CHAPTER 21 Treatment of the male neck
Anatomy
The preoperative markings
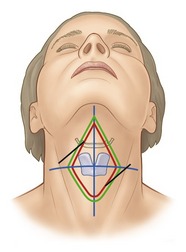
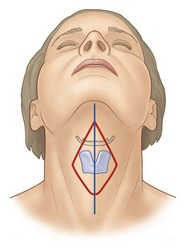
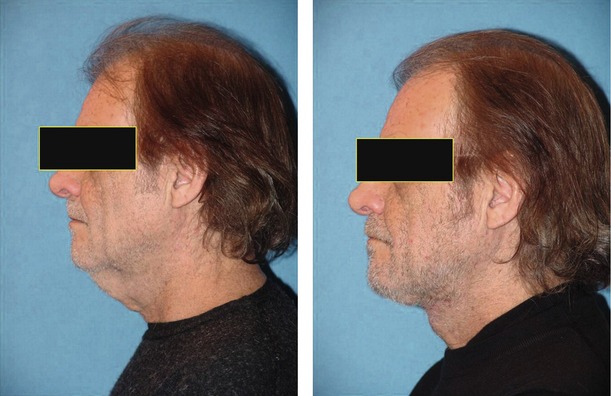
With the patient in the upright position, the redundant skin is grasped with the index finger and thumb. These points are established and two other points are made, one just beneath the angle of the chin and the other in the midline of the neck at the cephalic border thyroid cartilage. These dots are connected with lines to create an ellipse. It is important that the width of this ellipse be slightly less than the skin that was pinched with the index finger and thumb, because the last step of the operation involves the creation of a large Z and it is imperative that this not be so tight as to preclude the rotation of the Z flaps (Fig. 21.1). It is also important that this marking process be carried out with the patient in the upright position, because when the patient assumes the recumbent position these tissues rotate in a cephalad fashion, which would result in a scar below the thyroid cartilage if the marks were made with the patient in this recumbent position. It is the effort of the surgeon to keep the entire scar between the submental crease and the upper level of the thyroid cartilage so as not to be obtrusive.
Technical steps
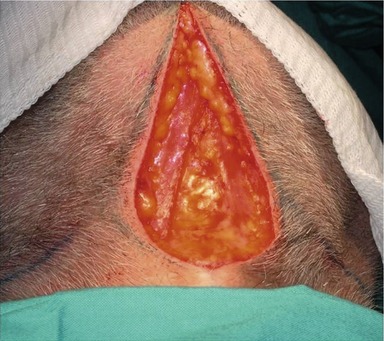
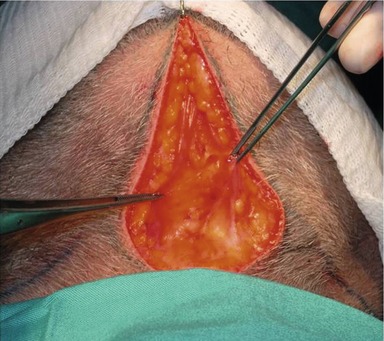
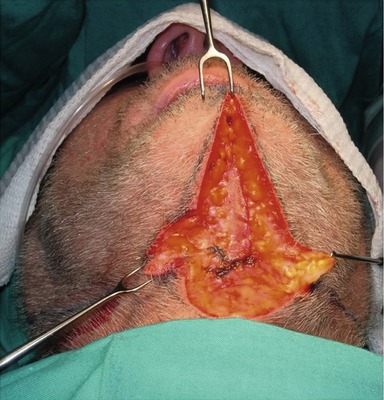
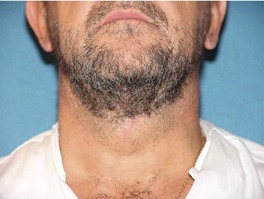
The patient is taken to the operating room and with either general anesthesia or with sedation and local anesthesia, the elliptical excision of the previously marked skin is carried out (Fig. 21.2). This ellipse includes skin and subcutaneous fat. After the ellipse is excised the skin and subcutaneous tissue is undermined laterally to a distance approximating the angle of the mandible. Redundant subcutaneous fat which is preoperatively determined to be obtrusive is excised. Likewise, the subplatysmal fat is evaluated and if it is determined that this fat is obtrusive it is likewise excised, keeping in mind the fact that significant anatomical structures are in this area and dissection carries with it some element of risk. This is determined by the surgeon as to the necessity for excision of subplatysmal fat (Fig. 21.3).
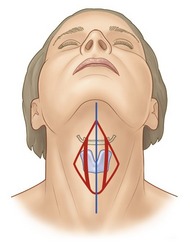
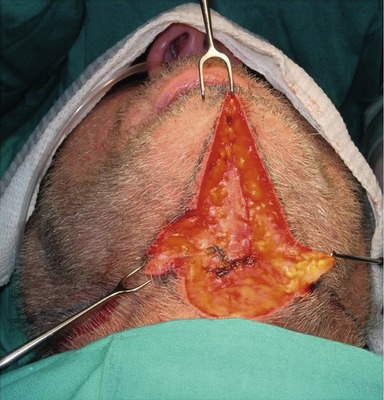
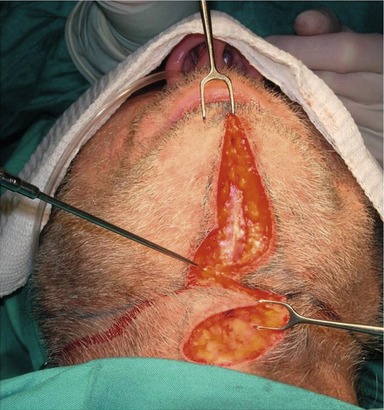
After the skin has been undermined and the redundant fat has been removed, the platysmal flaps are evaluated. The subsequent project is to get the platysmal flaps closed in a tight fashion so as to facilitate the creation of the angle of the neck above the thyroid cartilage. This closure can be carried out in one of three ways. The edges can be sutured side to side or, in the case of a thin platysma with significant redundancy, they can be closed in a vest-over-pants type of procedure. In most instances, however, the preferred method of getting platysmal tightening is with a large Z-plasty in the muscle itself (Figs 21.4 and 21.5). This is designed so as to create the maximal angle just above the thyroid cartilage.
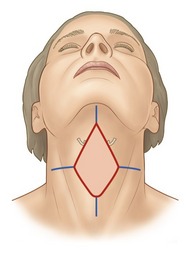
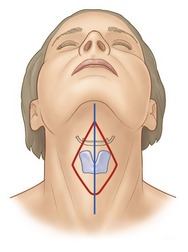
After the platysma has been closed, the elliptical excision is closed in a temporary fashion so as to allow us to determine the location of the Z-plasty to be performed in the skin. The Z-plasty is designed to be the mirror image of the Z-plasty in the platysmal edges (Fig. 21.6). It is imperative that the cross mark of the Z be at the maximal angle that is to be desired, above the thyroid cartilage. Furthermore, the Z is to be made as large as possible so as to interrupt the scar’s extending from the submental angle to the thyroid cartilage. After designing these Zs, and after their incision, they are rotated and sutured with a minimal number of subcutaneous sutures followed by skin closure of the surgeon’s preference (Fig. 21.7).