Abdominal lymphadenopathy is most common

 usually seen in elderly individuals who have had exposure to enteric mycobacteria, often from drinking unpasteurized milk.
usually seen in elderly individuals who have had exposure to enteric mycobacteria, often from drinking unpasteurized milk.
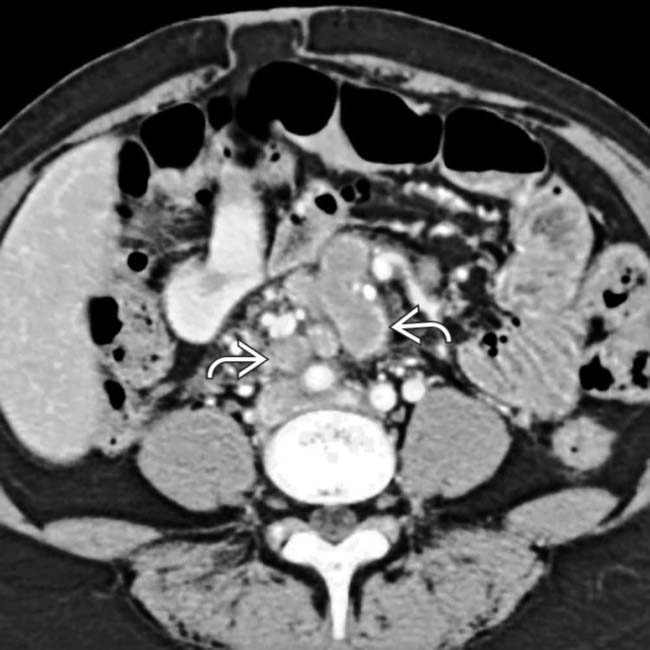
 , peritoneum, and mesentery, with enlargement of mesenteric nodes
, peritoneum, and mesentery, with enlargement of mesenteric nodes  . Loculated ascites was also present (not shown). This patient’s reactivated TB with TB peritonitis was first acquired in his native country.
. Loculated ascites was also present (not shown). This patient’s reactivated TB with TB peritonitis was first acquired in his native country.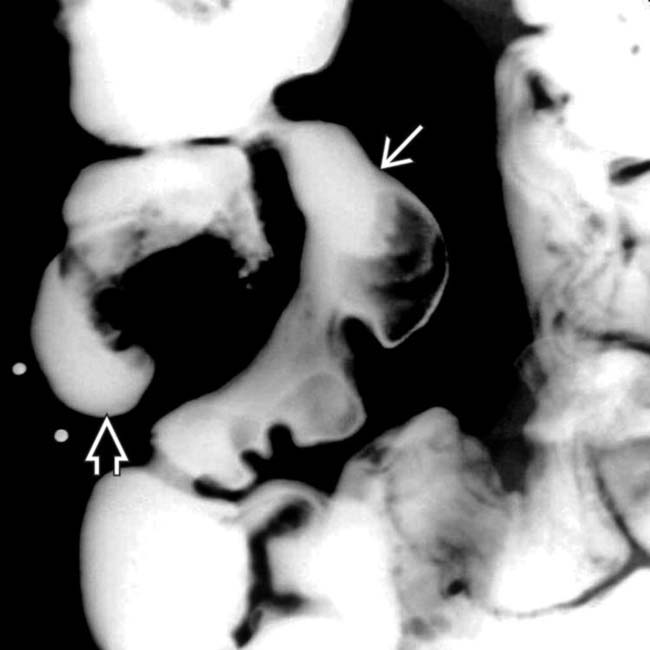
 and cecum
and cecum  , with asymmetric thickening and stiffening of the bowel walls, ultimately found to represent TB.
, with asymmetric thickening and stiffening of the bowel walls, ultimately found to represent TB.
 of the cecum, which has a cone-shaped appearance in a patient with tuberculous colitis.
of the cecum, which has a cone-shaped appearance in a patient with tuberculous colitis.IMAGING
General Features
Radiographic Findings
• Lymphadenopathy (tuberculous lymphadenitis)
 Can range from increased number of normal-sized nodes to massively enlarged conglomerate nodal masses
Can range from increased number of normal-sized nodes to massively enlarged conglomerate nodal masses
 Can range from increased number of normal-sized nodes to massively enlarged conglomerate nodal masses
Can range from increased number of normal-sized nodes to massively enlarged conglomerate nodal masses
• Tuberculosis peritonitis
• Gastrointestinal tuberculosis
• Hepatosplenic tuberculosis
 Micronodular pattern
Micronodular pattern
 Micronodular pattern
Micronodular pattern
• Renal tuberculosis
 characteristic of mycobacterial infection.
characteristic of mycobacterial infection.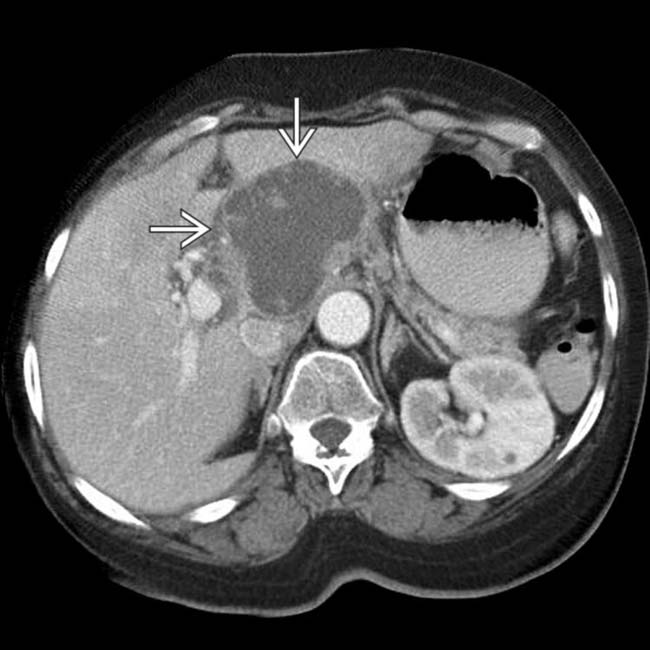
 in the porta hepatis and pancreatic head region, representing conglomerate caseated, enlarged nodes due to Mycobacterium tuberculosis infection.
in the porta hepatis and pancreatic head region, representing conglomerate caseated, enlarged nodes due to Mycobacterium tuberculosis infection.
 and multilobar bronchoalveolar infection of the lungs, typical of active tuberculosis. This patient was a young female college exchange student from Asia.
and multilobar bronchoalveolar infection of the lungs, typical of active tuberculosis. This patient was a young female college exchange student from Asia.
 , along with regional mesenteric lymphadenopathy
, along with regional mesenteric lymphadenopathy  typical of intestinal and nodal involvement by TB.
typical of intestinal and nodal involvement by TB.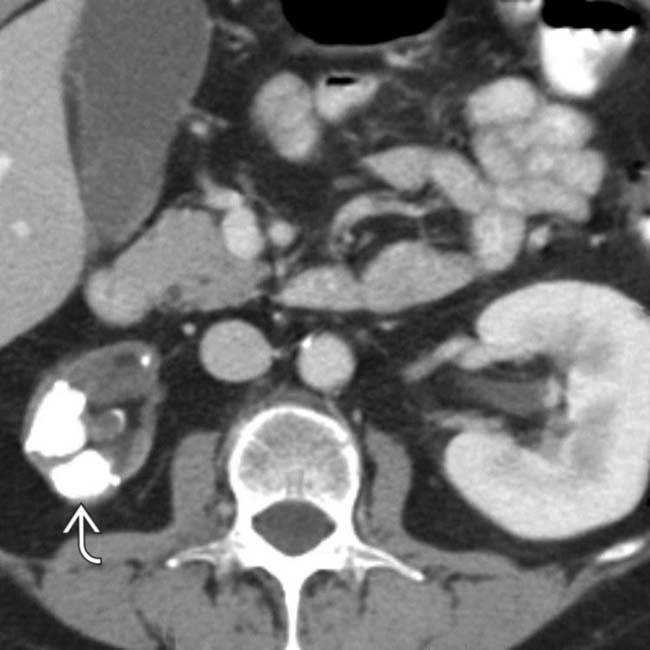
 , typical of chronic TB infection of the kidney. The patient had a known history of pulmonary TB.
, typical of chronic TB infection of the kidney. The patient had a known history of pulmonary TB.
 . The left kidney
. The left kidney  is totally calcified and nonfunctional, an autonephrectomy or “putty” kidney due to chronic renal TB. Small focal calcifications were also present in the adrenals.
is totally calcified and nonfunctional, an autonephrectomy or “putty” kidney due to chronic renal TB. Small focal calcifications were also present in the adrenals.






































































 in the porta hepatis and pancreatic head region, representing caseated, enlarged nodes due to M. tuberculosis infection.
in the porta hepatis and pancreatic head region, representing caseated, enlarged nodes due to M. tuberculosis infection.
 .
.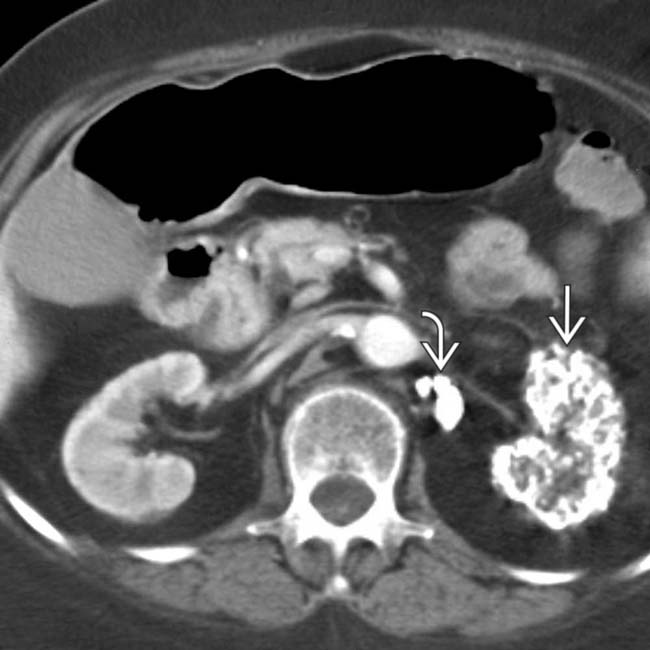
 . The left kidney
. The left kidney  is totally calcified and nonfunctional, representing an “autonephrectomy” due to chronic renal TB.
is totally calcified and nonfunctional, representing an “autonephrectomy” due to chronic renal TB.


