Traumatic brain injury
PATRICIA A. WINKLER, PT, DSc, NCS
After reading this chapter the student or therapist will be able to:
1. Describe the application of current concepts in motor control and motor learning theories for clients with traumatic brain injury.
2. Understand the meaning of impairment, activity limitation, and participation limitation and their interrelationships as they apply to clients with traumatic brain injury.
3. Prescribe methods of examining, evaluating, and developing interventions for clients with brain injuries on the basis of task, impairment, and activity limitation analysis.
4. Describe prognosis and outcomes for clients with traumatic brain injury.
5. Differentiate between development of basic movement patterns and motor skills.
6. Understand the role of synergy formation, synergy selection and modification, and anticipatory and feedback information as used in motor skills.
7. Describe the long-term effects of different types of feedback and practice on learning.
Traumatic brain injury (TBI) is defined as a blow or jolt to the head or a penetrating head injury that disrupts the function of the brain. Not all blows or jolts to the head result in a TBI. The severity of such an injury may range from mild—a brief change in mental status or consciousness—to severe—an extended period of unconsciousness or amnesia after the injury. A TBI can result in short- or long-term problems with independent function.1
Overview of brain injury
Epidemiology of traumatic brain injury
One and three-quarter million people sustain a TBI every year.1 Of these, 1.3 million are treated in emergency departments and 275,000 injuries are severe enough to require hospitalization.2 Fifty-two thousand people die yearly of TBI, 80,000 injuries result in disabilities, and 5.3 million people are living with permanent disabilities from TBI. It is the leading killer and disabler of children and young adults. Motor vehicle crashes cause 20% of all TBIs, falls cause 28%, violence causes 11% (the majority from firearms), and sports and recreation account for 10%. Child abuse accounts for 64% of infant brain injuries.1 Fifty-thousand children sustain bicycle-related brain injuries, and 400 of them die.3 Two thirds of firearm-related TBIs are suicidal. Falls are the leading cause of TBI in people aged 65 years and older, with 11% proving fatal. The incidence of TBI is 506.4 per 100,000 population, with 43% of those hospitalized having long-term activity limitation.4
Population of clients with brain injury
The incidence of brain injuries is higher for the male population than for the female population by more than 2:1. Most of those injured are 15 to 24 years old.4 The greatest risk of injury is for those younger than 10 years old or older than 74. American Indians and African Americans have the highest rate of TBI. People in lower socioeconomic status also have a higher rate of injury.
Mechanisms of injury
There are four main types of injury, as follows:
1. Those from external forces hitting the head or the head hitting hard enough to cause brain movement. Injuries include those with skull fracture and those without skull fracture (closed head injuries). Direct blows to the head can cause coup injuries (at the site of impact) and contrecoup injuries (distant from the site of impact).
2. Severe acceleration and deceleration of the head can cause TBI without the head hitting an object. An example is shaken baby syndrome.
3. Blast injuries have become very common in the past 10 years, mainly affecting military personnel.
4. Penetrating objects cause direct cellular and vascular damage. Injuries to the face and neck can cause brain injury by damaging the blood supply to the brain.5
Pathophysiology of injury
Primary damage
Contusions—a bruise or bleeding on the brain—and lacerations can occur with or without skull fractures. Either an object hits the head, neck, or face, or the head hits an object. Damage can be to any area of the brain. Occipital blows are more likely to produce contusions than are frontal or lateral blows. Areas in which the cranial vault is irregular, such as on the anterior poles, undersurface of the temporal lobes, and undersurface of the frontal lobes, are commonly injured. Lacerations of blood vessels within the brain itself or of blood vessels that feed the brain from the neck or face reduce the flow of blood carrying oxygen to the brain. Contusions and lacerations can also injure the cranial nerves. The most commonly injured are the optic, vestibulocochlear, oculomotor, abducens, and facial nerves. Lacerations of the dura or in the arachnoid space may cause cerebrospinal fluid to discharge from the nose (cerebrospinal fluid rhinorrhea discharge increases with neck flexion, coughing, or straining).6 An example of a computed tomography (CT) scan of a cerebral contusion can be found in Chapter 37, Figure 37-17, B.
Subdural hematomas occur with acceleration-deceleration injuries when bridging veins to the superior sagittal sinus are torn. Blood accumulates in the subdural space. Symptoms include weakness and lethargy. Symptoms such as weakness and lethargy that come on acutely are life-threatening. Symptoms caused by slow bleeding may not be present for several weeks. A CT scan of this problem can be found in Chapter 37, online image Figure 37-17, A. Also, note on the same figure the midline shift of the brain.
Diffuse axonal injuries, or shearing injuries, are among the most common types of primary lesions in patients with brain trauma.7,8 Brain tissues that differ in structure or weight experience unequal acceleration, deceleration, or rotation of tissues during rapid head movement or during impact, causing diffuse axonal injury and changes in chemical processing. Refer to Chapter 37, Figure 37-17, D for an illustration of what axons are most affected by this shearing motion. Severing of the axons may be severe enough to result in coma. In milder forms, more spotty lesions are seen, including deficits such as memory loss, concentration difficulties, decreased attention span, headaches, sleep disturbances, and seizures. Damage often involves the corpus callosum, basal ganglia, brain stem, and cerebellum.6,8 For a complete image of how the axons diffuse throughout the entire CNS, refer to Figure 37-17, C.
Blast injuries occur when a solid or liquid explosive material explodes, turning into a gas. The expanding gases form a high-pressure wave (overpressure wave) that travels at supersonic speed. Pressure then drops, creating a relative vacuum (blast underpressure wave) that results in a reversal of air flow, which is in turn followed by a second overpressure wave. Blast-related injury can occur through several mechanisms. The primary blast wave generates extreme pressure changes that can cause stress and shear injuries. For example, rupture of the tympanic membranes is very common after blast injury, and lung and gastrointestinal injuries also occur. The exact mechanism of injury to the brain is unknown, with speculation about both axonal shearing and shearing of vasculature.9,10
Secondary damage
 Increased intracranial pressure (ICP) (resulting from swelling or intracranial hematoma). Swelling of the brain causes distortion because the brain is held in the skull, a rigid, unyielding structure. The resultant increased ICP can lead to herniation of parts of the brain. The most often seen herniations include cingulate herniation under the falx cerebri, uncus herniation, central (or transtentorial) herniation, and herniation of the brain stem through the foramen magnum.11 Acute hydrocephalus occurs when blood accumulates in the ventricular system, expanding the size of the ventricles and causing increased pressure on brain tissue being compressed between the skull and the fluid-filled ventricles. The increased pressure can then result in changes in Pco2, which is also harmful to nervous tissue. Increased ICP has been correlated with poorer outcomes and higher mortality rates.12
Increased intracranial pressure (ICP) (resulting from swelling or intracranial hematoma). Swelling of the brain causes distortion because the brain is held in the skull, a rigid, unyielding structure. The resultant increased ICP can lead to herniation of parts of the brain. The most often seen herniations include cingulate herniation under the falx cerebri, uncus herniation, central (or transtentorial) herniation, and herniation of the brain stem through the foramen magnum.11 Acute hydrocephalus occurs when blood accumulates in the ventricular system, expanding the size of the ventricles and causing increased pressure on brain tissue being compressed between the skull and the fluid-filled ventricles. The increased pressure can then result in changes in Pco2, which is also harmful to nervous tissue. Increased ICP has been correlated with poorer outcomes and higher mortality rates.12
 Cerebral hypoxia or ischemia (occurring when blood vessels are ruptured or compressed). Hypoxia can occur from a lack of blood to the brain or from lack of oxygen in the blood as a result of airway obstruction or chest injuries.
Cerebral hypoxia or ischemia (occurring when blood vessels are ruptured or compressed). Hypoxia can occur from a lack of blood to the brain or from lack of oxygen in the blood as a result of airway obstruction or chest injuries.
 Intracranial hemorrhage causes hypoxia to tissues fed by the hemorrhaging blood vessels and adds pressure and distortion to brain tissue. Metabolic products from damaged cells and blood bathe the brain. Cell death occurs within minutes after injury from ischemia, edema, necrosis, and the toxic effects of blood on neural tissues.
Intracranial hemorrhage causes hypoxia to tissues fed by the hemorrhaging blood vessels and adds pressure and distortion to brain tissue. Metabolic products from damaged cells and blood bathe the brain. Cell death occurs within minutes after injury from ischemia, edema, necrosis, and the toxic effects of blood on neural tissues.
 Electrolyte imbalance and acid-base imbalance. Secondary cell death occurs either by swelling and then bursting of the cellular membrane (necrosis) or by destruction from within the cell through changes in the deoxyribonucleic acid (DNA) (apoptosis). Cell death can occur days, weeks, or months after injury.13
Electrolyte imbalance and acid-base imbalance. Secondary cell death occurs either by swelling and then bursting of the cellular membrane (necrosis) or by destruction from within the cell through changes in the deoxyribonucleic acid (DNA) (apoptosis). Cell death can occur days, weeks, or months after injury.13
 Infection from open wounds. Infection in brain tissue may cause swelling and cell death.
Infection from open wounds. Infection in brain tissue may cause swelling and cell death.
 Seizures from pressure or scarring. Seizures are most common immediately after injury and 6 months to 2 years after injury. The seizures can cause additional brain damage owing to high oxygen and glucose requirements.
Seizures from pressure or scarring. Seizures are most common immediately after injury and 6 months to 2 years after injury. The seizures can cause additional brain damage owing to high oxygen and glucose requirements.
Physiological, cognitive, and behavioral changes after brain injury
Autonomic nervous system
Box 24-114 lists possible autonomic nervous system symptoms resulting from brain injury.
Motor, functional, sensory, and perceptual changes
Motor abnormalities after severe head trauma are common. More severe head injuries tend to manifest more persistent physical problems.6 In at least two studies6,15 a fourth of the cases had no neurophysical sequelae. Changes in muscle tone may reflect the physiological effects of changes in the amount of tissue compression or irritation.16 Box 24-2 lists motor changes and provides symptoms of sensory and perceptive involvement.
Cognitive, personality, and behavioral changes
The social consequences of inappropriate behavior can be disastrous and a stumbling block to achieving therapy goals. A correlation between preinjury personality and postinjury changes has not been established.6 It does seem reasonable, however, that factors within an individual’s psychological makeup may affect reaction to the injury. Brain trauma frequently happens to adolescents—an age group fraught with its own problems that may be aggravated by the injury. Outcomes at 1 year postinjury have shown the most common problems to be poor memory and problem solving, problems managing stress and emotional upsets, and an inability to control temper. Finally, managing money and paying bills were still a problem at the 1-year mark.17 Box 24-318 lists both cognitive and behavioral changes resulting from brain injury.
Changes in consciousness and coma
Coma and changes in consciousness result from conditions in which there are diffusely extensive and bilateral cerebral hemispheric depression of function, direct depression or destruction of the brain stem–activating system that is responsible for consciousness or a combination of the two. In moderate or severe head injury, unconsciousness can be prolonged. Plum and Posner’s definitions16 of various stages of acutely altered consciousness are briefly presented, intermingled with some insights from the descriptions offered by Gilroy and Meyer.11 Plum and Posner19 do not equate the presence or absence of motor responses with the depth of coma. These authors point out that the neural structures regulating consciousness differ from and are more anatomically distant from those regulating motor function.
Concussion.
In mild concussion, the loss of consciousness may not occur or lasts a relatively short time (20 minutes or less) and there is little or no retrograde amnesia. A concussion can cause diffuse axonal injury and result in either temporary or permanent damage. The client may be irritable or distractible and have difficulty with reading and memory. There may be complaints of headache, fatigue, dizziness, and changes in personality and emotional disposition. This group of symptoms constitutes what is called posttraumatic syndrome. The effects of repeated concussions (second impact syndrome) are cumulative.20
Coma.
Coma is defined as a complete paralysis of cerebral function; a state of unresponsiveness. The eyes are closed, and there is no response to painful stimuli. Within 2 to 4 weeks, nearly all clients in coma begin to awaken. Oculomotor and pupillary signs are valuable in assisting with the diagnosis, localizing brain stem damage, and determining the depth of coma.19 In coma, brain stem responses may include grimacing to pain, which is frequently associated with a flexor or localizing motor response, loss of hearing or balance, abnormal palate and tongue movements, and loss or distortion of taste.
Persistent vegetative state.
Finally, no discussion of changes in consciousness would be complete without mention of those unfortunate enough to remain in a “persistent vegetative state.” This state is characterized by a wakeful, reduced responsiveness with no evident cerebral cortical function. The vegetative state can result from diffuse cerebral hypoxia or from severe, diffuse white matter impact damage. The brain stem is usually relatively intact. Clients may track with their eyes and show minimal spontaneous motor activities that even appear purposeful, but they do not speak, nor do they respond to verbal stimulation.21 Life expectancy can be weeks, months, or years.22,23 Clients with brain injury who remain vegetative for 3 months rarely achieve an independent outcome. However, the term “persistent” should not be added to “vegetative state” until the injury has stabilized or the state has lasted for approximately 1 year.24 Functional magnetic resonance imaging (fMRI) was recently used to test clients who were diagnosed as being in persistent vegetative states. Five of 54 clients diagnosed as in a persistent vegetative state demonstrated “willful, neuroanatomically specific blood-oxygenated–level–dependent responses when told to visualize one of two tasks.”25 The diagnosis of persistent vegetative state indicates lack of cortical function, and fMRI may be useful in this diagnosis in the future. Recovery of consciousness, if it occurs, includes a gradual return of orientation and recent memory.19 The duration of each of these stages is variable and can be prolonged. Improvement can stop at any point.
Other complications
A list of the complications that may accompany brain injury would be limitless. In addition to any concomitant injuries, some of the diagnostic, monitoring, and therapeutic procedures themselves carry hazards. So does prolonged bed rest. Catheters, nasogastric tubes, and tracheotomies can cause iatrogenic injuries. Infections, contractures, skin breakdown, thrombophlebitis, pulmonary problems, heterotopic ossification (HO), and surgical complications are but a few of the risks. Posttraumatic epilepsy is also a possible sequela. Depression occurs frequently after brain injury, and it can alter functional outcome. It appears that a combination of neuroanatomical, neurochemical, and psychosocial factors are responsible for the onset and maintenance of the depression.26
Amnesia.
Two types of amnesia are frequently associated with brain injury: retrograde and posttraumatic.28 Cartlidge and Shaw14 define retrograde amnesia as a “partial or total loss of the ability to recall events that have occurred during the period immediately preceding brain injury.” The duration of the retrograde amnesia may progressively decrease. Posttraumatic amnesia (PTA) is defined “as the time lapse between the accident and the point at which the functions concerned with memory are judged to have been restored.”14 The duration of PTA is considered a clinical indicator of the severity of the injury.14 An additional deficit can be the inability to form new memory, referred to as anterograde memory. The capacity for anterograde memory is frequently the last function to return after recovery from loss of consciousness.29
Memory.
The client’s inability to develop continuing short-term memory can be quite frustrating for the rehabilitation team as well as for the client because memory is an important component of learning.30 There are two types of memory: declarative and procedural. Memory in which the client can recall facts and events of a previous experience is declarative memory. Explicit learning, a conscious verbal learning, is based on declarative memory. However, many clients who cannot reproduce memories through conscious recollection do have the ability to learn new motor skills. Implicit learning, a noncognitive type of learning in which clients can show changes in performance after prior experience, is based on procedural memory. Clients can show the ability to change motor, perceptual, or cognitive behaviors with practice or training but may lack declarative memory. That procedural memory may be present without declarative memory in clients with TBI has been demonstrated.28
Initial care and medical interventions
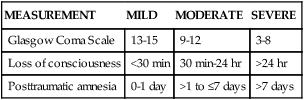
On the client’s admission to the hospital, a neurosurgeon usually assumes initial and primary responsibility for the client. The first priority in medical care is resuscitation, after which baseline assessments are made and a history is obtained. Immediate surgery may or may not be indicated. Surgery is indicated when blood and necrotic tissue are present in the cranial vault. Early concerns may include the management of respiratory dysfunction, cardiovascular monitoring, treatment of raised ICP by means of pharmacological, mechanical, or surgical procedures,14 and general medical care. Examples of general medical care are familiar: maintenance of fluid and electrolyte balance, nutrition, eye and skin care, prevention of contractures, postural drainage, and safety considerations.6 The need for this type of care gradually lessens as the client responds, or it may continue if unconsciousness persists. Initially, a determination of Glasgow Coma Scale31 (GCS) score (Box 24-4) is performed to test the function of the brain stem and the cerebrum through eye, motor, and verbal responses. It provides a measure of the level of consciousness. Scores range from 3 to 15, with lower scores associated with lower levels of function. Scores from 13 to 15 indicate a mild brain injury, 9 to 12 a moderate brain injury, and 8 or less a severe injury.
Several scales define TBI as mild, moderate, or severe based on specific measurements (Table 24-1). Because the definition of mild brain injury has varied so widely, the CDC convened a panel of experts to further define it. The new definition of mild TBI is an injury to the head (arising from blunt trauma or acceleration or deceleration forces) that results in one or more of the following: any period of confusion, disorientation, or impaired consciousness; any dysfunction of memory around the time of injury; loss of consciousness lasting less than 30 minutes; or the onset of observed signs or symptoms of neurological or neuropsychological dysfunction.2 According to the Brain Injury Association of America, with a moderate TBI the client experiences a loss of consciousness that lasts from a few minutes to a few hours; confusion that lasts from days to weeks; and physical, cognitive, or behavioral impairments that last for months or are permanent. A severe brain injury occurs when a prolonged unconscious state or coma lasts days, weeks, or months. With the possible exception of the diagnosis and hence prognosis of diffuse white matter impact damage,32 one third of clients hospitalized with brain injuries have extracranial injuries,6 which are explored with a physical examination and appropriate special tests. Additional testing depends on the client’s particular dysfunctions. CT,33 MRI, positron emission tomography (PET), radioisotope imaging, ventriculography, echoencephalography, electroencephalography, monitoring of ICP, measurement of cerebral blood flow and metabolism, monitoring of cardiorespiratory and cardiovascular function, and tests of cerebrospinal fluid and other biochemical studies all provide important information. Changes in electrocerebral potentials that occur in response to specific stimuli also are studied. Visual, auditory, and somatosensory evoked potential examinations are used with clients with brain injury but are more effective when combined with other examinations.34 These examinations make it possible to observe the presence, evolution, and resolution of a lesion.6 Reflex motor responses in unconscious clients are tested by applying a noxious stimulus, such as pressure on a nail bed with a pencil or supraorbital pressure, and observing the response. Most responses generally fall into three categories: appropriate, inappropriate, or absent.19 Testing for cognitive and behavioral functions is usually done via neuropsychological tests. In some circumstances the results of IQ tests, achievement tests, and Armed Forces tests may be available for comparison. Differentiating changes in cognitive and behavioral functions caused by brain injury from posttraumatic stress syndrome, conversion or hysterical reactions, malingering, depression, and anxiety is extremely important.
TABLE 24-1 
SEVERITY OF TRAUMATIC BRAIN INJURY
| MEASUREMENT | MILD | MODERATE | SEVERE |
| Glasgow Coma Scale | 13-15 | 9-12 | 3-8 |
| Loss of consciousness | <30 min | 30 min-24 hr | >24 hr |
| Posttraumatic amnesia | 0-1 day | >1 to ≤7 days | >7 days |
Pharmacological interventions
Medications are chosen according to symptoms to be treated. Many of these recommendations are from a meta-analysis of management of severe TBI published in 2007.35–39
Drugs that decrease intracranial pressure.
When ICP increases, changes in Pco2 are seen. The maintenance of a Pco2 at 30 to 40 mm Hg appears most appropriate. Osmotic agents such as mannitol are used to pull fluid from brain tissue back into the blood system, thus lowering ICP. Propofol, a barbiturate, is recommended for control of ICP if it cannot be controlled by other means.35 Use of mannitol is recommended for clients who have profusion problems.35 ICP has been lowered by intentional hyperventilation, which causes an increase in blood Pco2, resulting in vasoconstriction of the central vessels and reduced cerebral blood flow. However, Muizelaar and colleagues40 as well as information from the Traumatic Coma Data Bank41 showed that dramatically reducing a client’s Pco2 in this manner resulted in a worse outcome than that in clients managed with medication. Therefore hyperventilation is currently used only for nonresponsive cases and for short durations. Glucocorticoids (dexamethasone [Decadron], methylprednisolone [Solu-Medrol]) have been used to treat cerebral edema, but most studies show no long-term changes in outcome, and methylprednisolone is contraindicated because it increases mortality.39 See Chapter 36 for additional information.
Drugs that control blood pressure.
Blood pressure control is important in clients with brain injury. Cerebral perfusion pressure42 or adequate blood pressure to maintain cerebral blood flow against increased ICP is calculated by subtracting the ICP from the mean arterial pressure. If fluid management cannot keep the blood pressures elevated, then vasopressor drugs such as phenylephrine (Neo-Synephrine) are used to constrict peripheral vessels but not the vessels of the brain.
Drugs that affect the motor, behavioral, and cognitive functions (see chapter 36).
Medications also may be prescribed for motor abnormalities involving increases in tone. Baclofen is now used more frequently with clients with brain injury; however, it can produce lethargy, confusion,43 and reduction in attention span44 in some clients. These effects are greatly reduced with implantation of a pump to deliver the drug. Dantrolene sodium is another medication used to decrease spasticity and rigidity. This drug works directly at the muscle level and therefore is less likely to cause cognitive disturbances but more likely to cause generalized weakness.45 Botulinum toxin type A (Botox) is widely used to inject into specific muscles, such as the finger flexors, biceps, or gastrocnemius, to decrease their tone. Diazepam (Valium) initially was the drug most commonly administered for spasticity or high tone. However, diazepam also promotes drowsiness and decreased responsiveness and can increase muscle weakness and ataxia.43 These side effects actually hinder rather than assist in rehabilitation. Glenn and Wroblewski44 conclude that “rarely, if ever, are the benefits of diazepam’s antispasticity effect great enough to justify its use in the brain-injured population.” Drugs to treat behavioral or cognitive dysfunction have not been particularly successful. Antidepressive drugs as well as carbamazepine (Tegretol) and propranolol (Inderal) have been used to treat aggression and agitation. Carbamazepine appears to reduce agitation or aggression in clients with brain injury.46 Confusion and other neuropsychotic symptoms have been treated using neuroleptic medications. A recent review article suggests that these drugs may negatively affect motor outcomes.47 Sedative drugs prescribed in an attempt to control delirium may add to the client’s confusion and may also contribute to a decreased responsiveness. Later in the rehabilitative process, various antidepressants may be used to treat aggressive and disruptive behaviors. These, too, may have deleterious side effects. Antidepressants other than the tricyclics appear to be the most effective for treating depression.
Prognostic indicators
Numerous problems are encountered in trying to predict outcome. Included among these problems are the validity and reliability of the tests used, the uniform implementation and interpretation of predictive factors, the percentage of error in prediction, the possible effects of intervention strategies and bias in treatment on the basis of predictions, and, finally, the definition of what constitutes a “successful” outcome. Understanding these problems is imperative because the therapist can provide persuasive suggestions regarding the type and intensity of rehabilitative care after injury. The differences in operational definitions, types and sizes of populations, and length of time after injury when the outcome assessment was made contribute to the lack of consistency in studies of predictive factors for clients with brain injury. For example, several authors have found that clients younger than age 20 years usually recover better50–52; however, this has not been uniformly confirmed. A reason for caution in using tests for prediction is the percentage of error in prediction. If prediction is 80% or even 90% accurate, there are still 10% to 20% of the clients with head trauma whose outcome may be predicted incorrectly.53
Lesion size and area
There is conflicting evidence regarding recovery outcomes on the basis of lesion size and area because the type of lesion and the rapidity with which lesions occur have an impact on both the deficits and the size. There is some evidence that lesion area rather than size is important. Van der Naalt and co-workers54,55 looked at 67 patients with brain injuries in the mild to moderate injury categories and found that frontal and frontotemporal lesions were predictive of poorer outcomes than lesions in other areas. However, Kurth and colleagues56 looked at number of acute hemorrhages, lesion volume, and location in TBI using neuropsychological outcome measures and found no relationship between the numbers of hemorrhages and the volume of injury. Brain MRI in 80 adult patients (6 to 8 weeks after injury) was predictive of nonrecovery from persistent vegetative states at 12 months when the client had corpus callosum and dorsolateral brain stem lesions.57 Lesion location is not a significant predictor of GOS scores. Lesions in the brain stem do appear to cause poorer outcomes on the GOS than other lesions.58,59
Time since lesion
Better functional outcomes were found in monkeys when rehabilitation occurred earlier after the lesion. Black and colleagues60 created lesions in the motor cortices of 27 adolescent rhesus monkeys and then trained them in motor tasks involving the arm. Active postoperative training of the weak hand led to recovery of 82% of the preoperative function in 6 months if the therapy was initiated immediately. Recovery was only 67% of preoperative control if training was delayed 4 months.
Posttraumatic amnesia
PTA duration is better related to outcome than either lesion area or size.61 Postinjury amnesia had a predictable relationship to length of coma in patients with diffuse axonal injury. Duration of PTA was strongly correlated with the GOS score at 6 and 12 months after injury in patients with diffuse axonal injury but poorly correlated in patients with primarily focal brain injury. Van der Naalt and colleagues’54 study of the GCS indicates that this scale, applied 12 months after injury, is a simple and consistent predictor of outcomes in clients with a score of 9 to 11 (mild to moderate brain injury). PTA is a strong predictor of outcome as measured by the Functional Independence Measure (FIM) (an activity level measurement tool)62; and when PTA is combined with age, sitting balance, and limb strength at admission, prediction of productive outcome is high.63 Walker and colleagues64 also found that when PTA lasted less than 4 weeks, a severe activity limitation was unlikely; and if longer than 8 weeks, a good recovery was unlikely when measured by GOS.
Sitting and standing balance
Age younger than 50 years had a significant association with normal sitting and standing balance. Measures of severity of TBI, including admission Glasgow Coma GCS score, length of PTA, length of coma, and acute care length of stay, were also each significantly related to impaired sitting and standing balance. Initial abnormalities in pupillary response, respiratory failure, pneumonia, soft tissue infections, and urinary tract infections had a significant relationship with impairment of sitting but not standing balance. Presence of intracranial hemorrhages did not have a significant relationship with either sitting or standing balance. Intracranial compression had a significant relationship with standing balance. Discriminant functional analysis showed no relationship between balance ratings and neurological or radiological findings, injury severity, or medical complications.65
Other factors
Finally, several studies have reported that absence of previous TBI,42 a higher level of educational achievement, and stable work history also are positive preinjury variables for a better prognosis.66 The Wechsler Adult Intelligence Scale (WAIS)—Revised IQ test may correlate with prognosis according to other studies.66
Motor disturbances resulting from brain injury generally have a good prognosis.14 Of the physical deficits encountered, dysfunctions in the cerebral hemispheres and of the cranial nerves are the most common disorders, and these may partially resolve. Losses of these functions can be more permanent,11,14 especially without skilled rehabilitation interventions. Complete recovery is rare except with hearing, vestibular function, and smell. In one Glasgow study, some degree of hemiparesis was present 6 months after injury in 49% of the 150 clients who regained consciousness after severe brain injury.6
Psychosocial outcomes vary after severe brain injury.67 Psychosocial variables that significantly increased life satisfaction for persons with TBI were total family satisfaction, being employed, being married, having memory, bowel independence, and not blaming oneself for the injury. Those who do not blame themselves show a greater number of functional activities as indicators for their self-satisfaction.68
See Box 24-6 for factors that can influence recovery and management.
Conceptual framework for therapeutic intervention
Motor control theory
Motor control and learning theories try to explain how the central nervous system (CNS) accomplishes the miracle of coordinated, meaningful movement. Motor control theory and factors affecting effectiveness and speed of motor learning are reviewed in this section and are discussed in detail in Chapter 4. This chapter’s examination, evaluation, and intervention technique sections are based on that framework. A quick review of basic principles follows.
Synergistic organization
Synergies, or motor patterns, were viewed by Bernstein69 as the basis of movement. The need for the brain to use synergistic organization comes from the infinite number of movement combinations that are available. By use of motor patterns, which decrease the number of degrees of freedom, speed and efficiency are added while flexibility of response is maintained. Force (amplitude) of contraction, velocity, and timing can still be changed to meet task demands. Research suggests that motor patterns are shaped through experience and that they develop before birth (innate) and after birth (learned). Early experiments on motor learning demonstrate how motor patterns may develop. Payton and Kelley70 showed that with practice of a novel motor task, movements become more organized and skilled.
Characteristics of A learned skill (motor pattern).
In learning a new skill, movement begins with a “gross approximation” of the movement that includes agonist-antagonist co-contraction. As movement is refined, reciprocal movement replaces co-contraction.71 In electrophysiological studies of skill acquisition, less electrical activity is seen on electromyography (EMG) and less time to peak activation of the muscle is noted in motor tasks after they become skillful. In addition, fewer muscles are recruited for the same movement.72 PET scans have confirmed these EMG findings, demonstrating decreasing areas of brain activity after skill acquisition. Neuronal changes brought about through long-term potentiation and long-term depression are a basis for learning new tasks and developing motor patterns and behavioral changes.73 As neurons are repetitively fired at the same time, networks develop. These neuronetworks, or cell assemblies, are formed with increasing complexity and self-organization. The more they are used, the stronger and more permanent are the changes that occur. Finally, a specific stimulus now provokes a learned or skilled response as an organized synergy. The output of the networks is not a summation of individual functions but has “emergent properties” that are more than the sum of the output of individual neurons.
The best understood motor patterns are the balance and reaching patterns. Both appear to be basic innate synergies. Quiet standing in humans is maintained by somatosensory, visual, and vestibular inputs (see Chapter 22). It requires the coordination of many muscles, especially those of the hips, knees, and ankles, to maintain the body’s center of gravity over its base of support. This complex coordination of muscle control is accomplished by sequences of stereotyped patterns mediated through the brain stem, cerebellum, and spinal cord. Somatosensory input during body sway stimulates the response in which posture is stabilized by small changes in the angle between the foot and the leg. For small and slower center of gravity movements, these synergies are sequenced in a distal to proximal manner. The direction of sway determines the particular synergy elicited to correct for the shift in the center of gravity. In forward losses of balance, the posterior extensor muscles of the legs and trunk respond at about 100 ms. In backward losses the anterior muscles respond, including the anterior tibialis, hip flexors, and abdominals. The timing between muscle contractions and the proximal-to-distal sequence are preset. The amplitude of contraction varies with the environmental demands and the amount and velocity of sway. In larger or more rapid sway, a different synergy is used; the person may bend at the hips and knees, or a hip strategy or a combination of hip and ankle strategies is used. If the balance loss is great enough, the person takes a step to maintain upright balance.74 (For additional information, see Chapter 22A on balance and 22B on vestibular dysfunction). In gait, weight shifts from one leg to the other and stability after the weight shift are other aspects of dynamic balance performed through motor patterns. The movement pattern of the swing leg in gait is limited in the number of degrees of freedom at each joint and the sequence of movement by motor patterns. There is also a specific coordination and timing of swing leg movement in relation to the stance leg movement (interlimb timing and coordination) accomplished through motor patterns. In gait, the sequence of contraction of the leg muscle from ankle to hip, the time of onset of the contraction of each muscle, and a ratio of force for each muscle is preset in the motor control program of the brain or spinal cord. If an increase in speed is needed, step length, cadence, and force can be increased within the synergy, but the basic synergies, or motor patterns, are what give identity to a gait pattern. Whether the person is walking quickly or slowly, there is an individually recognizable pattern.
In the reaching and grasping pattern, three components have been identified: the reaching portion (transport), the grasping or prehension portion, and the maintenance of balance. Reaching and maintenance of balance are accomplished through motor patterns.75,76 The target determines the reaching pattern. Characteristics of the reaching synergy include a distal-to-proximal sequence of firing, and movement is in a straight line with a bell-shaped velocity curve.77 The prehension portion of reach and grasp is not a synergistic movement, and the motor-sensory cortex helps with force production and selection of muscles78 during hand movement to meet task demands. This may be why more severe deficits are seen in the hand after cortical injury.
Anticipatory and adaptive responses
To meet the motor task (external) requirements, motor patterns are used and modified through a feed-forward and feedback system of control. The brain adapts motor patterns to environmental constraints, such as obstacles, by modifying the basic motor patterns’ velocity, intensity, or duration of contractions before the movement even begins. Feed-forward or anticipatory responses (often from vision and past memory of successful movements) are provided by muscles that will stabilize before the prime mover of a motion begins to fire and thus are the first muscle contraction that occurs during a movement that might disrupt stability. For example, before a rapid forward reach, the gastrocnemius muscles fire to reduce the amount of forward sway that would occur secondary to the forward movement of the center of gravity.79
Adaptive responses use sensory feedback (visual or proprioceptive feedback is most commonly used) to improve the effectiveness of a response. After a movement, the brain checks to determine that the motor pattern matched the original “planned” pattern. Adaptive responses provide for modifications of movements, especially when the environment is changing. An example would be the ability to change the balance response when stepping from a firm surface onto a surface that is unexpectedly soft. A person will lose balance the first time but should be able to perform with good balance after several attempts. Sensory information helps fine-tune or adapt the subsequent movements within a synergistic movement. For gait, sensory impulses drive motor system adaptations to the environment. In the reaching-prehension pattern, tactile input from the fingertips (feedback) is used to make adjustments in grip force if the initial grip was not effective.80 Once movement occurs, there is a final comparison of the original planned pattern with the executed pattern to see whether they match; if not, then more adaptations are made.
Dynamic pattern theory and new patterns
Once called motor control theory, the dynamic pattern theory81,82 addresses problems when motor behavior changes and also uses concepts of basic patterns of movement. This theory states that certain patterns are stable or unstable and that transition between patterns or to a new pattern depends on pattern stability. (See Giuliani83 for a summary of this theory.) The challenge for therapists is to identify what makes these “stuck” behaviors become unstable and perhaps amenable to change. Patterns that are “set” are much more difficult to change than those that are more variable. In fact, phase transitions between old and new patterns are noted by periods of increased variability. The client appears to vacillate between the old and the new behaviors during transition phases and before new behavior establishment points. Transition phases are often frustrating for clients, as they feel unstable and may think that therapy is making them worse. Repetition is important to develop more consistent motor patterns and new establishment points; however, more important is preparing the client to expect this change.
Motor learning
Byl84 noted that motor cortex (M1) changes occurred (motor learning) when (1) new or novel tasks were used, (2) movements were practiced together (spatial organization and temporal organization), (3) movements were frequently repeated, and (4) movements were important to the individual.
Interventions are designed to produce a task-oriented behavioral change that becomes permanent without continued therapist help or intervention. When this does not happen, the client performs well during therapy but does not seem to carry the improved performance outside the clinic. This difference between performance and learning is discussed by Schmidt.85,86 Many things affect motor learning, among which are knowledge of results (KR) and type of practice. (See Chapter 4.)
Knowledge of results
Information on how successful the movement was in meeting the task goal is basic to learning. Knowledge of results (KR) consists of extrinsic information over and above that provided by the task itself.87 During the practice portion of most tasks, increasing any type of feedback appears to improve task performance.88 But long-term learning may be improved when KR is provided less often. The relative frequency with which KR is provided in relation to the number of trials is important in learning. Bandwidth KR, in which information is given about trials falling outside a certain range, and a random schedule of feedback appear to be effective for many learning situations in therapy. Delaying KR also improves learning.87
Practice type
The type of practice is important for clients who are learning new skills. A commonly used technique to simplify a task by practicing at a slower speed or practicing a part of a motor task is often not effective. For example, weight shifting is often practiced as a component of gait before walking is initiated. Winstein and colleagues89 demonstrated that this part practice did not transfer to gait in a group of clients who had had a stroke. In a study by Man and colleagues,90 a complex task was broken down into adaptive training methods (e.g., slower motions) and part-task training (on components of the task). Subjects who practiced the whole task had better performance than either of the other groups. A finding that practicing small components of a task does not make one better at the whole task is not too surprising. Many of us can jump, have good shoulder power, and can throw overhead but cannot, without practice, put this together to play basketball. A minimum basic amount of strength, range of motion (ROM), and interlimb sequencing is necessary to play basketball but is not adequate to play without the actual practice of the sport.
However, practicing other than the whole task may be possible. By use of the same task as that used by Man and colleagues,90 Newell and colleagues91 showed that part-task training was effective when it was conducted in natural subtasks of the whole. These subtasks are part of the whole task but are distinguished by changes in speed or direction. This area of skill acquisition has not been studied adequately to identify subtasks of most common movements. A recent meta-analysis reviews use of part practice and methods of part practice for the most effective motor learning.92 Whole practice appears best for tasks low in complexity and high in organization as well as for discrete or serial tasks with high organization. An example might be a golf swing. Part practice appears effective for tasks high in complexity and low in organization, for example, dancing.
Examination, evaluation, prognosis, diagnosis, and intervention
Terminology and structure for client management
The World Health Organization (WHO), in the International Classification of Functioning, Disability and Health (ICF),93 has developed a common terminology that is used in this chapter. Definitions are as follows (also see Chapter 1 and Figure 30-2):
 Body functions are physiological functions of body systems (including psychological functions).
Body functions are physiological functions of body systems (including psychological functions).
 Body structures are anatomical parts of the body such as organs, limbs, and their components.
Body structures are anatomical parts of the body such as organs, limbs, and their components.
 Impairments are problems in body function or structure such as a significant deviation or loss.
Impairments are problems in body function or structure such as a significant deviation or loss.
 Activity is the execution of a task or action by an individual.
Activity is the execution of a task or action by an individual.
 Participation is involvement in a life situation.
Participation is involvement in a life situation.
 Activity limitations are difficulties an individual may have in executing activities.
Activity limitations are difficulties an individual may have in executing activities.
 Participation restrictions are problems an individual may experience in involvement in life situations.
Participation restrictions are problems an individual may experience in involvement in life situations.
 Environmental factors make up the physical, social, and attitudinal environment in which people live and conduct their lives.
Environmental factors make up the physical, social, and attitudinal environment in which people live and conduct their lives.
The American Physical Therapy Association has published levels of client management leading to optimal outcomes.94 The Association’s Guide to Physical Therapist Practice, which uses examination, evaluation, diagnosis, prognosis, intervention, and outcomes as its basis, will be followed in this chapter. Although this is the terminology used by physical therapists, its application and integration into the profession of occupational therapy should be simultaneously acknowledged. The method used in this chapter for gathering the guide information is based on the Hypothesis-Oriented Algorithm for Clinicians (HOAC II) model.95 See Box 24-7 for an overview of this method, and see the text that follows for details of how to perform these items.
Examination
Once activity limitations have been determined, a task analysis can be completed by having the client demonstrate the problem—in this case, walking. The therapist will develop a hypothesis as to why the observed deviation from typical performance is present. Tests and measures will be chosen on the basis of the therapist’s knowledge of their importance in the task being performed to confirm the hypothesis. For example, in a client who drags his foot in initial swing, the client might lack 45 degrees of full passive knee flexion, but this is not critical in the task of walking. However, being able to dorsiflex the foot at initial swing is important. Therefore testing of both the ability to dorsiflex with the leg in the extended position and the speed at which the client can perform this task would be appropriate. The tests and measures should be chosen on the basis of the hypothesis that the therapist generates from the task analysis. For the components of examination, see Box 24-8.
Outcomes must be tested and usually are chosen to measure all levels of dysfunction from impairment through participation limitation to determine effectiveness of the intervention strategies and whether or not the client has met the goals. An example of the process is presented in Box 24-9.
Examination of the client with brain injury
Cognitive, behavioral, and communication deficits.
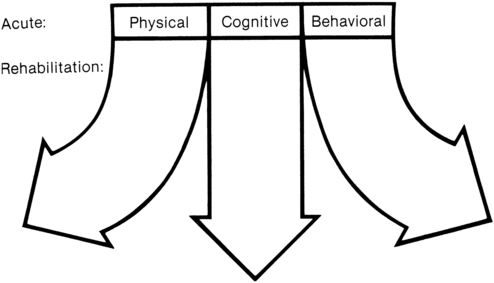
Figure 24-1 depicts the close association of cognitive, behavioral, and physical functioning soon after injury. The three domains gradually become more distinguishable in later stages of recovery and can be assessed more independently; however, their interrelationships remain exceedingly complex. Cognition includes many aspects of function, including memory, learning, information processing, attention span, motivation, and initiation. Cognitive impairment was the primary contributor to activity limitation in most clients with TBI who scored at moderate to severe levels on the GOS.96 Neuropsychologists, speech pathologists, and occupational therapists all perform testing of cognitive function. These tests may include word association, written word fluency, figural fluency, and card-sorting tests. Attention can be tested with the digit span and arithmetic tests on the WAIS97 and by serial counting by 7. Information processing is reflected in reaction time tests and digit symbol tests. Choice reaction time is an indicator of information processing and commonly remains below normal in clients with brain injury.98 Testing of intellectual functions is often done with the WAIS. However, formal testing of intellectual function can be hampered by inadequate perceptual, visual, and motor performance. Memory can also be tested with the WAIS and with the Galveston Orientation and Amnesia Test.99 The Mini-Mental State Exam100 is a memory screen often used by health care providers to determine whether further testing is indicated. Language and cognitive problems are frequently examined by speech pathologists and/or neuropsychologists using naming tests, aphasia examinations, and tests of auditory comprehension and speed of comprehension. A widely used system of cognitive function at the activities level is based on numerous observations of clients with brain injuries at Rancho Los Amigos Hospital. This has resulted in a descriptive categorization of various stages of “cognitive function,” as shown in Appendix 24-A, with use of the Rancho Los Amigos Levels of Cognitive Functioning Scale.
Examination of motor functions
Task analyses and common activity level impairments after moderate to severe injury.
Often the physical therapist begins the examination at the activity limitation level. This usually involves observing those functions that the client or family identifies as problems. Activity limitations in clients with TBI range over the entire spectrum of problems depending on the severity of injury. They may include loss of mobility in bed, coming to sit, sitting to standing; loss of household and community ambulation; loss of running, jumping, and kicking skills; poor reach and grasp; loss of throwing and batting skills; loss of activities of daily living (ADLs) such as dressing, toileting, and feeding; and loss of instrumental ADLs such as shopping and driving. The physical or occupational therapist performs a task analysis of the impaired function by comparing the client’s performance of the task with typical task performance. For example, the therapist would observe the client performing the sitting-to-standing activity, observing that there is inadequate forward trunk momentum in the preextension phase.101 A reasonable hypothesis may be that the client is fearful of falling forward. If the problem is loss of balance in the extension phase, a hypothesis may be poor timing of the gastrocnemius firing. Both these hypotheses are based on the task analysis but also on the literature, which defines the importance of trunk momentum to initiate seat-off and timing of gastrocnemius firing during the end of the sitting-to-standing activity to maintain balance.
Impairments
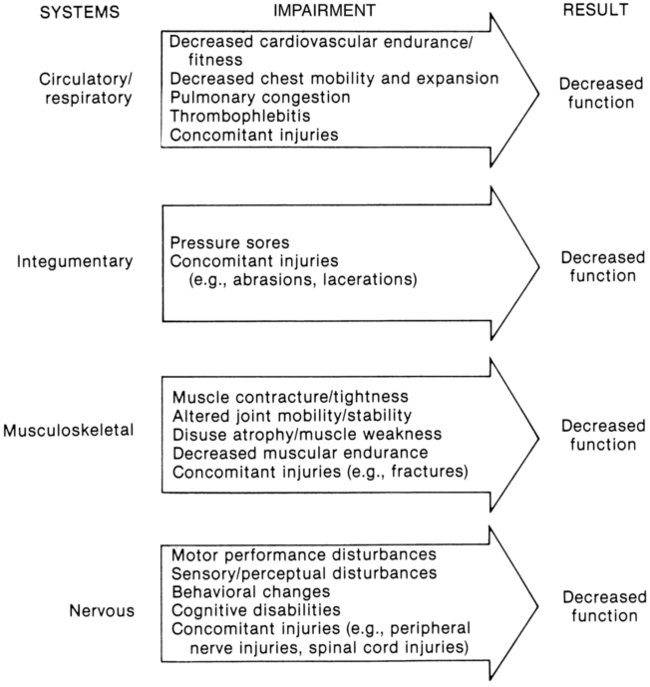
Impairments can be identified and evaluated for their contribution to an activity or participation limitation. Some critical impairments will have more influences on an activity than will others. For example, in children with cerebral palsy who have gait disabilities, Olney and colleagues102 demonstrated that poor force output by ankle plantarflexors during the late stance phases of gait was the most important factor in poor gait performance within this population. Another example comes from Perry and colleagues,103 who showed that for normal walking velocity to be attained, although cadence and stride length are important, a strength level of 3+/5 is a critical component in the ankle muscles. Deficiencies of timing, strength, or sequencing can contribute to poor hand function, but sensory deficits at the hand level may be the critical impairment related to poor manipulation skills. In addition, impairments in the circulatory, respiratory, integumentary, and musculoskeletal systems can account for activity limitation in the client with TBI (Figure 24-2). Relative contributions of the impairments to the activity limitation or participation limitation are addressed by the therapist’s task analyses, hypothesis, subsequent evaluation, and diagnosis,104 which will determine the focus of the intervention program. Second, treating the individual impairments will not necessarily result in the client learning a skill. Skills result from an organization of many motor functions together and require whole task practice. Conversely, not having a critical component, such as arm strength, may be the one factor preventing a person from learning to perform a skill (e.g., enough force cannot be generated to throw a ball 5 feet in the air to hit a basket).
Many examinations address the impairment level. These include muscle strength tests, flexibility (ROM) tests, speed of motion, reaction time, sensation, vision, vestibular, tone, and proprioceptive examinations (see Chapter 7).
Impairments that are common after traumatic brain injury and measuring impairments
Strength or force production
Evidence consistently shows that strength and force production are problems in both the upper extremities and lower extremities after TBI. In cases in which strength control or force gradations are significantly impaired at initial admission (about 25% of clients), these problems had generally resolved at a 2-year follow-up, with only 12% of problems remaining in the upper extremities and 7% in the lower extremities.105
In the case of upper motor neuron lesions, weakness can be a major problem. The number of motor neurons activated and the type of motor neurons and muscle fibers recruited affect force. Motor neurons in the motor cortex can be deficient, leading to disordered and reduced recruitment. Individuals with brain damage show early atrophy and loss of motor units, as well as motor units that fatigue easily.106,107 Disuse, cast immobilization, joint dysfunction, improper nutrition, drugs, and aging can cause differential weakness with altered morphological, biochemical, and physiological characteristics within the muscle.108 EMG studies by numerous investigators109,110 suggest that reduced activity alters motor unit properties, discharge frequency, and recruitment patterns. Performance problems are reflected in the inability to generate force in different directions and against different loads as well as in problems sustaining force output.11
Changes in muscle length affect strength. In clients who have had a cerebrovascular accident (CVA), shortened muscles tend to be strong in short ranges and lengthened muscles are strongest in lengthened ranges but weak in shorter positions compared with the strength-length curves of normal muscles.111
Strength or force may be examined functionally—for example, by seeing if the client has enough strength to lift the arm overhead, out to the side, and up to the mouth or is able to go from sitting to standing. In some cases, such as those in which the client is unable to perform balance reactions or has been on extended bed rest, testing individual muscles may be important. Traditional manual muscle testing (MMT) with force transducers or strength testing with isokinetic testing112 throughout the range provides good strength information. The level of testing chosen should be consistent with the deficit and the therapist’s knowledge of its importance in contributing to the activity limitation.
Tone
Whatever the cause of increased tone, the therapist can evaluate tone at two levels: is it interfering with function, and, if so, can it be changed? Spasticity is not a single problem.107–110,113,115–119 Spasticity can have any or all of the following characteristics:
 Changes in response to stretch
Changes in response to stretch
 Decreased ability to produce appropriate force for a specific task
Decreased ability to produce appropriate force for a specific task
 Increased latency of activation
Increased latency of activation
 Inability to rapidly turn off muscles
Inability to rapidly turn off muscles
 Loss of reciprocal inhibition between spastic muscles and their antagonists
Loss of reciprocal inhibition between spastic muscles and their antagonists
 Changes in the intrinsic properties of the muscle fibers
Changes in the intrinsic properties of the muscle fibers
 Inability to generate enough antagonist power to overcome spastic muscles
Inability to generate enough antagonist power to overcome spastic muscles
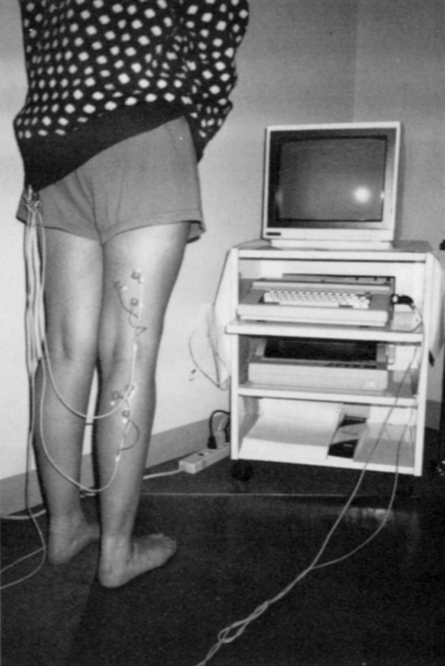
Spatial sequencing of movement involves the contraction of a preset group of muscles. Temporal sequencing involves muscles contracting in a fixed sequence. EMG and video analysis provide additional depth of information regarding the sequence and timing of movement patterns (Figure 24-3). For example, is the normal temporal sequencing in the distal-to-proximal manner present in the upper extremity during a reaching task? In a balance reaction, are the ankle, hip, and back extensors (spatial sequencing) all contracting in response to a forward perturbation? The most commonly used tool in examination of tone is the Ashworth Scale or Modified Ashworth Scale120 (Box 24-10). The Tardieu Scale121 is similar, but testing is done at three different velocities and may provide a clearer picture of what is caused by tone versus muscle shortening. Testing of deep tendon reflexes identifies problems with stretch reflexes, and surface EMG (sEMG) can determine the presence of co-contraction, prolonged contraction, sequence and timing problems, and increased latencies.
Reaction time
Simple reaction time examination gives insight into the time for neurological processing because it is the measurement of time from a stimulus to a response. Rapid reaction times may be critical for many patterns to be effective, but especially for automatic patterns such as balance responses. Simple reaction times appear impaired even long after TBI (moderate to severe),123 although there is conflicting literature in this area.
Endurance and fatigue
Fatigue, which is separate from impaired endurance, may result from increased energy requirements resulting from less efficient motor patterns or from more CNS activity. Fatigue is a common complaint after TBI124 and is associated with insomnia.125 Testing for fatigue is difficult. There are a few paper and pencil tests, including the Chalder fatigue scale.126
Muscle endurance refers to the ability of a muscle to produce the same level of contraction over time. The subjective feeling of effort and weakness after fatiguing exercise may be related to the need to recruit more motor units and to increase the mean firing frequency of the motor units to maintain constant force output.127 EMG with medium-frequency analysis can test this type of fatigue. Fatigue can also be assessed by measurement of maximal voluntary force, maximal voluntary shortening velocity, or power.127 Decreased force production, prolonged time to relaxation of muscle fibers, and recruitment of additional muscles during an activity are characteristic of fatigue.128 Although repeated muscle testing can pick up decreased strength in specific muscles, in most instances overwork fatigue is first noted by an altered pattern of movement of body segments during activity.
Cardiovascular endurance determines how effectively the body can use oxygen and how soon fatigue sets in. This type of endurance can be measured with several bicycle tests129,130 and with a treadmill using the Bruce131 protocol or a branching protocol for clients with less endurance. A simple test is heart rate before and after activity; the less change and the more rapid the return to resting rate, the better the client’s fitness level. The 3- and 6-minute walk tests are also reliable and valid for endurance testing.132
Incoordination
Ataxia was one of the most common findings among military personnel who had sustained TBI,105 with 32% of clients showing ataxia initially and 14% at the 2-year follow-up. There are many subcategories of ataxia, including dysmetria, rebound, diadochokinesia, and intention tremor. Many clinical tests are available. Common tests include having the client touch an index finger to the examiner’s finger and back to the client’s nose. Running the heel up and down the opposite shin is a test for ataxia in the lower extremity. For a list of coordination tests see Chapter 21.
Sensory function
Proprioception, light touch, two-point discrimination, and stereognosis.
After TBI, sensory deficits are common. Deficits associated with poor balance included a high number of subjects with discriminative touch deficits (20 of 27 subjects),133 an impairment related to poor upper-extremity function.
Light touch is tested with a brush for localization and quality of sensation. For more definitive light-touch discrimination, especially on the hands and feet to determine peripheral neuropathies, a monofilament test134 can be used. Two-point discrimination can be tested with instruments specifically designed to measure how far apart two separate spots of contact need to be to identify them as distinct. For clients who are thought to be ignoring stimuli on one side, testing at the same time bilaterally is first performed, and then each limb is retested separately. Clients who extinguish stimuli will respond that they feel only one stimulus when both limbs are tested simultaneously but will perceive the stimulus just fine when each limb is tested separately. This is called the bilateral extinction test.
Vision and visual perception.
Vision is critical in recovery of many motor functions because it is responsible for much of the feed-forward or anticipatory control of movement as well as the initial development of a movement pattern. For example, balance can be maintained through the visual system by modifying synergies before surface change occurs. Feedback through the peripheral field through the movement of the visual array on the retina can also trigger balance responses. Campbell133 found problems with visual functions in most clients with mild to moderate TBI; these problems involved poor visual acuity (48%) and problems with vergence (85%), which can cause blurring and doubling of vision, and smooth pursuit (63%), which can cause a “jumping” of the visual image.
General visual functions can be screened by the physical or occupational therapist as follows:
1. Tracking is assessed by use of an H pattern of movement of the object being tracked. The examiner observes any nystagmus or refixation saccades. Eye muscle paralysis can be observed during tracking if the client cannot move the eye(s) laterally, up, down, or medially.
2. Focus or accommodation can be checked by observing constriction and dilation of the pupil. Constriction occurs as an object is moved toward the nose, and dilation as the object is moved away from the nose.
3. Binocular vision is controlled through feedback from blurred or doubled vision. This reflex signals whether the eyes and fovea are focused on a single point or target, as the images in both eyes fall on the same retinal points. A “cover test” can screen for binocular vision. The client stares at an object at about 18 inches from the nose. The therapist covers one eye. If there is movement to adjust the remaining uncovered eye back to the object, both retinas may not be focusing on the same point. Observing whether light reflections fall on exactly the same place on both pupils is useful in evaluating binocular eye focus. Vergence testing can also be an indicator of binocular visual functions.
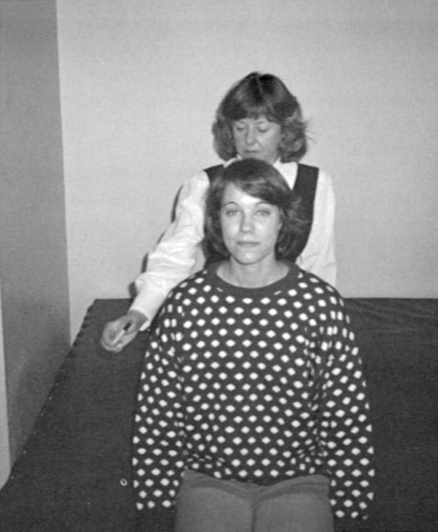
4. Visual fields can be grossly tested by having the client look forward at a point (observer sits in front of the client to be sure the client remains focused straight ahead [Figure 24-4]). The client indicates when he or she first sees an object coming into the peripheral field from behind, or the “spotter” notes when the client looks toward the object.
5. Vergence is tested by having the client observe an object or pen tip as it is brought from about 20 inches away. The client is told to follow the object with his or her eyes. The object is moved at a moderate speed toward the bridge of the nose, and the client reports when the object becomes blurred or doubles. When typical convergence is present, there will be no blurring or doubling until the object is 2 inches away or closer, and when the object is moved back out, the client will report the object as single within 4 inches.
6. Visual interactions with the vestibular system are assessed through the vestibuloocular reflex (VOR). This reflex maintains a fixed gaze on a target as the head moves. The object should not appear to blur, move, or double during head motion at various speeds.
7. Perceptual tests that evaluate how visual information is used include visual memory tests, cancellation tests, and figure-ground tests.
8. Visual acuity is tested using a Snellen eye chart. Poor acuity can affect balance responses.
Neuro-optometrists and neuro-ophthalmologists are appropriate referrals for clients needing in-depth visual workups, especially when visual perception is involved. See Chapter 28 for additional information on vision and visual testing.
Vestibular system.
Clients with mild or moderate TBI have a high rate of complaints of dizziness.135 In many cases the dizziness is a sign of vestibular dysfunction.105 Campbell and Parry133 found that 26 of 27 clients with TBI and poor balance also had abnormal VOR testing results. Impairments that can occur with vestibular injury after TBI include verticality and orientation dysfunctions.79,116,117,133,136
The VOR is indicative of vestibular system dysfunction. Vestibular tests can be performed at the screening level to note dizziness with body, head, or eye motions. A practical division includes testing head movement in lying, sitting, and standing positions. Vestibular system evaluation and training137 is one such outcome test. Symptoms occurring only with specific head movements can be an indicator of problems in the semicircular canals. Benign paroxysmal positional vertigo (BPPV) is common after brain injury. Dizziness with head tilts might indicate problems in the otolithic system. In-depth evaluation tools may be used when clients are symptomatic, and clients can be referred for electronystagmography, the gold standard for diagnosing unilateral peripheral vestibular dysfunction. See Chapter 22 for additional information on balance and vestibular testing.
Activity level dysfunction and testing
Although there are no data on frequency of problems with rolling and rolling to sit in the literature, a recent study of multiple centers that treat clients with acute TBI showed that sitting balance,138 sitting to standing,139 and losses of standing balance, gait, running, and reaching and grasping have high incidences of impairments at admission.
Standing balance
Standing balance after TBI is usually affected in mild, moderate, and severe injuries, with 82% of clients showing standing balance problems. Problems include both motor strategy problems and appropriate use and integration of somatosensory, visual, and vestibular information. Newton140 reported that clients with moderate and severe TBI showed significantly impaired reaction times to perturbation in standing. Although they could grade their responses to the perturbations appropriately, the responses were often asymmetrical.
Balance is tested with feet shoulder width apart, feet together (Romberg), and feet in tandem (sharpened Romberg) with eyes open and eyes closed. A Clinical Test of Sensory Interaction on Balance (CTSIB) test141 is used to test sensory balance components. Perturbations to balance can be used to examine motor components of ankle, hip, and stepping strategies. See Chapter 22.
Gait
People with TBI walk with a significantly slower speed than matched healthy controls. There is a significant difference between groups for cadence, step length, stance time on the affected leg, double support phase, and width of base of support. The most frequently observed biomechanical abnormality is excessive knee flexion at initial foot contact. Other significant gait abnormalities are increased trunk anterior and posterior amplitude of movement, increased anterior pelvic tilt, increased peak pelvic obliquity, reduced peak knee flexion at toe-off, and increased lateral center of mass displacement. Walker105 found that testing of clients using the tandem gait identified the most frequent physical impairment remaining at a 2-year follow-up in a group of people with TBI. He suggests using tandem gait as one part of the clinical examination for all clients with TBI.
The Barthel Index,142 FIM,143 Tinetti assessment,144 Gait Assessment Rating Scale,145 and Motor Assessment Scale146 also examine different components of gait but more at the activity limitation level. Speed of walking for functional activities such as crossing a street at a stoplight and endurance can be measured by distance and a stopwatch.147 Endurance can be measured with a 6-minute walk test.132
Complex task level problems
Are basic motor patterns available, accessible, and used appropriately?
Are the three basic components of movement all present? They are as follows148:
1. Reflex responses that are involuntary, such as the withdrawal reflex.
2. Rhythmic motor patterns, such as walking, that initiate and terminate a sequence of voluntary movements; the movements are relatively stereotypical and almost automatic.
3. Voluntary (volitional) movements that are purposeful, goal directed, complex, and learned. Playing the piano would be an example of this type of movement.
Variability of performance
The plastic nervous system can adapt and change its motor output to meet different requirements. VanSant149 showed that children and adults vary in the way they stand from supine, even under the same environmental conditions. She states that the most striking observation in nondisabled individuals is this variability of performance. The lack of variability has been suggested as a sign of system damage.86 When the client with brain injury is assessed, the therapist should look for variability of performance in basic motor acts. Can the client accomplish the same task in several ways? Can the client adapt to different task demands? As the complex task is being performed, keep in mind that the extent of deficit is important. To what extent is the observed motor behavior involved? Is the behavior totally absent, is it deficient, or are there signs of substitution of function or adaptation?
Following is an example of the examination process. The client complains of difficulty in walking and is experiencing several falls daily. Walking requires several complex elements including extensor strength, postural control, and balance.150 First, a task analysis is performed, and in this case the therapist would look at the gait pattern, perhaps using the Rancho Los Amigos Observational Gait Analysis to analyze the kinematic aspects of the pattern. The therapist then hypothesizes about specific problems observed during the task (gait) analysis. For example, if the client is dragging his toe in swing and does not have adequate knee flexion in this phase, the therapist might hypothesize that the thigh is advancing too slowly (speed of motion impairment) to promote good knee flexion and that dorsiflexion is limited because of poor anterior tibialis activation (force production problem). Timing the speed of hip flexion and doing MMT might confirm or rule out these hypotheses.
Prognosis for improvement by activity limitation
In a review63 of long-term problems after moderate or severe TBI, standing balance was most impaired initially (82%) and at 1-year follow-up (24%) compared with other systems. Sitting balance was impaired 52% of the time initially but only 5% at the 1-year follow-up. Strength was more often impaired (about 42% of clients) than coordination (40%) or tone (20%) but showed significant improvement, with less than 20% of clients being impaired in strength and less than 10% in coordination or tone at the 1-year follow-up. Dysphagia was present in 40% of the clients but in only 0.4% at 1 year.