13 Trunk and spine
Pain in the back is the commonest symptom encountered in orthopaedic practice. Indeed, if accident cases are excluded, it probably accounts for nearly a third of all orthopaedic out-patient attendances.
SPECIAL POINTS IN THE INVESTIGATION OF BACK AND SCIATIC SYMPTOMS
Exposure
The patient should be stripped completely, except for undergarments and, in women, a brassière.
Steps in routine examination
A suggested plan for the routine clinical examination of the back is summarised in Table 13.1.
Table 13.1 Routine clinical examination in suspected disorders of the back
| 1. LOCAL EXAMINATION OF THE BACK, WITH NEUROLOGICAL SURVEY OF THE LOWER LIMBS | |
| (Patient standing) | Costo-vertebral joints |
| Inspection | Range indicated by chest expansion |
| Bone contours and alignment: | Sacro-iliac joints |
| (?visible deformity) | (Impracticable to assess range) |
| Soft-tissue contours | ? Pain on movement imparted by |
| Colour and texture of skin | lateral compression of pelvis |
| Scars or sinuses | (Patient recumbent) |
| Palpation | Palpation of iliac fossae |
| Skin temperature | Examine specifically for abscess |
| Bone contours | or mass |
| Soft-tissue contours | Neurological state of lower limbs |
| Local tenderness | Straight leg raising test |
| Movements | Muscular system |
| Spinal joints | Sensory system |
| Flexion | Reflexes |
| Extension | |
| Lateral flexion | |
| Rotation | |
| ? Pain on movement | |
| ? Muscle spasm | |
| 2. EXAMINATION OF POTENTIAL EXTRINSIC SOURCES OF BACK PAIN AND SCIATICA | |
| This is important if a satisfactory explanation for the symptoms is not found on local examination. The investigation should include: | |
| 1. the abdomen | |
| 2. the pelvis, including rectal examination | |
| 3. the lower limbs | |
| 4. the peripheral vascular system | |
| 3. GENERAL EXAMINATION | |
| General survey of other parts of the body. The local symptoms may be only one manifestation of a widespread disease | |
Movements of the spinal column and related joints
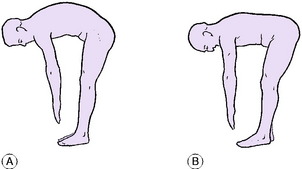
The spinal column. The joints of the spinal column must necessarily be considered as a group, for it is impracticable to study the movement of each joint independently. The movements to be examined are flexion, extension, lateral flexion to right and left, and rotation to right and left. It should be noted particularly whether the spinal muscles go into protective spasm when movement is attempted. Flexion: Instruct the patient to stretch the fingers towards the toes, keeping the knees straight. It is important to judge what proportion of the movement occurs at the spine and how much is contributed by hip flexion (Fig. 13.1). Some patients can almost reach their toes, despite a stiff back, simply by flexing unusually far at the hips. (Normally the hamstrings limit hip flexion to about 90 ° when the knees are straight.) The range may be expressed roughly as a percentage of the normal, or as the distance by which the fingers fail to reach the floor. A more accurate assessment is made by measuring the linear widening of the interspinous spaces as indicated by a tape measure laid along the line of the spinous processes, which may be marked with a pen. The excursion of the spinous processes between full extension and fullest flexion may thus be measured on the tape. An excursion of four centimetres between the twelfth thoracic spinous process and the first sacral prominence between full extension and fullest flexion indicates good lumbar mobility. Extension: Instruct the patient to arch the spine backwards, looking up at the ceiling. Judge the range and express approximately as a percentage of the normal; or measure the excursion as described above. Lateral flexion: Instruct the patient to slide each hand in turn down the lateral side of the corresponding thigh. Observe the range. Rotation: With the feet fixed, the patient rotates the shoulders towards each side in turn. Hold the pelvis steady, and note the range of spinal rotation as distinct from that which occurs at the knees and hips.
Related joints. The costo-vertebral joints: The mobility of the costo-vertebral joints is judged from the range of chest expansion. The normal difference in chest girth between full inspiration and full expiration is about 7 or 8 cm. A marked reduction of chest expansion is of particular significance when ankylosing spondylitis is suspected. The sacro-iliac joints: It is not practicable to measure the range of sacro-iliac movement. But the joints should be moved passively to determine whether pain is produced, as it will be in arthritic conditions of the joints. A simple method is to grip each iliac crest and compress the pelvis strongly from side to side.
Palpation of iliac fossae and groins
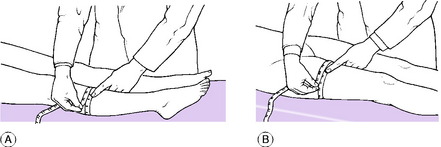
Palpation of the iliac fossae and groins is an essential step in the examination of the back. Its specific purpose is to determine whether or not there is a soft-tissue thickening or abscess. It should be remembered that a ‘psoas’ abscess originating from a tuberculous lesion of the lumbar spine first becomes palpable deep in the iliac fossa. Such an abscess is felt most easily by pressing the flat palmar surface of the hand and fingers against the flat inner aspect of the iliac bone. To do this the surgeon must stand at the side of the couch corresponding to the side being examined – that is, he must stand on the right of the patient to examine the right iliac fossa and on the left to examine the left iliac fossa (Fig. 13.2).
Neurological examination of the lower limbs
Straight leg raising test. Holding the knee straight, lift each lower limb in turn to determine the range of pain-free movement (normal = 90 °; often more in women) (Fig. 13.3). When associated with clearly defined sciatica (and in the absence of gross disease of the hip), marked impairment of straight leg raising by pain suggests mechanical interference with one or more of the roots of the sciatic nerve. The pain is easily explained. Even a normal sciatic nerve is tautened by straight leg raising, though not to the point of causing pain by dragging on the meningeal sheath that encloses the nerve root. If a nerve is already stretched or anchored, as by a protruded piece of an intervertebral disc or a tumour, the further tautening entailed in lifting the limb is sufficient to cause pain.

Fig. 13.3 The straight leg raising test, an important part of the neurological examination of the lower limbs.
When a nerve is tensely stretched, raising the straight leg on the unaffected side may cause pain on the affected side. This sign, termed the crossed sciatic reflex, is a well-recognised feature of prolapsed lumbar intervertebral disc with nerve pressure.
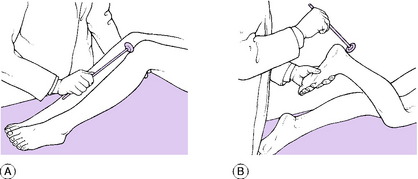
Muscular system. Examine the muscles for wasting, hypertrophy, and fasciculation. Note the tone and test the power of each muscle group, comparing it with its counterpart in the opposite limb. Circumferential measurement is a reliable method of comparing the bulk of the calf muscles, the girth being measured at the widest part or ‘equator’ (Fig. 13.4A). Circumferential measurement of the thighs, on the other hand, tends to be inaccurate, and may be misleading, on account of the conical shape of the thigh (Fig. 13.4B). Often a more accurate assessment of the relative volume of the two thighs is obtained from inspection and palpation. If the thighs are measured, the girth should be taken on each side at an equal distance above the knee – 12 or 15 cm above the upper margin of the patella is usually a convenient level.
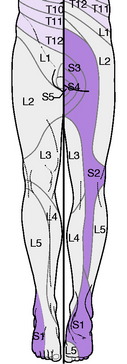
Sensory system. Examine the patient’s sensibility to touch and pin prick, paying particular attention to the sites of any impairment. A knowledge of the innervation of the dermatomes (Fig. 13.5) is essential as this may give an indication of the level of any nerve roots affected. When indicated, test also the sensibility to deep stimuli, joint position, vibration, and heat and cold.
Reflexes. Compare on the two sides the knee jerk (dependent mainly on the L4 nerve) and the ankle jerk (mainly S1). It is important to note not only the presence or absence of the response, but also any difference of intensity (Fig. 13.6). Test the plantar reflex.
Imaging
Radiographic examination. If the complaint is clearly localised to the thoracic spine, antero-posterior and lateral radiographs of that area alone will usually suffice. If the lumbar spine is the part complained of, radiographs should include not only antero-posterior and lateral views of the lumbar spine but also at least one view of the sacro-iliac joints, pelvis, and hip joints. In cases of doubt additional projections may be required. Oblique projections – from half right and half left – are essential for the proper study of the sacro-iliac joints and the posterior intervertebral (facet) joints of the lumbar region. If a spinal tumour is suspected further imaging with magnetic resonance scanning is required.
Other methods of imaging. Radioisotope bone scanning p. 21 is of particular value in examination of the spinal column, especially in the early detection of metastatic deposits.
Computerised tomography (CT scanning) p. 12 is valuable in selected cases. It gives cross-sectional images of the trunk that reveal bony abnormalities very clearly.
CONGENITAL ABNORMALITIES AND DEFORMITIES
LUMBAR AND SACRAL VARIATIONS
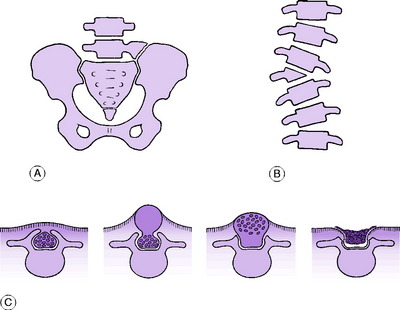
Minor variations of the bony anatomy are common, especially in the lumbar and sacral regions. Most are of little practical importance. They include: deficient or rudimentary lowest ribs; incomplete or complete incorporation of the fifth lumbar vertebral body in the sacrum (sacralisation of the fifth lumbar vertebra); persistence of the first sacral segment as a separate vertebra (lumbarisation of the first sacral vertebra); and over-development of the fifth lumbar transverse process on one or both sides with, in marked cases, a false joint between the hypertrophied process and the ilium (Fig. 13.7A). In the last- mentioned condition the false joint is sometimes a source of pain.
HEMIVERTEBRA
In this anomaly a vertebra is formed in one lateral half only. The defect may occur at any level. The body of the half-vertebra is wedge-shaped, and the spine is angled laterally at the site of the defect (Fig. 13.7B). This anomaly is a rare cause of scoliosis.
SPINA BIFIDA (Spinal dysraphism)
The basic fault in spina bifida is a failure of the embryonic neural plate to fold over to form a closed neural tube, or of mesodermal tissue fully to invest the neural tube as it does in the normal embryo to form the vertebral arch with its spinous process and the surrounding muscles and ligaments. Different grades of the anomaly are shown in Figure 13.7C.
In most cases spina bifida is of minor degree and not a cause of disability. Indeed it is often found incidentally during radiography for some other reason. The importance of spina bifida lies in the fact that in the more severe forms there is a co-existing lesion of the nerve elements. The subject of spina bifida with neurological involvement was discussed in Chapter 11 p. 171.
SCOLIOSIS
Idiopathic structural scoliosis
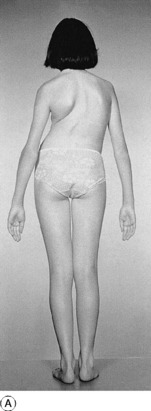
Pathology. Any part of the thoraco-lumbar spine may be affected. There is a primary structural curve, with secondary compensatory curves above and below. The pattern of curve and its natural evolution are fairly constant for each site, and the following types are recognised: lumbar scoliosis, thoraco-lumbar scoliosis, and thoracic scoliosis (Fig. 13.8A). The lateral curvature is constantly accompanied by rotation of the vertebrae on a vertical axis, the body of the vertebra rotating towards the convexity of the curve and the spinous process away from the convexity. By thrusting the ribs backwards on the convex side this rotation increases the ugliness of the deformity (Fig. 13.8).
Treatment. The first essential is to assess the prognosis for progression of the deformity from a consideration of the age of onset and the site and severity of the curve. This requires the identification of the first and last vertebrae in the primary curve and the measurement of the Cobb angle between them on an erect AP radiograph of the spine (Fig. 13.9). When the prognosis is good (for instance, in most cases of lumbar scoliosis) expectant treatment, with regular clinical and radiological reviews every six months, may be all that is required. But when the prognosis is poor (as in thoracic scoliosis with early onset or a curve in excess of 45–50°) active treatment is advised. This usually necessitates operation, and much surgical endeavour has been spent in the quest for an effective and safe method of correcting the deformity and maintaining the correction while fusion occurs. Surgical treatment is usually deferred until early adolescence to minimise the loss of height which may result from fusion of a significant length of the growing spine. To prevent further deterioration in the curvature during this waiting period, conservative management with various types of orthotic bracing has been used.
For many years the brace most commonly employed was the Milwaukee brace. This used the principle of three-point correction by distracting the spine between a pelvic band and an occipito-cervical support, with additional lateral pressure from a pad applied to the chest wall at the apex of the curvature. Recently doubt has been cast on the effectiveness of this type of bracing, and because of frequent problems of acceptance by the patient, an alternative under-arm thoraco-lumbar jacket, or Boston brace (Fig. 13.10), has been used. This provides only two-point correction and it acts by flattening the lumbar lordosis; thus it is most suitable for lower curvatures with an apex below the ninth thoracic vertebra.
The principle of surgical treatment is to fuse the joints of all the vertebrae within the primary curve, after having first achieved the greatest possible correction of the curvature. When surgical treatment was first introduced correction was obtained by pre-operative traction or corrective plaster casts. It is now routinely gained at the time of operation by the use of an internal corrective implant. For many years the device used for this purpose was the Harrington distraction rod. This was inserted posteriorly in the concavity of the curve between two hooks placed under the laminae of the top and bottom vertebrae and then forcibly elongated to produce straightening. The results from this technique were encouraging, with up to 50% correction of the lateral curvature, though this was not reflected in improvement of the cosmetic deformity, which largely results from vertebral rotation. This led to a search for other methods of correction including the use of anterior interbody fixation devices, though these necessitated thoracotomy with its associated morbidity in terms of decreased lung function. Currently most specialist surgeons favour posterior correction with multiple-level segmental pedicle screw fixation devices (Cotrel-Dubousset instrumentation) (Fig. 13.11). This was an advance over the Harrington instrumentation because it improved correction in both the sagittal and coronal planes.


Fig. 13.11 A and B Radiographs of the same patient shown in Figure 13.9 after surgical correction and fusion with segmental pedicle fixation which has reduced the curve to 8 °.
Other methods of fixation and correction may be required for more severe curvatures, or when abnormal vertebral pathology exists, as in congenital curvatures which may include a kyphotic component.
Secondary structural scoliosis
In this group the spinal curvature is secondary to a demonstrable underlying abnormality.
Pathology. In congenital hemivertebra there is a sharp angulation at the site of the anomaly, with compensatory curves above and below (Fig. 13.7B). Scoliosis following poliomyelitis is explained by unequal pull of the muscles on the two sides. The mechanism of scoliosis complicating neurofibromatosis is not clear; in this type the deformity may be very severe.
Treatment. In most cases treatment is along the lines suggested for idiopathic scoliosis.
Sciatic scoliosis
Sciatic scoliosis is a temporary deformity produced by the protective action of muscles in certain painful conditions of the spine.
Cause. In many cases the underlying cause is a prolapsed intervertebral disc impinging upon a lumbar or sacral nerve. But the deformity may also be observed in some cases of acute low back pain p. 241, the pathogenesis of which is not entirely clear.
Clinical features. The predominant feature is severe back pain or sciatica, aggravated by movements of the spine (see prolapsed lumbar intervertebral disc, p. 236. The onset is usually sudden. The scoliosis is poorly compensated; so the trunk may be tilted over markedly to one side (see Fig. 13.27, p. 238. The curvature is not associated with rotation of the vertebrae.
Treatment. The treatment is that of the underlying condition.
TUBERCULOSIS OF THE THORACIC OR LUMBAR SPINE (TUBERCULOUS SPONDYLITIS; POTT’S DISEASE1)
Tuberculosis of thoracic or lumbar vertebral bodies was formerly one of the commonest forms of skeletal tuberculosis, and it is still prevalent in some Eastern countries, though now seen only rarely in the West.
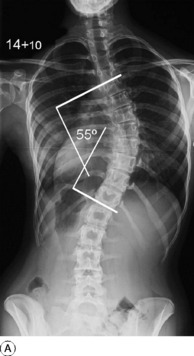
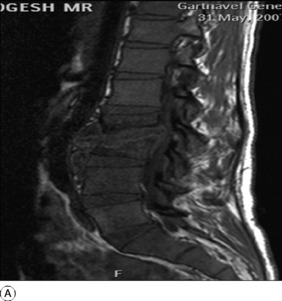
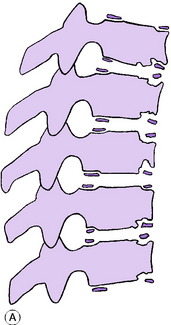
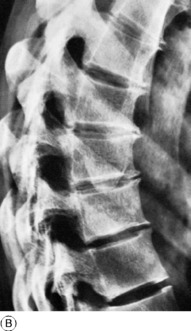
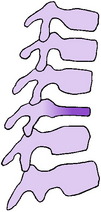
Pathology. The infection begins at the anterior margin of a vertebral body, near the intervertebral disc (Fig. 13.12A). The disc itself is usually involved at an early stage. The extent of the destruction varies widely from case to case. Commonly there is complete destruction of one intervertebral disc with partial destruction of the two adjacent vertebrae, most marked anteriorly (Fig. 13.12B). But the changes may extend over several spinal segments; or, on the other hand, they may be confined to a single intervertebral disc, without evident bone involvement (Fig. 13.13A). Anterior collapse of the affected vertebrae leads to an angular kyphosis (Figs 13.12B, 13.13B and 13.14).
Abscess formation is usual. In the thoracic region pus collects around the spinal column, forming a fusiform paraspinal abscess (Fig. 13.14); or it may track towards the surface between ribs. From the lower thoracic or lumbar region pus tracks downwards behind the fascial sheath of the psoas muscle and generally bursts into the compartment behind the iliacus fascia to form a palpable abscess in the iliac fossa (psoas abscess). An abscess occasionally points posteriorly, or in the thigh. As in most instances of skeletal tuberculosis, the inflammation is low-grade and chronic rather than acute: hence the term ‘cold abscess’ for the quiet suppuration that is a common feature.
Secondary effects. An abscess or mass of granulation tissue encroaching upon the spinal canal may interfere with the spinal cord or with a spinal nerve. In cases of long-standing severe kyphosis the spinal cord is occasionally damaged by the bony ridge at the site of deformity.
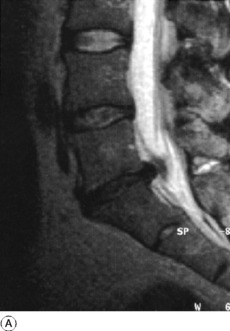
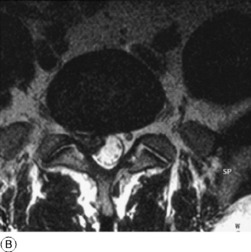
Imaging. On radiographic examination the earliest signs are narrowing of an intervertebral space (Fig. 13.13A) and local vertebral osteoporosis. Later, there is usually destruction of bone at the anterior margin of one or more of the vertebral bodies, leading to anterior collapse and wedge-shaped deformity of the affected vertebrae (Figs 13.13B and 13.14). An abscess shadow is nearly always visible: in the thoracic region it is seen as a fusiform paraspinal shadow (Fig. 13.14); in the lumbar region it is indicated by lateral bulging of the psoas outline, usually on one side. In the healing stage the bone outline in the area of destruction becomes sharper, and normal density is regained. Abscesses may become calcified. Magnetic resonance imaging (MRI) is useful in defining the extent of the soft-tissue abscess more clearly, especially if there are signs of spinal cord dysfunction (Fig. 13.15). Ultrasound scanning is useful in defining the extent of an abscess.
Prognosis. The prognosis is worse in certain Asian and African countries where the disease tends to be more florid, than in Britain, North America and the Antipodes where it is usually mild and responsive to treatment.
Treatment. Treatment of spinal tuberculosis is now much more often ambulatory than it was in the past, largely because of the efficacy of antituberculous drugs. Nowadays treatment may entail only a brief stay in hospital – or indeed it may often be carried out entirely on an out-patient basis.
PYOGENIC INFECTION OF THE THORACIC OR LUMBAR SPINE (Pyogenic spondylitis; osteomyelitis of the spined; discitis)
Pathology. Organisms usually reach the spinal column through the general blood stream, from a septic focus elsewhere. Other possible routes are through the spinal venous plexus from a focus in the pelvis, or through lymphatic channels from a neighbouring focus. As in tuberculous spondylitis, there is destruction of an intervertebral disc and erosion of the adjacent bone, with or without abscess formation. The spinal cord may be damaged by pressure, or by thrombosis of its vessels.
Imaging. Radiographs show local rarefaction or erosion of bone, diminution of disc space, and sometimes sub-ligamentous new bone formation. MRI scanning may also reveal the extent of soft tissue and bone involvement by the infective abscess (Fig. 13.16). After healing, spontaneous bony fusion of affected vertebrae is often observed.
Treatment. Appropriate antibacterial drugs are given. The spine is rested, at first in bed, but later with a suitable brace, until healing occurs. An abscess may require early drainage, especially if the spinal cord is threatened.
OSTEOARTHRITIS OF THE THORACIC AND LUMBAR SPINE (Spondylarthritis; spondylarthrosis; spondylosis)
Cause. Predisposing factors are:
Pathology. The changes affect the central intervertebral (body-to-body) joints and the posterior intervertebral (facet) joints. One segment or several segments may be affected. In the central joints, which are affected first, there is degeneration with consequent narrowing of the intervertebral disc, and hypertrophy of bone at the joint margins leads to the formation of osteophytes (Fig. 13.17). In the posterior intervertebral (facet) joints the changes are those of osteoarthritis in any diarthrodial joint – namely, attrition of the articular cartilage and osteophyte formation (spurring) at the joint margins. These changes in the facet joints are probably the more important from a clinical point of view.

Fig. 13.17 Osteoarthritis of the lumbar spine. Marked narrowing of an intervertebral disc, with anterior osteophytes. Note also the slight posterior displacement of the upper vertebra. (See also Fig. 13.23B.)
Secondary effects. Rarely, osteophytes encroach upon an intervertebral foramen sufficiently to interfere with the function of the issuing nerve. Thinning of the articular cartilage of the posterior intervertebral (facet) joints reduces the stability of the affected segment and predisposes to one type of spondylolisthesis p. 242. In severe cases the osteophytes around the facet joints may encroach on the spinal canal resulting in the syndrome of spinal stenosis p. 245.
Clinical features. Spinal osteoarthritis can exist in quite marked degree without causing symptoms. But there is often a complaint of aching pain in the affected area, worse on activity or after prolonged standing or sitting in one position, and especially after stooping or lifting. Pain is often worse first thing in the morning, and there may be a feeling of stiffness when rising from a sitting position. In the lumbar region there is a tendency to acute exacerbations of pain, usually arising suddenly and lasting a few weeks. These are possibly explained by strain or momentary subluxation of an unstable degenerate joint. Interference with a nerve in a narrowed intervertebral foramen leads to radiating pain in the distribution of the affected nerve (girdle pain or sciatica according to the level affected).
Radiographic features. The changes are most obvious in the central (body-to-body) intervertebral joints, which show narrowing of the intervertebral space and osteophyte formation (spurring) at the joint margins (Fig. 13.17). Later the posterior intervertebral (facet) joints also show changes: there is narrowing of the joint space with sharpening of the margins of the facets. These changes are seen clearly only in oblique projections or on CT scans.
Diagnosis. Osteoarthritis has to be distinguished from other causes of back pain and from other causes of radiating nerve pain (girdle pain or sciatica) (see Fig. 13.29, p. 240). It should be remembered that the demonstration of osteoarthritic changes in the radiographs does not necessarily mean that the arthritis is the cause of a patient’s symptoms, for spinal osteoarthritis is common and often painless. The diagnosis is always presumptive rather than proved, and it is justified only when other possible causes have been excluded by careful consideration of the history, clinical examination, and radiographs.
Thoracic spine. In osteoarthritis of the thoracic spine the symptoms are seldom severe, and if treatment is required a course of active spinal exercises to strengthen the posterior muscles is usually sufficient.
ANKYLOSING SPONDYLITIS
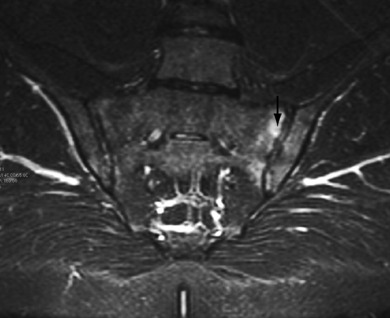
Imaging. Radiographs in the early stage show fuzziness and widening of both the sacro-iliac joints, so that the joint outline is no longer clearly defined (Fig. 13.18). MRI scanning is far more sensitive in detecting these early changes in the sacro-iliac joints (Fig. 13.19). Later, the sacro-iliac joints are completely obliterated and, if the disease progresses, the intervertebral joints in the lumbar, thoracic, and sometimes even the cervical region undergo bony ankylosis, with prominent anterior bridging of the vertebral bodies producing the so-called ‘bamboo spine’ (Fig. 13.20).

Fig. 13.18 AP radiograph of sacroiliac joints. The joints are completely fused showing the typical appearances of advanced sacroiliitis seen in ankylosing spondylitis.
Diagnosis. In the early stages ankylosing spondylitis has to be distinguished from other causes of back pain and sciatica (see Fig. 13.29, p. 240). The marked limitation of spinal movement, the reduced chest expansion, the typical radiographic features, and the raised erythrocyte sedimentation rate are diagnostic.
Course and complications. The disease usually ceases to progress after ten or fifteen years, leaving permanent stiffness, the extent of which varies widely from case to case. Complications include fixed flexion deformity of the spine (Fig. 13.21A), intercurrent respiratory infections, and iridocyclitis, which in severe cases may lead to blindness. There is also a relationship with Crohn’s disease (regional ileitis), which may co-exist.
If a severe flexion deformity of the spine occurs through neglect of these precautions it can result in severe functional disability. This is particularly the case when the hips are involved and develop flexion contractures in addition to the spinal deformity. Relief may be obtained by replacement arthroplasty of both hips to restore an upright stance. In a few patients where this fails it may be necessary to undertake a corrective wedge osteotomy of the spine in the lumbar region followed by internal fixation (Fig. 13.21). This is high-risk surgery and should only be performed by surgeons experienced in the procedure.
SCHEUERMANN’S KYPHOSIS (Adolescent vertebral osteochondritis; adolescent kyphosis)
Formerly termed osteochondritis, Scheuermann’s disease1 is now regarded as unrelated to osteochondritis juvenilis p. 130 and should no longer be so called. Basically, it seems to be an intrusion of part of the intervertebral disc into the vertebral end plate at multiple levels, mostly in the thoracic region. This leads to a rounded kyphosis. The cause and precise nature of the affection are uncertain. It is uncommon.
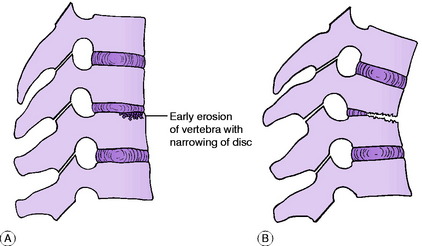
Pathology. The vertebral bodies ossify from three centres – a primary centre for the middle of the body, and secondary centres for the upper and lower surfaces. These secondary centres, known as the ring epiphyses, appear at about the time of puberty in the cartilaginous end plates that separate the vertebral bodies from the adjacent intervertebral discs. In Scheuermann’s disease there is a disturbance of the normal development of the cartilage plates and ring epiphyses, possibly because they are damaged by bursting of the disc contents through the cartilage into the subjacent vertebral body (Fig. 13.22A). The changes occur predominantly near the anterior margins of the vertebrae, where the greatest weight-thrust is borne. In consequence the disc is somewhat narrowed anteriorly, and through deficient growth of the affected part of the ring epiphysis the vertebral body becomes slightly wedge-shaped (Fig. 13.22B). The deformity predisposes to the later development of osteoarthritis.
Clinical features. The patient is usually 13 to 16 years old, and more often a boy than a girl. In the active stage there is pain in the thoracic spine, with ‘round’ back. After some months the pain subsides, leaving a rounded kyphosis of varying severity (Fig. 13.23A). In later life there may be renewed pain from the development of osteoarthritis. On examination there is a slight or moderate rounded kyphosis in the thoracic region. In the active stage there is tenderness on firm palpation over the affected vertebrae.
Radiographic features. In the active stage of the disease the affected vertebral bodies show deep notched defects at their anterior corners, and the corresponding parts of the ring epiphyses may be irregular in shape and size (Fig. 13.23B). The disc spaces are slightly narrowed but never totally destroyed. After healing, there is slight antero-posterior wedging of the affected vertebral bodies. Years later, osteoarthritic spurring of the anterior vertebral margins is observed, probably as a result of the vertebral malalignment (Fig. 13.23B).
Treatment. In a mild case treatment is often unnecessary. If pain is troublesome, support for the spine in extension, by a brace or plaster jacket, may be advisable. Bracing may have to be continued for up to six months, according to progress. Meanwhile active exercises to strengthen the posterior spinal muscles are encouraged. In the worst cases – a small minority – operative correction may be considered. Operation entails excision of intervertebral discs, with interbody grafting, in the affected region of the spine, and it usually entails posterior instrumentation to provide correction and stability. It is a major procedure and clearly must not be undertaken without very careful assessment of every facet of the problem, since at best only 40% of the deformity can be corrected.
CALVÉ’S1 VERTEBRAL COMPRESSION (Vertebra plana; vertebral osteochondritis)
Pathology. From its radiological features and benign course, Calvé’s disease was regarded as an osteochondritis. Histological studies have shown that the majority of cases are in fact caused by an eosinophilic granuloma p. 72.
Radiographic features. Radiographs show the characteristic extreme flattening of the affected vertebral body, which appears greatly increased in density (Fig. 13.24): it has been likened to a coin seen end on.
Treatment. Calvé’s disease is non-progressive, and in practice treatment is required only for as long as the symptoms last. If pain is severe the child should be kept recumbent in bed, but in most cases he may safely resume an active life without external support within a few weeks.
PROLAPSED LUMBAR INTERVERTEBRAL DISC
Pathology. The discs between L5 and S1 and between L4 and L5 are those most often affected. Part of the gelatinous nucleus pulposus protrudes through a rent in the annulus fibrosus at its weakest part, which is postero-lateral (Figs 13.25 and 13.26); or sometimes the torn annulus itself protrudes backwards. If it is small, the protrusion bulges the pain-sensitive posterior longitudinal ligament, causing pain in the back. If it is large, the protrusion herniates through the posterior ligament and may impinge upon an issuing nerve to cause sciatic pain. The nerve affected is that which leaves the spinal canal at the interspace next below the site of the disc lesion. Thus the first sacral nerve is impinged upon by a prolapse between L5 and S1, the fifth lumbar nerve by a prolapse between L4 and L5, and so on. Natural healing is by shrinkage and fibrosis of the extruded disc material; not by its reposition within the disc.
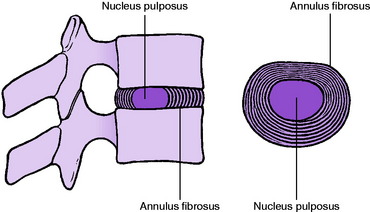
Fig. 13.25 A normal intervertebral disc seen in sagittal section (left) and in horizontal section (right).
Clinical features. In a typical case of disc prolapse at the L4–L5 or L5–S1 level the clinical picture is clearly defined. The patient is aged between 18 and 60. A few hours or days after jarring or straining the back he or she is seized, while twisting, stooping, or coughing, with agonising pain in the lumbar region. Any movement of the back is impossible. The acute pain gradually lessens in severity, but after a few days a radiating pain is felt in one or other buttock and down the back or side of the thigh to the calf and foot. Tingling or numbness is felt in the calf or foot. The pain is aggravated by coughing or sneezing.
On examination the patient with a fully developed acute attack stands either with a lumbar scoliosis (sciatic scoliosis) (Fig. 13.27) or with the normal anterior lumbar curve obliterated. Forward flexion is greatly restricted, as also may be extension. Lateral flexion, on the other hand, is usually free and painless – certainly to one side if not to both. Straight leg raising is restricted on the affected side, usually markedly – an important clinical sign. Careful tests may reveal slight muscle wasting or weakness in the distribution of the affected nerve, and the corresponding tendon jerk (knee jerk in L3–L4 lesions; ankle jerk in L5–S1 lesions) is impaired or absent.
In a severe case in which the prolapse is almost central there may be pressure upon the cauda equina, with consequent loss of bladder sensibility and retention of urine. This is the dangerous cauda equina syndrome, which must be regarded as an acute surgical emergency, for in the absence of immediate effective treatment serious permanent disability is likely to ensue (see below, p. 241).
Imaging. Radiographic features. In a case of acute prolapsed disc plain radiographs do not show any abnormality, and the purpose of radiography is mainly to exclude other causes of back pain and sciatica. It is only when a disc has been deranged for many months or years that appreciable narrowing of the disc space and spurring of the joint margins, denoting secondary degenerative arthritis (osteoarthritis), are observed.
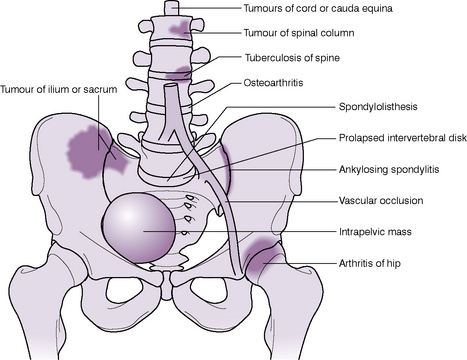
Magnetic resonance imaging (MRI scanning) can show the intervertebral disc substance and the nerve roots: the bulging disc material can thus be visualised directly, particularly on sagittal projection (Fig. 13.28). Discography has only an occasional place as a diagnostic tool to confirm the level of symptomatic disc disease.
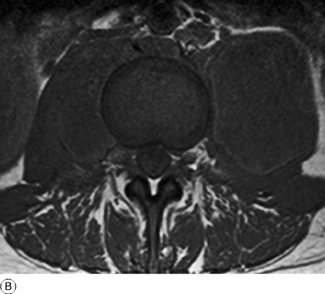
Diagnosis. Prolapsed intervertebral disc must be differentiated from other causes of pain in the back or leg (Fig. 13.29). A dramatically sudden onset is always suggestive of a mechanical derangement and especially of a prolapsed disc, whereas pain that increases relentlessly without intermission suggests a progressive lesion, inflammatory or neoplastic. Although the clinical features are often highly suggestive, definitive diagnosis rests upon appropriate imaging, preferably by magnetic resonance scans.
Treatment. Conservative treatment is successful in relieving the symptoms in a high proportion of cases – probably at least nine out of ten, though most of this improvement may be the result of natural healing. Prolonged bed rest, other than for a few days when symptoms are most acute, should be avoided. The patient should be encouraged to mobilise but the lumbar spine may be supported with a moulded plastic jacket or a well-fitted spinal orthosis (Fig. 13.30). The patient should be encouraged to discard the support as soon as the severe pain has subsided and mobilise the spine with physiotherapy supervision.
Operative treatment. Excision of the displaced disc material, or discectomy, is indicated in the following circumstances:
ACUTE LOW BACK PAIN (LUMBAGO)
The pathogenesis of acute low back pain is not entirely clear. Indeed there may be more than one cause. Probably in many cases the underlying lesion is a prolapsed disc that has not yet been retropulsed far enough to interfere with a nerve root (Fig. 13.26B). It is in these cases that sciatica may develop later, as the size of the prolapse increases. But other examples of acute back pain are more convincingly ascribed to some other mechanical fault, such as sudden nipping of synovial membrane in one of the facet joints, or momentary subluxation at an intervertebral joint that is unstable on account of disc degeneration or degenerative arthritis. Nerve irritation may also be the result of leakage of inflammatory cytokines from the degenerative lumbar disc. In most cases acute attacks of pain may recur at intervals of months or years, with intervals of relative freedom between the attacks.
SPONDYLOLYSIS
In spondylolysis there is a defect in the neural arch of the fifth (rarely the fourth) lumbar vertebra. There is loss of bony continuity between the superior and the inferior articular processes, the deficiency being bridged by fibrous tissue (Fig. 13.31). If this stretches or gives way, the consequent vertebral displacement constitutes one variety of spondylolisthesis (see below).
Treatment. This is often unnecessary. Aching may be relieved by a surgical corset or belt. If pain is unusually troublesome an attempt may be made to close the defect in the pars interarticularis on each side by transfixing it with a screw and laying in slender bone grafts; or alternatively, local fusion of the spine may be undertaken (see p. 245).
SPONDYLOLISTHESIS (Lumbar spondylolisthesis)
Cause. There are three predisposing factors leading to spondylolisthesis of three distinct types:
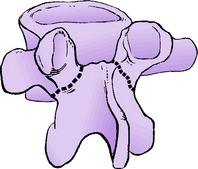
In the first type of spondylolisthesis, the least common, there is a congenital basis for the displacement. The posterior intervertebral joints are unstable because the articular processes are congenitally malformed or even rudimentary: thus they form no bar to forward displacement of the spinal column (Fig. 13.32). This defect occurs most often at the lumbo-sacral joint. Displacement may be severe and, since the whole vertebra is displaced complete with its neural arch, the cauda equina may be trapped, with consequent severe neurological disturbance (Fig. 13.32).
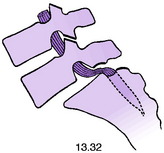
In the second type, which is the best recognised, a defect in the neural arch of a vertebra allows separation of its two halves (see spondylolysis, and Fig. 13.33). The body, with the pedicles and superior articular processes (and the whole of the spinal column above it), slips forwards, leaving behind the laminae and inferior articular processes (Fig. 13.33). The fifth lumbar is the vertebra usually affected, the fourth occasionally. Displacement may gradually increase, especially during adolescence, and it sometimes reaches a severe degree. There may be minor irritation of one of the issuing nerves, with consequent sciatica; but despite severe bony displacement serious interference with the nerves of the cauda equina is exceptional in this type of spondylolisthesis.
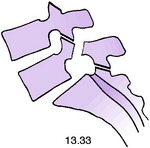
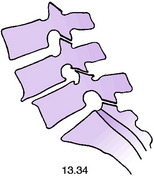
In the third type of spondylolisthesis (sometimes termed pseudospondylolisthesis), seen fairly commonly, the arthritic posterior intervertebral facet joints become unstable with degeneration of the articular cartilage and osteophyte formation displacing the joint surfaces (Fig. 13.34). It may occur at any level in the lumbar spine—most commonly between the fourth and fifth lumbar vertebrae. In this type the vertebral displacement is occasionally backwards rather than forwards (see Fig. 13.17), but in either case displacement is never severe, and neurological disturbance is unusual.
Clinical features. The clinical features of spondylolisthesis are inconstant: they depend to some extent upon the nature of the causative lesion and upon the degree of displacement. Thus in spondylolisthesis from under-development of the articular processes (Fig. 13.32), and in that from a defect of the pars interarticularis (Fig. 13.33), the patient is usually a young adult, whereas displacement from degeneration of the facet joints in osteoarthritis (Fig. 13.34) is seen characteristically in patients beyond middle age. In some cases the deformity is entirely symptomless. When symptoms occur they take the form of chronic backache, with or without sciatica. The back pain is worse on standing.
On examination there is often a visible or palpable ‘step’ above the sacral crest, due to the forward displacement of the spinal column; but this is obvious only when the displacement is severe. Spinal movements are restricted only slightly, if at all. Abdomen: When displacement is severe the spinal column is projected forwards and the lumbar vertebral bodies may be palpable through the abdominal wall. Lower limbs: Minor irritation of a sciatic root is often evidenced by impairment of straight leg raising; but severe neurological disturbance is seldom observed except in the rare cases in which congenital malformation of the articular processes allows dislocation of the whole vertebra complete with its neural arch (Fig. 13.32).
Radiographic features. Lateral and oblique views will sometimes demonstrate a defect of the neural arch (Fig. 13.35), but CT scans will show this more clearly (Fig. 13.36).
Treatment. When spondylolisthesis is symptomless treatment is not required.
SPINAL STENOSIS (Claudication of the cauda equina)
Examination may reveal little abnormality, though frequently there are features to suggest degenerative change in the lumbar spine – for instance impairment of spinal mobility.
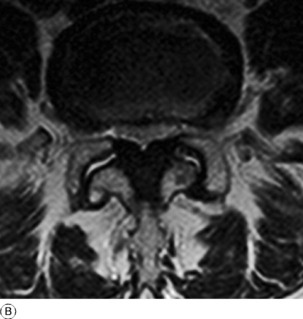
Imaging. Plain radiographs may give the impression that the spinal canal is narrower than usual and they may show further constriction of the canal by posterior osteophytes upon the margins of the vertebral bodies or in relation to the facet joints. Magnetic resonance imaging (MRI) shows very clearly the shape of the spinal canal, and may also show bony or soft-tissue outgrowths encroaching upon either a normal or a congenitally constricted canal (Fig. 13.37).
Treatment. Mild symptoms may be controlled by appropriate modification of activities – for instance by using a bicycle instead of walking, and by the avoidance of prolonged standing. In the fully established case with severe intractable symptoms, treatment should be by operation to decompress the spinal canal by removal of intruding osteophytes and enlargement of the lateral recesses at the level of the constriction. Decompression may have to be carried out over a number of segments, depending upon the longitudinal extent of the constriction as shown by appropriate imaging.
TUMOURS OF THE TRUNK AND SPINE
TUMOURS IN RELATION TO THE SPINAL COLUMN, SPINAL CORD, OR EMERGING NERVES
Local destruction of the skeleton. The commonest cause is a malignant tumour of the bones of the spinal column (Fig. 13.38) – usually a metastatic carcinoma. The predominant symptom is pain, which is constant and increases relentlessly in its severity. Frequently there are associated neurological manifestations from involvement of the spinal cord or nerve roots. Sometimes deformity, from collapse of the bony structure, is evident clinically; or there may be marked restriction of spinal movement, with protective muscle spasm.
Interference with peripheral nerves. Peripheral nerves – especially the nerves of the cauda equina – may be involved by tumours of the nerves themselves (neurofibroma), by tumours of the spinal column (benign or malignant), or by tumours in the peripheral course of the nerves (for example, a tumour of a rib, or a tumour arising from or within the pelvis). The clinical features depend upon the particular nerve or nerves affected and upon the extent of the involvement. Typically, there will be constant, progressive, and ultimately severe pain along the course of the affected nerve, with sensory impairment, increasing motor weakness, and depression of reflexes in the distribution of the nerve. Retention of urine is usually a prominent feature of a tumour interfering with the cauda equina.
Imaging. Plain radiographs will usually help in discovering a tumour arising in the bones of the spinal column (Fig. 13.38), or eroding the bone from outside. In cases of vertebral destruction by a tumour the adjacent intervertebral discs are typically preserved. This point helps in the distinction from erosion and collapse due to infection, in which the discs are destroyed at an early stage (compare Figs 13.13A and 13.38).
Radiographs of the chest may reveal a primary lung tumour or a metastasis; and radiographs of the rest of the skeleton may be helpful in the diagnosis of disseminated tumours. Magnetic resonance imaging is indispensable in showing the full extent of the tumour and the extent to which the adjacent tissues have been infiltrated (Fig. 13.39).
Diagnosis. The possibility of a tumour has to be borne in mind constantly in the differential diagnosis of back pain and lower limb pain, especially when associated with radiological signs of vertebral erosion or collapse or with neurological disturbance affecting the trunk, lower limbs, or viscera (Fig. 13.29).
Treatment. This is dependent on the site and nature of the tumour, but it should be remembered that many of these patients will survive for a considerable period of time and may require more active treatment than analgesic therapy alone for their increasing pain. Radiotherapy to the bone lesions and sometimes operative spinal decompression and fusion may be required in selected cases.
OTHER TUMOURS OF THE TRUNK
Tumours of the scapula
The commonest tumour of the scapula is a chondroma. It grows outwards from the flat body of the bone and is therefore classed as an ecchondroma. It may attain a large size. Although it is often benign at first, there is a risk of malignant change, with the development of a chondrosarcoma. For that reason a chondroma that appears to be enlarging should always be excised with an adequate margin of healthy bone. A large part of the scapula can be removed without causing serious disability.
CHRONIC LOWER LUMBAR LIGAMENTOUS STRAIN (Postural back pain)
COCCYDYNIA
Cause. Typically coccydynia develops after an injury – usually a fall on the ‘tail’. Occasionally a history of injury is lacking.
OSTEOPOROSIS
The vertebrae of the thoracic and lumbar spine are one of the commonest sites affected by osteoporosis, or so-called ‘brittle bone’ disease. This is a general affection of the skeleton and is described in more detail on page 81. It is commonest in postmenopausal women, but it can also affect men in the same age group. Its onset is insidious, but crush fracture of the vertebral body is the commonest of the fragility fractures associated with this condition. Its onset may be associated with an episode of minor trauma, but there is often no significant injury and only minor local pain. More commonly, the patient presents with progressive loss of height and an increasing kyphotic deformity of the thoracic spine. This results from collapse of the thoracic vertebrae at several levels with anterior wedging of the bodies (Fig. 13.40). In advanced cases the radiographs show little difference between the density of the bone and the intervertebral discs.
Disorders of the sacro-iliac joint
Sacro-iliac lesions are a rather uncommon but nervertheless important cause of back symptoms or of referred pain in the lower limb. Of the various types of arthritis, ankylosing spondylitis is the best recognised. Tuberculous arthritis is seen occasionally, but mainly in developing countries.
EXTRINSIC DISORDERS SIMULATING SPINAL DISEASE
LOWER LIMB DISORDERS
Pain from an arthritic hip may sometimes simulate sciatic pain from a spinal lesion, but characteristically is referred from the groin down to the front of the thigh rather than on its posterior aspect. A full examination of the hip and if necessary radiology should establish the true diagnosis.
1 Percivall Pott (1714–1788) London surgeon who worked at St. Bartholomew’s Hospital and described the paraplegia from spinal disease in 1779 as well as the ankle fracture that bears his name.
1 Holger Scheuermann (1877–1960) a famous Danish radiologist who worked at the Cripples Hospital in Copenhagen and described the deformity and its cause in 1921.
1 Jacques Calvé (1875–1954) French orthopaedic surgeon; worked in TB Hospital at Berck Plage and described the vertebral condition thought to be an osteochondritis, in 1925.