Traumatic Lesions of the Skull and Face*
Congenital Depressions
Congenital depressions of the calvaria occur as a result of mechanical factors that occur before or during birth.1 These depressions usually are visible by direct inspection, but radiographs often are obtained to search for associated fractures. During labor, depressions of the calvaria are caused by excessive localized pressure on the head by the bony prominences in the maternal pelvis, including the sacral promontory, pubic symphysis, and sciatic spines (e-Fig. 23-1). Application of forceps to the fetal head and traction with excessive force is another less common cause of congenital depressions that occurs during labor.
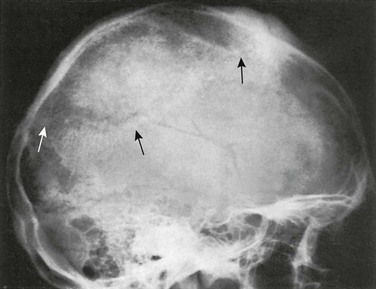
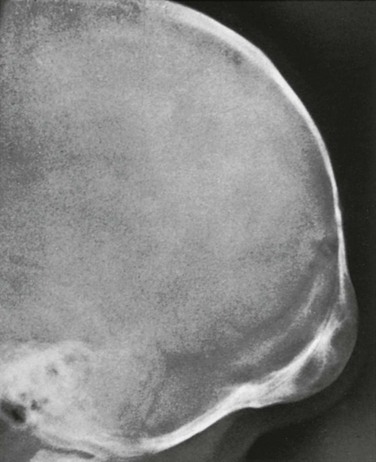
e-Figure 23-1 Congenital parietal depression.
A, A film shows a congenital parietal depression (arrow) in a 37-day-old infant. B and C, A computed tomography scan of another infant with a depressed right parietal fracture. B, Brain window; C, bore window.
Severe cranial deformities also may develop during fetal life from sustained abnormal fetal positions (e-Fig. 23-2). Grooves in the calvarium and face may be caused by excessive pressure of an ectopic shoulder or limb. Lower and upper limb positions may be responsible and represent restrictions of the usual active movements of the fetus. Deformities also may arise as a result of pressure from amniotic bands.
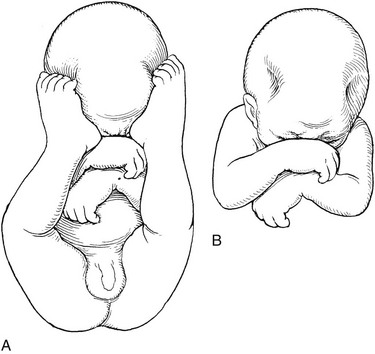
e-Figure 23-2 A schematic drawing of the pathogenesis of congenital depressions in the cranium resulting from a faulty fetal posture.
A, An abnormal fetal position in which the feet indent the calvaria. B, Lateral frontoparietal depressions in the calvaria after removal of the feet from the depressions.
Cranial depressions that are present at birth and are not associated with edema or hemorrhage of the underlying soft tissues usually are due to long-standing faulty fetal position rather than to a recent birth injury. Spontaneous elevation of prenatal depressions during the first year after birth without adverse residual effects have been reported.1 Acute depressions as a result of the application of forceps, often called “ping-pong ball depressions,” have been elevated by simple tangential digital pressure on opposite sides of the depression and by suction with a hand-operated breast pump.2
Hemorrhage
Hemorrhage in the neonatal scalp may occur at three different levels: subcutaneous (as in caput succedaneum), subaponeurotic (subgaleal), and subperiosteal. More superficial bleeds cross suture lines and may extend widely into the face ventrally, onto the neck dorsally, and onto the zygomatic arches and mastoid processes laterally. Subgaleal hemorrhages also are known as cephalohematoceles and may contribute to the swelling and clinical findings in massive caput succedaneum. Subperiosteal hemorrhages are known as cephalhematomas. In contrast to the previous two conditions, cephalhematomas are confined sharply by the edges of the bones they overlie, and shells of bone form over them during resolution, arising from the elevated periosteum that covers them externally (Fig. 23-3). The usual cause of cephalhematomas is trauma to the fetal head during labor. Cephalhematomas also may develop after cephalic injuries during infancy and childhood. Fine linear fractures of the underlying bone may be found in the sites of cephalhematomas and are thought by some investigators to be the principal cause of bleeding of the pericranium. The incidence of cephalhematomas in two very large series of neonates was found to be 1.5% to 2.5%.3,4 Associated fractures were found in 25% of the cephalhematomas studied radiographically.3 The incidence of forceps delivery in the two studies was 75% and 33%, a probable explanation for the difference in the incidence of fracture-associated lesions.
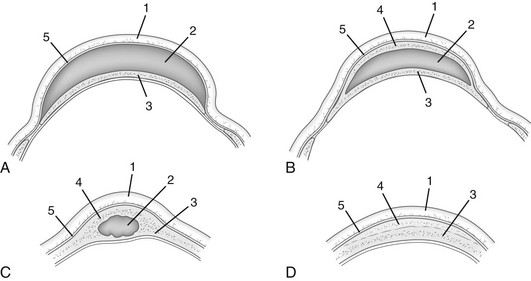
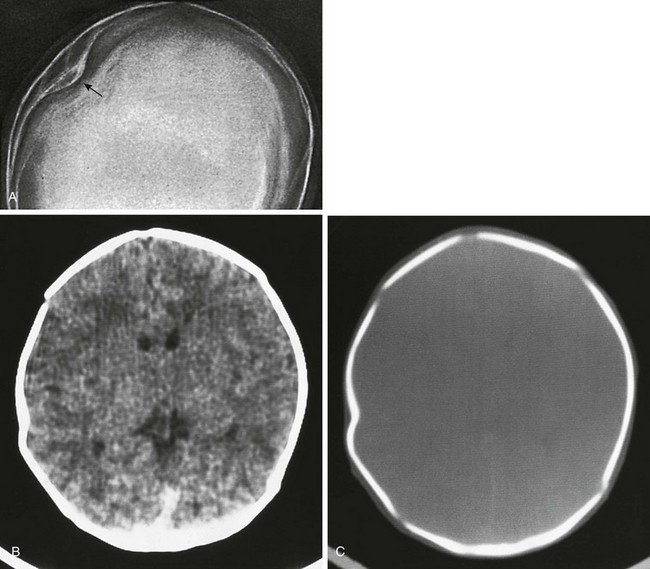
Figure 23-3 Diagrammatic sketches of anatomic changes that occur in a person with a cephalhematoma.
A, A fresh subperiosteal hematoma. B, The healing phase, which shows a new shell of subperiosteal bone over the hematoma. C, Persistence of an organized hematoma in the diploic space. D, Persistent residual external thickening of the outer table after complete resorption of subperiosteal blood. C and D represent late residuals that may persist into adult life. 1, Scalp; 2, hematoma; 3, normal calvaria; 4, new subperiosteal bone; 5, periosteum.
Clinically, subperiosteal cephalhematomas appear as localized swellings, usually over the parietal and occipital bone (Fig. 23-4). The fresh lesions characteristically extend over the entire surface of the affected bone and are sharply limited at the edges of the bone where the periosteum is bound tightly to the membranous tissue of the sutures. The parietal bones are most often affected, but occipital lesions are common and may be confused with occipital meningoceles during the first days of life. Frontal cephalhematomas are very rare.
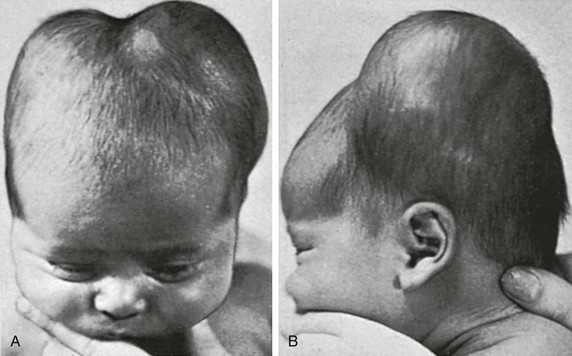
Figure 23-4 Bilateral parietal cephalhematomas in a 13-day-old neonate.
Limitation of the edges of the tumors to the sutures is shown clearly at the sagittal, coronal, and lambdoid sutures. The deep furrow between the two parietal cephalhematomas is due to fixation of the periosteum at the sagittal suture. Frontal (A) and lateral (B) views are provided.
The radiographic findings vary with the age of the cephalhematomas. During the first 2 weeks, the lesion is composed of fluid blood and casts a shadow of water density (Fig. 23-5). Near the end of the second week, bone begins to form under the elevated periosteum. It appears first at the margins, but soon the entire cephalohematoma is overlaid with a complete shell of bone (e-Fig. 23-6; see Fig. 23-5). Depending on their size, cephalhematomas clinically are gradually absorbed over 2 weeks to 3 months. The radiographic findings, in contrast, persist long after the clinical signs have disappeared (e-Fig. 23-7). The outer table usually remains thickened as a flat, irregular hyperostosis for several months and is gradually resorbed. Fresh cephalhematomas may become infected during bacteremia or needle aspiration.5 Ultrasonography may be used for early diagnosis, thus avoiding the use of radiation (Fig. 23-8). Associated fractures generally are of no clinical significance.
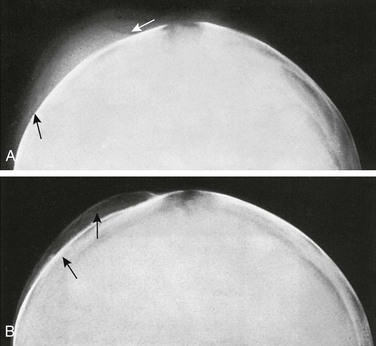
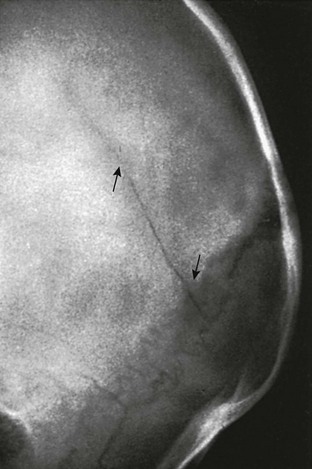
Figure 23-5 A cephalhematoma.
A, Rounded soft tissue swelling (arrows) of water density over the left parotid bone at age 7 days. B, The same skull at age 32 days shows a thin shell of newly formed subperiosteal bone (upper arrow) overlying the margin of the partially resorbed hematoma (lower arrow).
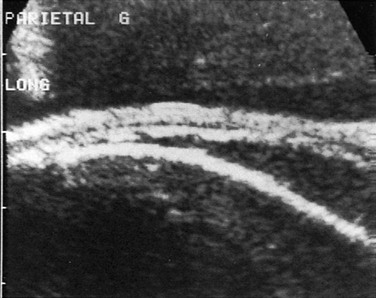
Figure 23-8 An ultrasound scan of the edge of a parietal cephalhematoma (compare with Fig. 23-3, B).
The periosteum is raised by the sonolucent blood; its width and echogenicity result from subperiosteal bone formation that is too minimal to show on radiographs. (Courtesy Dr. Daniel Nussle, Geneva, Switzerland.)
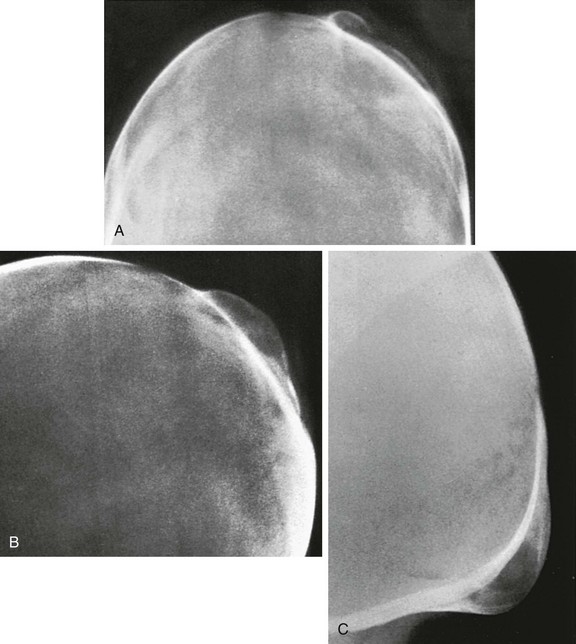
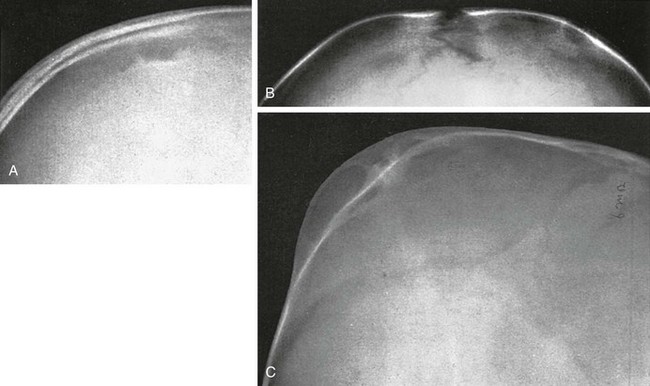
e-Figure 23-6 Changes in an ossifying subperiosteal hematoma on the left parietal bone of a 6-week-old infant who had been delivered by forceps.
Frontal (A) and lateral (B) projections are shown. A thin but incomplete shell of bone covers the hematoma. C, An occipital subperiosteal cephalhematoma with a complete and thicker shell of bone over the radiolucent mass of organized hematoma, both of which are sharply limited below at the level of the mendosal suture.
e-Figure 23-7 An ossifying subperiosteal cephalhematoma on the occipital squamosa of a 4-month-old infant.
The cephalhematoma extends from the lambdoid suture above to the level of the mendosal suture below, which is already fused. The large radiolucent patches beneath the subperiosteal shell of newly formed bone are cast by masses of blood in varying degrees of organization and resorption.
In some cases, the space between a new shell of bone and the inner table remains widened for many years, and the space originally occupied by the hematoma becomes filled with normal diploic bone (Fig. 23-9). In other cases, large and small cystlike defects persist in the sites of cephalhematomas (e-Fig. 23-10).6 Infantile cephalhematoma occasionally persists into adult life, when symptomless large segments of bone production and destruction still may be visible in the calvarium (cephalhematoma deformans) (e-Fig. 23-11).7 The possibility of a prior neonatal cephalhematoma should be considered in practically all lesions of parietal and occipital bones in older infants, children, and adults. An adequate history of the state of the neonatal head should be taken before the final radiographic evaluation of lesions of the calvarium is made.
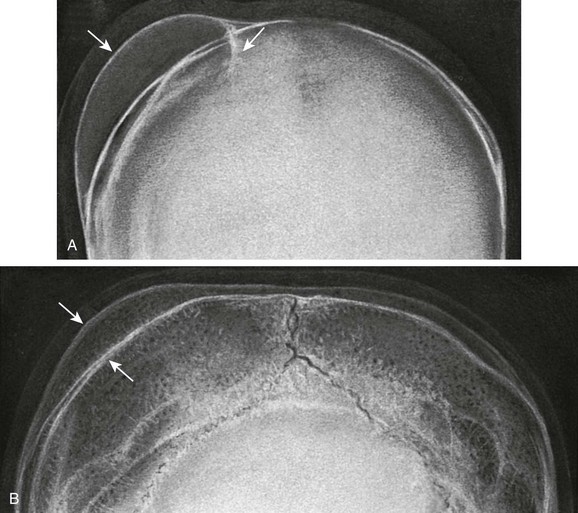
Figure 23-9 Radiographs show late residual thickening of the calvaria resulting from neonatal cephalhematoma.
A, At 7 weeks of age, a large hematoma (arrows) is covered by a thin osseous shell on the right parietal bone. B, At 3 years and 11 months of age, a widening of the diploic space (arrows) occurs in the right parietal bone, where the neonatal hematoma was located.
e-Figure 23-10 Radiolucent cystlike residues of neonatal cephalhematomas.
Lateral (A) and frontal (B) projections of a defect in the parietal bone in an 11-month-old infant. Residual thickening of the contiguous portions of the parietal bone is still evident. C, Residual thickening of the parietal bone in a 6-month-old infant with large cystlike defects in the area of thickening.
Subgaleal Hygroma
A subgaleal hygroma clinically may simulate a cephalhematoma or a caput succedaneum. Radiographically, the swellings in the parietal regions usually are associated with underlying fractures (Fig. 23-12). Trauma from use of obstetric forceps is a common cause of subgaleal hygromas. In older children, a subgaleal hygroma may result from hair-pulling in cases of child abuse or accidental entrapment of long hair in mechanical equipment. A subgaleal hematoma may occur without antecedent trauma in patients with coagulation abnormalities. The scalp swells because of the accumulation of cerebrospinal fluid (CSF), and usually some blood, beneath the epicranial aponeurosis. The abnormal fluid extends across the sutures, contrary to the pattern seen with cephalhematomas.
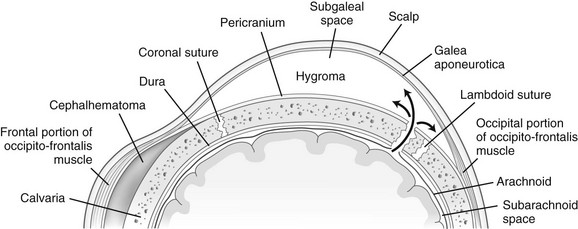
Figure 23-12 Course of flow of the cerebrospinal fluid after fracture of the calvaria.
Tears of the arachnoid and dura internally and of the periosteum externally into the subgaleal (epicranial) space form a large subgaleal hygroma under the galea aponeurotica. (Modified from Epstein JA, Epstein BS, Small M. Subepicranial hygromas: a complication of head injuries in infants and children. J Pediatr. 1961;59:562-566.)
Cranial Fractures
A 12% incidence of skull fractures, all depressed, was reported in a large series of head injuries sustained at birth.8 Forceps were used in most of these deliveries. The fractures were almost all in the parietal and occipital bones. When clinical signs warrant intracranial evaluation, CT may be used in emergent situations, but MRI will provide more detailed brain evaluation.
Infants and Children
Plain radiographic examination of the skull has little to offer in the management of nonabusive head trauma in infants and children. The presence or absence of a fracture neither correlates with the clinical situation nor affects management.9–14 In a series of 256 children younger than 5 years who fell out of bed at home or in the hospital, only three skull fractures were found, and clinically these fractures were insignificant.14 Serious injuries attributed to falls from a bed must be evaluated very carefully for possible child abuse factors (see Chapters 47 and 144).
The major indication for skull radiographs is suspected child abuse. Prospective study of a series of more than 7000 patients suggests that if certain clinical criteria are present singly or in combination, CT or MRI examination is warranted to evaluate for intracranial injury.15–21 The selection criteria are (1) unconsciousness or a documented decreasing level of consciousness; (2) a history of a craniotomy with a shunt in place; (3) the probability of a skull depression or identification of a skull depression by probing through a laceration or a puncture wound; (4) blood in the ear or fluid discharge from the ear; (5) CSF discharge from the nose; (6) ecchymosis behind the ear (Battle sign); (7) bilateral orbital ecchymoses; and (8) unexplained focal neurologic signs. If cephalhematoma, drowsiness, and age younger than 1 year were added as criteria, no fractures would have been missed in these series.
In a multi-institutional study in which more than 42,000 children with head trauma and a Glasgow Coma Scale score of 14 or 15 were evaluated, a negative predictive value of almost 100% and a sensitivity of greater than 96.8% were found when the criteria in Box 23-1 were absent. In the absence of these findings, no risk is posed to the patient when a CT scan is not obtained.
Depressed fractures of the skull occur most frequently when large vectors of force are involved, as in vehicular accidents or direct local trauma or after forceps deliveries in the neonate. Many fractures are compounded by associated lacerations or communication with the nasal or aural cavities, and the fractures often are comminuted. Dural tears are relatively common with depressed fractures, whereas extradural and subdural hematomas are far less common.8
When performing an examination for fractures in young patients in whom the cranial sutures are conspicuously visible, it is necessary to keep in mind the great normal variability of these structures (see Chapter 18). Sutures may widen radiographically as a possible disturbance of desmogenous ossification as a result of the long-term administration of prostaglandin E1.22 The observation of sutural widening during recovery from nutritional deprivation may involve similar mechanisms.23 The linear shadows of diminished density arising from fractures must be differentiated from linear vascular markings, particularly those of the grooves for the middle meningeal artery and its branches. Whether or not the fractures are depressed, they may result in tears of dural sinuses, especially when located in areas through which they course. The position of the bone edges at the time of posttrauma examination may give no indication of how much displacement took place at the moment the fracture occurred. Oblique single-bevel fractures that interrupt the continuity of the inner and outer tables in different planes may be invisible or simulate two fractures in certain projections. In some cases, especially with depressed fractures, the edges of the fragments may overlap and cast linear shadows of increased density. CT is the optimal modality for evaluating the depressed fragments and their relation to the underlying brain (Fig. 23-13). Some of the radiographic characteristics of cranial fractures are shown in e-Figure 23-14, Figures 23-15 through 23-17, and e-Figure 23-18.
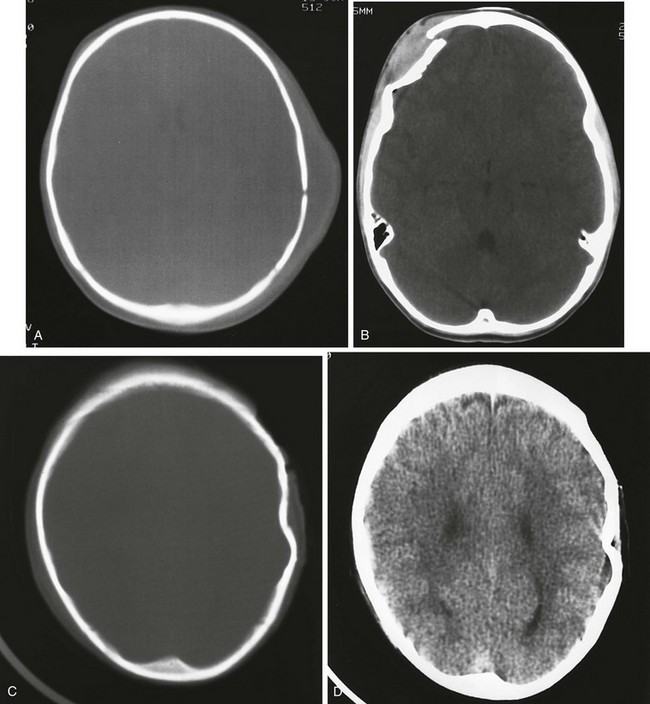
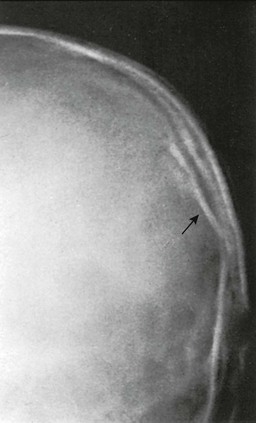
Figure 23-13 Computed tomography (CT) in evaluating calvaria and intracranial trauma.
A, A CT scan with bone windows shows a large soft tissue hematoma and linear fracture in the left parietal region. B, A CT scan in another child shows a depressed right frontal fracture with a large external hematoma and a small epidural lesion anteriorly. Bone (C) and brain (D) windows reveal lack of any intracranial involvement, but the child has sustained a left parietal fracture and lacerations of the soft tissues of the left scalp.
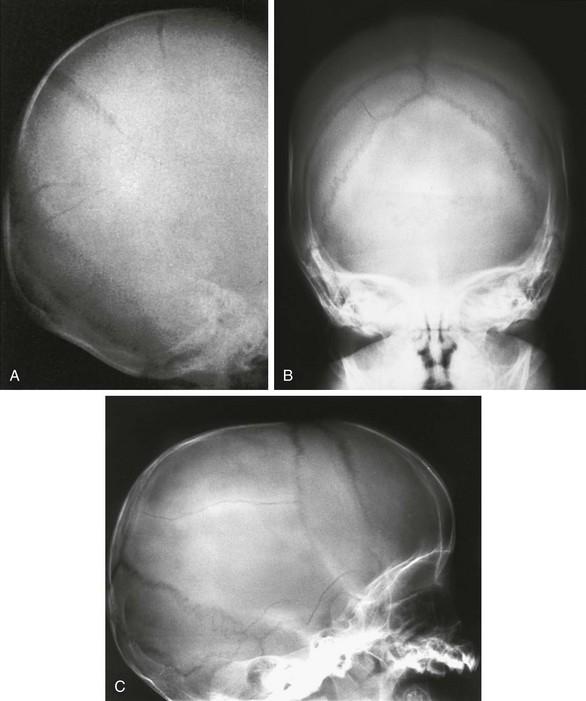
Figure 23-15 Linear fractures alone and with signs of increased intracranial pressure.
A, Multiple fractures of the right parietal bone in a 9-month-old infant. B and C, A linear parietal fracture in another child, who also has diastatic sutures denoting increased intracranial pressure.
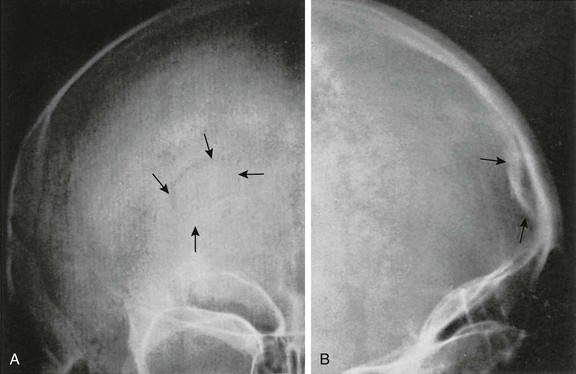
Figure 23-16 Depressed fracture of the frontal bone in a 9-year-old child.
A, A posteroanterior projection with the fracture indicated by arrows. In the medial inferior segment, the arcuate shadow of diminished density is replaced by a curved linear shadow of increased density that is caused by overlapping of the fragments in this segment. B, A lateral projection clearly demonstrating the depression of the tables (arrows).
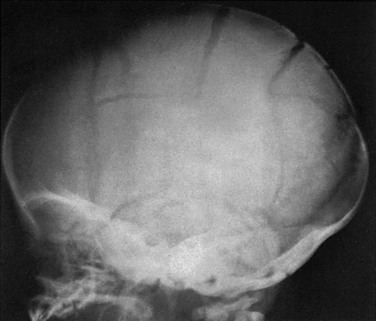
Figure 23-17 A case of nonaccidental trauma.
Comminuted diastatic fractures of both parietal bones in a 2-month-old infant are shown. Both ocular fundi contained retinal hemorrhages, and bilateral subdural hematomas were present. The child had been severely beaten by the mother.
e-Figure 23-14 A fine linear fracture of the parietal bone (arrows) in a 15-month-old infant who fell from a highchair.
e-Figure 23-18 A spurious depressed fracture (arrow) of one parietal bone.
The fracture resulted from hypoplasia and flattening of the left side of the calvaria produced a segment of the inner table of the smaller parietal bone that is central to the larger right parietal bone. The patient was an asymptomatic 7-year-old girl in whom the left side of the calvaria was smaller than the right. She had no history of previous trauma.
Linear fractures in infants and children generally heal with few or no sequelae. The relatively sharp margins become hazy, and obliteration of the fracture line itself may occur 3 to 6 months after the original injury. In some instances in which considerable comminution has occurred, bone may be resorbed locally, leaving a defect. If the dura has been disrupted at the time of the fracture, the bony edges of the fracture have a tendency to separate. Leakage of CSF from damaged underlying pia-arachnoid into the area of fracture can result in the development of a leptomeningeal cyst (a growing fracture of childhood).24,25 The leptomeninges disappear from the inner surface of the torn dura and over the underlying brain. Cysts are thought to be most common in fractures that involve the sutures because the dura is tightly bound there and more likely to rupture when the bone edges separate. Cysts have been reported after vacuum extraction when too anterior a placement of the cup was followed by widening of one coronal suture.26
By transmitting the pulsations of the brain, the cyst causes pressure atrophy of bone that is unprotected by dura, and a large defect may develop after many months or years (Fig. 23-19). The progressive changes are shown schematically in Figure 23-20. Before the development of a cyst, it is probably the pulsating CSF that begins the erosion of the internal table. Progressive enlargement of the calvarial defect has given rise to the term “growing fracture.” If the brain has been damaged by the trauma, a porencephalic cavity may underlie the calvarial defect. The scalloped margin of the defect results from differential erosion of inner and outer tables. Occasionally, an intradiploic cyst is present. These lesions generally occur after fractures in infancy and seldom are observed in fractures that occur after the fifth year.
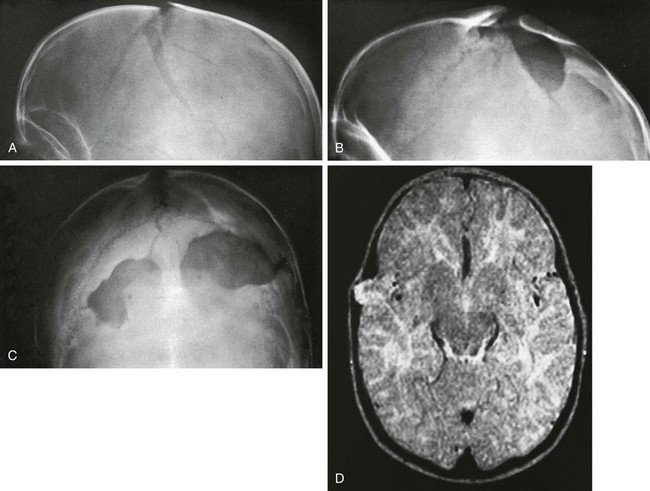
Figure 23-19 A pulsating leptomeningeal cyst with residual bilateral large defects in the calvaria.
A, Diastatic bilateral comminuted parietal fractures after a head injury during infancy. Lateral (B) and frontal (C) projections 5 years later show large bilateral defects in the sites of the earlier parietal fractures. At surgery, the dura beneath the fractures was found to be torn. The bone on the margins of the defect is sclerotic and thickened. D, Magnetic resonance imaging in another child with a leptomeningeal cyst reveals herniation of the brain outward in the right parietal region. (A, B, and C Courtesy Walter E. Berdon, MD.)
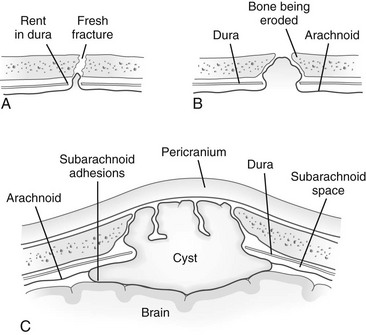
Figure 23-20 A schematic drawing of the mechanism and progressive changes in the formation of a leptomeningeal cyst.
A, Immediately after an injury occurs, fresh fractures of the parietal bone, a fresh rent in the underlying dura, and early protrusion of the arachnoid membrane into and through the fracture are seen. B, Lateral marginal erosion of bone and widening of the dural defect. C, Later incomplete cyst formation in the arachnoid as a result of adhesions, depression, and pressure atrophy of the underlying brain and leptomeninges and increases in bony and dural defects. (Courtesy Juan M. Taveras, MD.)
References
1. Axton, JHM, Levy, LF. Congenital moulding depressions of the skull. BMJ. 1965;1:1644–1647.
2. Schrager, GO. Elevation of depressed skull fracture with a breast pump. J Pediatr. 1970;77:300–301.
3. Kendall, N, Woloshin, H. Cephalhematoma associated with fracture of the skull. J Pediatr. 1952;41:125–132.
4. Zelson, C, Lee, SJ, Pearl, M. The incidence of skull fractures underlying cephalhematomas in newborn infants. J Pediatr. 1974;85:371–373.
5. Chan, MSM, Wong, YC, Lau, SPC, et al. MRI and CT findings of infected cephalhaematoma complicated by skull vault osteomyelitis, transverse venous sinus thrombosis and cerebellar haemorrhage. Pediatr Radiol. 2002;32:376–379.
6. Chorobski, J, Davis, L. Cyst formation of the skull. Surg Gynecol Obstet. 1934;58:12–31.
7. Schüller, A, Morgan, F. Cephalhematoma deformans: late developments of infantile cephalhematoma. Surgery. 1946;19:651–660.
8. Harwood-Nash, DC, Hendrick, EB, Hudson, AR. The significance of skull fractures in children: a study of 1,187 patients. Radiology. 1971;101:151–155.
9. Lloyd, DA, Carty, H, Patterson, M, et al. Predictive value of skull radiography for intracranial injury in children with blunt head injury. Lancet. 1997;349:821–824.
10. Frush, DP, O’Hara, SM, Kliewer, MA. Pediatric imaging perspective: acute head trauma—is the skull radiography useful? J Pediatr. 1998;132:553–554.
11. Leonidas, JC, Ting, W, Binkiewicz, A, et al. Mild head trauma in children: when is a roentgenogram necessary? Pediatrics. 1982;69:139–143.
12. Lloyd, DA. Skull radiographs and children with blunt head injury. Br J Surg. 1998;85:580–581.
13. Masters, SJ, McClean, PM, Arcarese, JS, et al. Skull x-ray examinations after head trauma: recommendations by a multidisciplinary panel and validation study. N Engl J Med. 1987;316:84–91.
14. Helfer, RE, Slovis, EL, Black, M. Injuries resulting when small children fall out of bed. Pediatrics. 1977;60:533–535.
15. Haydel, MJ. Clinical decision instruments for CT scanning in minor head injury. JAMA. 2005;294:1551–1553.
16. Klassen, TP, Reed, MH, Stiell, IG, et al. Variation in utilization of computed tomography scanning for the investigation of minor head trauma in children: a Canadian experience. Acad Emerg Med. 2000;7:739–744.
17. Oman, JA, Cooper, RJ, Holmes, JF, et al. Performance of a decision rule to predict need for computed tomography among children with blunt head trauma. Pediatrics. 2006;117:e238–e246.
18. Palchak, MJ, Holmes, JP, Vance, CW, et al. Does an isolated history of loss of consciousness or amnesia predict brain injuries in children after blunt head trauma? Pediatrics. 2004;113:e507–e513.
19. Schutzman, SA, Barnes, P, Duhaime, AC, et al. Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics. 2001;107:983–993.
20. Smits, M, Dippel, DWJ, de Haan, GG, et al. External validation of the Canadian CT head rule and the New Orleans criteria for CT scanning in patients with minor head injury. JAMA. 2005;294:1519–1525.
21. Stiell, IG, Clement, CM, Rowe, BH, et al. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA. 2005;294:1511–1518.
22. Beitzke, A, Stein, J. Pseudo-widening of cranial sutures as a feature of long-term prostaglandin E1 therapy. Pediatr Radiol. 1986;16:57–58.
23. Capitanio, MA, Kirkpatrick, JA. Widening of the cranial sutures: a roentgen observation during periods of accelerated growth in patients treated for deprivation dwarfism. Radiology. 1969;92:53–59.
24. Roy, S, Sarkar, C, Tandon, PN, et al. Cranio-cerebral erosion (growing fracture of the skull in children), Part I: pathology. Acta Neurochir. 1987;87:112–118.
25. Tandon, PN, Banerji, AK, Bhatia, R, et al. Cranio-cerebral erosion (growing fracture of the skull in children), Part II: clinical and pathological observations. Acta Neurochir. 1987;88:1–9.
26. Hansen, KN, Pedersen, H, Pedersen, MB. Growing skull fracture—rupture of coronal suture caused by vacuum extraction. Neuroradiology. 1987;29:502.