CHAPTER 54 Treatment of Ununited Fractures of the Distal Radius
Rationale
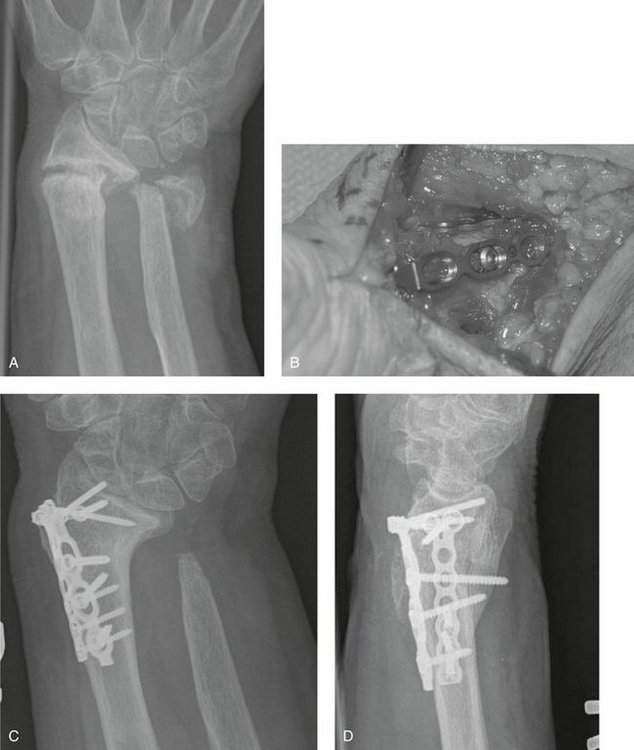
Nonunion of the distal radius—long considered to be extremely rare1,2—has been noted more frequently in recent years.3–7 Although some authors have speculated that the advent of external fixation and other techniques for maintaining the length of the radius has created bony defects that can lead to nonunion,7 nonunion also is seen after internal fixation or nonoperative treatment (Figs. 54-1 through 54-3).3–7 There seems to be an association with concomitant fracture or dislocation of the distal ulna (see Fig. 54-2).4,5
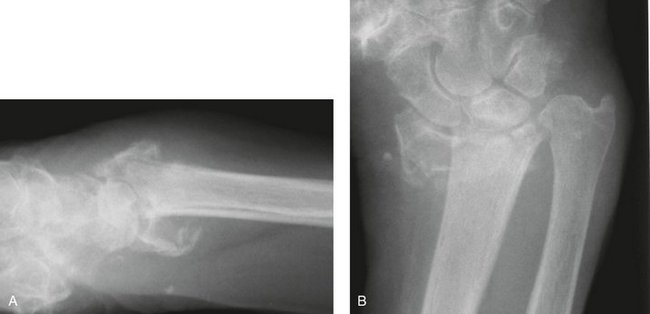
Although the cause and incidence of nonunion of the distal radius are uncertain, the need for operative treatment is clear. Most nonunions are synovial.4–7 The wrist is usually deformed, unstable, and painful. Some patients have a severe radial deviation deformity reminiscent of congenital clubhand, which has been referred to as acquired or post-traumatic clubhand (Fig. 54-4).8,9
Operative treatment can improve upper limb function in patients with nonunion of the distal radius by either fusing the wrist or healing the fracture. Improved implants and operative techniques have improved healing of the fracture, preserving some wrist motion.5,6 Even small amounts of wrist motion can enhance upper limb function.10
Operative Techniques
Treatment Options
The most common treatment of ununited fractures of the distal radius has been wrist arthrodesis,4,7 probably because attempts at internal fixation of the small, metaphyseal distal radius fragment seem risky. The appeal of retaining some wrist motion along with the development of better implants and techniques for the fixation of small articular fractures has influenced us to offer our patients an attempt to heal the fracture with internal fixation and autogenous cancellous bone grafting.5,6
Two principles have proved useful. First, the concept of applying two plates in orthogonal planes—as practiced at other anatomical sites, such as the distal humerus,11 and as supported by mechanical principles—is particularly useful in the distal radius, where the distal fragment can be very small.5 A second, orthogonal plate provides a greater number of fixation points in the distal fragment. Second, the use of fixed-angle devices instead of standard screws for osteoporotic bone—also used in the humerus12—can provide more secure fixation of bone in which preexisting osteoporosis has often been exacerbated by disuse of the limb.13
Wrist arthrodesis may be optimal in infirm patients and patients with limited functional demands in whom pain relief is the primary goal, and as a salvage of failed attempts to gain union. Some nonunions, in particular complex articular nonunions, are not amenable to operative fixation, and wrist fusion is the only option (see Fig. 54-3). Some authors have suggested that when there is less than 6 mm of bone between the lunate facet of the distal radius articular surface and the fracture site, there is insufficient bone to support internal fixation.7 I believe that although this increases the challenge of internal fixation, there is usually a larger amount of bone in the radial styloid portion of the distal fragment that can accept internal fixation (see Fig. 54-2).
Wrist Arthrodesis
Standard wrist arthrodesis techniques using specific wrist fusion plates14 have proved adequate for ununited fractures of the distal radius.4,7 In this situation, the nonunion represents another “articulation,” which must be débrided, bone grafted, and stabilized with the plate. Bone graft can be obtained from the resected ulna when a concomitant Darrach procedure is performed, from the radial styloid, or from the iliac crest (see Fig. 54-2).
Open Reduction and Internal Fixation
A volar Henry15 exposure provides access to the volar and radial aspects of the distal radius. The fracture site is identified, and fibrous or synovial tissues are removed. The sclerotic fracture ends are opened with rongeurs and curets and drilled repeatedly with a small bit to open the intramedullary canal. Opening of the sclerotic fracture ends and intramedullary canal facilitates the ingress of a vascular supply providing cells, nutrients, and growth factors to support healing.
To facilitate and stabilize reduction, a small skeletal distractor or other external fixator can be applied between two 2.5-mm Schantz screws, one placed in the distal fragment and one in the proximal fragment. The Schantz screws are placed so that distraction between them realigns the fragments, but the screws themselves do not interfere with internal fixation devices. In patients with a severe radial deviation deformity, consideration is given to releasing or Z-lengthening the brachioradialis and flexor carpi radialis tendons to facilitate realignment of the distal radius, but this is rarely necessary if the decision has been made to accept the shortening of the radius and resect the distal ulna.
With the skeletal distractor holding the fragments reduced—sometimes with an ancillary Kirschner wire transfixing the fragments—the plates and screws are applied. A variety of volar plates with fixed-angle (locked) screws are now available. The fixed-angle screws or pins are better suited to fixation of the metaphyseal bone of the distal radius, which is often osteopenic. In some patients with very small distal fragments, it can be useful to enhance the fixation in the more substantial radial styloid portion of the distal fragment by applying a second plate, orthogonal to the volar plate on the direct radial surface of the distal radius. Several implants are designed for placement on this part of the bone, many with locking screws. Autogenous cancellous bone graft is applied to the defect, and the wound is closed.
Complications
We have not encountered infection, wound problems, or nerve injury.5,6 If the fracture fails to heal, the implants eventually loosen or break, and the decision to undertake further attempts to heal the fracture or to salvage the situation with wrist arthrodesis is based on the specific circumstances and the desires of the patient. Wrist motion is never returned to normal, and some patients regain very little wrist motion. Progressive arthrosis also can compromise the result and may require subsequent wrist arthrodesis in rare cases. The implants often irritate the overlying tendons and can lead to tendon rupture. I have a low threshold for recommending implant removal when implants are associated with pain, swelling, or crepitance of the tendons over the plate.
Results
Segalman and Clark7 reported on 12 nonunions of the distal radius treated over a 24-year period at the Curtis Hand Center. This report is testament to the relative rarity of the problem. Also, the findings should be interpreted in the context of the older treatment methods available at the time many of the patients were managed. Segalman and Clark7 divided the nonunions into two groups:
In contrast, Prommersberger and colleagues6 supported attempts at gaining fracture healing in all patients in their report of a multicenter retrospective series of 23 patients, including 13 patients with an ununited fracture of the distal radius in whom the distal fragment had more than 5 mm of subchondral bone supporting the articular surface distal to the site of the nonunion and 10 patients with an ununited fracture of the distal radius with a smaller distal fragment. Bony union was achieved in 22 of 23 patients, an average of greater than 80 degrees of wrist flexion arc was maintained, and grip strength averaged greater than 59% of the opposite arm. One patient in the large fragment group failed to heal the fracture and had wrist arthrodesis. There were no significant differences in the radiological and clinical outcome between the two groups. These findings may reflect what is possible with newer implants and techniques.
1. Watson-Jones R. Fractures and Other Bone and Joint Injuries, 2nd ed. Edinburgh: Livingstone; 1942.
2. Bacorn RW, Kurtzke JF. A study of two thousand cases from the New York State Workmen’s Compensation Board. J Bone Joint Surg Am. 1953;38:643-658.
3. Harper WM, Jones JM. Non-union of Colles’ fracture: report of two cases. J Hand Surg [Br]. 1990;15:121-123.
4. McKee MD, Waddell JP, Yoo D, et al. Nonunion of distal radial fractures associated with distal ulnar shaft fractures: a report of four cases. J Orthop Trauma. 1997;11:49-53.
5. Fernandez DL, Ring D, Jupiter JB. Surgical management of delayed union and nonunion of distal radius fractures. J Hand Surg [Am]. 2001;26:201-209.
6. Prommersberger KJ, Fernandez DL, Ring D, et al. Open reduction and internal fixation of un-united fractures of the distal radius: does the size of the distal fragment affect the result? Chir Main. 2002;21:113-123.
7. Segalman KA, Clark GL. Un-united fractures of the distal radius: a report of 12 cases. J Hand Surg [Am]. 1998;23:914-919.
8. Netrawichien P. Radial clubhand-like deformity resulting from osteomyelitis of the distal radius. J Pediatr Orthop. 1995;15:157-160.
9. Ono CM, Albertson KS, Reinker KA, et al. Acquired radial clubhand deformity due to osteomyelitis. J Pediatr Orthop. 1995;15:161-168.
10. Adams BD, Grosland NM, Murphy DM, et al. Impact of impaired wrist motion on hand and upper-extremity performance. J Hand Surg [Am]. 2003;28:898-903.
11. Helfet DL, Hotchkiss RN. Internal fixation of the distal humerus: a biomechanical comparison of methods. J Orthop Trauma. 1990;4:260-264.
12. Ring D, Perey B, Jupiter JB. The functional outcome of the operative treatment of ununited fractures of the humeral diaphysis in elderly patients. J Bone Joint Surg Am. 1999;81:177-189.
13. Perren SM. Evolution of the internal fixation of long bone fractures: the scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093-1110.
14. Hastings H, Weiss AP, Quenzer D, et al. Arthrodesis of the wrist for post-traumatic disorders. J Bone Joint Surg Am. 1996;78:897-902.
15. Henry AK. Extensile Exposure, 2nd ed. Edinburgh: Churchill Livingstone; 1973.