comfortable technique that can allow treatment on an outpatient basis.
The approach is deepened ulnar to the sixth extensor compartment to enable the stabilizing implant to be applied on the surface of the distal ulna between the tendons of the flexor carpi ulnaris and extensor carpi ulnaris. It is unusual to need to visualize the articular fragments directly, but in these rare instances a second approach can be made using the same skin incision but passing through the floor of the fifth extensor compartment. Retraction of the tendon of the extensor digiti minimi will allow direct inspection of any articular fragments.
Reduction of the fracture fragments is best performed indirectly using a small angularly stable implant. If reduction is attempted using pointed reduction forceps, the thin cortical bone of the ulnar head often fragments under load, leading to further comminution and possible failure.
The implant is best placed on the medial border of the ulna directly in line with the ulnar styloid. This acts as a buttress for the distal radius to be reduced onto (Fig. 28-6), in this case utilizing a specially designed implant for treating distal ulnar fractures.
Clinical testing of DRUJ stability will reveal if a coexistent unstable TFCC tear is present.
Clinical Examples
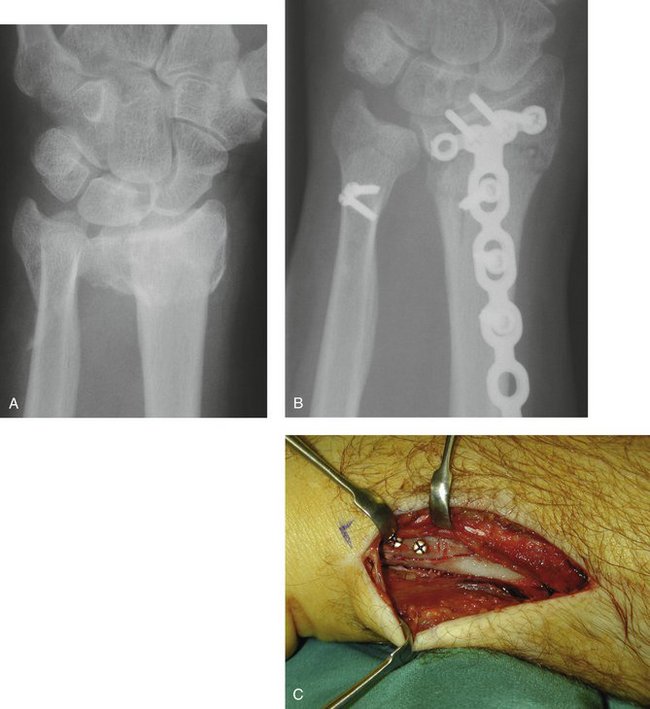
Case 1
A 77-year-old woman presented after a fall with a painful and deformed wrist. The initial radiographs reveal a displaced articular fracture of the distal radius and a minimally displaced long oblique extra-articular fracture of the distal ulna (Fig. 28-7A, B). Initial treatment consisted of the application of a bridging external fixator. The surgeon clearly concentrated on the reduction of the distal radius fracture, but—in the absence of an intact ulnar buttress—displacement of the unstable ulnar fracture was inevitable (see Fig. 28-7C, D).

FIGURE 28-7 Case 1. A and B, Fractures of both distal radius and ulna. C and D, After application of a bridging external fixator to the distal radius only. E, After ORIF of both bones with angularly stable implants.
Stabilization by open reduction and internal fixation (ORIF) using a 2.0-mm mini-condylar plate (Synthes) (see Fig. 28-7E) and a volar distal radius plate (Synthes) allowed early movement and an almost complete recovery of function 3 months after surgery.
Had the necessity for the distal ulna to act as a weight-bearing buttress been appreciated at an early stage, the ulnar fracture could have been treated by a much simpler method of stabilization such as multiple lag screws. An example of this method of treatment for a similar fracture is shown in Figure 28-8.
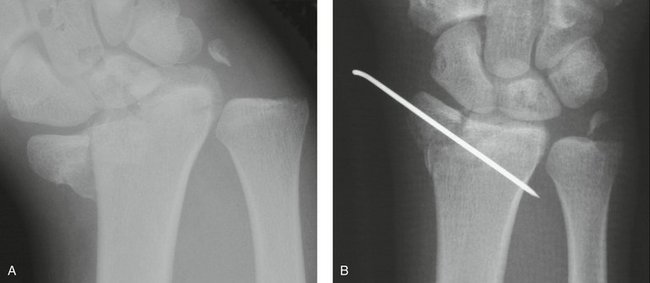
Case 2
A 20-year-old man was involved in a motor vehicle accident, sustaining multiple life-threatening injuries. His initial treatment concentrated on his major visceral trauma and unstable pelvic fracture. He sustained a displaced fracture of the distal radius and ulna (Fig. 28-9A, B) that was managed initially by a bridging external fixator (see Fig. 28-9C, D).

FIGURE 28-9 Case 2. A and B, Extra-articular fracture of distal radius with associated palmarly displaced ulnar head fracture. C and D, After initial stabilization with bridging external fixator to the distal radius only. E, After ORIF to stabilize both bones using angularly stable implants.
ORIF of both fractures using a 2.0-mm mini-condylar plate (Synthes) and a dorsal distal radius plate (Synthes) (see Fig. 28-9E) allowed immediate rehabilitation and a return to full function.
Results
Reports of treatment of these unusual fractures are rare.
In 2004, we reported our series of 24 distal ulna fractures, associated with fractures of the distal radius, stabilized with a mini-condylar plate (Synthes).4 The majority of cases (83%) were comminuted neck fractures. In a small number of isolated ulnar head fractures, simple lag screws were also used. An average range of rotation of 146 degrees (76 degrees of pronation, 70 degrees of supination) was achieved at an average of 26 months after surgery. The average flexion/extension arc was 102 degrees (50 degrees flexion, 52 degrees extension). Nonunion of the distal ulna was seen in only one case and was treated by revision grafting and plating and went on to uneventful union.
Ulnar Styloid Fractures
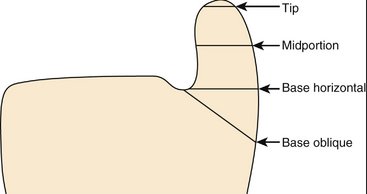
It is generally recognized that there are four distinct fracture configurations of the ulnar styloid process (Fig. 28-10).
Incidence
All authors agree that more than 50% of distal radial fractures are accompanied by fractures of the ulnar styloid. In a study of 130 distal radius fractures,7 71 were noted to have a coexistent ulnar styloid fracture (55%). Of these, 39% involved the base (Fig. 28-11).
Radiographic Prediction of DRUJ Instability
Instability of the DRUJ complicates a reported 3% to 37% of distal radius fractures,8,9 yet fewer than 10% of distal radius fractures demand a surgical procedure on the distal ulna.7,10 Instability relates to detachment of a significant portion of the TFCC—significant in either size or location. These situations arise either by a direct tear through a critical amount of the soft tissue component or by fracture through its bony anchorage.
Nakamura and colleagues11 assessed the relevance of each of the four levels of ulnar styloid fracture on DRUJ stability in 10 cadaveric wrists and found no instability in styloid tip or midportion fractures but up to a 20% loss of stiffness (stability) in basal horizontal fractures. Basal oblique fractures, however, produced up to 70% loss of stiffness.
Wide displacement of any type of ulnar styloid fracture was also recognized as a significant risk for development of DRUJ instability—presumably because wide displacement would not be possible without a significant soft tissue tear (Fig. 28-12).
Surgical Technique
Soft tissue reattachment of the TFCC is not discussed in this chapter.
A number of different bony reconstruction techniques can be used.
Clinical Examples
Case 3
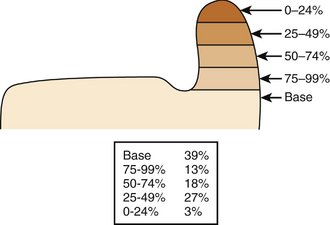
A 35-year-old man was involved in a motor vehicle accident in which he was thrown from his vehicle. He sustained an open injury to the ulnar side of his right wrist (Fig. 28-13A). After appropriate wound débridement, the displaced ulnar styloid basal oblique fracture was reduced and secured with a single 1.5-mm lag screw (see Fig. 28-13B). After reconstruction of the soft tissue defect with a lateral arm free flap, the skeletal stability allowed early rehabilitation and return to full function.
Case 4
A 23-year-old male professional rugby player complained of pain and “clunking” in his wrist on impact after an injury sustained during play. Plain radiographs revealed a displaced basal oblique fracture of the ulnar styloid (Fig. 28-14A). There was a suspicion that this was not a totally new injury and that a fibrous union of a previous fracture had been disrupted. Perifracture sclerosis was seen, suggesting a mature injury. The fracture was opened as described earlier and the fracture surfaces débrided to healthy cancellous bone. A tension band wiring was performed to stabilize the DRUJ and prevent further instability and “clunking” (see Fig. 28-14B, C), allowing a stable normal active range of motion.

FIGURE 28-14 Case 4. A, Displaced basal oblique fracture of the ulnar styloid. B and C, Tension band wiring.
An alternative method of securing the tension band wire loop is shown (Fig. 28-15). This technique should be used with caution in the distal ulna because of the often uncomfortable prominence of the screw head through the skin.
Results
It remains the case that the presence of an ulnar styloid fracture represents a poor prognostic sign in wrist injuries.13–17 The natural progression of this idea is to recommend regular operative stabilization of these injuries,18 but this approach fails to differentiate between different styloid fracture patterns.
In contrast to an interventional approach, Tsukazaki and coworkers19 examined 83 distal radius fractures to assess prognostic factors. In keeping with other descriptions on incidence, 44 cases (53%) had evidence of ulnar styloid injury. Again, no information was provided on the exact fracture configurations, yet only 19 fractures (43%) showed radiological evidence of union. There was no correlation between functional outcome, residual pain, and the presence or absence of an ulnar styloid fracture or nonunion. It is likely that the vast majority of these injuries were stable injuries of the DRUJ.
Few studies comment on the effects of fixation of ulnar styloid fractures.20 No correlation between TFCC stabilization and outcome was found in a heterogenous group of Colles’ fractures. Since these studies were published, the accuracy of classification has improved enormously. We now accept that the exact fracture configuration in both the radial and ulnar sides of each injury is the critical determinant in stability and, therefore, outcome.
Nonunion
As previously stated, there seems to be no correlation between ulnar styloid nonunion and functional outcome. Fractures of the tip of the ulnar styloid frequently fail to unite but appear to be less of a clinical problem because they are unlikely to be associated with instability17 (Fig. 28-16).
Ulnar styloid nonunion has been classified21 into type 1 (with a stable DRUJ) and type 2 (with an unstable DRUJ). Those patients with symptomatic type 1 nonunion respond well to simple excision of the ununited fragment, whereas those patients with symptomatic type 2 nonunion require formal reconstruction and TFCC reattachment.
1 Nakamura T, Takayama S, Horiuchi Y, Yabe Y. Origins and insertions of the triangular fibrocartilage complex: a histological study. J Hand Surg [Br]. 2001;26:446-454.
2 Haugstvedt JR, Berger RA, Nakamura T, et al. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg [Am]. 2006;31:445-451.
3 Biyani A, Simison AJM, Klenerman L. Fractures of the distal radius and ulna. J Hand Surg [Br]. 1995;20:357-364.
4 Ring D, McCarty LP, Campbell D, Jupiter JB. Condylar blade plate fixation of unstable fractures of the distal ulna associated with fracture of the distal radius. J Hand Surg [Am]. 2004;29:103-109.
5 McKee MD, Waddell JP, Yoo D, Richards RR. Nonunion of distal radial fractures associated with distal ulnar shaft fractures: a report of four cases. J Orthop Trauma.. 1997;11:49-53.
6 Kambouroglou G. Fractures of the distal ulna. In: Giannoudis PV, Pape HC, editors. Orthopaedic Trauma Surgery. Cambridge, England: Cambridge University Press; 2006:56-59.
7 May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg [Am]. 2002;27:965-971.
8 Frykman G. Fractures of the distal radius including sequelae of shoulder-hand-finger syndrome, disturbance in the distal radioulnar joint and impairment of nerve function: a clinical and experimental study. Acta Orthop Scand. 1967;108(Suppl.):1-124.
9 Solgaard S. Function after distal radius fracture. Acta Orthop Scand. 1988;59:39-42.
10 Fernandez DL. Fractures of the distal radius: operative treatment. AAOS Instruct Course Lect.. 1993;42:73-88.
11 Nakamura T, Moy OJ, Peimer CA. Relationship between the ulnar styloid fracture and DRUJ instability. J Hand Surg [Br]. 2003;28(Suppl 1):48.
12 Ruch DS, Lumsden BC, Papadonikolakis A. Distal radius fractures: a comparison of tension band wiring versus ulnar outrigger external fixation for the management of distal radioulnar instability. J Hand Surg [Am]. 2005;30:969-977.
13 Knirk JL, Jupiter JB. Intraarticular fractures of the distal end of the radius in young adults. J Bone Joint Surg [Am]. 1986;68:647-659.
14 De Bruijn HP. Functional treatment of Colles’ fracture. Acta Orthop Scand Suppl. 1987;223:1-95.
15 Roumen RMH, Hesp WLEM, Bruggink EDM. Unstable Colles fractures in elderly patients: a randomised trial of external fixation for redisplacement. J Bone Joint Surg Br. 1991;73:307-311.
16 Sanders RA, Keppel FL, Waldrop JI. External fixation of distal radius fractures: results and complications. J Hand Surg [Am]. 1991;16:385-391.
17 Stoffelen D, De Smet L, Broos P. The importance of the distal radioulnar joint in distal radial fractures. J Hand Surg [Br]. 1998;23:507-511.
18 Buterbaugh GA, Palmer AK. Fractures and dislocations of the distal radio-ulnar joint. Hand Clin. 1988;4:361-375.
19 Tsukazaki T, Takagi K, Iwasaki K. Poor correlation between functional results and radiographic findings in Colles’ fracture. J Hand Surg [Br]. 1993;18:588-591.
20 Ekenstam F, Jakobsson OP, Wadin K. Repair of the triangular ligament in Colles’ fracture: no effect in a prospective randomized study. Acta Orthop Scand. 1989;60:393-396.
21 Hauck RM, Hershey PA, Shahen J, Palmer AK. Classification and treatment of ulnar styloid nonunion. J Hand Surg [Am]. 1996;21:418-422.