CHAPTER 336 Traumatic and Penetrating Head Injuries
In recent years there has been an apparent paradigm shift of scientific interest in the long-term effects of mild traumatic brain injury (MTBI) and its contribution to posttraumatic stress disorder (PTSD).1–6 It is estimated that more than 320,000 American soldiers may have sustained TBI in Operation Iraqi Freedom (OIF),4 the majority of which were mild, contributed to PTSD and physical ailments, and thus had the potential to disrupt postwar American lives.1,3,5,7–9 We have also witnessed major initiatives by the U.S. government to support the neuroscience community in its attempts to better understand the pathogenetic mechanisms, manifestations, and more effective management of TBI and PTSD caused not only by PBI but also by blast overpressure generated by complex explosive devices.4,10–14 Newly designed protective body armor has reduced the incidence of PBI significantly.4,15 However, the nature of the asymmetric warfare during OIF has exposed military personnel to sophisticated explosive devices generating blast overpressure that results in secondary cellular and molecular insults to the brain parenchyma akin to diffuse brain injury.4,11–13,16,17 Significant progress has been made in achieving a more detailed understanding of the manifestations of vascular insults and diffuse brain edema, some of which can be managed effectively by endovascular interventions and decompressive craniectomy.11,17–20
The biomechanics of civilian gunshot wounds to the head (GSWHs)21–36 tends to be different from that of military craniocerebral battle wounds and blast overpressure.4,5,10–13,16,17,21 Translation of kinetic forces into injury to the brain parenchyma in civilian GSWHs is direct and devastating with no hope of rescue in the majority of victims.21,22,37 When compared with military conflicts,38 civilian GSWHs have unacceptably high mortality.39 Only 18% of GSWH victims in Hernesniemi’s service were cared for by a neurosurgeon,25 and only 28 of 143 subjects in Kaufman and colleagues’ study underwent craniotomy.40 More than 90% of civilians sustaining GSWHs die—almost two thirds of them at the scene.39 In 2000, 250 people sustained GSWHs in the state of Maryland (unpublished data), 222 (89%) of whom eventually died (177 at the scene and 45 in the emergency departments of eight trauma centers). Only 10 patients were seen at the trauma resuscitation unit of the Shock Trauma Center alive; 8 of the 10 underwent surgery, and 6 (2.4%) eventually made a favorable recovery. This grim prospect has also been the general impression of other investigators.21,41–43
Ballistics, Wounding Energy, and Pathogenesis
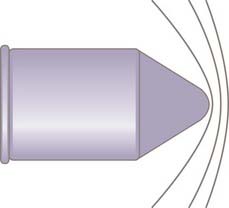
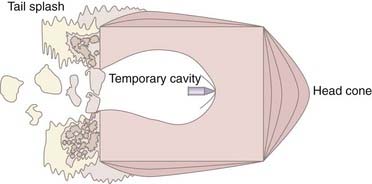
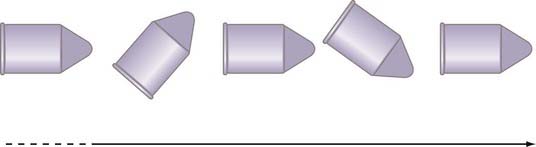
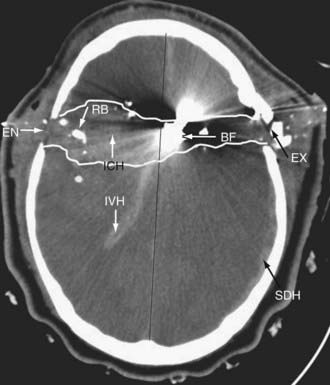
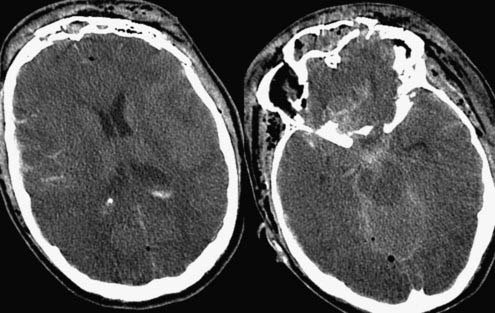
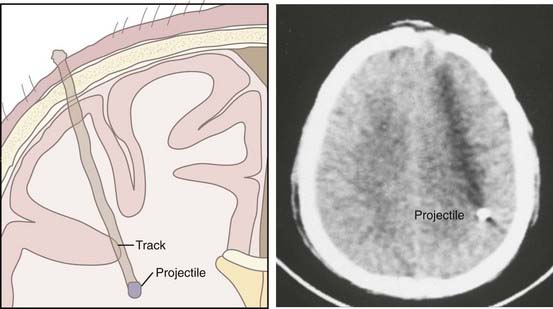
There are three components to ballistics: (1) interior, (2) exterior, and (3) terminal. Interior ballistics is defined as the science of motion of a projectile through a gun barrel as a result of combustion and expansion of a powder charge, a science extensively studied in the early 18th century by the British scientist Benjamin Robins and the Anglo-American researcher Benjamin Thompson.44,45 Exterior ballistics is the projectile’s behavior in a medium such as air and is dependent on the projectile’s shape, caliber, weight, initial velocity, and ballistic coefficient. Niccolo Tartaglia and Galileo defined the parabolic trajectory of a bullet in space until it loses all of its kinetic energy.44–50 The behavior of a projectile on impacting its target is termed terminal ballistics. Factors important in terminal ballistics include penetration, tissue density, fragmentation, detonation, shape of the charge, blast overpressure, combustion, and incendiary effect.44–46,48,50 The science of ballistics has evolved considerably since 1411 when the first matchlocks appeared in Europe. The introduction of rifling in 1520, elongated bullets by Delvigne in 1841, minié bullets in 1847, and breech loading and coated bullets in the 1850s resulted in projectiles with velocities greater than 2000 ft/sec (615 m/sec).44,45,50–52 The wounding energy (E) of a projectile depends mainly on its weight and velocity; hence, E =  M(VI2 − VR2), where M is the projectile’s weight, VI is the impact velocity, and VR is the residual velocity if the projectile has a perforating mode.45,53 The small-firearm injuries encountered in civilian GSWHs follow conventional ballistic rules of wounding energy; however, when the velocity of a projectile crosses 700 m/sec, the wounding energy depends on the power (P) of the projectile and is expressed as P = MV3. Many of the victims in the vicinity of a cased explosive or an improvised explosive device (IED) will incur injuries by fragments with a velocity of greater than 700 m/sec and low ballistic coefficient. Translation of kinetic energy into tissue damage is brought about by the tremendous amount of crushing pressure exerted on the brain parenchyma. Juxtamissile pressure affects the brain tissue immediately in the path of a projectile and may be in the thousands of atmospheres. Longitudinal strong shock waves (Fig. 336-1) start immediately after impact of the projectile with brain tissue and travel in spheres ahead of the projectile with velocities in excess of 1460 m/sec.54 Shock waves last up to 10 µsec and measure up to 80 atm. Ordinary pressure waves measuring up to 20 to 30 atm are generated as the projectile transfers its kinetic energy to the surrounding brain tissue and produces a temporary cavity.54 The negative pressure generated by the temporary cavity can suck contaminated material into the cavity, which must be débrided during surgical management of the permanent cavity.45,54,55 Experiments with 20% gelatin have indicated that as the projectile is dissecting its way through a gelatin cube, it produces a head cone and a tail splash (Fig. 336-2).55,56 Tissue density is critical in defining parenchymal damage. Solid organs such as the brain have tissue densities up to 800 times that of air, thus giving high-velocity bullets explosive power.52 The sectional area defines the impact surface of a projectile and is determined by the shape and flight characteristics of a projectile, including yaw (Fig. 336-3), spin, precession, tumbling, nutation, and drag, all of which determine the ballistic coefficient.44–51,54,56–58 GSWHs, being contact or near-contact injuries, not only plow through the brain but also deposit a tremendous amount of energy that disrupts brain tissue and major blood vessels, displaces the brainstem, arrests cardiorespiratory function, and results in instantaneous death in more than 70% of victims (Fig. 336-4).31–3354
M(VI2 − VR2), where M is the projectile’s weight, VI is the impact velocity, and VR is the residual velocity if the projectile has a perforating mode.45,53 The small-firearm injuries encountered in civilian GSWHs follow conventional ballistic rules of wounding energy; however, when the velocity of a projectile crosses 700 m/sec, the wounding energy depends on the power (P) of the projectile and is expressed as P = MV3. Many of the victims in the vicinity of a cased explosive or an improvised explosive device (IED) will incur injuries by fragments with a velocity of greater than 700 m/sec and low ballistic coefficient. Translation of kinetic energy into tissue damage is brought about by the tremendous amount of crushing pressure exerted on the brain parenchyma. Juxtamissile pressure affects the brain tissue immediately in the path of a projectile and may be in the thousands of atmospheres. Longitudinal strong shock waves (Fig. 336-1) start immediately after impact of the projectile with brain tissue and travel in spheres ahead of the projectile with velocities in excess of 1460 m/sec.54 Shock waves last up to 10 µsec and measure up to 80 atm. Ordinary pressure waves measuring up to 20 to 30 atm are generated as the projectile transfers its kinetic energy to the surrounding brain tissue and produces a temporary cavity.54 The negative pressure generated by the temporary cavity can suck contaminated material into the cavity, which must be débrided during surgical management of the permanent cavity.45,54,55 Experiments with 20% gelatin have indicated that as the projectile is dissecting its way through a gelatin cube, it produces a head cone and a tail splash (Fig. 336-2).55,56 Tissue density is critical in defining parenchymal damage. Solid organs such as the brain have tissue densities up to 800 times that of air, thus giving high-velocity bullets explosive power.52 The sectional area defines the impact surface of a projectile and is determined by the shape and flight characteristics of a projectile, including yaw (Fig. 336-3), spin, precession, tumbling, nutation, and drag, all of which determine the ballistic coefficient.44–51,54,56–58 GSWHs, being contact or near-contact injuries, not only plow through the brain but also deposit a tremendous amount of energy that disrupts brain tissue and major blood vessels, displaces the brainstem, arrests cardiorespiratory function, and results in instantaneous death in more than 70% of victims (Fig. 336-4).31–3354
The science of ballistics and quantification of the wounding energy in cased ammunitions and complex explosives, such as car bombs and IEDs, is much more unpredictable in that it is a combination of primary blast overpressure, PBI, and closed head injury.4,10,11,13,16 Although injuries during the American Civil War were primarily due to bullets, injuries in subsequent international and regional conflicts have been caused to a major extent by shell fragments.55,59–64 In a recent presentation at the annual meeting of the conference on Advanced Technology Applications for Combat Casualty Care (ATACCC) in Florida, Bell and coauthors reported that 228 of 408 patients who sustained TBI in OIF suffered PBI and 139 had closed head injury.65 In 229 patients the predominant mechanism was exposure to complex explosive devices, which resulted in significant blast overpressure on the brain parenchyma in addition to PBI and closed TBI (Fig. 336-5). Additional mechanisms behind TBI in modern warfare and terror attacks include thermal and ischemic injuries and energy sources not appreciated in a typical measurement spectrum, such as electromagnetic energy.4,10,11 Fragments tend to most commonly be low-velocity spall (see Fig. 336-7).4,10,11,60,63,66–70 This spall can emanate from the casing of the explosive device and from packed supplemental bolts, nails, ball bearings, or the metal from a vehicle-borne explosive (i.e., a car bomb). In some cases this spall can also contain body parts of the suicide bomber, window frames, glass, gravel, or in-driven bone fragments acting as secondary impacting fragments. When such explosives impact a patient, the results vary. Factors such as proximity to the explosion, protection by both personal and vehicular armor, and the effect of the environment are all important.4 Open field explosions are less likely to have the effect of reverberating pressure waves, building collapse, or fragmenting glass, as is commonly seen when victims are located within a closed structure.4 Explosions occurring within a closed space are particularly lethal because of the proximity to the explosion, the incendiary nature of the blast, and the reverberation of the blast force.4,10,16 This lethality is commonly witnessed in bombs detonated in buses, trains, planes, and enclosed buildings.69,70 The number of survivors is typically inversely proportional to the size of the enclosure, with bus bombs having the highest lethality.69
Pathology
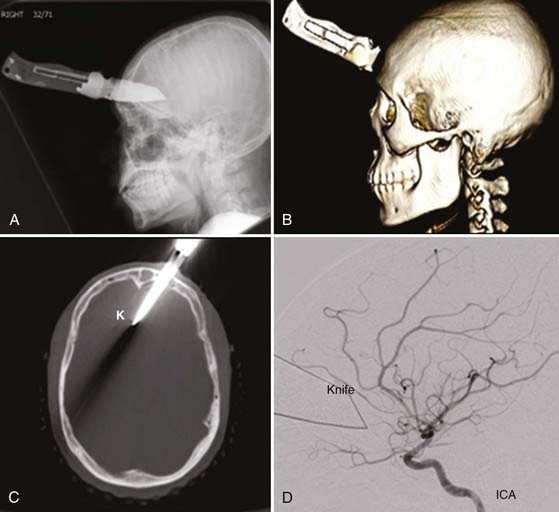
Low-velocity sharp objects, which lack any definable ballistics, penetrate the scalp, skull, and dura and lacerate the brain parenchyma, including the cortex, subcortical white matter, basal ganglia, and diencephalon or brainstem and any blood vessels in their path (Fig. 336-6).71,72 Similarly, low-velocity projectiles from artillery shells, IEDs, and spent bullets cut into the brain just like sharp objects do (Fig. 336-7). The focal motor, cognitive, and behavioral consequences of these injuries depend on the neuronal circuitry that is interrupted and the completeness of injury to blood vessels, hence producing subarachnoid hemorrhage, intracranial hematomas or traumatic intracranial aneurysms (TICAs), and arteriovenous fistulas (AVFs).71–83
The pathology with contact or near-contact injuries by civilian GSWHs is much more devastating.23,27,40,41,84 In a detailed necropsy study of 254 patients who died of firearm injuries, Freytag noticed single-track injury (permanent cavity) from ricochets in 82% of cases and multiple tracks in the remaining cases. In her study an ischemic ring was seen surrounding the permanent cavity and was topped by a layer of small hemorrhages from disruption of blood vessels.23 A robust class III literature indicates that in victims of civilian GSWHs who survived the initial injury to reach a trauma center, the path of penetration and the extent of brain injury defined the mortality. The mortality was 48% after lobar injuries,22,31,41,42,85,86 72% after unilateral multilobar injuries,22,31,35,43 77% if the midsagittal plane was crossed,22,30,31,40–43,87 84% if the midcoronal plane was crossed,86,87 and 96% if both the midsagittal and midcoronal planes were crossed.86,87 In 2000, 45 patients survived long enough to reach one of the eight trauma centers in the state of Maryland. Of the 24 patients admitted to the shock trauma center, 10 survived: 2 of 12 patients with perforating, 5 of 9 patients with penetrating, and 3 of 3 patients with tangential injuries. The relationship of the injury mode to mortality was also reflected in 816 soldiers from the Iran-Iraq War.88 In this study the proportion of patients who survived a median of 41 hours to reach an academic center were as follows: 54.8% with penetrating, 22.4% with tangential, and 7.5% with perforating injuries. The incidence of intracranial hematomas differs between reports: acute subdural hematoma, 3% to 56%27,42; intracerebral hematomas, 4% to 37%24,42; intraventricular hematoma, 1% to 56%24,27; and subarachnoid hemorrhage, 9% to 78%.21,35
In soldiers with varying amounts of body armor, the pattern is quite different. What had previously been fatal PBIs now become treatable brain injuries as a consequence of secondary damping of energy by the helmet.4,11,15 The energy absorbed by the helmet results in mechanical deformation of the inner and outer protective covering of the shield. The outer deformity tends to be smaller and focal and rarely completely penetrates, whereas the inner deformity tends to have a broader base with less depth and also rarely penetrates. The deformation of the inner aspect of the helmet may impact on the underlying scalp, transfer energy to the skull, and deform the calvaria and intracranial compartments. A piston-like deformity of this inner table can lead to a stellate scalp laceration with a severe abrasion or burn, and the resulting impact on the skull leads first to a fracture and loss of anatomic continuity of the skull. In extreme cases, commonly seen after an IED impact, the dura is violated and the local cerebral tissue will be contused by both blunt trauma and secondary impacting fragments of bone or body armor (or both). These fragments of bone typically course in a radial direction from the point of impact. Traveling perpendicular to the cortical vasculature underlying the sulci and gyri, they disrupt the vessels in their path (Fig. 336-8).
Military personnel incurring complex injuries from explosive devices sustain blast overpressure and penetrating or closed head injuries.4,11,13,16 Reporting on 234 American soldiers who were evacuated a mean of 7.4 ± 8.6 days after their war injuries, Bell and coauthors noted severe head injury (Glasgow Coma Scale [GCS] score <9) in 61 (26%).65 It was projected that a significant proportion of wounded OIF soldiers suffered from high-frequency low-amplitude or low-frequency high-amplitude shock waves, which rendered these injuries much more complex to comprehend.4,10,16 Low-intensity blast waves are not necessarily accompanied by pulmonary or gastrointestinal injuries. Because disruptive energy is transmitted to the brain with complex and high-energy blasts and may even occur through major blood vessels, TBI is not prevented by a protective helmet.10 High- and low-frequency blast waves disrupt the blood-brain barrier and produce massive brain swelling in a very short time,89–92 thereby necessitating urgent decompressive craniectomy, and when low in energy, such blast waves may result in cytoskeletal and diffuse axonal injury that leads to neurodegeneration.4,10,11,20,93
Clinical Findings
Demographics
Most patients involved in civilian GSWHs are males (87%) in the third to fourth decade of life and are nearly equally divided between homicides (50%) and suicides (46%), with a small percentage being due to accidents (4%). Almost 78% of the victims of homicide are black; 86% of the victims of suicide are white.21–25,28–32,34,36,39,42,84,94–98 Unpublished data from the Trauma Registry of the R. Adams Cowley Shock Trauma Center indicate that from 2000 through 2005, of the 333 patients admitted with civilian GSWHs, only 34 were female.99 The mean age was 30.6 ± 14.4 years, 214 were black, 100 were white, and 19 were other races. The GSWHs occurred concomitant with injuries to the face in 165, the upper extremity in 94, the thorax in 74, the lower extremity in 51, the neck in 45, the spine in 43, and the abdomen in 42 patients. The Injury Severity Score (ISS) was 31 ± 16, the head Abbreviated Injury Score (AIS) was 4.7 ± 0.7, and the Trauma Injury Severity Score (TRISS) was 0.52 ± 0.4. Military victims of PBI tend to be younger,59,60,63,64,88,100 and in OIF the mean age was reported to be 24.7 years.65
Level of Consciousness
When sharp objects,71,72,76,79,83 low-velocity spall,59,60,63,64,66,100 and spent bullets penetrate the brain, they may cause focal deficits; however, if they do not disrupt the neuronal circuitry in the brainstem tegmentum or ascending reticular activating system, they may not cause a depressed level of consciousness or coma.18,27,71,72,76,79,83,101–108
In civilian PBI an altered level of consciousness is the rule.* In a prospective study of 100 civilian GSWHs by the Barrow Neurological Institute, Grahm and associates reported postresuscitation GCS scores to be 3 to 5 in 58 patients, 6 to 8 in 8 patients, 9 to 12 in 12 patients, and 13 to 15 in 22 patients.41 Unpublished data from the University of Maryland Trauma Registry in Baltimore showed 333 patients with GSWHs in the period 2000 to 2005.99 Of these 333 patients, 187 (56%) had a GCS score of 3 to 5, 31 (9%) a GCS score of 6 to 8, 20 (6%) a GCS score of 9 to 12, and 95 (29%) a GCS score of 13 to 15. Similarly, Liebenberg and coauthors reported a GCS score of 3 to 8 in 70.4% of their patients evaluated from West Sussex England (Fig. 336-9).28
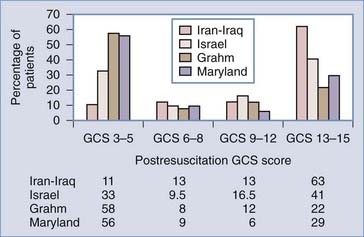
FIGURE 336-9 Stratified admission Glasgow Coma Scale (GCS) scores of victims of penetrating brain injury from the frontlines of the Iran-Iraq War, the Israeli involvement in Lebanon, and civilian gunshot wounds to the head (see references 41, 60, 66, 99).
Military experience in recent years has recorded varied levels of consciousness at the time of arrival at a medical facility. In 1990, Aarabi reported the functional outcomes of 435 patients from the Iran-Iraq War.66 In that study, 274 (63%) patients were admitted to a tertiary hospital with a GCS score of 13 to 15, 57 (13%) with a GCS score of 9 to 12, 58 (13%) with a GCS score of 6 to 8, and 46 (11%) with a GCS score of 3 to 5. In 1991, Brandvold and coworkers, reporting on 113 war casualties from the Israeli involvement in Lebanon, recorded 41% with a GCS score of 13 to 15, 16.5% with a GCS score of 9 to 12, 9.5% with a GCS score of 6 to 8, and 33% with a GCS score of 3 to 5.60 Natural selection by prolongation of time at the scene may explain some of the differences. In the Iran-Iraq War, time after injury to admission to the tertiary academic facility was 49 hours, whereas in Israel the average time at the scene was 2 hours.60,110 Bell and colleagues recorded the following GCS scores in 234 patients from OIF who were treated by neurosurgeons within 0.5 to 1.5 hours of their injury and evacuated to the continental United States (CONUS) within 7 days of their injury, with the last 38 patients arriving in CONUS within 4 days of their injury: GCS scores of 12 to 15 in 103, 9 to 11 in 70, 6 to 8 in 37, and 3 to 5 in 24 subjects.65 In a report presented by Ling, almost 20% of the military personnel deployed in OIF were subject to TBI; however, only a minority suffered secondary blast injuries and had a very low GCS score.4
Brainstem Function
Checking for brainstem dysfunction (i.e., abnormal pupillary response to light, corneal and doll’s eye reflexes, cold calorics, cough and gag reflexes) is particularly important in civilian GSWHs and military PBIs. These injuries reflect damage by either brain shift secondary to a temporary cavity resulting from ordinary pressure waves54 or uncontrollable intracranial hypertension secondary to swelling or hematomas and hence are of major prognostic significance.38,54,57,111,112 With regard to the pupils, one has to consider end-organ injury resulting from the bullet tracking around the orbital apices and cavernous sinuses. In the report of Grahm and associates, 95% of the patients with GCS scores of 3 to 5 did not exhibit any pupillary reaction, whereas in patients with higher scores, a lack of reaction was noticed in only 50%.41 In the series of Kaufman and coworkers, 30 of 38 patients with no abnormal pupillary response to light survived, but only 1 in 70 survived if both pupils were not reactive to light.40 Stone and colleagues believed the GCS score to be much more valuable in predicting outcome than the pupillary reaction to light was.35
Focal Deficits
Depending on the entrance site, a persistent focal neurological deficit is quite common in the survivors of GSWH or military PHI. In 1872, Mitchell described 7 individuals with cranial nerve injuries, including 4 with facial nerve injuries, after GSWHs during the American Civil War.113 Stookey and Scarff reported 72 instances of facial nerve injuries in 153,537 war casualties during 1917 and 1918.114 Orbital injuries during World War I (WWI) were the subject of extensive discussion by Lagrange.115 Examining injuries during World War II (WWII), Jefferson and Schorstein reported 14 patients with complex trigeminal damage,116 and Lathrop reported 150 patients with facial nerve damage.117 The incidence of visual field cuts in the Vietnam Head Injury Study (VHIS) cohort as reported by Salazar and colleagues was 13.7%.118 Eighty of 1303 casualties from the Iran-Iraq War had cranial nerve involvement: the optic nerve or globe in 60, the olfactory nerve in 24, the oculomotor nerve in 23, the abducens nerve in 13, the trochlear nerve in 11, the trigeminal nerve in 10, the facial nerve in 7, the vestibulocochlear nerve in 3, the glossopharyngeal nerve in 3, the vagus nerve in 3, and the hypoglossal nerve in 2.119 Mohr and colleagues studied speech involvement and recovery in 244 of 1030 casualties from Vietnam (VHIS cohort).120 The authors reported that sensorimotor aphasia usually changed to motor aphasia; the motor aphasia disappeared and the sensory aphasia persisted. Aphasia correlated with a bullet as the cause (versus a fragment, P < .03) and initial loss of consciousness (P < 10−6). In the same study the incidence of paresis was 28% (292 of 1030 casualties). Smutok and coauthors reported that 55% of patients in the VHIS cohort had recovered from the hemiparesis 15 years after their missile head wound.121 The incidence of motor deficits, visual field cuts, and speech difficulties in the casualties from the Iran-Iraq War was 34.6%, 13.7%, and 6.1%, respectively.3
Mild Traumatic Brain Injury, Blast, and Posttraumatic Stress Disorder
More than 320,000 OIF soldiers (20% of the deployed force) may have suffered varying degrees of TBI.130 Although the functional, cognitive, and psychological consequences of penetrating and closed head injuries incurred in armed conflicts have been extensively investigated over many years,13,38,54,59,63,66,100,118,122–129 there is no clear understanding of the exact pathogenetic mechanisms and epidemiology of MTBI and PTSD as a consequence of blast overpressure.4,11–13,16–18,65
Experimental studies indicate that blast waves have some of the characteristics of complex Friedlander waves. Blast waves rise instantaneously to a peak overpressure and decay exponentially, followed by a negative phase. Blast waves interact with the central nervous system directly through the cranium or indirectly through oscillating pressure in fluid-containing large blood vessels.10,130 Protective body armor does not prevent the interaction of brain parenchyma with shock waves.4,10 High-frequency (0.5 to 1.5 kHz) low-amplitude stress waves damage the blood-brain barrier, and low-frequency (<0.5 kHz) high-amplitude shear waves damage the gray-white matter junction. The result is brain edema, cellular necrosis and apoptosis, cytoskeletal damage, diffuse axonal injury, and neuronal degeneration.10,11,16,18,65,92,130 These structural injuries may be the backbone of PTSD as a consequence of MTBI after exposure to blast overpressure waves.3,4,9,10,13,16,17,130 A recent study of the southeastern European regional conflicts by Cernak and colleagues reported the presence of long-term signs and symptoms reflecting a central nervous system disorder in 30% of 665 of patients sustaining blast overpressure.16 In this study pure PTSD was noted in 11% of patients.
TBI is considered to be a strong cause of PTSD and physical health problems among veterans of the Iraq War. A survey of 2525 U.S. soldiers 3 to 4 months after their return from a year-long deployment to Iraq indicated a significant association of PTSD and MTBI. Of these soldiers, 124 (4.9%) reported loss of consciousness and 260 (10.3%) reported altered mental state. Of the soldiers reporting loss of consciousness, 43.9% had PTSD as compared with 27.3% who reported altered mental status. PTSD and depression were important mediators of the relationship between MTBI and poor general health, missed workdays, and medical visits. A similar study of 2235 American veterans by Schneiderman and colleagues showed about 12% with MTBI and 11% with PTSD.5 Other studies have corroborated these findings.1,7–9,16 Further studies are in progress to understand the exact molecular, cellular, and clinical manifestations of blast-induced MTBI and PTSD.4,10
Management
Imaging Studies
Computed Tomography
Injury Profile
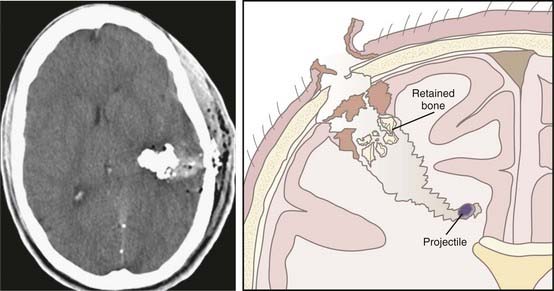
Computed tomography (CT), including three-dimensional reconstruction of the head, defines the entry site and trajectory of the fragment into the brain, terminal ballistics (perforating, penetrating, and tangential),66 and involvement of the paranasal sinuses, orbits, skull base, and mastoids. It defines the missile track,21 number of tracks and ricochet,23 whether the penetration is across the midsagittal or midcoronal planes,27 and the presence or absence of intracranial hematomas such as acute epidural, subdural, intracerebral, or intraventricular hematomas.24,27,35,42 The extent of brain edema and ischemia and brainstem involvement is defined by CT (see Fig. 336-5).
Vascular Injury Profile
Direct or indirect evidence of vascular injury can clearly be shown by cranial CT. Various degrees of subarachnoid hemorrhage and delayed traumatic intracerebral hematomas can indicate the need for CT or conventional angiography. Patients with pterional and orbitocraniocerebral injuries, fragments associated with acute or delayed intracerebral hematomas, and fragments passing through two dural compartments are specifically prone to harbor TICAs.101,131
Involvement of Air Sinuses and Mastoid Air Cells
Particular attention should be paid to fragments penetrating the paranasal air sinuses and mastoid air cells. These patients are specifically susceptible to leakage of cerebrospinal fluid (CSF) and deep intracranial infections.88,110,132,133
Retained Fragments
There is no question that CT is the best tool for diagnosing retained bone or missile fragments,134–136 especially if the surgery is being performed for minimal débridement.
Deep Infections
During WWII, almost 25% of retained bone fragments were a nidus for deep infections such as abscesses. With the widespread use of antibiotics and proper débridement, the chance of deep central nervous system infection occurring has dropped precipitously; however, for the rare cases of brain abscess attributable to inadequate débridement, the track of the projectile needs to be kept under close scrutiny for several weeks after the missile head wound.110,137–140
Prognosticating Tool
There seems to be a statistically significant relationship between outcome and CT profile,* especially in the case of intraventricular hematoma, penetration of the midsagittal and midcoronal planes, perforating injuries as opposed to tangential injuries, and injuries involving multiple lobes (see Fig. 336-4).
Medical Management
The prehospital rescue, intubation, oxygenation, ventilation, volume resuscitation, and medical management of patients with PBI must clearly be adapted from different prehospital, emergency department, critical care, and surgical guidelines.141–145 Broad-spectrum antibiotics and anticonvulsants should be used according to the guidelines for the “Management and Prognosis of Penetrating Brain Injury.”141
Surgical Management
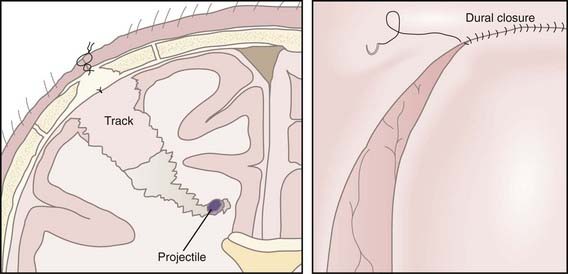
Débridement and Repair of the Scalp
Scalp lacerations from missile head wounds are usually contaminated, have devitalized edges, and may be hard to repair. Several studies have indicated that wound contaminants originate from organisms on the skin of the soldier or civilian subject. Staphylococci with or without gram-negative organisms (coliform bacteria, Aerobacter aerogenes, Klebsiella species, and Acinetobacter species) were the most frequently encountered skin contaminants during WWII and the Vietnam and Iran-Iraq wars.67,134,146,147 Preliminary unpublished data indicate that Acinetobacter species is one of the contending organisms encountered in OIF, and it was also cultured from the skin of soldiers during the Iran-Iraq War.134,148 When scalp is penetrated by a projectile, it is shredded, torn, or burned with devitalized edges of up to a few millimeters. If feasible, it is strongly recommended that a plastic surgeon be consulted for primary closure of the skin over a torn dura, especially if the dural tear is at the base in the vicinity of the basal cisterns, near the air sinuses or mastoid air cells, to prevent CSF fistulas.88,132 In addition, patients with ventricular penetration are subject to CSF leakage from the skin incision.88 Tripod incisions are not favored because of the possibility of delayed healing at their center. The skin edges are débrided and approximated in two layers. We prefer a continuous monofilament skin closure. Sutures are not to be removed for up to 2 weeks.
Craniectomy versus Craniotomy
Although craniectomies around the entrance site of a projectile have been the favored technique in previous military conflicts,60,63,67,88,100,149 the present recommendation is craniotomy and débridement of the skull with replacement of the bone to avoid the future need for cranioplasty. Contrary to civilian decompressive craniectomies, where the bone flap is stored in a tissue bank or the patient’s abdominal wall for future reimplantation, this policy was stopped in OIF because of the increased risk for contamination and infection at the implanted site.89,148
Débridement and Watertight Closure of the Dura Mater
In complex orbitofaciocraniocerebral and temporal fossa injuries with exposed air sinuses and mastoid air cells and in patients with extensive injury to the scalp, dura, and brain, a multidisciplinary approach to repair the dura and scalp is necessary to prevent postoperative CSF fistulas and deep infections.110,132
Débridement of Devitalized Brain
The degree of surgical débridement of devitalized brain tissue remains controversial.61 On the basis of class III historical and limited experimental evidence,129,137–140,150–154 traditional protocol-driven military practices have been aggressive débridement and an attempt to extract all retained bone fragments.61,67,110,155 Brandvold and colleagues,60 Taha and associates,156 and more recently Amirjamshidi and coworkers,135 based on their experience in Israel, Lebanon, and Iran, respectively, have reported on minimal débridement of missile head wounds in special circumstances (Figs. 336-10 and 336-11). Although we agree that every effort should be made to preserve eloquent cortex, one needs to understand that civilian GSWHs and a significant number of military missile head wounds are much more devastating and must be managed in consultation with ear, nose, and throat, ophthalmologic, oromaxillofacial, and plastic surgeons to preserve the integrity of the basal dura in the region of the orbits, mastoid air cells, and air sinuses.61,88,132,133,141 Minimalism is only applicable to small fragments with small entrance wounds and no evidence of massively devitalized scalp and no penetration of the air sinuses, ventricular system, or mastoid air cells. In a recent analysis of the data reported by the aforementioned authors, Carey found increased risk for deep infections with minimally débrided missile head wounds.61
Débridement of Retained Fragments
Retained bone fragments after a missile head wound with or without previous débridement are always a source of worry. Reports from WWII and the Vietnam War indicate that retained bone fragments could be a source of abscess and deep infections.67,129,137–140,152,154,157 Retained bone fragments after satisfactory débridement may not cause significant infection over the long run, and there does not seem to be a reason for aggressive pursuit of the fragments.88,136
Repair of the Skull Base
Recent wartime explosive injuries from a transfrontal or transtemporal direction may disrupt the anterior and lateral skull base. Such injuries are associated with significant risk for CSF leaks and loss of anatomic continuity between the anterior cranial fossa, orbits, maxilla, and infratemporal fossa. During the recent conflict this has led to an aggressive strategy of early skull base repair with titanium mesh, local pericranium, fat, temporalis fascia, and muscle. This step is followed by more extensive skull base reconstruction at level 5 medical centers consisting of rotational or myocutaneous free flaps in patients with persistent CSF leaks, progressive skull base deformity, and encephalocele.88,110,132,133,148
Complications
Vascular Injuries with Gunshot Wounds to the Head
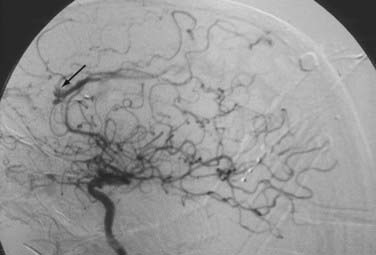
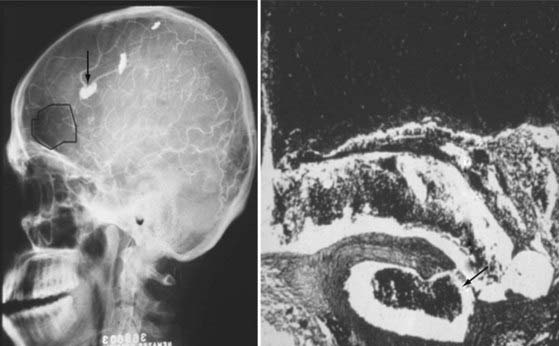
The true incidence of traumatic neurovascular injury in patients with blast overpressure, closed brain injury, and PBI remains largely speculative.19,27,101,102,106,131,158 The incidence of TICA after such injuries ranges from 3% to 40%, depending on the timing of imaging studies. The urgency to detect and intervene is related to the consequences (delayed traumatic intracerebral hematoma, new stroke, persistent coma, death) associated with rupture.80,101,102,108,131 Before the first reported series of endovascular management of TICAs in 1993,159 treatment options available to the neurosurgeon were limited to balloon occlusion,160–165 balloon trapping,166 copper wire thrombosis,167,168 surgical ligation, and clipping or occlusion of the parent artery with or without bypass.101,102,104,166,169
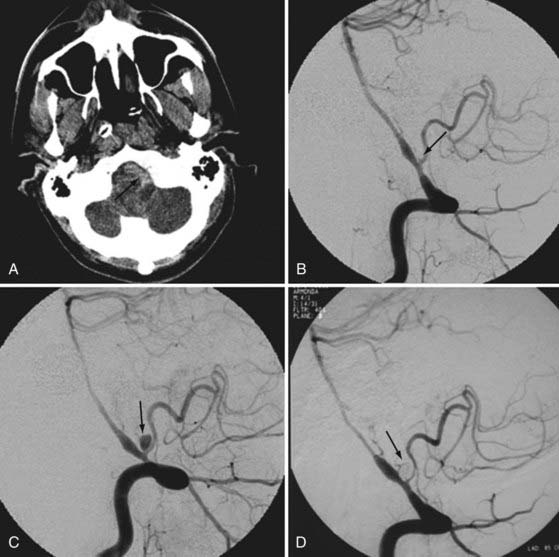
The incidence and natural history of TICA in war casualties are unknown. Although first reported by Lunn during WWII,107 only a few cases of TICA were reported in Vietnam War casualties.103,105 In one report from the Iran-Iraq War, cerebral angiography an average of 17 days after missile head wounds in 255 patients disclosed 8 aneurysms (3%). Of significance was discovery of 6 of these aneurysms before and 2 after rupture.131 A subsequent study of the same conflict by Amirjamshidi and colleagues described a series of 1150 penetrating head injuries.102 One specific and uniform subpopulation within this study was the 470 patients who underwent digital subtraction angiography 2 to 35 (average, 16.2) days after their initial injury. Twenty-seven traumatic aneurysms/AVFs were discovered in this group (5.7%).102 Jinkins and coworkers performed cerebral angiography within 24 hours of GSWHs in 12 patients and found 3 internal carotid/vertebral and 1 combined aneurysm/AVF (33%).106 In a recent study by Cohen and colleagues, angiography was performed in 34 patients at high risk of harboring a TICA.19,101,131,158 These investigators found 10 TICAs in 25 (40%) patients with PBIs involving the pterion or when the fragment crossed the midline.19 The timing of angiography after a missile head wound may be an in important factor in detecting aneurysms.19,101,102,106,131,158 Figure 336-12 shows a 70-year-old man after attempted suicide by GSWH in the glabella. Angiography within an hour of admission to the emergency department showed extravasation of dye in the interhemispheric space. The patient died soon after admission. An autopsy study of Lunn’s case by Dr. Dorothy Russell and cases reported during the Iran-Iraq War indicated that TICA caused by shell fragments is due to partial laceration of the arterial wall (Fig. 336-13).107,131
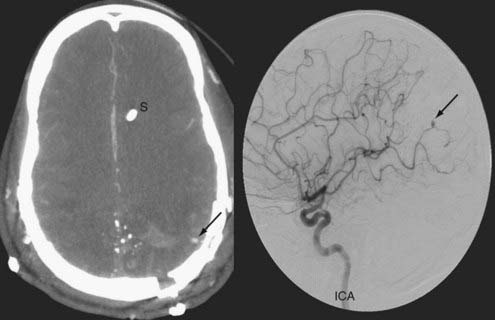
The “Management and Prognosis of Penetrating Brain Injury” guidelines recommend angiography for patients with PBI who are at risk for TICA.141 Risk factors include orbitofaciocraniocerebral injuries, injuries near the pterion, and patients harboring intracranial hematomas.19,101,141 It is recommended that any patient with these risk factors undergo either CT angiography or conventional angiography to rule out TICA (Fig. 336-14).
The current conflicts in the Middle East have helped us better understand the pathogenetic mechanisms of TICA and cerebral vasospasm secondary to blast injuries and PBIs and to provide better management by endovascular navigation.18,19 Over a 5-year period at the National Naval Medical Center in Bethesda, Maryland, and the Walter Reed Army Medical Center, 279 angiographic studies were performed in 187 patients (25 with closed craniocervical injury, 162 with penetrating craniocervical injury) and resulted in the detection of 64 vascular injuries in 47 patients and 47 cases of posttraumatic vasospasm. The vascular injuries were characterized by TICAs (31 aneurysms), traumatic extracalvarial aneurysms (TECAs) (19 aneurysms), dissecting aneurysms,170 and AVFs.66 The average TICA size on admission was 4.7 mm, with an observed increase in aneurysm size in 11 patients. Within the TICA/TECA group, 24 aneurysms in 23 patients were treated endovascularly with either coiling or stent-assisted coiling, which resulted in preservation of the parent artery in 12 of 24 vessels (50%). Three patients in this group progressed despite endovascular treatment and required definitive clip exclusion. Thirteen additional aneurysms in 8 patients were treated surgically, and the parent artery was preserved in 4 cases (31%). Twelve of the 13 TICAs/TECAs resolved spontaneously without treatment, with 1 of the 13 rupturing and resulting in death. Six aneurysms ruptured during the study and resulted in 3 deaths. Five of 6 ruptures occurred in TICAs in which an interval increase in size was noted angiographically. Of the 11 dissections, 6 were treated with either a stent or stent-assisted coiling if a significant aneurysm was present. The remaining 5 dissections resolved spontaneously with just antiplatelet therapy. Stents were deployed in all cases in the setting of minimal intracranial hemorrhage or in a delayed fashion after the resolution of intracranial hemorrhage. This is an important point because all patients with a deployed stent required pretreatment with aspirin and clopidogrel (Plavix) and a minimum of 6 weeks of antiplatelet therapy after deployment. In addition, a decision to stent the carotid or vertebral artery was made if an infarct occurred while the patient was receiving antiplatelet therapy or if a significant flow-limiting intimal flap was present. The three AVFs were treated in the following fashion. The first AVF was a direct carotid-cavernous fistula (CCF) with flow-limiting carotid dissection on the same carotid artery in a patient without significant intracranial injury. It was necessary to first stent the carotid dissection to access the diseased cavernous segment. The direct CCF was then treated by deployment of a stent and transarterial coiling of the cavernous sinus. The second CCF was occluded with transarterial coiling using 200 cm of coil. The last, a vertebral artery AVF, was surgically occluded 16 days after the initial injury. In the series of Cohen and colleagues, 1 of 13 patients treated with a bare stent and coiling had a growing intracavernous pseudoaneurysm necessitating occlusion and bypass of the internal carotid artery.19 No recanalization occurred in 12 patients. In no patient in this series was renewed bleeding seen after a mean follow-up of 2.6 years.
Intracranial Infections
Missile head wounds are contaminated wounds. Microbiologic studies of incurred scalp wounds, in-driven bone fragments, and brain tracks during WWII and the Vietnam and Iran-Iraq wars indicated that 35% to 98% of scalp wounds, 21% to 83% of in-driven bone fragments, and 28% to 78% of brain tracks were contaminated with gram-positive and gram-negative organisms.67,134,141,147 Unpublished data from OIF indicate that Acinetobacter, which was cultured from the scalp wounds, in-driven bone fragments, and brain tracks of soldiers wounded during the Iran-Iraq War, was a commonly encountered organism in bone flaps implanted in the abdominal wall of American soldiers after decompressive craniectomy in Iraq.134,148 The extent to which contaminating organisms contribute to deep wound infections is debatable; however, since WWII, combat troops in all the regional conflicts and civilians with GSWHs have been treated with broad-spectrum antibiotics for a variable number of days from the time of injury. Although a Cochrane Database meta-analysis did not support antibiotic prophylaxis for preventing meningitis in patients with basilar skull fracture,171 the guidelines on “Management and Prognosis of Penetrating Brain Injury” recommend prophylactic antibiotics for all patients with missile head wounds.141 Deep infection remains the most important aspect of PBI that a neurosurgeon has to deal with. Strong class III historical evidence as far back as WWI supports the value of meticulous wound débridement, removal of retained bone fragments, and watertight closure of the dura.* Simple scalp débridement and meticulous closure, as recommended by Cushing,123 instead of leaving the scalp undébrided and packed, as recommended by Whitaker,173 precipitously dropped the rate of deep wound infections—even without the benefit of antibiotics. Cushing’s tradition was continued into WWII and the Korean and Vietnam conflicts, and the infection rate was kept as low as 6% to 15%.104,138,174
Posttraumatic Epilepsy
PBI is one of the major risk factors for posttraumatic epilepsy.93,170,175–180 Studies of veterans from WWI, WWII, and the Korean, Vietnam, and Iran-Iraq wars indicate that between 34% and 50% of victims of PBI become epileptic when monitored for 2 to 15 years.93,170,177,179–182 Follow-up studies indicated that the incidence of posttraumatic epilepsy in victims of PBI is higher than that in victims of closed head injury.183–186 In the study of Annegers and associates, the incidence of posttraumatic epilepsy in those with mild, moderate, and severe closed head injury was 1.5%, 2.9%, and 17%, respectively.183 In the studies of Temkin and colleagues, risk factors for the development of seizures up to 2 years after head injury included evacuation of subdural hematoma, surgery for intracerebral hematoma, severe head injury, early seizures, a depressed skull fracture that was not elevated, dural penetration by injury, at least one nonreactive pupil, and parietal lesions on CT.185,187,188 Risk factors for veterans to become epileptic include low GCS score at admission; low Glasgow Outcome Scale (GOS) score at follow-up; early posttraumatic seizure; PBI involving the temporal and parietal lobes; deep central nervous system infections; focal sensory/motor, visual, and speech deficits; intracerebral hematoma; and brain volume loss.93,178,179,182 In the studies of Salazar, Aarabi, and others, retained bone fragments were not significant prognostic factors for the development of epilepsy.170,178,179 Several prospective randomized studies have indicated that phenytoin, carbamazepine, and valproate are effective in preventing early posttraumatic seizures in patients with closed head injury, but these medications do not prevent long-term epileptic seizures.184–188 The guidelines for “Management and Prognosis of Penetrating Brain Injury” recommend prophylactic antiseizure medications for the first week after PBI but not beyond that.141
Prognosis
Evacuation within the first hour after injury, damage control by hemostasis and asepsis, and definitive management in well-equipped centers in Iraq, the Landstuhl Regional Medical Center in Germany, or even back in the United States at the Walter Reed Army Medical Center within 36 hours of injury have significantly reduced the mortality rate of American troops in Iraq and Afghanistan.189 The percentages of lethal war wounds among U.S. Soldiers in the American Civil War, WWI, WWII, and the Korean, Vietnam, and Persian Gulf wars were 33%, 21%, 30%, 25%, 24%, and 24%, respectively.38,189,190 It has been shown that 35% to 40% of all combat deaths are due to brain wounds.38 From 2001 to the present, 34,943 American soldiers have been wounded in Iraq and Afghanistan, 3541 of whom died of their war wounds (10%), thus putting mortality from warfare at its lowest level.189 Late mortality ranges anywhere from 8% to 12% and is usually related to craniocerebral missile head wounds.138,191
Contrary to lethality as a consequence of missile head wounds during war, the prognosis for civilian GSWHs remains abysmal.21,41–43 In the report of Siccardi and associates, 85% of 314 victims of civilian GSWHs died within 3 hours (228 at the scene and 38 in 3 hours).31 Carey analyzed mortality in four typical clinical series of GSWHs21,41–43 by stratifying admission GCS scores and long-term GOS scores in 349 patients.94 In his analysis only 2 of 231 patients with a GCS score of 3 to 5, 14 of 44 patients with a GCS score of 6 to 8, and 57 of 74 patients with a GCS score of 9 to 15 made a good recovery (GOS scores of 4 and 5). Mortality rates in the same strata were 93%, 45%, and 10%, respectively. Overall, 21% of patients admitted alive to the emergency department made a good recovery (73 of 349 patients). In 2000 in the state of Maryland, 250 subjects sustained GSWHs (unpublished data), 222 (89%) of whom eventually died (177 at the scene and 45 in the emergency departments of eight trauma centers). Only 10 patients were seen at the trauma resuscitation unit of a shock trauma center alive, 8 of whom underwent surgery and 6 (2.4%) eventually made a favorable recovery.
Extensive studies have evaluated long-term survival and cognitive, behavioral, and functional outcome after PBI, especially in war injuries sustained in WWII and the Korean and Vietnam conflicts.120,121,192–197 For patients who survive a PBI, the size and location of the parenchymal injury may have a long-lasting effect on intelligence test scores. Corkin noticed a long-lasting effect on hidden figures test performance when a missile head wound involved the left hemisphere.198 Grafman and colleagues noted isolated memory problems when the penetrating fragment cut into the fornix.196 Preinjury intelligence determined performance in intelligence tests, although the size and location of the penetrating missile head wound have a decisive effect on postinjury intelligence.175,194,195 The Wisconsin Card Sorting test indicated that victims of left dorsofrontal injuries had the most severe perseverative errors.194 Weinstein and Teuber noticed a long-term decline in intelligence in WWII war veterans,197 which was confirmed by Corkin and colleagues,192 who used the Army General Classification Test to evaluate vocabulary, arithmetic, block counting, and hidden figures between a group of 57 patients with missile head wounds and 27 veterans of WWII with peripheral nerve injuries. The authors reported significant drops in intelligence test scores over time in patients with missile head wounds. They postulated the decline in intelligence to be due to the primary effects of the missile head wound and the added effects of advancing age and stress on the remaining brain tissue caused by functioning for decades in a compromised state. In the studies by Corkin and associates, life expectancy and drop in intelligence were compared between 190 WWII veterans with PBI and 106 veterans with peripheral nerve injuries.193 These investigators found a significant relationship between formal education and life expectancy; however, change between preinjury and postinjury intelligence test scores did not determine survival.
In recent years, neuroscientists have focused specifically on MTBI secondary to blast trauma, PTSD, and their long-lasting effect on the functionality of victims of closed brain injury and PBI and exposure to primary blast overpressure.2,3,5–8,199–201 With the fall in the death rate among war casualties in Operation Enduring Freedom/Operation Iraqi Freedom189,190 and the fact that nearly 20% of all the deployed forces in Iraq and Afghanistan (nearly 320,000) may have suffered TBI, the fundamental question is what are the long-term cognitive, functional, and psychosocial outcomes of patients with MTBI. There is evidence that soldiers returning home from combat duties in Iraq and Afghanistan may suffer from poor general health and be more susceptible to cardiovascular complications, both of which can ultimately affect their job performance and productivity.1–3,5–7,202–204 The major link between MTBI and poor physical performance seems to center on PTSD, which is seen in 5% to 11% of all patients with MTBI.1–35 In the survey of Hoge and colleagues, 124 of 2525 (4.9%) soldiers surveyed 3 to 4 months after their return from a year-long deployment to Iraq suffered from loss of consciousness and 260 (10.3%) from altered mental state, consistent with MTBI.3 Moreover, 43.9% of soldiers with loss of consciousness and 27.3% with altered mental state suffered from PTSD. The incidence of PTSD was 16.2% in 435 soldiers with other injuries and 9.1% in those with no injuries.3 Soldiers with MTBI were significantly more likely to report high combat intensity, a blast mechanism of injury, more than one exposure to an explosion, and hospitalization during deployment. In a logistic regression analysis, only loss of consciousness and combat intensity remained significantly associated with PTSD.3 In another study, Schneiderman and associates surveyed 2235 soldiers with combat experience and found the incidence of MTBI to be 12% and that of PTSD to be 11%.5 Smith and coworkers noted PTSD symptoms in 7.6% to 8.7% of military personnel who reported combat exposure and in 1.4% to 2.1% of those who did not report combat exposure.6 It is possible that MTBI under unusually stressful circumstances, such as blast injuries resulting from the explosive effects of IEDs, may affect the neuronal circuitry designed to monitor stressful conditions, such as the amygdala, lateral hypothalamus, and pituitary/adrenal axis. This effect may result in excessive amounts of stressful hormones and icosanoids and deposition of implicit memory of trauma that will result in PTSD. Other systemic effects include cell-mediated immunity, disordered sleep physiology, and symptoms of altered perception.1,3,10,16 Cernak and colleagues showed statistically significant elevations in blood thromboxane A2, prostacyclin, and sulfidopeptide leukotrienes in 65 patients exposed to blast injury10,16 as opposed to 62 patients who suffered from non–blast-related injuries in the Balkan conflict.16 A multiphasic research project is currently ongoing to investigate pathogenesis and the best ways to manage MTBI and PTSD.4
Aarabi B. Surgical outcome in 435 patients who sustained missile head wounds during the Iran-Iraq war. Neurosurgery. 1990;27:692-695.
Aarabi B. Traumatic aneurysms of brain due to high velocity missile head wounds. Neurosurgery. 1988;22:1056-1063.
Aarabi B, Taghipour M, Alibaii E, et al. Central nervous system infections after military missile head wounds. Neurosurgery. 1998;42:500-509.
Aarabie B, Alden TD, Chesnut RM, et al. Management and prognosis of penetrating brain injury. J Trauma. 2001;51(Suppl):S1-S85.
Aldrich EF, Eisenberg HM, Saydjari C, et al. Predictors of mortality in severely head-injured patients with civilian gunshot sound: a report from the NIH Traumatic Coma Data Bank. Surg Neurol. 1992;38:418-423.
Annegers JF, Hauser WA, Coan SP, et al. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20-24.
Armonda RA, Bell RS, Vo AH, et al. Wartime traumatic cerebral vasospasm: recent review of combat casualties. Neurosurgery. 2006;59:1215-1225.
Brandvold B, Levi L, Feinsod M, et al. Penetrating craniocerebral injuries in the Israeli involvement in the Lebanese conflict, 1982-1985. J Neurosurg. 1990;72:15-21.
Carey ME. Experimental missile wounding of the brain. Neurosurg Clin N Am. 1995;6:629-642.
Carey ME. Learning from traditional combat mortality and morbidity data used in the evaluation of combat medical care. Mil Med. 1987;152:6-13.
Caveness WF, Walker AE, Ashcroft PB. Incidence of post-traumatic epilepsy in Korean veterans as compared with those from World War I and World War II. J Neurosurg. 1962;19:122-129.
Cernak I, Savic J, Ignjatovic D, et al. Blast injury from explosive munitions. J Trauma. 1999;47:96-103.
Corkin S. Hidden-figures-test performance: lasting effects of unilateral penetrating head injury and transient effects of bilateral cingulotomy. Neuropsychologia. 1979;17:585-605.
Corkin S, Sullivan EV, Carr FA. Prognostic factors for life expectancy after penetrating head injury. Arch Neurol. 1984;41:975-977.
du Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: the timing of angiography in patients presenting with the weapon already removed. Neurosurgery. 1992;31:905-911.
Frankowski RF, Lee RK. Epidemiology: incidence and mortality of craniocerebral missile wounds. In: Aarabi B, Kaufman HH, editors. Missile Wounds of the Head and Neck, vol VI. Lebanon, New Hampshire: American Association of Neurological Surgeons; 1999:17-33.
Gawande A. Casualties of war—military care for the wounded from Iraq and Afghanistan. N Engl J Med. 2004;351:2471-2475.
Grafman J, Jonas B, Salazar A. Wisconsin Card Sorting Test performance based on location and size of neuroanatomical lesion in Vietnam veterans with penetrating head injury. Percept Mot Skills. 1990;71:1120-1122.
Grahm TW, Williams FCJr, Harrington T, et al. Civilian gunshot wounds to the head: a prospective study. Neurosurgery. 1990;27:696-700.
Hoge; Hoge CW. Mild Traumatic Brain Injury in Service Members Returning from Iraq and Afghanistan. Paper presented at the 26th Annual National Neurotrauma Symposium, Orlando, FL, July 27-30, 2008.
McCrea M, Kelly JP, Randolph C, et al. Immediate neurocognitive effects of concussion. Neurosurgery. 2002;50:1032-1040.
Okie S. Traumatic brain injury in the war zone. N Engl J Med. 2005;352:2043-2047.
Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. Am J Epidemiol. 2008;167:1446-1452.
Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476-482.
Smith TC, Ryan MA, Wingard DL, et alfor the Millennium Cohort Study Team. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ. 2008;336:366-371.
1 Hoge CW. Mild Traumatic Brain Injury in Service Members Returning from Iraq and Afghanistan. Paper presented at the 26th Annual National Neurotrauma Symposium, Orlando, FL, July 27-30, 2008.
2 Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13-22.
3 Hoge CW, McGurk D, Thomas JL, et al. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358:453-463.
4 Ling GSF. Traumatic Brain Injury and the Global War on Terror. Proceedings of the 26th Annual National Neurotrauma Symposium, Orlando, Fla, July 27-30, 2008.
5 Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. Am J Epidemiol. 2008;167:1446-1452.
6 Smith TC, Ryan MA, Wingard DL, et alfor the Millennium Cohort Study Team. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ. 2008;336:366-371.
7 Hoge CW, Terhakopian A, Castro CA, et al. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164:150-153.
8 McCrea M. Traumatic Brain Injury and Post-Concussion Syndrome. Oxford: Oxford University Press; 2008.
9 Trudeau DL, Anderson J, Hansen LM, et al. Findings of mild traumatic brain injury in combat veterans with PTSD and a history of blast concussion. J Neuropsychiatry. 1998;10:308-313.
10 Cernak I. Preclinical Models of Blast TBI. Proceedings of The 26th Annual National Neurotrauma Symposium, Orlando, Fla, July 27-30, 2008.
11 Ecklund J. Surgical decompression in penetrating TBI. Proceedings of The 26th Annual National Neurotrauma Symposium, Orlando, Fla, July 27-31, 2008.
12 Gondusky JS, Reiter MP. Protecting military convoys in Iraq: an examination of battle injuries sustained by a mechanized battalion during operation Iraqi Freedom II. Mil Med. 2005;170:546-549.
13 Levi L, Feinsod M. Long-term outcome after craniocerebral missile wounds: recent military experience. Aarabi B, Kaufman H. Missile Wounds of the Head and Neck, vol II. Park Ridge, IL: American Association of Neurological Surgeons. 1999:411-421. Neurosurgical Topics
14 Nelson TJ, Wall DB, Stedje-Larsen ET, et al. Predictors of mortality in close proximity blast injuries during Operation Iraqi Freedom. J Am Coll Surg. 2006;202:418-422.
15 Carey ME, Herz M, Corner B, et al. Ballistic helmets and aspects of their design. Neurosurgery. 2000;47:678-688.
16 Cernak I, Savic J Ignjatovic D, et al. Blast injury from explosive munitions. J Trauma. 1999;47:96-103.
17 Okie S. Traumatic brain injury in the war zone. N Engl J Med. 2005;352:2043-2047.
18 Armonda RA, Bell RS, Vo AH, et al. Wartime traumatic cerebral vasospasm: recent review of combat casualties. Neurosurgery. 2006;59:1215-1225.
19 Cohen JE, Gomori JM, Segal R, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008;63:476-485.
20 Rosenfeld JV. Status of decompressive craniectomy for blast overpressure in Iraq. Personal communication, 2007.
21 Aldrich EF, Eisenberg HM, Saydjari C, et al. Predictors of mortality in severely head-injured patients with civilian gunshot sound: a report from the NIH Traumatic Coma Data Bank. Surg Neurol. 1992;38:418-423.
22 Cavaliere R, Cavenago L, Siccardi D, et al. Gunshot wounds of the brain in civilians. Acta Neurochiru (Wien). 1988;94:133-136.
23 Freytag E. Autopsy findings in head injuries from firearms. Arch Pathol. 1963;76:215-225.
24 Helling TS, McNabney WK, Whittaker CK, et al. The role of early surgical intervention in civilian gunshot wounds to the head. J Trauma. 1992;32:398-400.
25 Hernesniemi J. Penetrating craniocerebral gunshot wounds in civilians. Acta Neurochir (Wien). 1979;49:199-205.
26 Kim TW, Lee JK, Moon KS, et al. Penetrating gunshot injuries to the brain. J Trauma. 2007;62:1446-1451.
27 Levy ML, Rezai A, Masri LS, et al. The significance of subarachnoid hemorrhage after penetrating craniocerebral injury: correlations with angiography and outcome in civilian population. Neurosurgery. 1993;32:532-540.
28 Liebenberg WA, Demetriades AK, Hankins M, et al. Penetrating civilian craniocerebral gunshot wounds: a protocol of delayed surgery. Neurosurgery. 2005;57:293-299.
29 Raimondi AJ, Samuelson GH. Craniocerebral gunshot wounds in civilian practice. J Neurosurg. 1970;32:647-653.
30 Shaffrey ME, Polin RS, Phillips CD, et al. Classifications of civilian craniocerebral gunshot wounds: a multivariate analysis predictive of mortality. J Trauma. 1992;9:S279-S285.
31 Siccardi D, Cavaliere R, Pau A, et al. Penetrating craniocerebral missile injuries in civilians: a retrospective analysis of 314 cases. Surg Neurol. 1991;35:455-460.
32 Sosin DM, Sacks JJ, Smith SM. Head injury-associated deaths in the United States from 1979 to 1986. JAMA. 1989;262:2251-2255.
33 Sosin DM, Sniezek JE, Waxweiler RJ. Trends in death associated with traumatic brain injury, 1979 through 1992. Success and failure. JAMA. 1995;273:1778-1780.
34 Stone JL, Lichtor T, Fitzgerald LF, et al. Civilian cases of tangential gunshot wounds to the head. J Trauma. 1996;41:57-60.
35 Stone JL, Lichtor T, Fitzgerald LF. Gunshot wounds to the head in civilian practice. Neurosurgery. 1995;37:1104-1110.
36 Zafonte RD, Wood DL, Harrison-Felix CL, et al. Severe penetrating head injury: a study of outcomes. Arch Phys Med Rehabil. 2001;82:306-310.
37 Frankowski RF, Lee RK. Epidemiology: incidence and mortality of craniocerebral missile wounds. In: Aarabi B, Kaufman H, editors. Missile Wounds of Head and Neck, vol VI. Lebanon, NH: American Association of Neurological Surgeons; 1999:17-33.
38 Carey ME. Learning from traditional combat mortality and morbiditydata used in the evaluation of combat medical care. Mil Med. 1987;152:6-13.
39 Kaufman HH. Civilian gunshot wounds to the head [current perspective]. Neurosurgery. 1993;32:962-964.
40 Kaufman HH, Makela ME, Lee KF, et al. Gunshot wounds to the head: a perspective. Neurosurgery. 1986;18:689-695.
41 Grahm TW, Williams FCJr, Harrington T, et al. Civilian gunshot wounds to the head: a prospective study. Neurosurgery. 1990;27:696-700.
42 Levi L, Linn S, Feinsod M. Penetrating craniocerebral injuries in civilians. Br J Neurosurg. 1991;5:241-247.
43 Nagib MG, Rockswold GL, Sherman RS, et al. Civilian gunshot wounds to the brain; prognosis and management. Neurosurgery. 1986;18:533-537.
44 Belkin M. Wound ballistics. Prog Surg. 1978;16:7-24.
45 Liker MA, Aarabi B, Levy ML. Missile wounds to the head: ballistics and forensics. In: Aarabi B, Kaufman H, editors. Missile Wounds of Head and Neck. Lebanon, NH: American Association of Neurological Surgeons; 1999:35-55.
46 Amato JJ, Rich NM. Temporary cavity effects in blood vessel injury by high velocity missiles. J Cardiovascular Surg. 2008;13:147-155.
47 Black AN, Burns BD, Zucherman S. An experimental study of the wounding mechanism of high velocity missiles. Br Med J. 1941;2:872-874.
48 Callender GR. Wound ballistics: mechanism of production of wounds by small arms bullets and shell fragments. War Med. 1943;3:337-350.
49 DeMuth WEJr. Bullet velocity as applied to military rifle wounding capacity. J Trauma. 1969;9:27-38.
50 Ordog GJ. Wound Ballistics. In: Ordog GJ, editor. Management of Gunshot Wounds. New York: Elsevier; 1988:25-60.
51 Owen-Smith MS. High-velocity and military gunshot wounds. In: Ordog GJ, editor. Management of Gunshot Wounds. New York: Elsevier; 1988:61-77.
52 Wilson LB. Dispersion of bullet energy in relation to wound effect. Mil Surgeon. 1921;49:241-251.
53 Harvey EN, McMillen JH. An experimental study of shock waves resulting from the impact of high velocity missiles on animal tissues. J Exp Med. 1947;85:321-328.
54 Carey ME. Experimental missile wounding of the brain. In: Narayan R, Wilberger J, Povlishock J . Neurotrauma. New York: McGraw-Hill; 1996:1347-1356.
55 Aarabi B. Management of missile head wounds. Neurosurg Q. 2003;13:87-103.
56 Charters AC3rd, Charters AC. Wounding mechanism of very high velocity projectiles. J Trauma. 1976;16:464-470.
57 Carey ME. Experimental missile wounding of the brain. Neurosurg Clin N Am. 1995;6:629-642.
58 Harding D. Weapons, An International Encyclopedia from 5000 B.C. to 2000 A.D. New York: St. Martin’s Press; 1990.
59 Ascroft PB. Treatment of head wounds due to missiles: analysis of 500 cases. Lancet. 1943;2:211-218.
60 Brandvold B, Levi L, Feinsod M, et al. Penetrating craniocerebral injuries in the Israeli involvement in the Lebanese conflict, 1982-1985. J Neurosurg. 1990;72:15-21.
61 Carey ME. The treatment of wartime brain wounds: traditional versus minimal debridement. Surg Neurol. 2003;60:112-119.
62 Gönül E, Erdogan E, Tasar M, et al. Penetrating orbitocranial gunshot injuries. Surg Neurol. 2005;63:24-30.
63 Meirowsky AM. Neurological surgery in warfare. Mil Med. 1962;127:639-646.
64 Vrankovic D, Hecimovic I Splavski B, et al. Management of missile wounds of the cerebral dura mater: experience with 69 cases. Neurochirurgia. 1992;35:150-155.
65 Bell RS, Vo AH, Neal CJ, et al. Military traumatic brain and spinal column injury: a 5 year study of impact blast and other military grade weaponry on the central nervous system. Paper presented at the Annual Meeting of the Conference on Advanced Technology Applications for Combat Casualty Care, Orlando, Florida, August 11-13, 2008.
66 Aarabi B. Surgical outcome in 435 patients who sustained missile head wounds during the Iran-Iraq war. Neurosurgery. 1990;27:692-695.
67 Ascroft PB, Pulvertaft JV. Bacteriology of head wounds. Br J Surg War Surg Suppl. 1947;1:183-186.
68 Carey ME, Young HF, Mathis JL. The neurosurgical treatment of craniocerebral missile wounds in Vietnam. Surg Gynecol Obstet. 1972;135:386-390.
69 Almogy G, Luria T, Richter E, et al. Can external signs of trauma guide management? Lessons learned from suicide bombing attacks in Israel. Arch Surg. 2005;140:390-393.
70 Lakstein D, Blumenfeld A. Israeli army casualties in the second Palestinian uprising. Mil Med. 2005;170:427-430.
71 De Villiers JC, Sevel D. Intracranial complications of transorbital stab wounds. Br J Ophthalmol. 1975;59:52-56.
72 du Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: the timing of angiography in patients presenting with the weapon already removed. Neurosurgery. 1992;31:905-911.
73 Abe T, Nakamura N, Sugishita M, et al. Partial disconnection syndrome following penetrating stab wound of the brain. Eur Neurol. 1986;25:233-239.
74 de Villiers JC, Grant AR. Stab wounds at the craniocervical junction. Neurosurgery. 1985;17:930-936.
75 Exadaktylos AK, Stettbacher A, Bautz PC. The value of protocol-driven CT scanning in stab wounds to the head. Am J Emerg Med. 2002;20:295-297.
76 Haworth CS, de Villiers JC. Stab wounds to the temporal fossa. Neurosurgery. 1988;23:431-435.
77 Herring CJ, Lumsden AB, Tindall SC. Transcranial stab wounds: a report of three cases and suggestions for management. Neurosurgery. 1988;23:658-662.
78 Kennedy UM, Geary UM, Sheehy N. Intracranial stab wound: a case report. Eur J Emerg Med. 2007;14:72-74.
79 Kieck CF, de Villiers JC. Vascular lesions due to transcranial stab wounds. J Neurosurg. 1984;60:42-46.
80 Melville RL, de Villiers JC. Peripheral cerebral arterial aneurysms caused by stabbing. S Afr Med J. 1977;51:471-473.
81 Taylor AG, Peter JC. Patients with retained transcranial knife blades: a high-risk group. J Neurosurg. 1997;87:512-515.
82 Tudor M, Tudor L, Tudor KI, et al. [Unusual open craniocerebral injury caused by sickle’s tip.]. Acta Med Croatica. 2008;62:85-88.
83 van Dellen JR, Lipschitz R. Stab wounds of the skull. Surg Neurol. 1978;10:110-114.
84 Kirkpatrick JB, DiMaio V. Civilian gunshot wounds of the brain. J Neurosurg. 1978;49:185-198.
85 Miner ME, Ewing-Cobbs L, Kopaniky DR, et al. The results of treatment of gunshot wounds to the brain in children. Neurosurgery. 1990;26:20-25.
86 Shoung HM, Sichez JP, Pertuiset B. The early prognosis of craniocerebral gunshot wounds in civilian practice as an aid to the choice of treatment. Acta Neurochir (Wien). 1985;74:27-30.
87 Selden BS, Goodman JM, Cordell W, et al. Outcome of self-inflicted gunshot wounds of the brain. Ann Emerg Med. 1988;17:247-253.
88 Aarabi B, Taghipour M, Alibaii E, et al. Central nervous system infections after military missile head wounds. Neurosurgery. 1998;42:500-509.
89 Aarabi B, Hesdorffer DC, Ahn ES, et al. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006;104:469-479.
90 Marmarou A, Fatouros PP, Barzo P, et al. Contribution of edema and cerebral blood volume to traumatic brain swelling in head-injured patients. J Neurosurg. 2000;93:183-193.
91 Marmarou A. Pathophysiology of traumatic brain edema: current concepts. Acta Neurochir Suppl. 2003;86:7-10.
92 Neal CJ, Lee EY, Gyorgy A, et al. Effect of penetrating brain injury on aquaporin-4 expression using a rat model. J Neurotrauma. 2007;24:1609-1617.
93 Caveness WF, Walker AE, Ashcroft PB. Incidence of post-traumatic epilepsy in Korean veterans as compared with those from World War I and World War II. J Neurosurg. 1962;19:122-129.
94 Carey ME. Bullet wounds to the brain among civilians. In: Winn RH, Youmans JR, editors. Youmans Neurological Surgery. 5th ed. Philadelphia: Saunders; 2004:5223-5242.
95 Clark CW, Muhlbauer MS, Watridge CB, et al. Analysis of 76 civilian craniocerebral gunshot wounds. J Neurosurg. 1986;65:9-14.
96 Hubschmann O, Shapiro K, Baden M, et al. Craniocerebral gunshot injuries in civilian practice—prognostic criteria and surgical management experience with 82 cases. J Trauma. 1979;19:6-12.
97 Lillard PL. Five years experience with penetrating craniocerebral gunshot wounds. Surg Neurol. 1978;9:79-83.
98 Suddaby L, Weir B, Forsyth C. The management of .22 caliber gunshot wounds of the brain: a review of 49 cases. Can J Neurol Sci. 1987;14:268-272.
99 Kramer B. Trauma Registry of R Adams Cowley Shock. Trauma Center. Personal Communication. 2008.
100 Carey ME, Young HF, Mathis JL. The neurosurgical treatment of craniocerebral missile wounds in Vietnam. Surg Gynecol Obstet. 1972;135:386-389.
101 Aarabi B. Management of traumatic aneurysms caused by high-velocity missile head wounds. Neurosurg Clin N Am. 1995;6:775-797.
102 Amirjamshidi A, Rahmat H, Abbassioun K. Traumatic aneurysms and arteriovenous fistulas of intracranial vessels associated with penetrating head injuries occurring during war: principles and pitfalls in diagnosis and management. A survey of 31 cases and review of the literature. J Neurosurg. 1996;84:769-780.
103 Ferry DJJr, Kempe LG. False aneurysm secondary to penetration of the brain through orbitofacial wounds. Report of two cases. J Neurosurg. 1972;36:503-506.
104 Haddad FS, Haddad GF, Taha J. Traumatic intracranial aneurysms caused by missiles: their presentation and management. Neurosurgery. 1991;28:1-7.
105 Jackson FE, Gleave JRW, Janon E. Traumatic aneurysms, cranial and intracranial. US Navy Med. 1974;63:34-40.
106 Jinkins JR, Dadsetan MR, Sener RN, et al. Value of acute-phase angiography in the detection of vascular injuries caused by gunshot wounds to the head. AJR Am J Roentgenol. 1992;159:365-368.
107 Lunn GM. False cerebral aneurysm of the vertebral artery from remote missile injury of the neck. Br J Surg War Surg Suppl. 1947;1:258-260.
108 Sadar ES, Jane JA, Lewis LW, et al. Traumatic aneurysms of the intracranial circulation. Surg Gynecol Obstet. 1973;137:59-67.
109 Murano T, Mohr AM, Lavery RF, et al. Civilian craniocerebral gunshot wounds: an update in predicting outcomes. Am Surg. 2005;71:1009-1014.
110 Aarabi B. Causes of infections in penetrating head wounds in the Iran-Iraq War. Neurosurgery. 1989;26:923-926.
111 Carey ME, Sacco W, Merkler J. An analysis of fatal and non-fatal head wounds incurred during combat in Vietnam by U.S. forces. Acta Chir Scand Suppl. 1982;508:351-356.
112 Carey ME, Sarna GS, Farrell JB. Brain edema following an experimental missile wound to the brain. J Neurotrauma. 1990;7:13-20.
113 Mitchell SW. Injuries of Nerves and Their Consequences. Philadelphia: JB Lippincott; 1872.
114 Stookey B, Scarff J. Injuries of peripheral nerves. In: Neurosurgery and Thoracic Surgery Military Surgical Manuals. National Research Council. Philadelphia: Saunders; 1943:167.
115 Lagrange F. Fractures of the Orbit, and Injuries to the Eye in War. London: University of London Press; 1918.
116 Jefferson G, Schorstein J. Injuries of the trigeminal nerve, its ganglion and its divisions. Br J Surg. 1955;42:561-581.
117 Lathrop FD. Facial nerve surgery in the European theater of operations. Laryngoscope. 1946;56:665-676.
118 Salazar AM, Grafman JH, Vance SC, et al. Consciousness and amnesia after penetrating head injury: neurology and anatomy. Neurology. 1986;36:178-187.
119 Aarabi B. Cranial nerve injuries at the skull base after craniocerebral missile wounds. In: Aarabi B, Kaufman H, editors. Missile Wounds of Head and Neck, vol II. Lebanon, NH: American Association of Neurological Surgeons; 1999:343-351.
120 Mohr JP, Weiss GH, Caveness WF, et al. Language and motor disorders after penetrating head injury in Viet Nam. Neurology. 1980;30:1273-1279.
121 Smutok MA, Vance SC, Salazar AM, et al. Neurologic and anatomic correlates of recovery from hemiparesis following penetrating head injury. Neurology. 1985;35(Suppl 1):83.
122 Cairns H. Neurosurgery in the British Army, 1939-1946. Brit J Surg War Surg Suppl. 1947;1:9-26.
123 Cushing H. A study of a series of wounds involving the brain and it’s enveloping structures. Br J Surg. 1918;5:558-684.
124 Cushing H. From a Surgeon’s Journal, 1915-1918. Boston: Little, Brown; 1936.
125 Gillingham FJ. Neurosurgical experience in Northern Italy. Br J Surg War Surg Suppl. 1943;1:80-87.
126 Haddad FS. Nature and management of penetrating head injury during the Civil War in Lebanon. Can J Surg. 1978;21:233-238.
127 Matson DD. The Treatment of Acute Craniocerebral Injuries Due to Missiles. Springfield, IL: Charles C Thomas; 1948.
128 Salazar AM, Schwab K, Grafman JH. Penetrating injuries in the Vietnam War. Traumatic unconsciousness, epilepsy, and psychosocial outcome. Neurosurg Clin N Am. 1995;6:715-726.
129 Small JM, Turner EA. A surgical experience of 1200 cases of penetrating brain wounds in battle, N.W. Europe, 1944-1945. Brit J Surg War Surg. 1947;Suppl I:62-74.
130 Axelsson H, Yelverton JT. Chest wall velocity as a predictor of nonauditory blast injury in a complex wave environment. J Trauma. 1996;40(Suppl 3):S31-S37.
131 Aarabi B. Traumatic aneurysms of brain due to high velocity missile head wounds. Neurosurgery. 1988;22:1056-1063.
132 Arendall RE, Meirowsky AM. Air sinus wounds: an analysis of 163 consecutive cases incurred in the Korean War, 1950-1952. Neurosurgery. 1983;13:377-380.
133 Meirowsky AM, Caveness WF, Dillon JD, et al. Cerebrospinal fluid fistulas complicating missile wounds of the brain. J Neurosurg. 1981;54:44-48.
134 Aarabi B. Comparative study of bacteriological contamination between primary and secondary exploration of missile head wounds. Neurosurgery. 1987;20:610-616.
135 Amirjamshidi A, Abbassioun K, Rahmat H. Minimal debridement or simple wound closure as the only surgical treatment in war victims with low-velocity penetrating head injuries. Indications and management protocol based upon more than 8 years follow-up of 99 cases from Iran-Iraq conflict. Surg Neurol. 2003;60:105-110.
136 Gönül E, Baysefer A, Kahraman S, et al. Causes of infections and management results in penetrating craniocerebral injuries. Neurosurg Rev. 1997;20:177-181.
137 Campbell EH. Compound, comminuted skull fractures produced by missiles. Ann Surg. 1945;122:375-397.
138 Carey ME, Young HF, Rish BL, et al. Follow-up study of 103 American soldiers who sustained a brain wound in Vietnam. J Neurosurg. 1974;41:542-549.
139 Hagan RE. Early complications following penetrating wounds of the brain. J Neurosurg. 1971;34:132-141.
140 Hammon WM. Retained intracranial bone fragments: analysis of 42 patients. J Neurosurg. 1971;34:143-144.
141 Aarabi B Alden TD, Chesnut RM, et al. Management and prognosis of penetrating brain injury. J Trauma. 2001;51(Suppl):S1-S85.
142 Brain Trauma Foundation. Guidelines for management of severe head injury. J Neurotrauma. 2007;24(Suppl):S-1-S-106.
143 Brain Trauma Foundation. Guidelines for cerebral perfusion pressure. Available at http://www2.braintrauma.org/guidelines/downloads/btf_guidelines_cpp_ul.pdf, 2003.
144 Bullock MR, Chesnut R, Ghajar J, et al. Guidelines for the surgical management of traumatic brain injury. Neurosurgery. 2006;58:S1-S62.
145 Shakiba H, Dinesh S, Anne MK. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev. 2004;3:CD004173.
146 Carey ME, Young HF, Mathis JL. The bacterial contamination of indriven bone fragments associated with craniocerebral missile wounds in Vietnam. Mil Med. 1970;135:1161-1165.
147 Ecker AD. A bacteriologic study of penetrating wounds of the brain, from the surgical point of view. J Neurosurg. 1946;3:1-6.
148 Armonda RA. Wound infections in OIF. Personal communication, 2008.
149 Rish BL, Dillon JD, Meirowsky AM, et al. Cranioplasty: a review of 1030 cases of penetrating head injury. Neurosurgery. 1979;4:381-385.
150 Cairns H, Calvert CA, Daniel P, et al. Complications of head wounds, with especial reference to infection. Br J Surg War Surg Suppl. 1947;1:198-243.
151 Maltby GL. Penetrating craniocerebral injuries: evaluation of the late results in a group of 200 consecutive penetrating cranial war wounds. J Neurosurg. 1946;3:239-249.
152 Martin J, Campbell EH. Early complications following penetrating wounds of the skull. J Neurosurg. 1946;2:58-73.
153 Pitlyk PJ, Tolchin S, Stewart W. The experimental significance of retained intracranial bone fragments. J Neurosurg. 1970;33:19-24.
154 Wannamaker GT, Pulaski EJ. Pyogenic neurosurgical infections in Korean battle casualties. J Neurosurg. 1958;15:512-518.
155 Meirowsky AM. Secondary removal of retained bone fragments in missile wounds of the brain. J Neurosurg. 1982;57:617-621.
156 Taha JM, Saba MI, Brown JA. Missile injuries to the brain treated by simple wound closure: results of a protocol during the Lebanese Conflict. Neurosurgery. 1991;29:380-383.
157 Rish BL, Caveness WF, Dillon JD, et al. Analysis of brain abscess after penetrating craniocerebral injuries in Vietnam. Neurosurgery. 1981;9:535-541.
158 Aarabi B, Taghipour M, Kamgarpour A, et al. Traumatic intracranial aneurysms due to craniocerebral missile wounds. In: Aarabi B, Kaufman H, editors. Missile Wounds of Head and Neck, vol II. Lebanon, NH: American Association of Neurological Surgeons; 1999:293-314.
159 Halbach VV, Higashida RT, Dowd CF, et al. Endovascular treatment of vertebral artery dissections and pseudoaneurysms. J Neurosurg. 1993;79:183-191.
160 Gallina G, Gallo O, Boccuzzi S, et al. Aneurisma post-traumatico intracranico della carotide interna come causa di epistassi: considerazioni su due casi. Acta Otorhinolaryngol Ital. 1990;10:607-613.
161 Herrmann HD, Fischer D, Loew F. Experiences with intraluminal occlusion with the Fogarty catheter in the treatment of carotid-cavernous sinus fistulas and other lesions at the base of the skull. Acta Neurochir (Wien). 1975;32:35-54.
162 Negoro M, Kageyama N, Ishiguchi T. Cerebrovascular occlusion by catheterization and embolization: clinical experience. AJNR Am J Neuroradiol. 1983;4:362-365.
163 Saito R, Yazaki T, Kawase T, et al. [Traumatic intracranial aneurysms after removal of tuberculum sellae meningioma: case report.]. No Shinkei Geka. 1992;20:973-977.
164 Serbinenko FA, Lazarev VA. Primenenie ballona katekera v sluchaiakh travmaticheskikn loznykh anevrizm sonnoi arterii, soprovozhdaiushchikhsia profuznymi nosorymi Krovotecheniiami. Zh Vopr Neirokhir. 1981;6:9-16.
165 Simpson RKJr, Harper RL, Bryan RN. Emergency balloon occlusion for massive epistaxis due to traumatic carotid-cavernous aneurysm. Case report. J Neurosurg. 1988;68:142-144.
166 McGrail KM, Heros RC, Debrun G, et al. Aneurysm of the ICA petrous segment treated by balloon entrapment after EC-IC bypass. Case report. J Neurosurg. 1986;65:249-252.
167 Ding XM. Traumatic aneurysm of the intracavernous part of the internal carotid artery presenting with epistaxis. Case report. Surg Neurol. 1988;30:65-67.
168 Hatashita S, Nitta T, Koga N, et al. [Traumatic aneurysm of the intracavernous carotid artery. A case report.]. Neurol Med Chir. 1983;23:885-890.
169 Hahn YS, McLone DG. Traumatic bilateral ophthalmic artery aneurysms: a case report. Neurosurgery. 1987;21:86-89.
170 Aarabi B, Taghipour M, Haghnegahdar A, et al. Prognostic factors in the occurrence of posttraumatic epilepsy after penetrating head injury suffered during military service. Neurosurg Focus. 2000;8(1):e1.
171 Ratilal B, Costa J, Sampaio C. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst Rev. 2006;1:CD004884.
172 Haynes WG. Penetrating brain wounds: analysis of 342 cases. J Neurosurg. 1945;2:365-378.
173 Whitaker R. Gunshot wounds of the cranium: with special reference to those of the brain. Br J Surg. 1916;3:708-735.
174 Hammon WM. Analysis of 2187 consecutive penetrating wounds of the from Vietnam. J Neurosurg. 1971;34:127-131.
175 Grafman J, Jonas B, Salazar A. Epilepsy following penetrating head injury to the frontal lobes. Effects on cognition. Adv Neurol. 1992;57:369-378.
176 Meirowsky AM. Notes on posttraumatic epilepsy in missile wounds of the brain. Mil Med. 1982;147:632-634.
177 Russell WR, Whitty CWM. Studies in traumatic epilepsy; focal motor and somatic sensory fits: study of 85 cases. J Neurol Neurosurg Psychiatry. 1953;6:73-97.
178 Salazar A, Aarabi B, Levi L, et al. Posttraumatic epilepsy following craniocerebral missile wounds in recent armed conflict. Missile wounds of head and neck. In: Aarabi B, Kaufman H, editors. Missile Wounds of Head and Neck, vol II. Lebanon, NH: American Association of Neurological Surgeons; 1999:281-292.
179 Salazar AM, Jabbari B, Vance SC, et al. Epilepsy after penetrating head injury. I. Clinical correlates: a report of the Vietnam Head Injury Study. Neurology. 1985;35:1406-1414.
180 Taylor A, Jablon S, Kretschmann C. Posttraumatic Symptoms in Head Injured Veterans of the Korean Campaign. Bethesda, MD: National Institute of Neurological Diseases and Stroke; 1971.
181 Caviness VSJr. Epilepsy and craniocerebral injury of warfare. In: Caveness WF, Walker AE, editors. Head Injury: Conference Proceedings. Philadelphia: JB Lippincott; 1966:220-234.
182 Weiss GH, Salazar AM, Vance SC, et al. Predicting posttraumatic epilepsy in penetrating head injury. Arch Neurol. 1986;43:771-773.
183 Annegers JF, Hauser WA, Coan SP, et al. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20-24.
184 Glotzner FL, Haubitz I, Miltner F, et al. [Seizure prevention using carbamazepine following severe brain injuries.]. Neurochirurgia. 1983;26:66-79.
185 Temkin NR. Risk factors for posttraumatic seizures in adults. Epilepsia. 2003;44(Suppl 10):18-20.
186 Young B, Rapp RP, Norton JA, et al. Failure of prophylactically administered phenytoin to prevent late posttraumatic seizures. J Neurosurg. 1983;58:236-241.
187 Temkin NR, Dikmen SS, Anderson GD, et al. Valproate therapy for prevention of posttraumatic seizures: a randomized trial. J Neurosurg. 1999;91:593-600.
188 Temkin NR, Dikmen SS, Wilensky AJ, et al. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990;323:497-502.
189 Gawande A. The Wisdom to Be Better. Proceedings of the 2008 Annual Meeting of the Congress of Neurological Surgeons, Orlando, FL, September 20-25, 2008.
190 Gawande A. Casualties of war—military care for the wounded from Iraq and Afghanistan. N Engl J Med. 2004;351:2471-2475.
191 Rish BL, Dillon JD, Weiss GH. Mortality following penetrating craniocerebral injuries. An analysis of the deaths in the Vietnam Head Injury Registry population. J Neurosurg. 1983;59:775-780.
192 Corkin S, Rosen TJ, Sullivan EV, et al. Penetrating head injury in young adulthood exacerbates cognitive decline in later years. J Neurosci. 1989;9:3876-3883.
193 Corkin S, Sullivan EV, Carr FA. Prognostic factors for life expectancy after penetrating head injury. Arch Neurol. 1984;41:975-977.
194 Grafman J, Jonas B, Salazar A. Wisconsin Card Sorting Test performance based on location and size of neuroanatomical lesion in Vietnam veterans with penetrating head injury. Percept Mot Skills. 1990;71:1120-1122.
195 Grafman J, Jonas BS, Martin A, et al. Intellectual function following penetrating head injury in Vietnam veterans. Brain. 1988;111:169-184.
196 Grafman J, Salazar AM, Weingartner H, et al. Isolated impairment of memory following a penetrating lesion of the fornix cerebri. Arch Neurol. 1985;42:1160-1168.
197 Weinstein S, Teuber HL. Effects of penetrating brain injury on intelligence test scores. Science. 1957;125:1036-1037.
198 Corkin S. Hidden-figures-test performance: lasting effects of unilateral penetrating head injury and transient effects of bilateral cingulotomy. Neuropsychologia. 1979;17:585-605.
199 Kang HK, Natelson BH, Mahan CM, et al. Post-traumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157:141-148.
200 McCrea M, Kelly JP, Randolph C, et al. Immediate neurocognitive effects of concussion. Neurosurgery. 2002;50:1032-1040.
201 Schwab KA, Ivins B, Cramer G, et al. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: initial investigation of the usefulness of a short screening tool for traumatic brain injury. J Head Trauma Rehabil. 2007;22:377-389.
202 Breslau N, Anthony JC. Gender differences in the sensitivity to posttraumatic stress disorder: an epidemiological study of urban young adults. J Abnorm Psychol. 2007;116:607-611.
203 Kang HK, Bullman TA, Taylor JW. Risk of selected cardiovascular diseases and posttraumatic stress disorder among former World War II prisoners of war. Ann Epidemiol. 2005;16:381-386.
204 Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476-482.