CHAPTER 382 Traumatic Cerebral Aneurysms Secondary to Penetrating Intracranial Injuries
Traumatic intracranial aneurysms may be the result of either penetrating or nonpenetrating trauma.1–3 Traumatic aneurysms were first described in 1895 by Guibert,4 and despite the common occurrence of head trauma, they are rare entities that represent less than 1% of all intracranial aneurysms.5–13 The risk of a traumatic intracranial aneurysm developing depends on the mechanism of injury, with aneurysm formation being much less likely after closed head injury than after penetrating trauma. In addition to their occurrence after traditional trauma, traumatic aneurysms have been reported to occur iatrogenically, such as after transsphenoidal surgery,14–18 sinus surgery,17,19 ventricular taps,20,21 stereotactic brain biopsy,22 and endoscopic third ventriculostomy.23
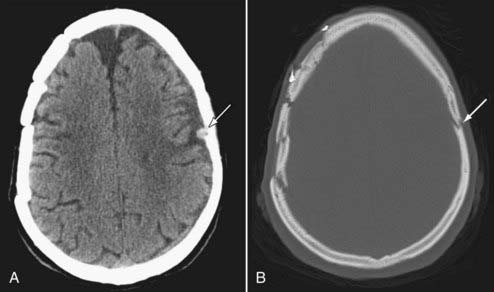
Penetrating trauma can be divided into low-velocity injuries, such as those created by knives, screwdrivers, and shotgun pellets,24 or high-velocity injuries caused by missiles such as bullets and shrapnel. South Africa has provided much of the literature with respect to low-velocity injuries, which are prevalent in this region, with stab wounds to the brain accounting for up to 6% of all trauma admissions.7,25 The incidence of aneurysm formation after this type of injury may be as high as 10% to 12%.7,25,26 Traumatic aneurysms can occur as a result of skull fractures as well (Figs. 382-1 and 382-2). The aneurysm can result directly from depressed bone fragments injuring an underlying vessel or dispersed bone fragments from a penetrating injury (e.g., shrapnel).
With respect to missile injuries, conflicts in Lebanon, Iraq, and Iran have demonstrated aneurysm formation in 0.1% to 8% of patients sustaining this type of injury. The incidence is related to velocity, with lower velocity shrapnel injuries having a higher incidence of aneurysm formation than higher velocity bullet injuries.1,3,5,27 The American experience was obtained during the Vietnam War and reported by Ferry and Kempe, who demonstrated only two traumatic aneurysms in 2187 patients with penetrating head trauma, primarily gunshot wounds.27
Despite the rarity of traumatic intracranial aneurysms, they have a mortality rate of 30%.5 This outcome is related more to the primary injury than to the aneurysm itself.3 However, it is important to make the diagnosis and offer surgical treatment because secondary insults affect the neurological outcome of patients.
Pathology
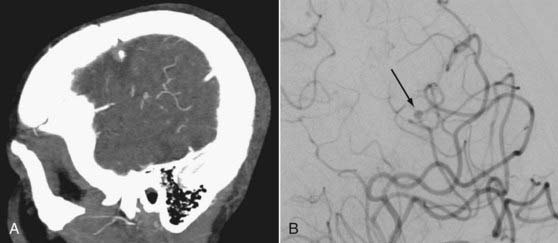
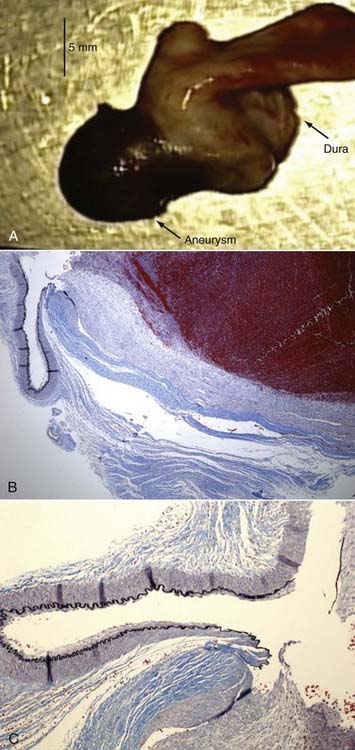
In penetrating trauma, the traumatic event disrupts the elements of the vessel wall, which may involve varying amounts of the intima, media, and adventitia.28 Depending on the degree of involvement of the different internal structures, a false aneurysm, true aneurysm, dissection, or fistula may occur. An example of vessel changes with a traumatic aneurysm is shown in Figure 382-3. The findings are from a patient who suffered a severe traumatic brain injury with bilateral skull fractures that required evacuation of a subdural hematoma on the right. A pial artery aneurysm was diagnosed 5 months after the injury (see Figs. 382-1 and 382-2). The aneurysm grew significantly in size and was removed surgically. The aneurysm showed loss of the internal elastic lamina and smooth muscle in the media and an increase in size of the adventitia.
Traumatic aneurysms occur distally in the vascular tree, in contrast to the proximal bifurcation site of saccular aneurysms. This peripheral location reflects the underlying mechanism of injury. The anterior circulation is most often affected, with the peripheral branches of the middle cerebral artery being the most frequent site, followed by branches of the pericallosal vessels.3
In penetrating injuries, the velocity of the projectile correlates inversely with aneurysm formation; that is, the lower the velocity, the more likely for aneurysm formation to occur. For example, traumatic aneurysms are 14 times more likely with shrapnel injuries than with bullet injuries, which are of higher velocity.3 Shotgun29,30 and low-caliber29,31,32 wounds also have a higher incidence of traumatic aneurysm formation than do injuries cased by high-velocity missiles. Bullets with higher velocity and thus greater kinetic injury are more likely to rupture a vessel than merely damage the wall.3 Further support for this theory is the very high incidence of traumatic aneurysms after stab wounds to the brain in the South African experience.7,25,26 Traumatic aneurysms have also been associated with skull fractures, and in this type of penetrating trauma it has been postulated that momentary herniation of the cerebral cortex and vessel through the fracture results in aneurysm formation.33 Figures 382-1 to 382-3 demonstrate an example of a distal middle cerebral artery pial artery aneurysm underlying a skull fracture.
Traumatic fistulas are abnormal connections between the intracranial arterial and venous circulation that can occur after severe or even relatively minor nonpenetrating trauma. Occasionally, they result from penetrating trauma, with the most common location being the cavernous sinus with the formation of a carotid–cavernous fistula—an acquired communication between the intracranial carotid artery and the cavernous sinus.34 This communication may occur at the time of trauma or in delayed fashion if a false aneurysm is created that ruptures later. Dural fistulas may also occur after penetrating trauma. In this type of fistula, the abnormal communication between the intracranial arterial and venous circulation lies within the dura.35 These dural fistulas may involve the cavernous sinus and other venous sinuses, including the transverse and sigmoid sinuses.36–39
Much less common is the formation of dissecting aneurysms after nonpenetrating trauma. They may occur at the skull base and involve the internal carotid artery and vertebrobasilar system. Dissecting aneurysms occur when injury to one or more of the arterial layers allows blood to force its way between the vessel layers along a dissection plane9 and create an intimal flap.40 This intimal flap may act as a nidus for embolic material or may occlude the arterial lumen. Occasionally, dissections originate within the media or adventitia, and in this situation, rupture may occur through the adventitia, with resultant subarachnoid hemorrhage or pseudoaneurysm formation.41 Dissections are more common after nonpenetrating trauma42–44 and may occur spontaneously.45,46 Dissections with pseudoaneurysm formation of the carotid artery can occur as a result of fractures of the skull base or clinoid secondary to traction on the artery at the dural ring.
Clinical Findings
The initial signs and symptoms in patients with head injuries, regardless of whether they have traumatic intracranial aneurysms, are largely related to the primary brain injury, with the initial Glasgow Coma Scale score being a good predictor of outcome.3,47 Secondary manifestations are related to the location and type of the vascular injury. In aneurysms involving the peripheral vascular tree, there is delayed neurological deterioration, usually within 3 weeks of the injury.7 Because most traumatic aneurysms are false aneurysms, intracranial hemorrhage is often the reason for this deterioration, but cerebral edema from the initial coexisting hemorrhage or stroke may be responsible. Patients with multiple episodes of hemorrhage tend to do poorly,48 so it is best to have a high index of suspicion for traumatic aneurysms and make the diagnosis before its overt clinical manifestations appear.
In patients with aneurysms involving the infraclinoid internal carotid artery, severe and life-threatening epistaxis can be the initial event if the arterial injury communicates with a sphenoidal sinus fracture.31,49–53 Aneurysms in this location may also be manifested as a bruit, chemosis, exophthalmos, visual loss, and cranial neuropathies referable to the cavernous sinus and formation of a carotid-cavernous fistula.15,49,50 The extent of these symptoms largely depends on the magnitude of the arterial injury and the adequacy of venous drainage.35
Dural fistulas are often manifested in delayed fashion, with pulsatile tinnitus or headaches being the only features. A less common finding is neurological deterioration secondary to an embolic stroke, which occurs with dissecting aneurysms involving the intracranial vessels, or a mass effect secondary to an enlarging unruptured pseudoaneurysm, particularly in children.54
Diagnosis
The most common cause of subarachnoid hemorrhage is trauma, so the diagnosis of a traumatic intracranial aneurysm requires a high index of suspicion. Making the diagnosis is important because patients with multiple episodes of hemorrhage or neurological insults do poorly.48 Computed tomography is usually the first investigation, and it may demonstrate nonspecific hemorrhages, infarctions, and skull base fractures. Penetrating trauma is often associated with intracranial hemorrhage, and after missile injuries, concomitant intracerebral hemorrhage is found in 39% to 80% of patients,35 with 26% having subdural hemorrhages.3 In low-velocity penetrating injuries, de Trevou and van Dellen demonstrated that 50% of patients had evidence of an intracerebral hemorrhage.26
Cerebral angiography is the “gold standard” and should be performed in all cases of penetrating trauma.7,55,56 Angiography is particularly important in patients with orbitopterional injuries, penetrating fragments, and subarachnoid, intracerebral, or subdural hemorrhage.3,5,26,57 In penetrating trauma, traumatic aneurysms may be visualized on angiography as early as 2 hours after the injury, but the majority of aneurysms are angiographically apparent in 2 to 3 weeks, with a mean of 20 days (median, 13 days).5 Therefore, it has been suggested that the first angiogram should be performed at the beginning of the second week after injury.7 In patients in whom there is a higher probability of a traumatic aneurysm being present or developing (e.g., those with stab wounds), angiography shortly after admission should be considered. Computed tomographic angiography can also be performed as a screening study and may reveal an unsuspected aneurysm. The timing of angiography is important, and it is not unusual for the first angiogram to be negative in patients with penetrating trauma.1,31,58 Twenty percent of traumatic aneurysms are multiple, and each individual aneurysm may regress, enlarge, or form in delayed fashion.36 Therefore, most authors agree that a follow-up angiogram should be obtained even if the initial one was negative. The second angiogram should be performed at least 2 to 3 weeks after injury, and it could be argued that a third angiogram should be obtained 6 weeks after injury. Traumatic internal carotid artery aneurysms occur relatively frequently in children (5% to 39% of pediatric intracranial aneurysms) and have a propensity to bleed weeks after the initial trauma. Blood in the basilar cisterns after closed head trauma in children should prompt both immediate and delayed angiographic evaluation.59
Treatment
Surgery has been the traditional method of therapy, with ligation of the carotid artery in the neck historically used for traumatic aneurysms involving the intracranial internal carotid artery.60 Some traumatic intracranial aneurysms have been documented to disappear on repeated angiograms,1,36 with Amirjamshidi and coworkers reporting that 19.4% of the aneurysms in their patients disappeared.61 This finding has not been supported by all authors, and most recommend that once a traumatic aneurysm has been diagnosed, therapy should be instituted. The principle of managing a saccular aneurysm is to exclude the aneurysmal bulge from the circulation by clipping or coiling, with preservation of the parent vessel and its branches. Traumatic aneurysms, however, are mostly false aneurysms, so this approach is not often possible; successful clipping has been reported, but it is unusual.23,62,63 Therefore, with traumatic aneurysms, preoperative planning must include the possibility of excising the involved vessel, as well as the high probability of rupture intraoperatively.
In very distal vessels, the likelihood of an ischemic event after resection of the aneurysm is low, and these aneurysms are often excised with no complications.3,5,64 In more proximal vessels, preparation for a vascular bypass should be considered, and the surgical approach should allow access to the superficial temporal artery, the saphenous vein, or both. In addition to a vascular bypass, an interposition graft with the superficial temporal artery can be placed.65 Some aneurysms may not be amenable to either resection or bypass; in such cases, wrapping with Dacron mesh or muslin may be performed.
Endovascular techniques have advanced over the past 3 decades, and intravascular embolization and occlusion now play a larger role in the management of intracranial traumatic arterial injuries.66–69 Endovascular therapy has not been a mainstay of treatment of traumatic aneurysms in the peripheral vascular tree because of the high incidence of false aneurysms and the risk for rupture. Recently, however, coils have been successfully placed in traumatic aneurysms.69,70
Endovascular therapy has become more important for vascular injuries involving the skull base.71 Traumatic aneurysms involving the skull base are difficult to access and control surgically. With carotid injuries, options include endovascular occlusion of the carotid artery at the skull base, a bypass graft, or rarely, direct repair of the vessel. Stenting may play an important role in the future; however, the need for antiplatelet therapy after stent placement limits the use of this treatment modality in the setting of trauma. Before carotid occlusion, the collateral circulation needs to be evaluated by balloon test occlusion. Adequate collateral circulation is defined as symmetrical angiographic filling of both hemispheres. Awake patients are also examined continuously for neurological deficits. In patients with evidence of adequate cross-flow and collateral flow based on transcranial Doppler studies, angiography, and balloon test occlusion, simple endovascular occlusion can be performed.53,72 Patients who deteriorate clinically or whose middle cerebral artery transcranial Doppler velocity decreases by 60% have inadequate collateral flow.73 In these patients, alternative therapies have to be considered, including direct surgical repair or endovascular treatment of the carotid artery in the skull base, as well as the cavernous sinus, but such treatment has had variable success.74–76 Most authors would advocate an extracranial-to-intracranial bypass.53 A saphenous vein bypass graft can be used, with sacrifice of the internal carotid artery surgically.65 In some patients, both endovascular and surgical techniques can be used simultaneously to achieve optimal results.65
Aarabi B. Management of traumatic aneurysms caused by high-velocity missile head wounds. Neurosurg Clin N Am. 1995;6:775-796.
Aarabi B. Traumatic aneurysm of brain due to high velocity missile head wounds. Neurosurgery. 1988;22:1056-1063.
Amirjamshidi A, Rahmat H, Abbassioun K. Traumatic aneurysms and arteriovenous fistulas of intracranial vessels associated with penetrating head injuries occurring during war: principles and pitfalls in diagnosis and management. A survey of 31 cases and review of the literature. J Neurosurg. 1996;84:769-780.
Buckingham MK, Crone CR, Ball WS, et al. Traumatic intracranial aneurysms in childhood. Neurosurgery. 1988;22:398-408.
Cohen JE, Gomori JM, Segal R, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008;63:476-485.
de Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: the timing of angiography in patients with weapon already removed. Neurosurgery. 1992;31:905-911. discussion 911-912
Haddad FS. Nature and management of penetrating head injuries during the civil war in Lebanon. Can J Surg. 1978;21:233-240.
Hemphill JC, Gress DR, Halbach VV. Endovascular therapy of traumatic injuries of the intracranial cerebral arteries. Crit Care Clin. 1999;15:811-829.
Hetzel A, von Reutern G, Wernz MG, et al. The carotid compression test for therapeutic occlusion of the internal carotid artery: comparison of angiography with transcranial Doppler sonography. Cerebrovasc Dis. 2000;10:194-199.
Higashida RT, Halbach VV, Dowd C, et al. Interventional neurovascular treatment of traumatic carotid and vertebral artery lesions: results in 234 cases. AJR Am J Roentgenol. 1989;153:577-582.
Kumar M, Kitchen ND. infective and traumatic aneurysms. Neurosurg Clin N Am. 1998;9:577-586.
Lempert TE, Halbach VV, Higashida RT, et al. Endovascular treatment of pseudoaneurysms with electrolytically detachable coils. AJNR Am J Neuroradiol. 1998;19:907-911.
Levy ML, Litofsky SN, Rezai A, et al. The significance of subarachnoid hemorrhage following penetrating craniocerebral injury; correlation with angiography and outcome in a civilian population. Neurosurgery. 1993;32:532-540.
Schuster JM, Santiago P, Elliot JP, et al. Acute traumatic posteroinferior cerebellar artery aneurysms: report of three cases. Neurosurgery. 1999;45:1465-1468.
Uzan M, Cantasdemir M, Seckin MS, et al. Traumatic intracranial carotid tree aneurysms. Neurosurgery. 1998;43:1314-1320.
Yokota H, Tazaki H, Murayama K, et al. Traumatic cerebral aneurysm: 94 cases from the literature and cases observed by the authors. No Shinkei Geka. 1983;11:521-528.
1 Aarabi B. Traumatic aneurysm of brain due to high velocity missile head wounds. Neurosurgery. 1988;22:1056-1063.
2 Bostrom K, Helander CG, Lindgren SO. Blunt basilar head trauma: rupture of posterior inferior cerebellar artery. Forensic Sci Int. 1992;53:61-68.
3 Han MH, Sung MW, Chang KH, et al. Traumatic pseudoaneurysm of the intracavernous ICA presenting with massive epistaxis: imaging diagnosis and endovascular treatment. Laryngoscope. 1994;104:370-377.
4 Guibert J. Anevrisme arteriel de la carotide interne au niveau du sinus cavernuex, communication avec le sinus sphenoidal droit, hemorrhagies nasales, mort, autopsie. Ann Oculist. 1895;113:314-318.
5 Aarabi B. Management of traumatic aneurysms caused by high-velocity missile head wounds. Neurosurg Clin N Am. 1995;6:775-796.
6 Fleisher AS, Patton JM, Tindall GT. Cerebral aneurysms of traumatic origin. Surg Neurol. 1975;4:233-239.
7 Kiek CF, de Villiers JC. Vascular lesions due to transcranial stab wounds. J Neurosurg. 1984;60:42-46.
8 McLaughlin MR, Wahlig JB, Kaufman AM, et al. Traumatic basilar aneurysm after endoscopic third ventriculostomy: case report. Neurosurgery. 1997;41:1400-1403.
9 Melvill RL, de Villiers JC. Peripheral cerebral arterial aneurysms caused by stabbing. S Afr Med J. 1977;51:471-473.
10 Mendel R, Carter L. Intracranial arterial injury. In: Carter L, Spetzler R, Hamilton M, editors. Neurovascular Surgery. New York: McGraw-Hill; 1995:1301.
11 Shinoda S, Murata H, Waga S, et al. Bilateral spontaneous dissection of the posteroinferior cerebellar arteries: case report. Neurosurgery. 1998;43:357-359.
12 van Dellen JR. Intracavernous traumatic aneurysms. Surg Neurol. 1980;13:203-207.
13 Wortzman D, Tucker WS, Gershater R. Traumatic aneurysm in the posterior fossa. Surg Neurol. 1980;13:329-331.
14 Ali S, Bihari J. Intracranial traumatic aneurysm following hypophysectomy. J Laryngol Otol. 1981;95:749-755.
15 Awad I, Sawhny B, Little JR. Traumatic postsurgical aneurysm of the intracavernous carotid artery: a delayed presentation. Surg Neurol. 1982;18:54-57.
16 Dolenc VV, Lipovsek M, Slokan S. Traumatic aneurysm and carotid-cavernous fistula following transsphenoidal approach to pituitary adenoma: treatment by transcranial operation. Br J Neurosurg. 1999;13:185-188.
17 Levy ML, Litofsky SN, Rezai A, et al. The significance of subarachnoid hemorrhage following penetrating craniocerebral injury; correlation with angiography and outcome in a civilian population. Neurosurgery. 1993;32:532-540.
18 Morard M, de Tribolet N. Traumatic aneurysm of the posterior inferior cerebellar artery: case report. Neurosurgery. 1991;29:438-441.
19 Barret JH, Lawrence VL. Aneurysm of the internal carotid artery as a complication of mastoidectomy. Arch Otolaryngol. 1960;72:366-368.
20 Lam CH, Montes J, Farmer JP, et al. Traumatic aneurysm from shaken baby syndrome: case report. Neurosugery. 1996;39:1252-1255.
21 Sahrakar K, Boggan JE, Salamat MS. Traumatic aneurysm: a complication of stereotactic brain biopsy: case report. Neurosurg. 1995;36:842-846.
22 Salar G, Mingrino S. Traumatic intracranial internal carotid aneurysms due to gunshot wounds: case report. J Neurosurg. 1978;49:100-102.
23 Lylyk P, Viñuela F, Campos J, et al. Diagnosis and endovascular therapy of vascular lesions in the cavernous sinus. Acta Radiol Suppl. 1986;369:584-585.
24 Courville CB. Traumatic aneurysm of an intracranial artery: description of a lesion incident to a shotgun wound of the skull and brain. Bull L A Neurol Soc. 1960;25:48-54.
25 Meguro K, Rowed DW. Traumatic aneurysms of the posterior inferior cerebellar artery caused by fracture of the clivus. Neurosurgery. 1985;16:666-668.
26 de Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: the timing of angiography in patients with weapon already removed. Neurosurgery. 1992;31:905-911. discussion 911-912
27 Ferry DJJr, Kempe LG. False aneurysm secondary to penetration of the brain through orbitofacial wounds. J Neurosurg. 1972;36:503-506.
28 Britz GW, Mayberg MR. Pathology of cerebral aneurysms and subarachnoid hemorrhage. In: Welch KMA, Caplan LR, Reis DJ, et al, editors. Primer on Cerebrovascular Diseases. New York: Academic Press; 1997:498-502.
29 Acosta C, Williams PE, Clark K. Traumatic aneurysms of the cerebral vessels. J Neurosurg. 1972;36:531-536.
30 Asari S, Nakamura S, Yamada O, et al. Traumatic aneurysm of peripheral cerebral arteries: report of two cases. J Neurosurg. 1977;46:795-803.
31 Rumbaugh CL, Bergerson RT, Talalla A, et al. Traumatic aneurysms of the cortical cerebral arteries. Radiology. 1970;96:49-54.
32 Sadar ES, Jane JA, Lewis LW, et al. Traumatic aneurysms of the intracranial circulation. Surg Gynecol Obstet. 1973;137:59-67.
33 Rahimizadeh A, Abtahi H, Daylami MS, et al. Traumatic cerebral aneurysms caused by shell fragments: report of four cases and review of the literature. Acta Neurochir (Wien). 1987;84:93-98.
34 Greatz KW, Imhof HG, Valavanis A. Traumatic carotid cavernous sinus fistula due to a gun shot injury. Int J Oral Maxillofac Surg. 1991;20:280-282.
35 Hemphill JC, Gress DR, Halbach VV. Endovascular therapy of traumatic injuries of the intracranial cerebral arteries. Crit Care Clin. 1999;15:811-829.
36 Halbach VV, Higashida RT, Hieshima GB, et al. Dural fistulas involving the transverse and sigmoid sinuses: results of treatment in 28 patients. Radiology. 1987;163:443-447.
37 Halbach VV, Hieshima GB, Higashida RT, et al. Carotid cavernous fistulae: indications for urgent treatment. AJR Am J Roentgenol. 1987;149:587-593.
38 Halbach VV, Higashida RT, Hieshima GB, et al. Transvenous embolization of dural fistulas involving the cavernous sinus. AJNR Am J Neuroradiol. 1989;10:377-383.
39 Halbach VV, Higashida RT, Barnwell SL, et al. Transarterial platinum coil embolization of carotid-cavernous fistulas. AJR Am J Roentgenol. 1991;12:429-433.
40 Yokota H, Tazaki H, Murayama K, et al. Traumatic cerebral aneurysm: 94 cases from the literature and cases observed by the authors. No Shinkei Geka. 1983;11:521-528.
41 Yonas H, Agamanolis D, Takaoka Y, et al. Dissecting intracranial aneurysms. Surg Neurol. 1977;8:407-415.
42 Auer RN, Kreck J, Butt JC. Delayed symptoms and death after minor head injury with occult vertebral injury. J Neurol Neurosurg Psychiatry. 1994;57:500-502.
43 Jafar JJ, Kamiryo T, Chiles BW, et al. A dissecting aneurysm of the posterior inferior cerebellar artery: case report. Neurosurgery. 1998;3:353-356.
44 Kumar M, Kitchen ND. infective and traumatic aneurysms. Neurosurg Clin N Am. 1998;9:577-586.
45 Paullus WSJr, Norwood CW, Morgan HW. False aneurysm of the cavernous carotid artery and progressive external ophthalmoplegia after transsphenoidal hypophysectomy: case report. J Neurosurg. 1979;51:707-709.
46 Schuster JM, Santiago P, Elliot JP, et al. Acute traumatic posteroinferior cerebellar artery aneurysms: report of three cases. Neurosurgery. 1999;45:1465-1468.
47 Aarabi B, Koleini MK. Traumatic aneurysms due to missile head wounds: report of twenty cases. Iran J Med Sci. 1989;14:26-32.
48 Buckingham MK, Crone CR, Ball WS, et al. Traumatic intracranial aneurysms in childhood. Neurosurgery. 1988;22:398-408.
49 Bavinzski G, Killer M, Knosp E, et al. False aneurysms of the intracavernous carotid artery—report of 7 cases. Acta Neurochir (Wien). 1997;139:37-43.
50 Bavinzski G, Killer M, Gruber A, et al. Treatment of post-traumatic carotico-cavernous fistula using electrolytically detachable coils: technical aspects and preliminary experience. Neuroradiology. 1997;39:81-85.
51 Dial DL, Maurer GB. Intracranial aneurysms: report of 13 cases. Am J Surg. 1937;35:2-21.
52 Jackson FE, Augusta FA, Sazima HJ, et al. Head injury and delayed epistaxis: report of case of rupture of traumatic aneurysms of internal carotid artery due to grenade fragment wound received in Vietnam conflict. J Trauma. 1970;10:1158-1167.
53 Teitelbaum GP, Bernstein K, Choi S, et al. Endovascular coil occlusion of a traumatic basilar-cavernous fistula: technical report. Neurosurgery. 1998;42:1394.
54 Endo S, Takaku A, Aihara H, et al. Traumatic cerebral aneurysm associated with widening skull fracture. Childs Brain. 1980;6:131-139.
55 Achram M, Rizk G, Haddad FS. Angiographic aspects of traumatic intracranial aneurysms following war injuries. Br J Radiol. 1980;53:1144-1149.
56 Haddad FS. Nature and management of penetrating head injuries during the civil war in Lebanon. Can J Surg. 1978;21:233-240.
57 Lempert TE, Halbach VV, Higashida RT, et al. Endovascular treatment of pseudoaneurysms with electrolytically detachable coils. AJNR Am J Neuroradiol. 1998;19:907.
58 Capanna AH. Traumatic intracranial aneurysms and Gradenigo’s syndrome secondary to gunshot wound. Surg Neurol. 1984;22:263-266.
59 Kneyber MCJ, Rinkel GJE, Ramos LMP, et al. Early posttraumatic subarachnoid hemorrhage due to dissecting aneurysms in three children. Neurology. 2005;65:1663-1665.
60 Cooper A. Account of the first successful operation performed on the common carotid artery for aneurysm in the year 1808: with the post-mortem examination, 1821. Guys Hosp Rep (Lond). 1836;1:53-58.
61 Amirjamshidi A, Rahmat H, Abbassioun K. Traumatic aneurysms and arteriovenous fistulas of intracranial vessels associated with penetrating head injuries occurring during war: principles and pitfalls in diagnosis and management. A survey of 31 cases and review of the literature. J Neurosurg. 1996;84:769-780.
62 Ding MX. Traumatic aneurysm of the intracavernous part of the internal carotid artery presenting with epistaxis: case report. Surg Neurol. 1988;30:65-67.
63 Serbinenko FA, Lazarev VA. Use of balloon catheter in cases of traumatic pseudoaneurysm of the carotid artery complicated by profuse nosebleed. Zh Vopr Neirokhir. 1981;6:9-16.
64 Pozzati E, Gaist G, Poppi M. Resolution of occlusion in spontaneously dissected carotid arteries. J Neurosurg. 1982;56:857-860.
65 Horowitz MB, Kopitnik TA, Landreneau F, et al. Multidisciplinary approach to traumatic intracranial aneurysms secondary to shotgun and handgun wounds. Surg Neurol. 1999;51:31-42.
66 Chen D, Concus AP, Halbach VV, et al. Epistaxis originating from traumatic pseudoaneurysm of the internal carotid artery: diagnosis and endovascular therapy. Laryngoscope. 1998;108:326-331.
67 Higashida RT, Halbach VV, Dowd C, et al. Interventional neurovascular treatment of traumatic carotid and vertebral artery lesions: results in 234 cases. AJR Am J Roentgenol. 1989;153:577-582.
68 Sure U, Becker R, Petermeyer M, Bertalanffy H. Aneurysm of the posterior inferior cerebellar artery caused by a traumatic perforating artery tear-out mechanism in a child. Childs Nerv Syst. 1999;15:354-356.
69 Cohen JE, Gomori JM, Segal R, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008;63:476-485.
70 Lassman LP, Ramani PS, Sengupta RP. Aneurysms of peripheral cerebral arteries due to surgical trauma. Vasc Surg. 1974;8:1-5.
71 Lister JR, Sypert GW. Traumatic false aneurysm and carotid-cavernous fistula: a complication of sphenoidotomy. Neurosurgery. 1979;5:473-475.
72 Scharfetter F, Fodisch HJ, Menardi G, et al. Falsches Aneurysma der Arteria gyri angularis durch Gefassverletzung bei einer Ventrikpunktion. Acta Neurochir (Wien). 1976;33:123-132.
73 Hetzel A, von Reutern G, Wernz MG, et al. The carotid compression test for therapeutic occlusion of the internal carotid artery: comparison of angiography with transcranial Doppler sonography. Cerebrovasc Dis. 2000;10:194-199.
74 Dolenc V. Direct microsurgical repair of intracavernous vascular lesions. J Neurosurg. 1983;58:824-831.
75 Fabian G. Traumatisches Aneurysma der Carotis interna in der Keilbeinhole. Hals-Nasen-Ohrenbeilk. 1952;3:346-349.
76 Uzan M, Cantasdemir M, Seckin MS, et al. Traumatic intracranial carotid tree aneurysms. Neurosurgery. 1998;43:1314-1320.