Treatment of the cervical spine
Treatment of discodural and discoradicular interactions
Manipulation
Controversy
Cervical manipulations can cause severe neurologic complications, which are both exceedingly rare and generally unpredictable.1 More than 200 cases of more or less serious complications after manipulative treatment of the neck have been reported,2 but it is suggested that they are probably under-reported.3,4 Many authors have therefore become very cautious in accepting the suitability of this modality. The main arguments against manipulation are the possible hazards to the vertebrobasilar system and the spinal cord that are usually irreversible.5–10 Therapists who are familiar with manipulative techniques continue to use them because they consider the risks to be minimal. However, such conclusions can only be made after comparative scientific studies have proven that the benefits of manipulation outweigh the risks.
Dangers of manipulation
Treatment decisions cannot be based on effectiveness data alone. Another important factor is safety, obviously. Weighing the risks of spinal manipulation against its benefits is therefore an exercise that should be done constantly. Every act in medicine, whether diagnostic or therapeutic, carries a risk of complications; an injection may result in an anaphylactic reaction, the use of anti-inflammatory agents may cause internal bleeding, and surgical procedures may lead to other, serious complications. It cannot be denied that spinal manipulation too, particularly when performed on the upper spine, is sometimes associated with adverse effects, which are usually mild to moderate. However, serious complications, such as vertebral artery dissection followed by stroke or death, myelopathy and epidural haematoma, have also been described. Mild side effects are very common. Surveys have shown that between one-quarter and one-half of all patients reported at least one post-manipulative reaction. The most common were headache, stiffness, local discomfort and fatigue.11,12 Most of these reactions began within 4 hours and generally disappeared within 24 hours of receiving spinal manipulation.13 The frequency of serious adverse events is difficult to estimate, but according to several publications it varies between 5 strokes/100 000 manipulations to 1.46 serious adverse events/10 000 000 manipulations and 2.68 deaths/10 000 000 manipulations.14–18
The complication that is feared the most is dissection of the vertebral artery, leading to infarction of the brain, cerebellum or brainstem, so-called Wallenberg’s syndrome (see online chapter Headache and vertigo of cervical origin).
Vertebral artery dissection
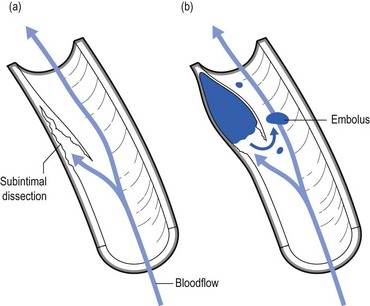
Furthermore, pulsatile pressure damages the muscular layer, resulting in a further splitting or dissection, extending in the direction of blood flow.19 The accrued blood soon develops into a thrombus and deforms the intima, pushing it into the arterial lumen. Blood flow in the cervical arteries can be obstructed either directly by the haematoma or indirectly by the detached emboli that move distally and obstruct the progressively smaller vessels in the brain, resulting in a stroke (Fig. 11.1).20
The cervical arteries are innervated with pain-sensitive nerve fibres that may generate neck pain and headache when provoked. Several studies have shown that pain is typically the first symptom associated with vertebral artery dissection (VAD), and a recent study reported that 8% of the patients presented with head or neck pain as their only symptom.21 Pain related to VAD frequently occurs suddenly and is of severe intensity, involving mostly the ipsilateral occipitocervical area. These symptoms may or may not be followed by ischaemic involvement in the brain, cerebellum or brainstem. The interval of time between the initial pain of VAD and the ischaemic symptoms is quite variable, with reports ranging from almost immediately to several weeks.
Although the pathophysiology of a dissecting vertebral artery is well understood, the underlying cause of intimal tears remains uncertain. Most experts link VAD to trauma of varying degrees of severity and maintain that, because tearing occurs, previous trauma was necessarily involved.22 A retrospective analysis of 80 patients with vertebrobasilar ischaemia determined to be caused by frank neck trauma reported that 70 of the cases were related to motor vehicle accidents.23 However, VADs more commonly occur after very minor trauma and even after everyday activities that most people would consider to be non-traumatic. Examples of such trivial ‘trauma’ include countless everyday activities that involve head and neck movement, such as reversing a vehicle, coughing, vomiting, unusual sleeping positions, having one’s hair washed at a beauty salon, and rhythmic movement of the head and neck to music.24–26 One article listed 68 activities that have been implicated in the development of VAD.27 Another article reviewing 606 cases of VAD reported that 371 or 61% were spontaneous. The remaining 39% were associated with trivial or other trauma, which included manipulation in 9% of the total number of cases.28
So far it remains unclear what the exact precipitating cause of the development of a VAD might be. Given that many VADs are not related to trauma or even abrupt head movements, one must wonder whether a clear cause-and-effect relationship can be established in cases that involve mechanical triggers. It has been suggested that a mechanical trigger is only one of multiple components and that an underlying arterial abnormality is the predisposing factor to dissection.29,30 This opinion is based on several observations: first, many VADs are not related to trauma and simply occur spontaneously; second, VAD patients frequently have coexisting physiological abnormalities, such as hypertension, recent infection, migraine headache and several others; third, the average person is exposed to trivial events involving the neck on a daily basis, yet most people do not develop VAD.
For the individual therapist who wants to exclude potential disasters, it is extremely important to determine the group of patients at risk and the kinds of manœuvre that are dangerous. Judging from the existing literature, it seems that at this time, neither is possible. Cerebrovascular accidents after manipulation appear to be unpredictable and should be considered an inherent, idiosyncratic and rare complication of this treatment approach.31 In a retrospective review, Haldeman and co-workers studied 64 medicolegal cases of stroke associated with cervical spine manipulation. The strokes occurred at any point during the course of treatment. Certain patients reported onset of symptoms immediately after the first treatment, while in others the dissection occurred after multiple manipulations. There was no apparent dose–response relationship to these complications. These strokes were noted following any form of standard cervical manipulation technique including rotation, extension, lateral flexion and non-force and neutral position manipulations. The results of this study suggest that stroke, particularly vertebrobasilar dissection, should be considered a random and unpredictable complication of any neck movement, including cervical manipulation. It may occur at any point in the course of treatment with virtually any method of cervical manipulation. The sudden onset of acute and unusual neck and/or head pain may represent a dissection in progress and be the reason a patient seeks manipulative therapy that then serves as the final insult to the vessel, leading to ischaemia.32 This puts another perspective on the relationship between cervical spinal manipulation and VAD: is VAD caused by the manipulation or is the patient manipulated because of incipient VAD?33
Although the risk of serious complications cannot be denied, it should be put into context. The incidence of VAD in relation to cervical manipulation remains very low. One Canadian survey, for instance, reported 23 cases of VAD after cervical manipulation over a 10-year period, representing a rate of 1/584 638 manipulations.34 Other publications estimate the incidence of VAD to be 1 in a million.35,36 Furthermore, several authors have made a comparison between the occurrence of injury following manipulation and the complications of other treatments for cervical disorders. The incidence of a serious complication such as a gastrointestinal event after the use of non-steroidal anti-inflammatory drugs is 1 in 1000.37 After surgical procedures to the cervical spine, 1.6% of complications occur. These figures can be used to argue that risks from other causes such as drug therapy can be between 100 and 400 times greater than after cervical manipulation.38
Premanipulative testing
During recent decades, tests have been described to detect vertebrobasilar insufficiency in order to identify those patients who may be at risk of serious post-manipulation complications. These tests are based on the assessment that blood flow to the contralateral vertebral artery is decreased when the cervical spine is rotated and extended to one side.39,40 This is because, during rotation, the contralateral vertebral artery slides forwards and down, causing it to narrow. However, in normal individuals, collateral vascular supply by means of the circle of Willis is sufficient to assure blood flow and to prevent symptoms (see online chapter Headache and vertigo of cervical origin).41,42
Mainly under the influence of the Australian Physiotherapy Association, performing a vertebral artery test routinely prior to manipulation has become widely accepted.43–45 It is believed that the test could determine tolerance to cervical extension and rotation or could differentiate between dizziness caused by vertebrobasilar insufficiency and dizziness caused by other conditions, such as benign paroxysmal positional vertigo and inner ear pathology.46,47
Although prudent premanipulative testing seems to reduce the level of risk,48 both its validity and safety have recently been questioned.49 Premanipulative testing should not be considered as the ultimate safety precaution; studies have shown a high likelihood of obtaining false negative results, suggesting that the validity of the test is poor.50–53 Furthermore, it can even be argued that examination procedures are more dangerous than therapeutic manipulation, because the sustained posture required for the test exposes the patient to greater risk than a quick, high-velocity manipulation.54–56
The doctor or physiotherapist who intends to manipulate should always be aware that even tests during examination carry a risk and that there will always be a factor of unpredictability even when all premanipulative tests are negative and even if the patient responded positively to earlier manipulations. Screening for manipulative risks should not rely on the outcome of provocation tests but on the whole clinical picture that emerges after thorough history taking and clinical examination. In this perspective, a recent study that compared the results of a simple questionnaire to a duplex Doppler ultrasound demonstrated excellent sensitivity (1.00) and good specificity (0.78).57 The questionnaire consisted of the following: ‘Do you avoid looking up as if into a high cabinet shelf because doing so causes neurological symptoms such as: visual problems, dizziness, unsteadiness, confusion, headaches and symptoms in the extremities?’ The same question was posed in relation to turning the head to the right and to the left, as if reversing a car. Review of the literature, especially of the many case histories that have been described, also leads to the conclusion that a number of serious complications could have been prevented had practitioners recognized warning signs which should have led them to exclude manipulation.58–60 One review mentions faulty diagnosis, insufficient clinical knowledge or examination, inaccuracy as a result of routine, overconfidence, bad technique and therapeutic obstinacy as the main causes of complications.61
In recent years another view of the relationship between cervical manipulative therapy and VAD has emerged. The relationship was usually seen as simple cause and effect, in which manipulation causes a dissection in certain susceptible individuals. Recent evidence, however, suggests that the relationship is not causal, and that patients with VAD often have initial neck symptoms which cause them to seek care; they then have a stroke some time later, independent of the treatment. This new understanding has shifted the focus for the therapist from one of attempting to ‘screen’ for ‘risk of complication with manipulation’ to one of recognizing the patient who may have a VAD so that early diagnosis and intervention can be pursued.62 Again, this recognition can only be achieved by looking at the complete clinical picture and by following the proper diagnostic procedures (Box 11.1).
Dangers of not manipulating
A posterocentral disc displacement that is left untreated exerts constant pressure against the posterior longitudinal ligament. It may slowly become larger or give rise to an osteophyte in the spinal canal as a consequence of ligamentous traction. When the bulge enlarges it may eventually compress the spinal cord as well as the anterior spinal artery (see p. 165). The symptoms and signs elicited may finally become irreversible. For all these reasons it is unwise to leave an early minor disc displacement unreduced.
Evidence: results
Everyone who undertakes manipulation sees good and sometimes spectacular results in daily practice. This is somewhat in contradiction with the results that often emerge from randomized trials.63,64 The discrepancy is mainly caused by the fact that, in most of the studies, subgroups of patients are not well defined. Prospective randomized trials that take more care with inclusion and exclusion criteria usually result in a stronger trend favouring manipulation. Koes and colleagues, for example, performed a randomized trial on back and neck pain and found promising results for manual therapy and physical therapy in subgroup analyses of patients with neck pain.65,66 Hoving et al conducted a randomized, controlled trial of manipulation, physical therapy, and continued care by a doctor, which confirmed the superiority of manual therapy over physical therapy and continued care.67 Other authors studied the cost-effectiveness of manipulative treatment. The cost-effectiveness ratios and the cost-utility ratios showed that manipulation was less costly and more effective than physiotherapy or general practitioner care. The manual therapy group showed a significantly faster improvement than the others, with a total cost of less than one-third of that of physiotherapy and general practitioner care.68 Other randomized clinical trials in patients with mechanical neck pain confirmed clinically and statistically significant short- and long-term improvements in pain, disability and patient-perceived recovery when treated with manipulation.69–71
Precautions
In orthopaedic medicine the utmost precautions are taken to avoid any possible complication. Therefore the therapist must follow a strict routine (see Box 11.1). First of all, there should be a firm clinical diagnosis, if necessary confirmed with technical investigation. Warning signs and contraindications are heeded. Manipulation is only considered if there is an unambiguous indication for it. Prognosis is determined and, if provisionally positive, manipulation is begun with strict methods. The manipulator will only proceed when sure of personal skill. During each manipulative session, constant reassessment is made and the decision as to whether or not to continue is totally dependent on the response obtained so far.
Proper interpretation of the examination (clinical reasoning)
The results of the examination, both positive and negative, are then interpreted in the light of anatomical reality (see p. 181). Correlation between history and functional examination is sought (inherent likelihoods): does the behaviour of the pain (onset and evolution, referred versus local) and the paraesthesia (development, presence and pattern) match the clinical findings? Examination features are related to possible articular, root or cord origin. Articular signs are mirrored by specific patterns of limitation. Root involvement may be obvious from motor or sensory deficit or disturbances of reflexes. Evidence of cord involvement is revealed by particular patterns of neurological presentation.
Diagnosis: discodural or discoradicular interaction
• The dura mater and/or dural nerve root investment. Multisegmental pain and tenderness show the dura mater to be affected; pure segmental pain points towards the investment of the nerve root. Scapular pain on coughing is considered to be a dural symptom.
• The intervertebral joint. An asymmetrical pattern of pain and/or limitation (‘partial articular pattern’) indicates internal derangement in the intervertebral joint. Other features are pain on movement and/or posture, twinges and, in more acute examples, deviation of the head.
• The nerve root parenchyma. Segmental (dermatomal) paraesthesia may accompany the root pain. Neurological deficit (motor, sensory and reflexes) is often present.
• The spinal cord. Multisegmental paraesthesia in the hands and/or feet is provoked by neck flexion; other signs of motor and/or sensory tract involvement may also be found.
Exclusion of warning signs
During history taking and functional examination, the examiner must remain alert and constantly aware so as not to overlook possible warning signs (Box 11.2). The presence of any one of these red flags indicates a non-mechanical lesion and is an absolute bar to any active treatment. The patient should be referred for further investigations immediately.
Exclusion of contraindications
It is crucial to know when a manipulation is unsafe. In this regard, data collected from history and clinical examination are far more important than the outcome of one or more premanipulative tests (see p. 183). Great caution should therefore be observed in detecting potential contraindications during history taking and functional examination (Box 11.3).
Absolute contraindications
The moment that there is clinical evidence of an upper motor neurone lesion, manipulation must be abandoned. Symptoms are: paraesthesia in the hands and/or the feet influenced by neck flexion.72 Signs are: positive plantar reflex, positive Hoffman sign, spasticity and incoordination.
This condition can lead to ligamentous laxity at the upper cervical joints, which creates an absolute contraindication to manipulation.73 The typical soggy end-feel puts the examiner on his/her guard.74,75
It is unwise to manipulate a patient who is on anticoagulant therapy because of the danger of an intraspinal haematoma.76 Only if the therapy can be stopped for the duration of treatment is manipulation possible.
In the inflammatory stage of ankylosing spondylitis or in the unlikely event of a patient with this disorder developing a disc lesion, manipulation is not at all safe, especially in the cervical spine, where luxations, fractures and cord compression have been described.77,78
Relative contraindications
Posterocentral disc protrusions
Rotation techniques are contraindicated. The larger the protrusion seems to be, the more the manipulator resorts to techniques without articular movement. Techniques are used under considerable traction, the effects of which help to reduce the fragment of disc (see p. 196).
Acute torticollis in patients under 30 years
Muscular guarding renders manipulation under traction in the direction limited by spasm impossible. Because the condition is the result of nuclear prolapse, the very restricted rotation and lateral flexion initially present are increased by gently sustained pressure. Restoration of movement is thus achieved (see p. 196).
Significant deviations of the cervical spine, either in side flexion or in flexion, make manipulation under traction impossible. Before the usual techniques can be used, the manipulator must bring the patient’s head back to the neutral position. This happens after repeated tractions (whether or not with manipulative thrust) in the line of the deformity (see p. 196).
Recognition of a clear indication
It is not enough to have excluded warning signs and contraindications. It is just as important to make sure that a clear indication is present: a posterocentral or posterolateral disc protrusion causing a discodural or discoradicular interaction (Box 11.4).
Posterocentral discodural interaction with unilateral cervicoscapular pain
Acute torticollis with side flexion deformity
A distinction is made between torticollis in the young (under 30 years old), which is usually of the nuclear type, and that in those over the age of 30, who suffer a cartilaginous displacement (see p. 196).
Posterocentral discodural interaction with central neck pain or bilateral cervicoscapular pain
Posterolateral discoradicular interaction with unilateral root pain, without neurological deficit
• When severe scapular pain has remained after the root pain began: usually the scapular pain and the articular signs disappear or considerably diminish when brachial pain occurs. In the rare event that some movements remain limited and cause severe pain in the scapular area, especially at night, one manipulative session may abolish the scapular pain and restore a full painless range of movement. The root pain remains unaltered and continues its spontaneous course (see p. 157).
• When root pain lasts for a considerable period: most root pain progresses to full recovery in the course of 3–4 months – except C8 pain, which may take up to 6 months to recover. Occasionally a patient may be seen with root pain that has lasted longer than 6 months, even up to 1 or 2 years, and investigation has not shown a neuroma or other similar lesion. Manipulation will not immediately influence the root pain; however, a few days after manipulation, the pain starts to diminish and after a second treatment 2 weeks later all symptoms may disappear. This peculiar clinical phenomenon could be explained by the concept that, although manipulation shifts the discal rim back immediately, it takes some time for the swelling and inflammation to abate and thus for pain to diminish.79,80
Prognosis: criteria of reducibility – presence of favourable or unfavourable signs
Before manipulation is decided upon, the chances of success should be assessed by considering the following questions. By answering these four questions one can make a reasonable prognosis for a number of clinical situations (Box 11.5).81
Is the protrusion central, unilateral or bilateral?
A central protrusion with spinal cord compression is potentially dangerous and any sign – positive plantar reflex, spasticity, incoordination, gross weakness – must therefore be considered as an absolute bar to manipulation (see p. 185).
Is the pain influenced by articular movements?
When movements affect scapular pain, this is considered as ‘favourable’ and manipulation has a fair chance of success. Circumstances in which neck movements augment root pain have to be regarded as ‘unfavourable’, as the result of manipulation is usually inferior (see p. 187).
Manipulation technique
General remarks
Position of the assistant
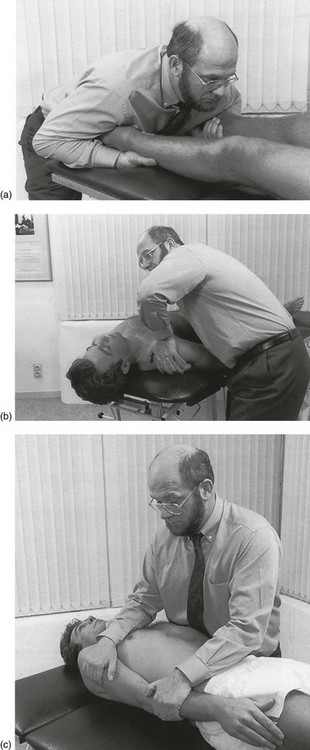
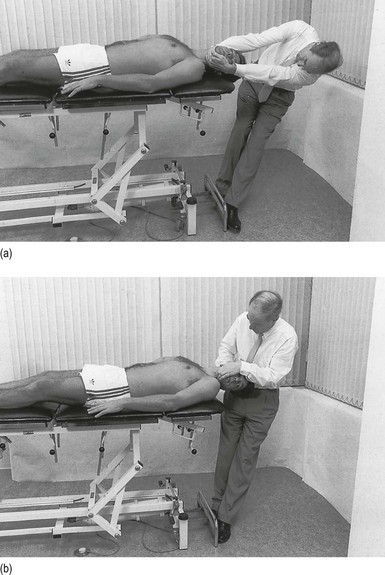
An assistant is needed for fixation. Positions are chosen whereby the patient’s body does not move when traction is applied to the head. There are a number of possibilities (Fig. 11.2).
Position of the manipulator
• Traction induces a subatmospheric pressure in the joint which results in a suction effect – a centripetal force.
• Compression on the pain-sensitive structures exerted by the protruded disc diminishes, with a resulting diminution or even disappearance of the pain. As an additional advantage, the patient will have no problems in relaxing muscles.
• As the muscles are well relaxed, the vertebrae can be distracted by a few millimetres so that the loose fragment has room to move.
• The facet joints are disengaged, which again makes movement easier.
• The posterior longitudinal ligament is taut and helps to exert a centripetal force on the disc.
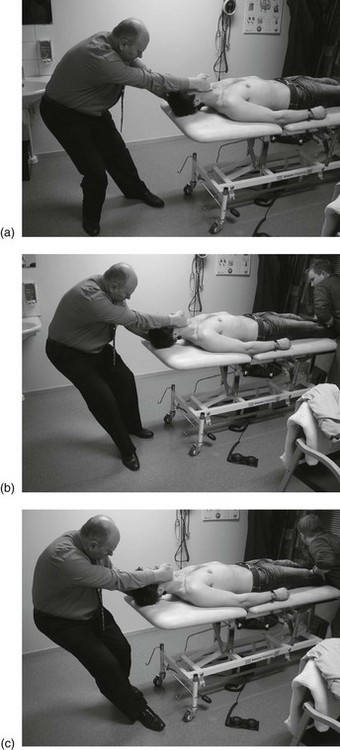
In order to become accustomed to how to apply traction, novices are advised in the beginning to put one foot further back. The traction force will be less. The foot is then gradually brought forwards until it reaches the couch (Fig. 11.3). The further the foot is brought forwards, the more traction is applied.
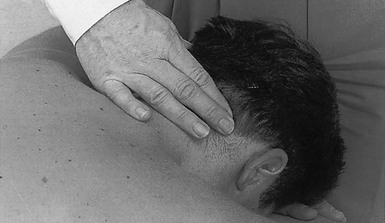
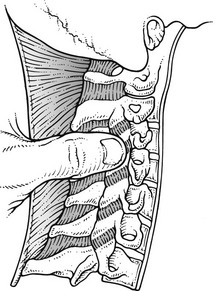
Preparative massage to splenius and semispinalis capitis muscles at their mid-cervical extent
The patient lies prone and the therapist stands level with the patient’s head at the contralateral side. The fingers are placed on the affected area while the thumb supplies counterpressure at the ipsilateral side of the neck (Fig. 11.4). Massage is imparted for 10 minutes by alternately flexing and extending the wrist, thus moving the fingers over the muscles.
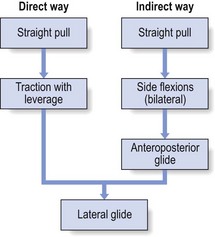
Techniques
Circumduction during traction
The patient lies supine on the couch, an assistant holding the feet.
During the manœuvre some ‘cracks’ may be felt. After a few movements traction is released.
Straight pull
The patient and assistant adopt the same position as for circumduction during traction. The manipulator hooks one hand under the patient’s mandible and the other under the occiput, puts his feet against the couch and leans well backwards. The elbows are straightened as far as possible (Fig. 11.5).
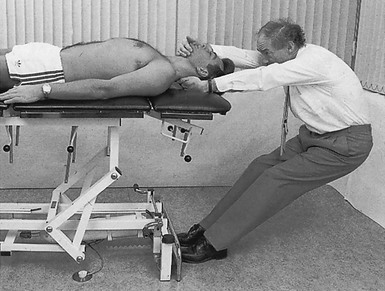
Fig 11.5 Straight pull.
Rotation during traction
The patient and assistant take up the same position as described for the previous two manœuvres. The manipulator takes hold of the patient’s head, places his feet against the couch and leans backwards to take up the slack (Fig. 11.6a). For a rotation to the right, the manipulator’s right hand is at the patient’s chin and the feet point in the same direction. The head is now slowly rotated to the right. This is not done with a hand movement but is the result of the manipulator side-flexing his trunk. The head is turned to half-range on the first occasion, then two-thirds and finally to the end of range. The degree of rotation depends on the response obtained from the patient, which is reassessed after each manœuvre. At full range the end-feel should be assessed and, when this is right, the impulse is given: a quick movement over a very small amplitude (1–2° only). In contrast to the previous trunk movement, this final thrust is performed with the hands only. The head is then brought back to the neutral position and traction is released.
Full rotation during traction
When repetition of the previous manipulation ceases to afford any benefit, this technique may follow. The traction force will be somewhat less but it will be easier to achieve full rotation (Fig. 11.6b).
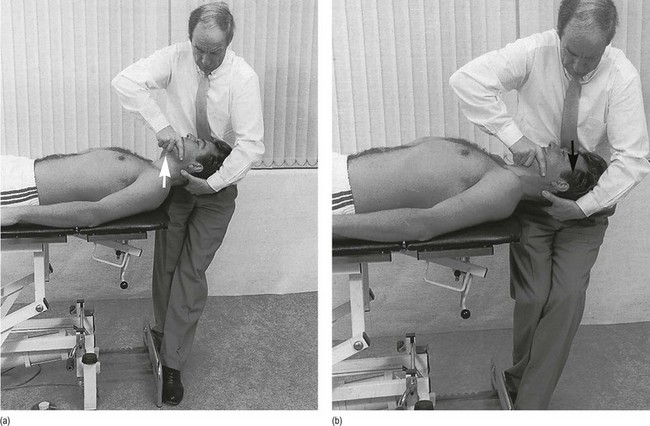
Side flexion during traction
The patient lies supine on the couch. The assistant stands level with the patient’s shoulder on the painful side to apply counter-traction (Fig. 11.7) (see p. 189).
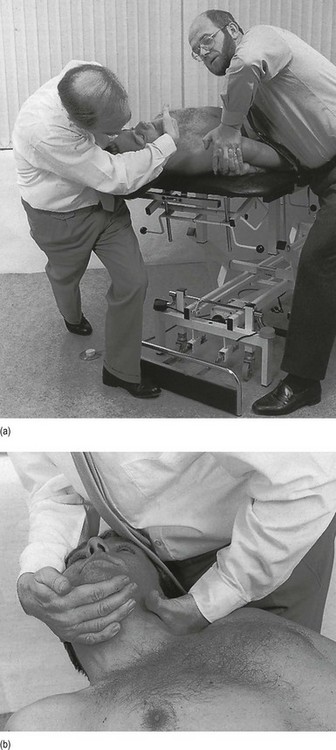
Fig 11.7 (a) Side flexion during traction. (b) Position of the hands for the side flexion technique.
The manipulator puts one hand under the patient’s occiput. The second metacarpophalangeal joint is applied against the posterior aspect of a facet joint at the mid-cervical area. The thumb is kept in extension to avoid pressure on the external carotid artery and the third, fourth and fifth fingers support the head. The other hand is hooked under the mandible in such a way that the forearm comes to lie anteriorly to the ear. The head will thus be prevented from rotating too much during side flexion (see Fig. 11.7b). The lateral aspect of the ipsilateral foot is now put against the nearer leg of the couch. The other leg is extended out and backwards. Traction in line with the spine is now achieved and this will be facilitated by bending the knee.
Anteroposterior glide during traction
The manipulator stands at one side of the patient’s head, facing it. One hand supports the head under the occiput and the other is positioned at the patient’s chin using the following grip: the web between thumb and index finger is applied to the chin so that thumb and index finger lie on either side. The forearm is kept vertical. The flexed third, fourth and fifth fingers hook under the chin in order to enable traction. The manipulator now places his feet against the legs of the couch and leans sideways, using his body weight for traction. After the slack is taken up, the head is gently glided anteriorly with the use of the hands (Fig. 11.8a). It is then glided posteriorly as far as it can go with a manipulative thrust, the result of a sudden flexion of both knees (Fig. 11.8b).
Lateral gliding
The patient lies supine on the couch. The assistant stands at the patient’s side and firmly fixes the patient’s body (see p. 189).
The manipulator stands at the patient’s head, feet apart. With the forearms supinated, the hands support the head and, with the thumbs kept horizontal along the cheeks, the thenar eminences are placed anteriorly to the ears on either side. Movement is now carried out without traction. By bringing the body weight over one leg and then back to the other as well as taking the patient’s head along with the movement, the neck is moved sideways (Fig. 11.9). The position of the hands should enable the manipulator to maintain the patient’s head in line with the body. Side-flexion movements should be avoided and the movement is purely horizontal.
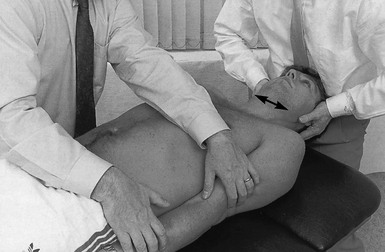
Fig 11.9 Lateral glide.
Traction with leverage
The manipulator then puts the feet against the couch and leans right back until the whole or part of the body weight is sustained by the hand under the chin. Traction is not applied via the hand under the occiput, which only steadies and is squeezed between head and couch to provide a fulcrum. The knees are now suddenly flexed, thus pulling the patient’s neck with a jerk (Fig. 11.10). This results in a sudden increase of traction in the anterior spinal column from the foramen magnum downwards.

Fig 11.10 Traction with leverage.
Manipulation procedure
Choice of technique
• A preparative massage to the muscles of the neck enhances relaxation and so is useful when a patient does not feel sufficiently relaxed (see p. 189).
• Circumduction and straight pull can be used as the first manœuvres, to accustom the patient to the traction element.
• Rotation manipulation is used for unilateral disc protrusions but is avoided in central displacements. Rotation is first performed in the most comfortable direction and then, if still necessary, in the least comfortable direction. It is executed to half-range first, then to three-quarters and only then to full range. When the other direction is chosen, a similar gentle start is again recommended.
• Full rotation during traction is only used when rotation caused improvement and only in the direction in which the result was obtained.
• Side flexion is mostly performed in the direction away from the painful side and very rarely towards the painful side – when, after a few sessions and after repeatedly trying the other techniques, a full result has not yet been obtained. When taking up the slack produces or increases arm pain, the manœuvre is abandoned.
• Anteroposterior gliding is indicated in unilateral disc displacements when the range of extension does not improve with rotation and/or lateral flexion techniques. In central protrusions it can be used in combination with straight pull and lateral flexion.
• Lateral gliding helps to get rid of possible post-manipulative soreness. When overcorrection is produced during a manipulation session – the unilateral pain changes sides – this manœuvre is performed.
• Pure traction techniques – straight pull and traction with leverage – are designed especially for the treatment of posterocentral disc protrusions. Articular movement is thus avoided.
Manipulation strategy
Course of the manipulative session
Posterocentral disc protrusion with unilateral cervicoscapular pain
Two types of case fall into this group.
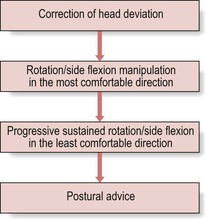
Acute torticollis with side flexion deformity
1. Traction manipulation (straight pull) in the direction of the deviation is performed, in which the head is gradually brought back to the neutral position. No other technique is used before the patient is able to maintain the head in the neutral position when seated upright.
2. Rotation manipulation under traction is then performed in the less restricted direction until this movement has become painless.
3. Lateral flexion manipulation under traction and towards the painless side should then restore a full painless range in that direction.
4. Progressive rotation, without traction, in the restricted direction, in which the head is gradually pushed to the point where pain begins and then immobilized in that position until the pain has disappeared; after this, further movement is undertaken and continued until a full range is achieved. The time taken for the pain to disappear at each stage may vary from a few minutes to 5 minutes or more, which means that up to 20 minutes may be necessary to restore the range of rotation.
5. Progressive lateral flexion, without traction, in the restricted direction is performed, in which the same slow procedure is followed until full side flexion is obtained. This movement usually improves more quickly than rotation; 5–10 minutes are required.
6. When the patient is reassessed after the whole procedure is finished, what has been achieved provides a basis for prognosis. When, after the first treatment, full painless range in all directions is attained, this indicates that by the next day the patient will be much improved or even cured.
7. The patient is then advised to repeat these progressive manœuvres every 2–3 hours and certainly before going to bed because there is a tendency to relapse. Instruction should also be given on what precautions to take to keep recurrence minimal; sleeping in the supine position is preferred. A very thin pillow should be used but support under the neck should be provided (e.g. a rolled towel with a diameter of 5–10 cm). Alternatively, if the patient sleeps on one side, a thick pillow should assure that the cervical spine lies in line with the thoracic spine. Sleeping prone should be avoided.
The patient is seen on a second day and, if considerably better, treatment then consists of manipulations for an ordinary unilateral disc protrusion (see below). When, on the contrary, a considerable relapse has taken place, the whole procedure is repeated. Full relief is usually obtained in 2–3 sessions (Fig. 11.11).
Annular-type torticollis in patients over 30 can be manipulated in the ordinary way (see below).
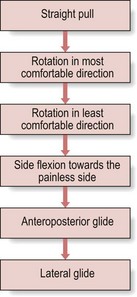
Unilateral cervicoscapular pain
1. Straight pull or circumduction under traction to familiarize the patient with strong traction techniques.
2. Rotation under traction to less than full range in the less restricted or less painful direction.
3. Rotation under traction to full range in the same direction.
4. Rotation under traction to less than full range in the most restricted or most painful direction.
5. Rotation under traction to full range in the same direction.
6. Lateral flexion under traction towards the painless side.
Posterocentral disc protrusion with central or bilateral cervicoscapular pain
Posterolateral disc protrusion with unilateral root pain, without neurological deficit
The normal techniques are used:
2. Rotation under traction in the less restricted or painful direction, first to less than full range and then to full range.
3. Rotation under traction in the most restricted or painful direction, first to less than full range and then to full range.
4. Lateral flexion under traction towards the painless side.
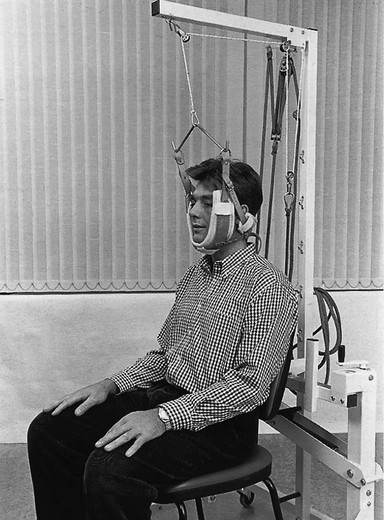
Traction
Traction as a treatment
For a long time, cervical traction has been regarded as an effective treatment for herniated cervical discs because it widens the intervertebral spaces82 and exerts a centripetal force on the disc.83,84 There is no doubt that traction induces pain relief and regression of herniated cervical discs.85 A recent MRI study during 15 minutes of traction with a traction force of 18 kg also showed partial (62%) or complete regression (10%) of protruded cervical discs.86 In spite of this, traction alone is not often used in orthopaedic medicine. The main reason is that clinical improvement is only achieved after 10 or more sessions – a result which could have been achieved much more quickly with ordinary manipulations.
Intermittent traction
Indications
Minor posterocentral discodural interactions
Traction is a good alternative when manipulations are contraindicated (see p. 185). Even if the lesion is of the annular type, it may respond very well to traction, provided the patient is not too old and the articular signs are minor. Four to eight daily sessions usually produce good results.
Contraindications
Technique
Traction can be applied with the patient sitting or lying supine (Figs 11.14 and 11.15). A leather collar is strapped under the patient’s chin and occiput in such a way that the anterior portion clears the trachea while supporting the mandible. The collar is attached to a spreader and hangs by a cord passing over a pulley to the centre of the spreader. The therapist must make sure that the patient’s ears are not squeezed. Traction is applied in the neutral position or with the head held in very slight flexion.
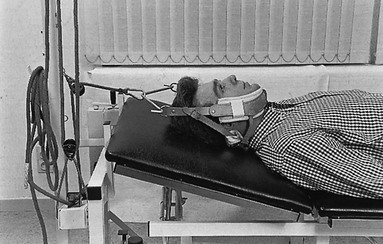
Fig 11.15 Traction performed lying down.
Continuous traction in bed
This is used only when everything else has been tried and failed. Often it is the only alternative to surgery. The treatment has to be carried out in hospital because the patient requires full nursing care 24 hours a day. The traction (4–5 kg) is maintained for the first 24 hours and then gradually diminished and released. The pain is expected to subside slowly and to have diminished after 7–12 days88; the patient may then be discharged from hospital.
Injection at a nerve root
Technique
A 2 mL syringe filled with 20 mg of triamcinolone acetonide is fitted to a 4 cm needle.
The lateral edge of the corresponding transverse process is identified, just behind the posterior edge of the sternocleidomastoid muscle. The needle is inserted between the palpating finger and the midline, and aims at the identified transverse process (Fig. 11.16). It is inserted until it meets bone. Half a millilitre is injected there, and the needle is then moved laterally and slightly cranially until it slips over the edge and the rest of the injection is made here. During the injection the patient may feel radicular pain, which disappears after a few minutes. One to six injections at weekly intervals may be necessary, depending on the severity of symptoms.
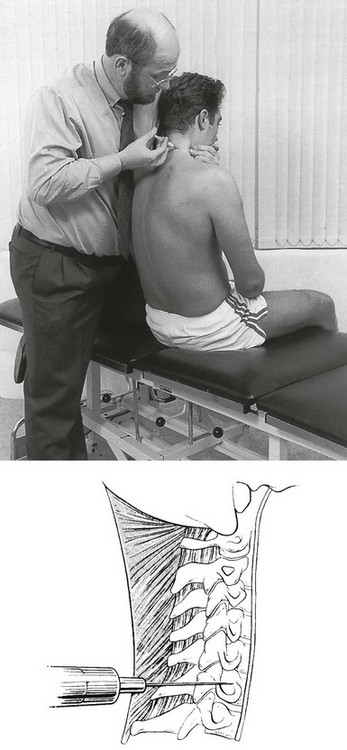
Fig 11.16 Injection at a nerve root.
Results
Radicular pain caused by a discoradicular interaction with or without neurological deficit usually benefits greatly from nerve root blocks. Most studies report a success rate of between 65 and 80% after one or two injections.89–92 Bush et al performed a prospective study with independent clinical review on 68 patients presenting with cervical radiculopathy and neurological signs. The average duration of symptoms prior to presentation was 2 months (range 1–12 months). They received an average of 2.5 periradicular corticosteroid injections per patient (range 1–6). Despite the fact that all 68 patients were potential surgical candidates, they all made a satisfactory recovery without the need for surgical intervention. Forty-eight patients (76%) did not experience any arm pain, and of the 15 patients (24%) who did, this improved from a score of 10 to an average of 2 (range 1–4) on a 10-point pain scale. The conclusion of the study was that patients with cervical radiculopathy make a satisfactory recovery with serial periradicular corticosteroid injections without the need for surgical intervention.93
Epidural injection
Epidural injections have been used to treat radicular pain from herniated discs, spinal stenosis, chemical discs, chronic pain secondary to post-cervical surgery syndrome, and chronic neck pain of discogenic origin. Epidural injections in the cervical spine are performed via either an interlaminar or a transforaminal approach. There are a number of studies supporting the benefit of cervical epidurals.94,95 However, the evidence for cervical interlaminar epidural injections has been a subject of debate and at best has had only moderate success in managing cervical radiculopathy, while there is no evidence available for the management of axial neck pain, post-surgery syndrome or discogenic pain.96–98 In our opinion, cervical epidurals are used far too often for conditions that are easily treated by simpler measures, such as manipulation and nerve root infiltrations. The injection is only called for in radicular pain that lasts longer than a year, has no tendency to spontaneous recovery and is not responding to manipulation (see p. 188).
The injection is always given in theatre conditions; access to the epidural space is obtained under sterile conditions with loss of resistance techniques under fluoroscopic visualization.99 The epidural space is entered between C7 and T1, and 10 mL of either a steroid solution or a mixture of local anaesthetic and steroid is injected.
Collars
Partial or total immobilization of the neck should not be considered as a treatment for neck pain. It does not bring about reduction nor does it influence the normal spontaneous evolution of radicular pain. The role of a collar in non-traumatic cervical lesions is restricted to that of a prevention measure or a psychological support: it gives the patient a sense of security.100
Immobilizing collars are intended to prevent excessive movement that could exacerbate pain. Soft collars seem to have little effect on controlling neck movement101,102 ; neither do hard collars (for example, the Philadelphia, NecLoc and Miami J collars) have the necessary effect, although they are more rigid.103–105 Weight-relieving collars (for example, the Four Poster brace) diminish the weight of the head on the spine and can therefore be used in compression phenomena, such as cord compression, lateral recess stenosis or intractable neck pain.106
Awaiting spontaneous recovery
Time and patience should be employed to explain the mechanism of spontaneous recovery to the patient and to give a good prognosis (see p. 157). A continued interest should be taken, with regular review until symptoms have largely subsided so as to discourage the patient from seeking futile and expensive treatments elsewhere.
Surgery
Surgical intervention for neck pain and/or radicular pain is seldom required.107 In the absence of neurological deficit, it has no better prognosis than the natural history of the process.108 If the neurological deficit is caused by a posterolateral disc protrusion, natural history usually provides just as good long-term results as surgical interventions.109,110 However, if the neurological deficit is caused by a bony outcrop in the lateral foramen, surgery will become inevitable. Surgery is also the treatment of choice in cervical canal stenosis, leading to myelopathy.
Technique
Currently, anterior cervical discectomy with fusion is the gold standard in the surgical treatment of cervical disc herniations.111–113 Since the introduction of the technique in 1958 various anterior fusion methods have been developed.114–116 The anterior approach has several advantages over posterior decompression, i.e. direct decompression of the spinal cord and roots, better alignment and a lower degree of invasiveness. Several modifications have been developed, but there is currently no consensus regarding the optimal technique.117 Microsurgery, known as the posterior keyhole laminotomy-foraminotomy, is used mainly for single-level radiculopathy caused by osteophytic compression in the lateral recess.118,119
Treatment of non-discogenic lesions
Manipulation/capsular stretching
Indications
Migraine
In middle-aged or elderly people, and especially in those who have had migraine from adolescence, manipulation can also be preventative. The techniques that are used are the same as for reduction of disc displacements: straight pull, rotation and side flexion under traction (see p. 189). When neck movements do not cause pain, one session – consisting of one manœuvre in all four directions – may suffice. Painful movements indicate that 2–3 treatments may be necessary before all discomfort ceases. This is a purely empirical finding, which Cyriax identified when patients treated for an ordinary disc lesion reported that, subsequent to manipulation, their attacks of migraine diminished or even disappeared.120
Capsuloligamentous disorders
Simple mobilizations without traction can be used to treat some soft tissue lesions in the neck.
Facet arthrosis
Manipulation of the facet joint by gradual capsular stretching produces reasonable results. The range of movement will probably remain unchanged but the discomfort is largely abolished after 2–4 sessions, perhaps in combination with deep transverse friction (see p. 202) or with facet injection (see p. 203).
Mobilization techniques without traction
Forced rotation
The patient lies supine on the couch.
Slow stretch is obtained by maintaining a steady push at the extreme of range for as long as the patient can tolerate, usually between 30 and 40 seconds. Pressure is then very slowly released and the head gradually brought back to the neutral position (Fig. 11.17). The movement is then repeated once or twice, depending on the patient’s age.

Fig 11.17 Forced rotation.
Forced side flexion
During slow stretch, sustained procedure keeps the head side-flexed at the extreme of range (Fig. 11.18). Because the force has to be maintained for some time, this technique is quite tiring for the operator and therefore extra pressure can be applied with the knee against the elbow. The foot is therefore placed on a stool.

Fig 11.18 Forced side flexion.
Deep transverse friction
Post-traumatic muscular lesions
Facet arthrosis
Technique
The patient sits at the couch with the elbows resting on it and the chin supported by cupped hands. The physiotherapist, standing by the patient’s painful side, palpates the area where the lesion is expected to lie. If the most tender spot corresponds to the facet joint considered to be responsible for the pain, massage is applied there. The articulation is found quite laterally, just behind the posterior border of the sternocleidomastoid muscle. Massage is performed with the flexed thumb and counterpressure with the fingers. The direction is oblique, so that, parallel to the joint line, the thumb passes downwards as it is drawn backwards by internally rotating and abducting the shoulder and flexing the wrist121 (Fig. 11.20).
Injection/infiltration
Technique
The patient sits at the couch with the elbows resting on it and the chin supported by cupped hands. The operator stands behind the patient and palpates for the tender facet joint, which lies 2–2.5 cm from the midline. A 1 mL tuberculin syringe is filled with 10 mg of triamcinolone acetonide suspension and fitted with a thin needle 3 cm long. The needle is inserted until it strikes the lamina and is then moved until it traverses a tough ligamentous structure, the capsule, before it abuts against cartilage. This feeling assures the operator that he has reached the joint. A few drops are then infiltrated at several adjacent points, some intracapsular, some intra-articular. If the needle is thrust in too close to the midline it is possible to traverse the interlaminar space and enter the spinal canal. One to two infiltrations will render the patient pain-free for a considerable period (Fig. 11.21).
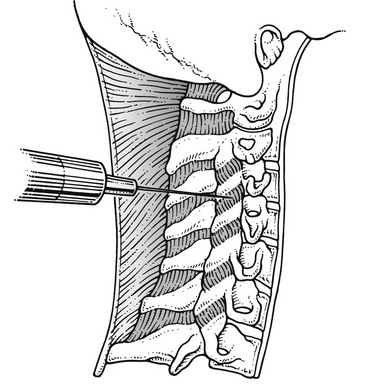
Fig 11.21 Infiltration of a facet joint capsule.
When a nerve root becomes compressed by an osteophytic outcrop and symptoms occur which are severe enough to concern the patient, infiltration with triamcinolone acetonide around the nerve root is tried. The technique for this is described on p. 199.
References
1. Paciaroni, M, Bogousslavsky, J, Cerebrovascular complications of neck manipulation. Eur Neurol. 2009;61(2):112–8.3. ![]()
2. Ernst, E, Prospective investigations into the safety of spinal manipulation. J Pain Symptom Mange 2001; 21:238–242. ![]()
3. Di Fabio, RP, Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79(1):50–65. ![]()
4. Stevinson, C, Honan, W, Cooke, B, Ernst, E, Neurological complications of cervical spine manipulation. J R Soc Med 2001; 94:107–110. ![]()
5. Chen, WL, Chern, CH, Wu, YL, Lee, CH, Vertebral artery dissection and cerebellar infarction following chiropractic manipulation. Emerg Med J. 2006;23(1):e1. ![]()
6. Tinel, D, Bliznakova, E, Juhel, C, et al, Vertebrobasilar ischemia after cervical spine manipulation: a case report. Ann Readapt Med Phys. 2008;51(5):403–414. ![]()
7. Haneline, M, Triano, J, Cervical artery dissection. A comparison of highly dynamic mechanisms: manipulation versus motor vehicle collision. J Manipulative Physiol Ther. 2005;28(1):57–63. ![]()
8. Jay, WM, Shah, MI, Schneck, MJ, Bilateral occipital-parietal hemorrhagic infarctions following chiropractic cervical manipulation. Semin Ophthalmol. 2003;18(4):205–209. ![]()
9. Oehler, J, Gandjour, J, Fiebach, J, Schwab, S, Bilateral vertebral artery dissection after chiropractic treatment. Orthopade. 2003;32(10):911–913. ![]()
10. Parenti, G, Orlandi, G, Bianchi, M, et al, Vertebral and carotid artery dissection following chiropractic cervical manipulation. Neurosurg Rev. 1999;22(2–3):127–129. ![]()
11. Cagnie, B, Vinck, E, Beernaert, A, Cambier, D, How common are side effects of spinal manipulation and can these side effects be predicted? Man Ther 2004; 9:151–156. ![]()
12. Hurwitz, EL, Morgenstern, H, Vassilaki, M, Chiang, L-M, Adverse reactions to chiropractic treatment and their effects on satisfaction and clinical outcomes among patients enrolled in the UCLA neck pain study. J Manipulative Physiol Ther 2004; 27:16–25. ![]()
13. Thiel, HW, Bolton, JE, Docherty, S, Portlock, JC, Safety of chiropractic manipulation of the cervical spine: a prospective national survey. Spine (Phila Pa 1976). 2007;32(21):2375–2378. ![]()
14. Krueger, BR, Okazaki, H, Vertebrobasilar distribution infarction following chiropractic cervical manipulation. Mayo Clin Proc 1980; 55:322–332. ![]()
15. Terrett, AGJ. Vascular accidents from cervical spine manipulation: report on 107 cases. J Aust Chiropract Assoc. 1987; 17:15–24.
16. Henderson, DJ. Vertebral artery syndrome. In: Vear HJ, ed. Chiropractic Standards of Practice and Quality of Care. Gaithersburg: Aspen; 1992:115–143.
17. Ernst, E, Adverse effects of spinal manipulation: a systematic review. J R Soc Med. 2007;100(7):330–338. ![]()
18. Gouveia, LO, Castanho, P, Ferreira, JJ, Safety of chiropractic interventions: a systematic review. Spine (Phila Pa 1976). 2009;34(11):E405–E413. ![]()
19. Stringer, WL, Kelly, DL, Jr., Traumatic dissection of the extracranial internal carotid artery. Neurosurgery. 1980;6(2):123–130. ![]()
20. Zetterling, M, Carlström, C, Konrad, P, Internal carotid artery dissection. Acta Neurol Scand. 2000;101(1):1–7. ![]()
21. Arnold, M, Cumurciuc, R, Stapf, C, et al, Pain as the only symptom of cervical artery dissection. J Neurol Neurosurg Psychiatry. 2006;77(9):1021–1024. ![]()
22. Benninger, DH, Georgiadis, D, Kremer, C, et al, Mechanism of ischemic infarct in spontaneous carotid dissection. Stroke. 2004;35(2):482–485. ![]()
23. Beaudry, M, Spence, JD, Motor vehicle accidents: the most common cause of traumatic vertebrobasilar ischemia. Can J Neurol Sci. 2003;30(4):320–325. ![]()
24. Ast, G, Woimant, F, Georges, B, et al, Spontaneous dissection of the internal carotid artery in 68 patients. Eur J Med. 1993;2(8):466–472. ![]()
25. Kumar, SD, Kumar, V, Kaye, W, Bilateral internal carotid artery dissection from vomiting. Am J Emerg Med. 1998;16(7):669–670. ![]()
26. Foye, PM, Najar, MP, Camme, AA, Pain, dizziness, and central nervous system blood flow in cervical extension: vascular correlations to beauty parlor stroke syndrome and salon sink radiculopathy. Am J Phys Med Rehabil. 2002;81(6):395–399. ![]()
27. Rome, P. Perspectives: an overview of comparative considerations of cerebrovascular accidents. Chirpr J Aust. 1999; 29:87–102.
28. Haneline, MT, Lewkovich, GN, An analysis of the etiology of cervical artery dissections: 1994 to 2003. J Manipulative Physiol Ther. 2005;28(8):617–622. ![]()
29. Schievink, WI, Mokri, B, Piepgras, DG, Spontaneous dissections of cervicocephalic arteries in childhood and adolescence. Neurology. 1994;44(9):1607–1612. ![]()
30. Brandt, T, Orberk, E, Weber, R, Pathogenesis of cervical artery dissections: association with connective tissue abnormalities. Neurology. 2001;57(1):24–30. ![]()
31. Haldeman, S, Kohlbeck, FJ, McGregor, M, Unpredictability of cerebrovascular ischemia associated with cervical spine manipulation therapy: a review of sixty-four cases after cervical spine manipulation. Spine (Phila Pa 1976). 2002;27(1):49–55. ![]()
32. Haldeman, S, Kohlbeck, FJ, McGregor, M, Stroke, cerebral artery dissection, and cervical spine manipulation therapy. J Neurol. 2002;249(8):1098–1104. ![]()
33. Miley, ML, Wellik, KE, Wingerchuk, DM, Demaerschalk, BM, Does cervical manipulative therapy cause vertebral artery dissection and stroke? Neurologist. 2008;14(1):66–73. ![]()
34. Haldeman, S, Carey, P, Townsend, M, Papadopoulos, C, Clinical perceptions of the risk of vertebral artery dissection after cervical manipulation: the effect of referral bias. Spine J. 2002;2(5):334–342. ![]()
35. Hosek, RS, Schram, SB, Silverman, H, et al, Cervical manipulation. JAMA. 1981;245(9):922. ![]()
36. Hurwitz, EL, Aker, PD, Adams, AH, et al, Manipulation and mobilization of the cervical spine: a systematic review of the literature. Spine 1996; 21:1746–1759. ![]()
37. Leboeuf-Y de, C, Rasmussen, LR, Klougart, N, The risk of over- reporting spinal manipulative therapy-induced injuries: a description of some cases that failed to burden the statistics. Manip Physiol Ther. 1996;19(8):536–538. ![]()
38. Dabbs, V, Lauretti, WJ, A risk assessment of cervical manipulation vs. NSAIDs for the treatment of neck pain. J Manipulative Physiol Ther 1995; 18:530–536. ![]()
39. Li, YK, Zhang, YK, Lu, CM, Zhong, SZ, Changes and implications of blood flow velocity of the vertebral artery during the rotation and extension of the head. J Manipulative Physiol Ther 1999; 22:91–95. ![]()
40. Licht, PB, Christensen, HW, Hoilund-Carlsen, PF, Vertebral artery volume flow in human beings. J Manipulative Physiol Ther 1999; 22:363–367. ![]()
41. Mitchell, JA, Changes in vertebral artery blood flow following normal rotation of the cervical spine. J Manipulative Physiol Ther 2003; 26:347–351. ![]()
42. Richter, R, Reinking, M, Clinical question: How does evidence on the diagnostic accuracy of the vertebral artery test influence teaching of the test in a professional physical therapy education program? Phys Ther 2005; 85:589–599. ![]()
43. (43Grant R. Clinical testing before cervical manipulation – can we recognise the patient at risk? Proceedings of Tenth International Congress of the World Confederation of Physical Therapy. Sydney, 1987. p. 192–197.
44. Anon. Protocol for premanipulative testing of the cervical spine. Aust J Physiother. 1988; 34:97–100.
45. Grant, R, Vertebral artery testing – the Australian Physiotherapy Association protocol after 6 years. Manual Therapy 1996; 1:149–153. ![]()
46. Arnold, C, Bourassa, R, Langer, T, Stoneham, G, Doppler studies evaluating the effect of a physical therapy screening protocol on vertebral artery blood flow. J Manipulative Physiol Ther 2004; 9:13–21. ![]()
47. Di Fabio, RP, Manipulation of cervical spine: Risks and benefits. Phys Ther 1999; 79:50–65. ![]()
48. Rivett, DA, Milburn, P. A prospective study of complications of cervical spine manipulation. J Manual Manip Ther. 1996; 4(4):166–170.
49. Sweeney, A, Doody, C, Manual therapy for the cervical spine and reported adverse effects: a survey of Irish manipulative physiotherapists. Man Ther. 2010;15(1):32–36. ![]()
50. Childs, JD, Flynn, TW, Fritz, JM, et al, Screening for vertebrobasilar insufficiency in patients with neck pain: manual therapy decision-making in the presence of uncertainty. J Orthop Sports Phys Ther 2005; 35:300–306. ![]()
51. Cote, P, Kreitz, BG, Cassidy, JD, Thiel, H, The validity of the extension-rotation test as a clinical screening procedure before neck manipulation: a secondary analysis. J Manipulative Physiol Ther 1997; 20:65. ![]()
52. Haynes, M, Vertebral arteries and cervical movement: Doppler ultrasound velocimetry for screening before manipulation. J Manipulative Physiol Ther 2002; 25:556–567. ![]()
53. Haynes, M, Cala, L, Melsom, A, et al, Vertebral arteries and cervical rotation: modeling and magnetic resonance angiography studies. J Manipulative Physiol Ther 2002; 25:370–383. ![]()
54. Di Fabio, RP, Manipulation of cervical spine: risks and benefits. Phys Ther 1999; 79:50–65. ![]()
55. Furman, JM, Whitney, SL, Central causes of dizziness. Phys Ther 2000; 80:179–184. ![]()
56. Wuest, S, Symons, B, Leonard, T, Herzog, WJ, Preliminary report: biomechanics of vertebral artery segments C1–C6 during cervical spinal manipulation. Manipulative Physiol Ther. 2010;33(4):273–278. ![]()
57. Johnson, EG, Houle, S, Perez, A, et al, Relationship between the duplex Doppler ultrasound and a questionnaire screening for positional tolerance of the cervical spine in subjects with suspected vascular pathology: a case series pilot study. J Man Manip Ther. 2007;15(4):225–230. ![]()
58. Terrett, AGJ. It is more important to know when not to adjust. Chiropract Tech. 1990; 2(l):l–9.
59. Assendelft, WJJ. Chiropractic in the Netherlands: Diagnosis and Effects of Treatment. Amsterdam: Akademisch Proefschrift; 1996.
60. Leboeuf-Y de, C, Hennius, B, Rudberg, E, et al, Side effects of chiropractic treatment: a prospective study. J Manip Physiol Ther. 1997;20(8):511–513. ![]()
61. De Bock, S. Medical Complications after Manipulation of the Spine. G.G.S. Brussels: Manual Therapy; 1993.
62. Murphy, DR, Current understanding of the relationship between cervical manipulation and stroke: what does it mean for the chiropractic profession? Chiropr Osteopat. 2010;18(1):22. ![]()
63. Gross, AR, Hoving, JL, Haines, TA, et al, A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine (Phila Pa 1976). 2004;29(14):1541–1548. ![]()
64. Bronfort, G, Haas, M, Evans, RL, Bouter, LM, Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4(3):335–356. ![]()
65. Koes, BW, Bouter, LM, van Mameren, H, et al, The effectiveness of manual therapy, physiotherapy, and treatment by the general practitioner for nonspecific back and neck complaints. A randomized clinical trial. Spine 1992; 17:28–35. ![]()
66. Koes, BW, Bouter, LM, van Mameren, H, et al, A randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints: subgroup analysis and relationship between outcome measures. J Manipulative Physiol Ther 1993; 16:211–219. ![]()
67. Hoving, JL, Koes, BW, de Vet, HC, et al, Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med. 2002;136(10):713–722. ![]()
68. Korthals-de Bos, IB, Hoving, JL, van Tulder, MW, et al, Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ. 2003;326(7395):911. ![]()
69. Walker, MJ, Boyles, RE, Young, BA, et al, The effectiveness of manual physical therapy and exercise for mechanical neck pain: a randomized clinical trial. Spine (Phila Pa 1976). 2008;33(22):2371–2378. ![]()
70. Hoving, JL, de Vet, HC, Koes, BW, et al, Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long-term results from a pragmatic randomized clinical trial. Clin J Pain. 2006;22(4):370–377. ![]()
71. Vernon, H, Humphreys, K, Hagino, C, Chronic mechanical neck pain in adults treated by manual therapy: a systematic review of change scores in randomized clinical trials. J Manipulative Physiol Ther. 2007;30(3):215–227. ![]()
72. García-Moreno, JM, Izquierdo, G, Lhermitte’s sign. Neurologia. 2002;17(3):143–150. ![]()
73. Bonic, EE, Stockwell, CA, Kettner, NW, Brain stem compression and atlantoaxial instability secondary to chronic rheumatoid arthritis in a 67-year-old female. J Manipulative Physiol Ther. 2010;33(4):315–320. ![]()
74. Robinson, HS, Rheumatoid arthritis – atlanto-axial subluxation and its clinical presentation. Can Med Assoc J. 1966;94(10):470–477. ![]()
75. Neva, MH, Häkkinen, A, Mäkinen, H, et al, High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann Rheum Dis. 2006;65(7):884–888. ![]()
76. Whedon, JM, Quebada, PB, Roberts, DW, Radwan, TA, Spinal epidural hematoma after spinal manipulative therapy in a patient undergoing anticoagulant therapy: a case report. J Manipulative Physiol Ther. 2006;29(7):582–585. ![]()
77. Rose, KA, Kim, WS, The effect of chiropractic care for a 30-year-old male with advanced ankylosing spondylitis: a time series case report. J Manipulative Physiol Ther. 2003;26(8):E1–E9. ![]()
78. Liao, CC, Chen, LR, Anterior and posterior fixation of a cervical fracture induced by chiropractic spinal manipulation in ankylosing spondylitis: a case report. J Trauma. 2007;63(4):E90–E94. ![]()
79. Takata, K, Inoue, S, Takahashi, K, Ohtsuka, Y, Swelling of the cauda equina in patients who have herniation of a lumbar disc. J Bone Joint Surg 1988; 70A:361–368. ![]()
80. Parke, WW, Watanabe, R, The intrinsic vasculature of the lumbo-sacral spinal nerve roots. Spine 1985; 10:508–515. ![]()
81. Cyriax, JH. Textbook of Orthopaedic Medicine. vol I. Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
82. Chung, CT, Tsai, SW, Chen, CJ, et al, Comparison of the intervertebral disc spaces between axial and anterior lean cervical traction. Eur Spine J. 2009;18(11):1669–1676. ![]()
83. Saunders, HD, Use of spinal traction in the treatment of neck and back conditions. Clin Orthop 1983; 179:31–38. ![]()
84. Wong, AMK, Leong, CP, Chen, CM, The traction angle and cervical intervertebral separation. Spine 1992; 18:136–138. ![]()
85. Valtonen, EJ, Moller, K, Wiljasalo, M. Comparative radiographic study of the effect of intermittent and continuous traction on elongation of cervical spine. Ann Med Intern Finn. 1968; 57:143–146.
86. Chung, TS, Lee, YJ, Kang, SW, et al, Reducibility of cervical disk herniation: evaluation at MR imaging during cervical traction with a nonmagnetic traction device. Radiology. 2002;225(3):895–900. ![]()
87. Newton, HB, Rea, GL, Lhermitte’s sign as a presenting symptom of primary spinal cord tumor. J Neurooncol. 1996;29(2):183–188. ![]()
88. Cyriax, JH. Textbook of Orthopaedic Medicine. vol II. Treatment by Manipulation, Massage and Injection, 11th ed. London: Baillière Tindall; 1984.
89. Kolstad, F, Leivseth, G, Nygaard, OP, Transforaminal steroid injections in the treatment of cervical radiculopathy. A prospective outcome study. Acta Neurochir (Wien). 2005;147(10):1065–1070. ![]()
90. Berger, O, Dousset, V, Delmer, O, et al, Evaluation of the efficacy of foraminal infusions of corticosteroids guided by computed tomography in the treatment of radicular pain by foraminal injection. J Radiol. 1999;80(9):917–925. ![]()
91. Cyteval, C, Thomas, E, Decoux, E, et al, Cervical radiculopathy: open study on percutaneous periradicular foraminal steroid infiltration performed under CT control in 30 patients. AJNR Am J Neuroradiol. 2004;25(3):441–445. ![]()
92. Lee, JW, Park, KW, Chung, SK, et al, Cervical transforaminal epidural steroid injection for the management of cervical radiculopathy: a comparative study of particulate versus non-particulate steroids. Skeletal Radiol. 2009;38(11):1077–1082. ![]()
93. Bush, K, Hillier, S, Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996;5(5):319–325. ![]()
94. Peloso, PMJ, Gross, A, Haines, T, et al, CervicalOverview Group. Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev 2007; 3. ![]()
95. Benyamin, RM, Singh, V, Parr, AT, et al, Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician 2009; 12:137–157. ![]()
96. Kwon, JW, Lee, JW, Kim, SH, et al, Cervical interlaminar epidural steroid injection for neck pain and cervical radiculopathy: effect and prognostic factors. Skeletal Radiol. 2007;36(5):431–436. ![]()
97. Catchlove, RF, Braha, R, The use of cervical epidural nerve blocks in the management of chronic head and neck pain. Can Anaesth Soc J 1984; 31:188–191. ![]()
98. Lin, EL, Lieu, V, Halevi, L, et al, Cervical epidural steroid injections for symptomatic disc herniations. J Spinal Disord Tech. 2006;19(3):183–186. ![]()
99. Michael, J, Murphy, J, Lieponis, V. Nonoperative treatment of cervical spine pain. In: Sherk HH, ed. The Cervical Spine. 2nd ed. Philadelphia: Lippincott; 1989:673.
100. McGuire, RA, Degnan, G, Amundson, GM, Evaluation of current extrication orthroses in immobilization of the unstable cervical spine. Spine 1990; 15:1064. ![]()
101. Teale, C, Mulley, GP. Support collars: a preliminary survey of their benefits and problems. Clin Rehab. 1990; 4:33.
102. Johnson, RM, Owen, JR, Hart, DL, Callahan, RA, Cervical orthroses – a guide to their selection and use. Clin Orthop Rel Res 1981; 154:34. ![]()
103. Kaufman, WA, Lunsford, TR, Lance, LL. Comparison of three prefabricated cervical collars. Orthop Prosthetics. 1986; 39:21.
104. Lavernia, CJ, Botte, MJ, Garfin, SR. The spine. In: Rothman RH, Simeone FA, eds. Spinal Orthoses for Traumatic and Degenerative Disease. 3rd ed. Philadelphia: WB Saunders; 1992:1197.
105. Richter, D, Latta, LL, Milne, EL, et al, The stabilizing effects of different orthoses in the intact and unstable upper cervical spine: a cadaver study. J Trauma. 2001;50(5):848–854. ![]()
106. Vaccaro, AR, Botte, MJ, Lind, BI, Gardin, SR. Cervical orthotics including traction and halo devices. In: Clark CR, ed. The Cervical Spine. 3rd ed. Philadelphia: Lippincott-Raven; 1998:113–140.
107. Kolstad, F, Leivseth, G, Nygaard, OP, Transforaminal steroid injections in the treatment of cervical radiculopathy. A prospective outcome study. Acta Neurochir (Wien). 2005;147(10):1065–1070. ![]()
108. Gore, DR, Sepie, SB, Gardner, GM, et al, Neck pain: a long-term follow-up of 205 patients. Spine 1987; 12:1–5. ![]()
109. Persson, LC, Moritz, U, Brandt, L, Carlsson, CA, Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. Eur Spine J. 1997;6(4):256–266. ![]()
110. Persson, LC, Carlsson, CA, Carlsson, JY, Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine (Phila Pa 1976). 1997;22(7):751–758. ![]()
111. Cloward, RB, The anterior approach for removal of ruptured cervical disks. J Neurosurg 1958; 15:602–617. ![]()
112. Smith, GW, Robinson, RA, The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A(3):607–624. ![]()
113. Bailey, RW, Badgley, CE, Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am 1960; 42-A:565–594. ![]()
114. Kepler, CK, Rawlins, BA, Mesh cage reconstruction with autologous cancellous graft in anterior cervical discectomy and fusion. J Spinal Disord Tech. 2010;23(5):328–332. ![]()
115. Park, HW, Lee, JK, Moon, SJ, et al, The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976). 2009;34(17):E591–E595. ![]()
116. Majd, ME, Vadhva, M, Holt, RT, Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976). 1999;24(15):1604–1610. ![]()
117. Lied, B, Roenning, PA, Sundseth, J, Helseth, E, Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg 2010; 10:10. ![]()
118. Jagannathan, J, Sherman, JH, Szabo, T, et al, The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 2009;10(4):347–356. ![]()
119. Cağlar, YS, Bozkurt, M, Kahilogullari, G, et al, Keyhole approach for posterior cervical discectomy: experience on 84 patients. Minim Invasive Neurosurg. 2007;50(1):7–11. ![]()
120. Cyriax, JH. Textbook of Orthopaedic Medicine. vol I, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
121. Troisier, O. Les Algies discales et ligamentaires du rachis. Paris: Masson; 1953.