Chapter 61
Traumatic Heart Disease
1. What is the most common cause of cardiac injury?
Motor vehicle accidents are the most common cause of cardiac injury.
2. List the physical mechanisms of injury in cardiac trauma.
3. What is myocardial contusion?
4. Which major cardiovascular structures are most commonly involved in cardiac trauma?
Cardiac trauma most commonly involves traumatic contusion or rupture of the right ventricle (RV), aortic valve tear, left ventricle (LV) or left atrial rupture, innominate artery avulsion, aortic isthmus rupture (Fig. 61-1), left subclavian artery traumatic occlusion, and tricuspid valve tear.

Figure 61-1 Traumatic rupture of the descending thoracic aorta (arrows) at the aortic isthmus. Modified from Valji K: Vascular and Interventional Radiology, ed 2, Philadelphia, 2006, Saunders.
5. What bedside findings can be detected in patients with suspected major cardiovascular trauma?
Obvious clinical signs in patients with nonpenetrating trauma are rare. However, a bedside evaluation by an astute clinician to detect possible life-threatening cardiovascular and thoracic complications can reveal important signs in just a few minutes (Table 61-1).
TABLE 61-1
IMPORTANT SIGNS OF CARDIOVASCULAR AND THORACIC TRAUMA
| Finding | Suggested Lesions |
| Pale skin color, conjunctiva, palms, and oral mucosa | Suggests important blood loss |
| Decreased blood pressure in the left arm | Seen in patients with traumatic rupture of the aortic isthmus, pseudocoarctation, or traumatic thrombosis of the left subclavian artery |
| Decreased blood pressure in the right arm | Consider innominate artery avulsion |
| Subcutaneous emphysema and tracheal deviation | Consider pneumothorax |
| Elevated jugular venous pulse with inspiratory raise (i.e., the Kussmaul sign) | Suggests cardiac tamponade or tension pneumothorax |
| Prominent systolic V wave in the venous pulse examination | Suggests tricuspid insufficiency as a result of tricuspid valve tear |
| Nonpalpable apex or distant heart sounds | Suspect cardiac tamponade |
| Pericardial rub | Diagnostic for pericarditis |
| Pulsus paradoxus | Seen in patients with cardiac tamponade, massive pulmonary embolism, or tension pneumothorax |
| Continuous murmurs or thrills | Consider traumatic arteriovenous fistula or rupture of the sinus of Valsalva |
| Harsh holosystolic murmurs | Suspect traumatic ventricular septal defect |
| Early diastolic murmur and widened pulse pressure | Suspect aortic valve injury |
| Cervical and supraclavicular hematomas | Seen in traumatic carotid rupture |
| New focal neurological symptoms | Traumatic carotid, aortic, or great vessel dissection |
6. Can an acute myocardial infarction complicate cardiac trauma?
7. What is the most common type of myocardial infarction suffered in trauma victims?
According to the universal definition of myocardial infarction, patients who have myocardial necrosis during trauma usually suffer a type 2 myocardial infarction. This type of myocardial necrosis is secondary to direct trauma or ischemia, and is a result of a relative imbalance of either increased myocardial oxygen demand or decreased myocardial oxygen supply (e.g., coronary artery spasm, coronary embolism, anemia, arrhythmias, hypertension, anemia, or hypotension), rather than coronary occlusion caused by advanced atherosclerosis or an acute coronary thrombotic event (type 1 myocardial infarction), and is characterized by a variable increase in cardiac biomarkers with no ischemic symptoms or ECG changes.
8. What is the preferred treatment for an ST elevation acute myocardial infarction in the event of chest trauma?
The treatment of choice is emergent coronary angiography. Thrombolytic therapy caries with it a high risk of bleeding complications. The withholding of nitrates, angiotensin-converting enzyme (ACE) inhibitors, and beta-adrenergic blocking agents (β-blockers) should be considered until it is established that the patient is hemodynamically stable. Aspirin can be used in patients with no evidence of severe bleeding. Aortic balloon counterpulsation is contraindicated in patients with acute myocardial infarction, and in patients in cardiogenic shock with acute traumatic aortic regurgitation or any suspected aortic lesions. If a coronary intervention is needed, percutaneous thrombectomy and balloon angioplasty without stenting are preferred, if the patient is not a candidate for dual antiplatelet therapy due to concomitant trauma.
9. List the causes of shock in patients with cardiac trauma.
10. What workup should be considered in a patient with suspected cardiac trauma?
 Laboratory testing: Hemoglobin, hematocrit, chemistries, blood typing, and coagulation panel are routine.
Laboratory testing: Hemoglobin, hematocrit, chemistries, blood typing, and coagulation panel are routine.
 Chest radiograph: Radiographs are used to evaluate the cardiac silhouette, mediastinum, and lung fields.
Chest radiograph: Radiographs are used to evaluate the cardiac silhouette, mediastinum, and lung fields.
 Electrocardiogram: ECG is not a sensitive or specific test, but it may reveal nonspecific ST or T changes, conduction abnormalities, sinus tachycardia, premature atrial contractions, ventricular premature beats, or more complex arrhythmias suggestive of myocardial contusion. Low voltage is suggestive of pericardial effusion, whereas electrical alternans is suspicious for impending cardiac tamponade.
Electrocardiogram: ECG is not a sensitive or specific test, but it may reveal nonspecific ST or T changes, conduction abnormalities, sinus tachycardia, premature atrial contractions, ventricular premature beats, or more complex arrhythmias suggestive of myocardial contusion. Low voltage is suggestive of pericardial effusion, whereas electrical alternans is suspicious for impending cardiac tamponade.
 Bedside ultrasound: A focused assessment with sonography in trauma victims (or FAST) is encouraged, because it is an accurate screening tool for pericardial tamponade and hemopericardium, allowing timely management of life-threatening conditions, and identifying those patients at risk for complications.
Bedside ultrasound: A focused assessment with sonography in trauma victims (or FAST) is encouraged, because it is an accurate screening tool for pericardial tamponade and hemopericardium, allowing timely management of life-threatening conditions, and identifying those patients at risk for complications.
11. What are the signs of cardiac tamponade?
12. Can a patient suffering from traumatic cardiac tamponade have a normal jugular venous pulse?
13. How can one confirm the diagnosis in a patient with suspected pericardial tamponade?
A large cardiac silhouette by chest radiograph and low-voltage QRS complexes or electrical alternans in the ECG can suggest the presence of cardiac tamponade. CT can identify the size of an effusion, but cannot confirm the diagnosis. Echocardiography can confirm the diagnosis of tamponade and is the test of choice. If cardiac tamponade is suspected, an echocardiogram (with respirometry) should be ordered promptly. Echocardiography can assess the amount and localization of the pericardial effusion, and identify signs of elevated intrapericardial pressure suggesting a tamponade physiology (i.e., right atrial and RV collapse, left atrial collapse). Respirometry is a very simple technique that can be performed during the echocardiographic examination, allowing timing of the respiratory cycle with the mitral and tricuspid inflow. It is used to assess the hemodynamic effect of the pericardial effusion in the ventricular filling (using spectral Doppler analysis) and can confirm the presence of cardiac tamponade.
14. How can one treat a patient with pericardial tamponade?
15. What interventions during resuscitation and management of an unstable trauma patient can precipitate cardiac tamponade in a patient with a pericardial effusion?
16. What are the mechanisms of injury of the thoracic great vessels?
17. Describe the management of thoracic arterial lesions.
18. What are potential late complications of heart trauma?
20. Describe the cardiac complications of electrical or lightning injuries.
The effect of lightning on the heart has been called cosmic cardioversion and results in ventricular standstill and, in some reports, ventricular fibrillation. Standstill usually returns to sinus rhythm, but often the patient has a persistent respiratory arrest that causes deterioration of the rhythm. If initial ECG changes are not seen, it is unlikely that significant arrhythmias will occur later.
21. Can a patient develop a trauma-related cardiomyopathy?
Tako-tsubo cardiomyopathy, also known as transient apical ballooning, stress-induced cardiomyopathy, and simply stress cardiomyopathy, is a nonischemic cardiomyopathy in which there is sudden temporary LV systolic dysfunction. The cause is debated and appears to involve high circulating levels of catecholamines and is not specific for mechanical trauma, but can be seen in patients after both emotional and physical trauma. Because this finding is associated with emotional stress, this condition is also known as broken heart syndrome. The typical presentation of someone with tako-tsubo cardiomyopathy is a sudden onset of congestive heart failure or chest pain associated with ECG changes suggestive of an anterior wall myocardial ischemia (which may be indistinguishable initially from an acute coronary syndrome) after a major trauma. During the course of evaluation, dilation of the LV apex with a hypercontractile base of the LV is often noted by echocardiography or angiography (Fig. 61-2). It is this finding that earned the syndrome its name tako-tsubo, or “octopus trap,” in Japan, where it was first described. Evaluation of individuals with tako-tsubo cardiomyopathy may include coronary angiography, which generally does not reveal any significant coronary artery disease. Provided that the individual survives the initial presentation, the LV function usually improves within several months with medical therapy.
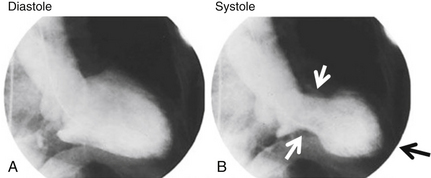
Figure 61-2 Left ventriculography of a patient who developed a tako-tsubo cardiomyopathy following a crush injury, showing the classic apical ballooning of the left ventricle. A is during diastole; B is during systole. There is systolic contraction of the base of the heart (white arrows) but apical ballooning of the left ventricular apex (black arrow). Modified from Daroff R, Fenichel G, Jankovic J, et al: Bradley’s Neurology in Clinical Practice, ed 6, Edinburgh, 2012, Saunders.
Bibliography, Suggested Readings, and Websites
1. Bansal, M.K., Maraj, S., Chewaproug, D., et al. Myocardial contusion injury: redefining the diagnostic algorithm. Emerg Med J. 2005;22:465–469.
2. Chockalingam, A., Mehra, A., Dorairajan, S., et al. Acute left ventricular dysfunction in the critically ill. Chest. 2010;138:198–207.
3. Cook, C.C., Gleason, T.G. Great vessel and cardiac trauma. Surg Clin North Am. 2009;89:797–820.
4. Gianni, M., Dentali, F., Grandi, A.M., et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–1529.
5. Holanda, M.S., Domínguez, M.J., López-Espadas, F., et al. Cardiac contusion following blunt chest trauma. Eur J Emerg Med. 2006;13:373–376.
6. Kapoor, D., Bybee, K.A. Stress cardiomyopathy syndrome: a contemporary review. Curr Heart Fail Rep. 2009;6:265–271.
7. Karmy-Jones, R., Jurkovich, G.J. Blunt chest trauma. Curr Probl Surg. 2004;41:211–380.
8. Khandhar, S.J., Johnson, S.B., Calhoon, J.H. Overview of thoracic trauma in the United States. Thorac Surg Clin. 2007;17:1–9.
9. Madias, C., Maron, B.J., Weinstock, J., et al. Commotio cordis—sudden cardiac death with chest wall impact. J Cardiovasc Electrophysiol. 2007;18:115–122.
10. Mandavia, D.P., Joseph, A. Bedside echocardiography in chest trauma. Emerg Med Clin North Am. 2004;22:601–619.
11. McGillicuddy, D., Rosen, P. Diagnostic dilemmas and current controversies in blunt chest trauma. Emerg Med Clin North Am. 2007;25:695–711.
12. Moore, E.E., Malangoni, M.A., Cogbill, T.H., et al. Organ injury scaling. IV: Thoracic vascular, lung, cardiac, and diaphragm. J Trauma. 1994;36:299–300.
13. Reissig, A., Copetti, R., Kroegel, C. Current role of emergency ultrasound of the chest. Crit Care Med. 2011;39:839–845.
14. Ritenour, A.E., Morton, M.J., McManus, J.G., et al. Lightning injury: a review. Burns. 2008;34:585–594.
15. Thygesen, K., Alpert, J.S., White, H.D. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–2195.
16. Wolf, S.J., Bebarta, V.S., Bonnett, C.J., et al. Blast injuries. Lancet. 2009;374:405–415.


