Chapter 65 Trauma Surgery
Cervical Spine
Injury to the cervical spine should be suspected in any patient complaining of neck pain after trauma. Initial management of the multiply injured patient will be dictated by established advanced trauma life support (ATLS) protocols, with priority directed to management of airway, breathing, and circulatory compromise. The “chin lift and jaw thrust” method of securing an airway may decrease the space available for the spinal cord (beyond that seen with nasal or oral intubation) and should be avoided in the patient with a known or suspected cervical spine injury. Spinal precautions (to include cervical spine immobilization) should be maintained throughout the early stages of evaluation and resuscitation of the multitrauma patient.1 The most common causes of injury to the neck are motor vehicle accidents (MVAs), diving into shallow water, and sport-related activities. A thorough history of a given accident may further influence clinical suspicion for the presence of a cervical spine injury. Did the patient strike his or her head? Was there evidence of cranial impact to the windshield from inside the vehicle? Was the patient ejected? Was there any indication of weakness or paralysis noted at the accident scene? Was the patient neurologically intact at the scene with later deterioration in neurologic function? Information gathered through such questioning will guide clinical suspicion for neck injury and may provide important prognostic information when neurologic compromise is present. Obtaining information regarding prior history of injury, underlying preexisting cervical spine disease, or systemic conditions (e.g., ankylosing spondylitis) is important as well.
The physical examination of the patient with known or suspected cervical spine injury begins at the patient’s head and progresses distally. It is complete only after a thorough evaluation of the entire musculoskeletal system has been performed.1 Abrasions or lacerations about the scalp, face, or neck provide mechanistic clues, alerting the examining physician to the potential for underlying spine trauma. The dorsal cervical spine should be palpated carefully to evaluate for focal tenderness, stepoff, or hematoma. Range of motion should be prohibited until the radiographic evaluation of the neck has been completed. All voluntary motion of the arms, hands, fingers, legs, feet, and toes should be observed, graded, and recorded, along with any noted sensory or deep tendon reflex compromise. Incomplete spinal cord lesions are described by a constellation of characteristic neurologic findings determined by the anatomic location of an injury. Examples include Brown-Séquard syndrome, central cord syndrome,2 anterior cord syndrome, and posterior cord syndrome (Table 65-1). A rectal examination is essential (particularly in the neurologically injured patient in order to document the degree of sacral sparing, if any) and should be accompanied by bulbocavernosus reflex testing to assess for spinal shock. Spinal shock is the transient loss of all motor, sensory, and reflex function distal to the level of an acute spinal cord injury. The classification of a neurologic deficit as complete or incomplete cannot be determined until spinal shock has resolved.3
TABLE 65-1 Incomplete Spinal Cord Injury Syndromes
| Syndrome | Characteristics |
|---|---|
Central cord syndrome |
The central cord syndrome is the most commonly encountered of all incomplete spinal cord injuries. It is characterized by upper extremity motor weakness with relative sparing of the lower extremities. Expected neurologic recovery is fair to poor. |
Anterior cord syndrome |
Anterior cord syndrome results from damage to the interior two thirds of the spinal cord with sparing of the posterior third. There is loss of motor function and pain and temperature sensation. There is preservation of vibration and position sense. Potential for recovery is variable. |
Posterior cord syndrome |
Posterior cord syndrome is the least common. Injury to the posterior columns results in loss of vibration and position sense. There may be sparing of crude touch. Potential for functional recovery is fair. |
Brown-Séquard syndrome |
Brown-Séquard syndrome is an uncommon injury pattern secondary to injury to half of the spinal cord. This is characterized by ipsilateral motor weakness and loss of proprioception, and contralateral loss of light touch, pain, and temperature sensation. Prognosis for ambulation is excellent in this setting. |
The radiographic evaluation often begins with the ATLS screening series that includes a cross-table lateral view of the cervical spine from the occiput to C7. Care should be taken that the lower part of the cervical spine is completely visualized; superimposition of the shoulders may be overcome with caudally directed manual traction on the patient’s arms. Experience at multiple centers has demonstrated that most missed cervical fractures and subluxations are those present at the lower aspect of the cervical spine.4,5 A swimmer’s view often proves useful for complete visualization of the cervicothoracic junction.6 An open-mouth odontoid view, an anteroposterior view, and a lateral plain radiograph of the entire spine should be obtained if a fracture is found because of the frequent occurrence of noncontiguous spinal injuries. Radiographic findings suggestive of cervical instability are summarized in Table 65-2.
TABLE 65-2 Radiographic Findings Suggestive of Cervical Instability
| Direct Evidence of Instability | Indirect Evidence of Instability |
|---|---|
| Angulation >11° between adjacent segments7 | Increased retropharyngeal soft tissue margin10 |
| AP translation >3.5 mm7 | Avulsion fractures at or near spinal ligament insertions |
| Segmental spinous process widening on lateral view8 | Minimal compression fractures of the anterior vertebral bodies11–14 |
| Facet joint widening3 | Nondisplaced fracture lines through the posterior elements or vertebral body |
| Malalignment of spinous processes on AP view | |
| Rotation of facets on lateral view9 | |
| Lateral tilt of vertebral body on AP view9 |
AP, anteroposterior.
Segmental injuries are common and the presence of injury at one level should prompt a careful search for subtle injuries elsewhere in the spine. CT should be routinely used to provide a more accurate delineation of osseous injuries. Sagittally reconstructed images are helpful in illustrating the sagittal alignment of the spine as well as injuries at the cervicothoracic junction. Such reconstruction is often helpful in demonstrating those fracture lines passing in the plane of the transaxial CT cuts.12 MRI is used further to evaluate the nature and extent of neural and connective soft tissue injury. As such, MRI may be used to identify intracanalicular associated disc herniations, spinal cord contusions, ligamentous disruption, and occult fractures.10,15 Flexion and extension dynamic radiography is frequently used in the awake, neurologically intact patient with isolated neck pain and negative plain radiographs.11 These films are often repeated in patients with persistent neck pain to rule out masked instability secondary to acute muscle spasm.
Soft Tissue Neck Injuries
Isolated soft tissue injury is a common occurrence that has been variably described as whiplash, cervical sprain, cervical strain, acceleration injury, and hyperextension injury.4,16,17 Each of these is nearly always the result of an excessive acceleration force acting violently to extend the neck beyond normal restraints. The overwhelming majority of these injuries occur as the result of MVAs.18,19
Symptoms may include nonfocal neck pain with or without accompanying radicular symptoms, isolated cervical radiculopathy, cervical myelopathy, and various incomplete spinal cord syndromes. Closed head injuries may be associated with these injuries. Intracranial manifestations include chronic headache, concussion, extra-axial/intracranial bleeding, and sympathetic dysfunction. Psychiatric changes, including sleep disturbance, depression, mood changes, or frank personality changes, also may occur.16
The most common radiographic finding is the loss of normal cervical lordosis as seen on a lateral plain radiograph.8 Delayed flexion and extension radiographs are again obtained approximately 1 week after resolution of acute muscle spasm to evaluate for evidence of potential destabilizing soft tissue disruption if an obvious injury is not present.3,11 Bone scan has a limited role in screening for occult fractures in selected patients with atypical chronic pain.8 If the bone scan is positive, a CT may then be performed for further evaluation. Early intervention and treatment are based on the presenting injury subtype, including its pathomechanics and severity, and the overall medical status of the patient. In the setting of a whiplash-type injury, initial use of a soft collar will improve comfort in many patients, although use should be limited to a 2- to 4-week period to minimize dependence, muscle atrophy, and decreased neck range of motion.20 Isometric exercises and gentle, supervised range of motion should be initiated as soon as symptoms permit (or within 2 weeks of injury). The regimen should be performed several times a day and should include neck flexion and extension, rotation, and lateral flexion. Enlisting the assistance of a physical therapist may be beneficial, particularly in the early phases of recovery.
Transient Quadriplegia
A neurapraxia-type injury to the cervical spinal cord resulting in transient quadriplegia is most commonly seen in athletes participating in contact sports. The incidence among collegiate football players is 7.3 per 10,000 athletes. Plain radiographs are negative in this setting. The mechanism of injury is most often axial compression combined with hyperflexion or hyperextension. Sensory and motor neurologic deficits are bilateral and usually persist from several minutes to 48 hours after trauma. There is an association with developmental cervical stenosis, although effective guidelines for identification of predisposed athletes have been difficult to establish. Efforts to establish sensitive and specific screening methods to reliably identify at-risk athletes are under way.17,21
Injuries to the Occipitocervical Articulation
Injuries to the occipitocervical junction are being recognized with increasing frequency while patient mortality rates are declining. Improved outcomes are likely a direct benefit of present trauma protocols that begin at the scene of an injury, supporting those who would not have previously survived. Heightened suspicion and early detection (with current imaging techniques) have further contributed to the aforementioned trends.
The occipital condyles are paired, semilunar-shaped projections from the inferior aspect of the occiput that articulate with the atlantal lateral masses. This articulation bears little intrinsic osseous stability, depending instead on the external and internal craniocervical ligaments for constraint. The internal craniocervical ligaments (tectorial membrane, cruciate ligament, and paired alar and apical ligaments) confer most of the intrinsic occipitoatlantal stability.22 Injury to the craniocervical junction commonly occurs through three primary forces: distraction, compression, and rotation.23 Injuries may be mild and stable or life threatening (with complete osteoligamentous disruption).24
Occipital Condyle Fractures
Occipital condyle fractures are most often identified incidentally on head CT in the unconscious patient, although awake patients with complaints of deep suboccipital pain or occipital headache should be suspected of having sustained an injury to the occipitocervical junction.25,26 The incidence is not high, with one trauma center estimating an incidence of 1.7/1000 per year.27 The neurologic examination in survivors is often negative, although mild cord injury and lower cranial nerve injury have been reported. Classification of occipital condyle fractures is based on CT morphology25,28 (Fig. 65-1). A type I fracture is a comminuted fracture of the condyle resulting from impaction of the condyle by the lateral mass of C1. The mechanism is often a direct blow to the head. A type II injury is characterized by the presence of a related basilar skull fracture. Type III injuries are avulsion fractures occurring at the attachment site of the alar ligaments. They may be bilateral in up to 50% of cases and, in this circumstance, are associated with an atlanto-occipital dislocation. Treatment of stable type I and II injuries is cervical immobilization in a hard collar, cervicothoracic brace, or halo vest for 8 to 10 weeks. Type II fractures demonstrating separation of the occipital condyle from the occiput may have inadequate lateral column support, thus requiring 8 to 12 weeks of halo-vest immobilization. Instability is commonly noted in type III injuries and is demonstrated by occipitoatlantal anteroposterior displacement, longitudinal diastasis, or joint incongruity. Injuries identified as unstable are best managed with a dorsal occipitocervical arthrodesis.23,29–32 Recently, Maserati et al. performed a retrospective review of 24,745 consecutive trauma patients over a 6-year period and identified 100 patients with 106 occipital cervical fractures (0.4% incidence). They concluded that immobilization in a rigid cervical collar with delayed radiographic follow-up was adequate as long as there was no evidence of occipitocervical misalignment, which would necessitate the need for occipitocervical fusion or halo fixation.33
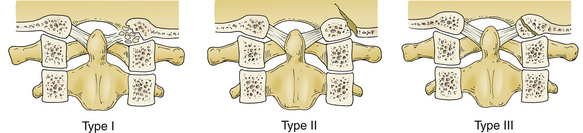
FIGURE 65-1 Occipital condyle fracture classification. A type I fracture is a comminuted fracture of the condyle resulting from impaction of the condyle by the lateral mass of C1. The mechanism is often a direct blow to the head. A type II injury is characterized by the presence of a related basilar skull fracture. A type III injury is an avulsion-type fracture occurring at the attachment site of the alar ligaments.
Occipitocervical Dislocation/Dissociation
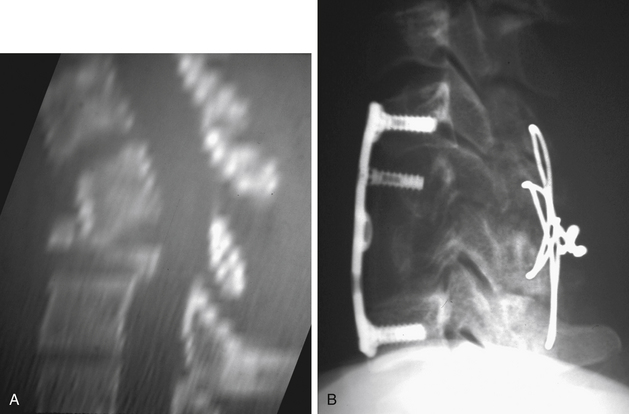
Until recently, few cases of patients surviving this entity had been reported.29–31,34–36 Most reports of survival from occipitocervical dislocation/dissociation have been in children.37 Occipitocervical dislocation or dissociation often results from high-energy trauma, is highly unstable, and is frequently fatal (Fig. 65-2). High-resolution CT (with or without MRI) is often required to evaluate these injuries because they may be difficult to appreciate on plain radiographs unless significant displacement is present (Fig. 65-3A). MRI is often required to evaluate these injuries. Occipitocervical instability (subluxation and dislocation) is classified according to the direction of displacement of the occiput.25,33,38 Type I injuries are ventral subluxations of the occipital condyle relative to the atlantal lateral masses. These represent the most commonly observed injury pattern. Type II injuries are vertical displacements of the occipital condyles greater than 2 mm beyond normal. C1-2 distraction injuries are included in this category. Type III injuries are dorsal occipital dislocations and are exceedingly rare. In evaluating these injuries, more than 2 mm of subluxation at the atlanto-occipital articulation indicates a functional loss of integrity of the major occipitocervical stabilizers such as the alar ligaments and the tectorial membrane.28,39 The treatment of occipitocervical instability is through closed or open reduction and surgical stabilization.40 Traction is to be avoided in these injuries (Figs. 65-3B and C). There has been a recent trend toward performing occiput-to-C1 fusion (C0-1 fusion) using transarticular screw fixation, instead of occipitocervical fusion, in order to maintain mobility across the C1-2 junction.35,37

FIGURE 65-2 Lateral plain radiograph revealing longitudinal diastasis of the occipital-C1 articulation.
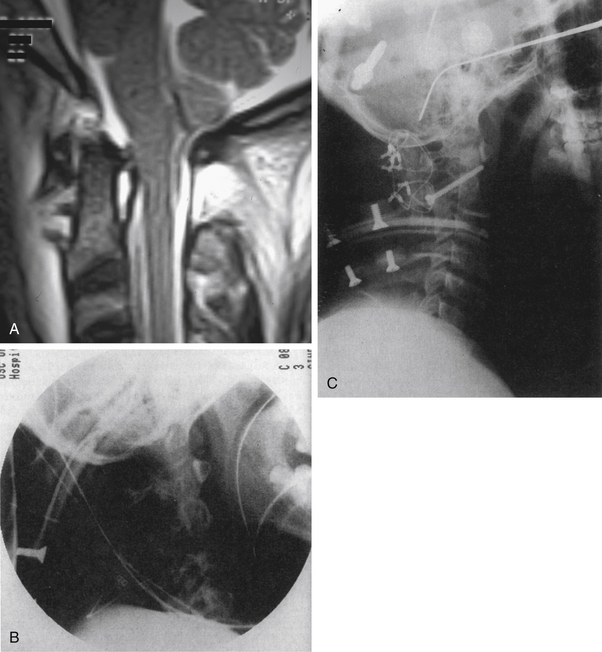
FIGURE 65-3 A, Sagittal MRI revealing longitudinal diastasis of the occipital-C1 and C1-2 articulations. B, Lateral plain film of type IIB occipitoatlantoaxial dislocation. Note that in addition to the longitudinal distraction of the occiput relative to the atlas, a distractive injury also exists at the atlantoaxial segment. C, Postoperative lateral plain film demonstrates the screw-cable-rib construct used to stabilize this occipitoatlantoaxial instability. Posterior C1-2 transarticular screw fixation was used to provide rigid fixation across the atlantoaxial level, thereby blocking rotational movement at this level. Multiple titanium cables were also placed to achieve occiput-to-C2 fixation. Rib was used because it conforms to the occipitoatlantoaxial contour.
(B and C, From Stillerman CB, Ranjan SR, Weiss MH: Cervical spine injuries: diagnosis and management. In Wilkins RH, Rengachary SS, editors: Neurosurgery, vol II, ed 2, New York, 1995, McGraw-Hill, p 2883.)
Injuries to the First Cervical Vertebra
Traumatic Transverse Atlantal Ligament Avulsion
Insufficiency or avulsion of the transverse atlantal ligament (TALA) may occur after a violent flexion force to the upper cervical spine. Associated head injuries are common, and although survival after acute traumatic rupture had previously been thought unusual, it is now being reported with increasing frequency.41,42 Findings range from normal to transient quadriparesis. Permanent quadriparesis is rare given the fatal sequelae that typically follow complete injury at this leve1.42–44 Associated clinical signs include cardiac and respiratory changes secondary to brainstem compromise, or dizziness, syncope, and/or blurred vision as a result of vertebral artery disruption. Symptoms may be exacerbated by neck flexion. A lateral plain radiograph often demonstrates abnormal translation (>5 mm) at the atlantodens interval.45,46 Conservative treatment strategies have generally failed to provide satisfactory results, and the treatment of choice in most patients is a C1-2 arthrodesis. Acute disruption of the transverse ligament may also be noted in association with a Jefferson-type burst fracture of C1.47–51 Treatment in this circumstance should consist of cervical immobilization for 10 to 12 weeks, awaiting union of the C1 arch. Persistent instability after completion of cervical immobilization may then be addressed with a C1-2 fusion.48,52 An atlas nonunion has been reported to result in basilar invagination with significant splaying of the C1 lateral masses.53
Traumatic Rotatory Subluxation
Acute trauma is an unusual cause of acute C1-2 rotatory subluxation. The clinical presentation of C1-2 rotatory subluxation is the complaint of neck pain with findings of torticollis, and it is more commonly seen in children than adults. Four types of fixed C1-2 rotatory injuries have been described54 (Figs. 65-4 and 65-5). Type I injuries involve fixed rotational changes without associated subluxation. In the type II pattern there is 3 to 5 mm of displacement of C1 on C2 (with one lateral mass acting as a pivot while the other rotates ventrally). Type III injuries have more than 5 mm of forward displacement of both lateral masses. Type II and III injuries are both associated with transverse ligament incompetence, and neurologic involvement is common. Associated C2 fractures (type II and III odontoid fractures) have been reported with severe rotatory atlantoaxial subluxation.55,56 Conservative treatment consists of halo or Gardner-Wells traction-reduction, followed by external immobilization for 2 to 3 months. Delayed instability is managed with a dorsal stabilization procedure. Severe rotations with associated cervical fractures (i.e., C2) need to be fixed with intraoperative fusion.55 Fixed or irreducible deformities as well as delayed presentation of this condition are again best managed with surgical stabilization.
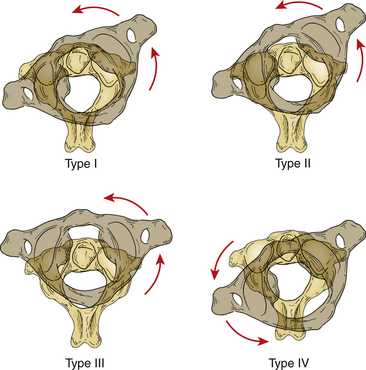
FIGURE 65-4 Classification of rotatory subluxation. Type I, simple rotatory displacement without anterior shift. The odontoid acts as a pivot point. Type II, rotatory displacement with anterior displacement of 3 to 5 mm. The lateral articular process is the pivot point. Type III, rotatory displacement with anterior displacement of more than 5 mm. Type IV, rotatory displacement with posterior translation.
(From Fielding JW, Hawkins RJ Jr: Atlanto-axial rotatory fixation [fixed rotatory subluxation of the atlanto-axial joint]. J Bone Joint Surg [Am] 59:37–44, 1977.)
Fractures of the First Cervical Vertebra
Fractures of C1 occur either as an isolated injury or often in combination with a fracture to the C2 vertebra. The most common associated cervical spine injuries are a type II odontoid fracture and spondylolisthetic fracture of C2.48,57,58 Fractures of C1, seen in up to 10% of all spine injuries, are encountered with relative frequency.59,60 Neurologic injury is unusual.46
Fractures of C1 are classified generally into three categories. This classification scheme has proven useful in determining treatment options, expected clinical course, and prognosis61 (Fig. 65-6). Type I fractures are limited to involvement of the dorsal arch, are often bilateral, and typically occur at the junction of the lateral masses and dorsal arch. This is the most common pattern of C1 fracture and likely occurs secondary to hyperextension in conjunction with an axial load. A type II atlas fracture is a unilateral lateral mass injury that occurs as the result of an asymmetrically applied axial load. Intra-articular extension is not common but is reported.46,62 A type III (or Jefferson) fracture is a burst-type fracture that involves three or more fractures through the ventral and dorsal aspects of the C1 ring. The mechanism of this second-most-common pattern is that of a pure axially applied load.63,64
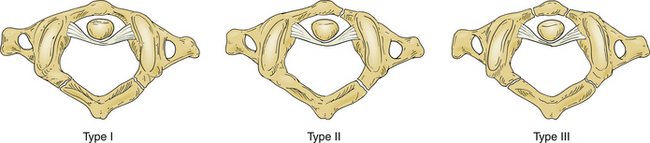
FIGURE 65-6 Classification of fractures of C1. Type I fractures are limited to involvement of the posterior arch, are often bilateral, and typically occur at the junction of the lateral masses and posterior arch. A type II atlas fracture is usually a unilateral injury defined by involvement of the lateral mass (with fracture lines passing both anteriorly and posteriorly) as the result of an asymmetrically applied axial load. A type III (or Jefferson) fracture is a burst-type fracture that involves three or more fractures through the anterior and posterior aspect of the C1 ring.
Plain radiographs are useful in the evaluation of these injuries and often demonstrate widening of the retropharyngeal soft tissue shadow from C1 to C3 (although these changes may take 6 or more hours to develop).65,66 The open-mouth odontoid view shows lateral displacement of the lateral masses in a Jefferson-type fracture and may appear normal with the more common type I dorsal arch fracture. If total combined lateral displacement of the C1 lateral masses over C2 is greater than 6.9 mm,65,67 the transverse ligament has been disrupted, resulting in an unstable injury.48,59,68 Type II fractures appear radiographically as unilateral displacement of the affected lateral mass on an open-mouth odontoid radiograph. Improvements in technique and image quality have made CT in the plane of the C1 ring helpful in fully defining these injuries. The most important factor governing treatment and outcome is the simultaneous occurrence of other injuries.48,57,69 Treatment of isolated C1 fractures has traditionally been nonoperative, although some European centers have reported the successful surgical reduction and stabilization of markedly displaced Jefferson burst fractures. Results with nonoperative treatment have been good,49 although mild neck pain is a chronic sequela in up to 80% of these patients.59 There has been no reported correlation between fracture union/nonunion and functional outcome.51
Fractures of the Second Cervical Vertebra
Fractures of the Odontoid Process
Fractures of the odontoid process of the axis are relatively common among injuries of the upper cervical spine, although the exact prevalence is not well established. Odontoid fractures in young adults are most often secondary to high-energy trauma, such as MVAs or violent blows to the head.70–73 Those sustained by the elderly or very young are more commonly due to lower-energy falls.74–76 As with other upper cervical injuries, clinical suspicion is critical to early recognition because several studies have reported a high incidence of missed injuries, especially in patients with depressed mental status. The degree of neurologic involvement is widely variable; however, the majority of patients have a negative neurologic examination. Odontoid fractures are best visualized on lateral and open-mouth anteroposterior plain radiographs, as well as on reformatted sagittal CT images (because routine axial imaging may miss the fracture).77
The most widely adopted classification system is that proposed by Anderson and D’Alonzo70 based on their experience with 60 patients with odontoid fractures treated over an 8-year period. This classification identifies three fracture types based on the anatomic location of the fracture line68,70 (Fig. 65-7). Type I fractures are the least common and are described as an oblique fracture involving the superior tip of the dens. Type II odontoid fractures occur at the junction of the base of the dens and the body of the axis. This is the most common of the three types and the most controversial regarding discussing treatment.70 Type II fractures have the highest rate of nonunion when treated nonoperatively, especially in the elderly.68 In type III fractures, the fracture line occurs in the body of the axis (primarily involving cancellous bone) and exits through the C2 superior articular facet.
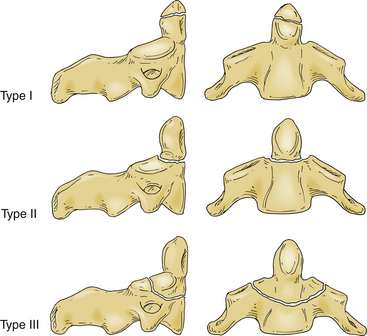
FIGURE 65-7 Classification of odontoid fractures. Type I fractures are the least common and are described as an oblique fracture involving the superior tip of the dens. Type II odontoid fractures, the most common type, occur at the junction of the base of the dens and the body of the axis. Type III odontoid fractures are characterized by the fracture line passing through the cancellous bone of the vertebral body.
Isolated type I odontoid fractures are considered stable (unless they are associated with instability involving the occipitocervical junction) and may be treated with a Philadelphia collar or similar orthosis. Type III fractures are often successfully managed with collar or halo immobilization. Type II fractures, however, lack both periosteum and cancellous bone at the fracture site, increasing the propensity for nonunion.72,78 Fractures that are significantly displaced may be realigned with traction-reduction and immobilized with a halo vest until definitive treatment measures are selected. Factors considered to be associated with nonhealing of type II fractures include the degree of displacement, angulation, age of patient, loss of fracture reduction, and medical comorbidities. Surgical stabilization, when chosen, may proceed through a ventral or dorsal approach, depending on patient variables and fracture subtype.69,71,79–81
Traumatic Spondylolisthesis of the Axis
Traumatic spondylolisthesis of the axis is a pars interarticularis fracture of the second vertebra with disruption of the C2-3 junction; it has been of interest for decades given its unique distinction as the “hangman’s fracture.”82–88 The lesion encountered today, frequently a result of an MVA, is similar in terms of location to the originally described hangman’s fracture, but from a mechanistic standpoint bears little resemblance to the fracture subtype characteristic of judicial hanging.78,88–90 The majority of these injuries are the result of MVA trauma and are infrequently associated with injury to the spinal cord (5.5%). The basic mechanism of injury is hyperextension with vertical compression of the posterior column with translation of C2 and C3.83,87 Each of the three primary fracture types (types I to III; Fig. 65-8) are characterized further by variations of this mechanism. Dynamic radiography may be required to differentiate injury types.
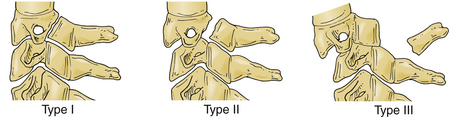
FIGURE 65-8 Classification of traumatic spondylolisthesis of the axis. Type I fractures occur through the neural arch in the region just posterior to the vertebral body. There is less than 3 mm of translation and no angulation at the fracture site. Type II fractures have greater than 3 mm of displacement and significant angulation. Type III fractures describe a type I (pars) fracture with an associated bilateral facet dislocation at C2-3. The critical feature is the classic presence of a free-floating posterior arch of C2.
Traumatic spondylolisthesis of the axis can be divided into three types of fractures. Type I fractures occur through the neural arch in the region just dorsal to the vertebral body. There is less than 3 mm of translation and no angulation at the fracture site. This fracture subtype is the result of hyperextension and an axial load. These may be treated with immobilization in a cervical orthosis for 3 months.75
Type II fractures are divided further into type II and type IIA injuries. Type II fractures have greater than 3 mm of displacement and significant angulation. The mechanism of injury is a combined force comprising hyperextension and axial loading (extension immediately followed by flexion). Fracture reduction may be achieved with skeletal traction in extension with immediate or delayed conversion to halo-vest immobilization. Vaccaro et al. have recently reported excellent results with early halo immobilization and reduction for type II or IIA hangman’s fractures. Decreased fusion rates were found for type II fractures with an angulation of 12 degrees or more, requiring an extended period of traction to ensure proper alignment before long-term fixation with halo immobilization.91 Surgical stabilization is infrequently necessary, although several surgical options exist for patients in whom a reduction cannot be maintained or those unable to tolerate prolonged halo traction or halo-vest immobilization. In reducible fractures, a primary screw fixation of the pars articularis has been performed with good realignment and fusion.92 In fractures that are not anatomically reducible, or in cases of displaced nonunion, a ventral C2-3 arthrodesis is a viable treatment option (Fig. 65-9). Recently, Chittiboina et al. performed a cadaveric biomechanical analysis of ventral C2-3 fusion versus dorsal fixation with C1 lateral mass screws and C2-3 dorsal fixation. The authors concluded that both methods resulted in a consistent increase in stability.83

FIGURE 65-9 Lateral plain radiograph after an anterior C2-3 fusion for late instability in a type II hangman’s fracture.
Type IIA fractures are distinguished by an oblique fracture line often running from dorsal-rostral to ventral-caudal along the length of the pars. The mechanism is a flexion-distraction force. This fracture subtype is seen in less than 10% of hangman’s fractures. Reduction is by extension and slight axial loading; axial traction will accentuate the deformity. Reduction should be followed by immobilization in a halo vest for 3 months.
Type III fractures describe a type I (pars) fracture with an associated unilateral or bilateral facet dislocation at C2-3. The critical feature is the classic presence of a free-floating dorsal arch of C2. These are unstable and irreducible by closed means, requiring surgical intervention.93
An additional group of injuries may also be described as traumatic spondylolisthesis of C2-3 with either bilateral laminar fractures (type IV) or bilateral facet fractures of the inferior articular processes of C2 (type V). The mechanism of both types is flexion or shear, producing a highly unstable pattern.82,85
Injuries to the Lower Cervical Spine
The C3 through C7 vertebrae are similar in anatomy and biomechanics, and generally incur similar fracture patterns. However, the C7 vertebra is exposed to greater axial compression and flexion load because of its location at the junction of the cervical and thoracic spine. Closed indirect injuries to the head and neck therefore often produce patterns of injury that are characteristic to the lower cervical vertebral column. The most severe neurologic sequelae arise as a result of a translational deformity, establishing ligamentous integrity as critically important to stability and treatment.
Both two- and three-column models are used in discussing the traumatic pathoanatomy of the lower cervical spine. The three-column model was originally described in 1984 with specific reference to thoracolumbar injuries94 but has since been modified to address cervical spine stability. It may be of greater utility to discuss the cervical spine as a two-column entity composed of an anterior and posterior column.7,95–97 In the two-column model, the ventral spine consists of the posterior longitudinal ligament and all remaining ventral structures, whereas the posterior column consists of all structures dorsal to the posterior longitudinal ligament (Box 65-1). The anterior and posterior columns are then reciprocally affected by flexion and extension moments.
A mechanistic classification of subaxial cervical spine injuries was described by Allen et a1.95 in 1982. This classification divides middle and lower cervical fractures into six groups based on force vector (initial dominant force) and subsequent incremental tissue failure (based on the attitude of the spine at failure). Abnormal relationships between adjacent vertebrae imply ligamentous failure, suggesting a shear force mechanism (because ligaments do not fail in compression). The three most common injury groups are compressive flexion, compressive extension, and distractive flexion. Vertical compression injuries occur with intermediate frequency, whereas distractive extension and lateral flexion injuries occur the least.98 The presence of neurologic injury has not been strongly associated with any individual group in the classification, although it is related to progressive osteoligamentous disruption or the severity of injury in a particular subgrouping. Injuries as identified on plain radiographs should undergo further evaluation with CT scanning and possibly MRI. Assessment of plain radiographic, CT, and MRI findings assists in the evaluation of spinal stability.
Traumatic Central Cord Syndrome
Traumatic central cord syndrome is the most common incomplete spinal cord injury. It is characterized by a disproportionately greater motor deficit in the upper extremities compared with the lower extremities. It is usually attributed to a hyperextension injury in the presence of osteophytic spurs. Varying degrees of sensory findings may be present. Myelopathic findings may be present. The upper extremities are more involved because the cervical long tract motor fibers for the upper extremities are located more medially than those for the lower extremities. The diagnosis of central cord syndrome is confirmed with an MRI scan, which demonstrates cervical stenosis with degenerative osteophytic spurs. Recovery is usually gradual, with recovery of motor function over a period of 6 to 8 weeks. Timing of surgery is still controversial. The old rule that surgery should be delayed while the patient regains neurologic function has been recently challenged. Subsequently, there has been a movement toward earlier surgery to decompress the spinal cord and prevent further compression due to delayed swelling. The consensus at this time is that early surgery is not harmful.99 Recently, Chen et al. analyzed 49 patients with traumatic central cord syndrome.98 They found that there was no correlation in improvement in neurologic recovery if the patients had surgery within 4 days or more than 4 days after their spinal cord injury. There was also no significant correlation in improvement based on the location of the injury or surgical approach used. There was a trend toward better recovery in patients younger than 65 years of age compared with patients older than 65 years.98 Similar data were reported by Aito et al., who found that subjects younger than 65 years of age had significantly better neurologic and functional recovery than patients older than 65 years.99
Spinal Cord Injury without Radiographic Abnormality in Adults
Although spinal cord injury without radiographic abnormality (SCIWORA) is typically attributed to pediatric spinal cord injuries (1.5–16 years of age) in which there is a neurologic deficit but no radiographic abnormality, SCIWORA has also been reported in adults. This section addresses SCIWORA in adults only. The incidence of adult SCIWORA is under-reported. Kasimatis et al. recently reported on 166 patients with cervical spine injury treated at a single institution. Seven of these 166 adult patients (4.2%) presented with frank neurologic symptoms but with no acute signs of trauma. On MRI, these patients were found to have intramedullary changes (five of six patients) with varying degrees of compression from a disc or the ligamentum flavum.100 The mechanism of adult SCIWORA has been explored by Imajo et al.101 Whereas pediatric SCIWORA has been hypothesized to be secondary to the increased elasticity of the spinous ligaments and paravertebral soft tissue, resulting in a “whiplash” type of effect on the normal cord after impact, adult SCIWORA has been hypothesized to be secondary to degenerative changes and translations.102 In adult SCIWORA, Imajo et al. performed three-dimensional finite element analysis to analyze biomechanical responses under compression and extension moments. They created facet surfaces from C3 to C5 under varying degrees of angulation, and found that 60 degrees of angulation at C3-4 resulted in the greatest flexibility in extension and the highest total translation. This increased translation, combined with facet and ligamentum flavum hypertrophy in the adult cervical spine, led to increased risk of SCIWORA in the adult patient.101 Shen et al. reported that diffusion-weighted MRI can detect signal changes that are not depicted on typical T1- or T2-weighted images in patients with thoracic SCIWORA.103 Tewari et al. have prognosticated recovery for adult patients with SCIWORA on the basis of MRI signal changes, with patients with minimal cord changes on MRI having the best outcome, followed by those with cord edema alone. Patients with parenchymatous hemorrhage and contusions on MRI had the worst prognosis, often with no significant improvement in their Frankel grade.104
Compressive Flexion
Compressive flexion injuries are caused by a ventral and axially directed load of increasing intensity. Compressive fractures without facet fracture or subluxation are usually stable injuries. Higher stages of injury involve increased ventral osseous and dorsal ligamentous injury and may be unstable (Figs. 65-10 and 65-11). Treatment is tailored accordingly, although a frequent complication with conservative management is late instability.13 Surgical intervention often involves a cervical corpectomy and instrumented fusion with a structural graft. Adjunctive dorsal stabilization may be necessary in highly unstable, advanced-stage lesions.105
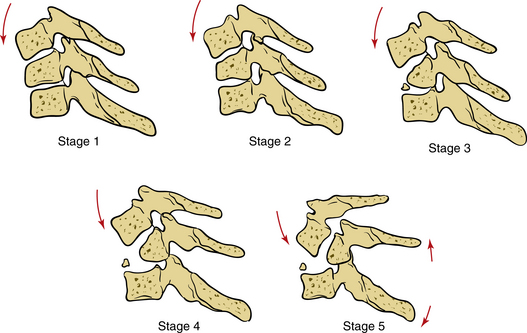
FIGURE 65-10 Compressive flexion injury. Stage 1: blunting and rounding-off of anterosuperior vertebral margin. Stage 2: loss of anterior vertebral height with anteroinferior beaking. Stage 3: fracture line extending from anterior surface of vertebral body extending obliquely through the subchondral plate (fractured beak). Stage 4: less than 3 mm of the posteroinferior vertebral margin into the neural canal. Stage 5: greater than 3 mm of displacement of the posterior aspect of the vertebral body with complete disruption of the posterior ligamentous complex. The vertebral arch is intact.
(From Rizzolo SJ, Cotler JM: Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1:57–66, 1993.)
Compressive Extension
Compressive extension injuries result in a spectrum of pathologic processes, ranging from unilateral vertebral arch fractures to bilateral laminar fractures, and finally to vertebral arch fractures with full ventral displacement of the vertebral body (Fig. 65-12). Management is based on injury severity and instability. An initial dorsal reduction and stabilization procedure is often required, followed by adjunctive ventral stabilization if necessary.106
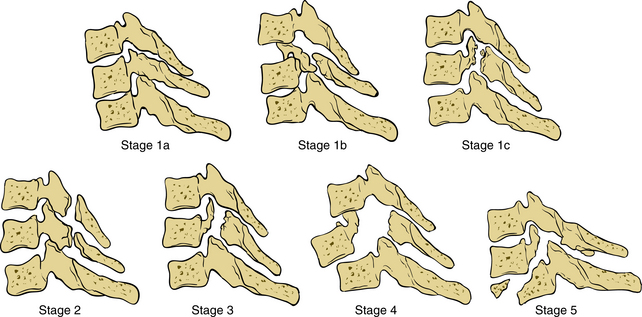
FIGURE 65-12 Compressive extension injury. Stage 1: unilateral vertebral arch fracture through the articular process (stage 1a), the pedicle (stage 1b), or lamina (stage 1c), either with or without a rotary spondylolisthesis of the centrum. Stage 2: bilaminar fracture at one or more levels. Stage 3: bilateral fractures of the vertebral arch with partial-width anterior vertebral body displacement. Stage 4: partial-width anterior vertebral body displacement. Stage 5: complete anterior vertebral body displacement.
(From Rizzolo SJ, Cotler JM: Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1:57–66, 1993.)
Distractive Flexion
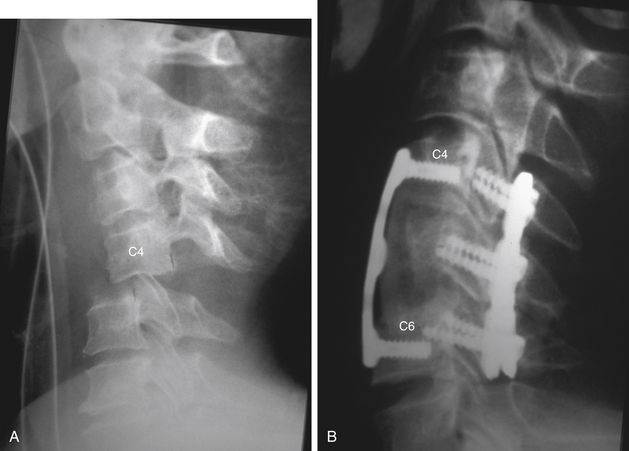
Distractive flexion injuries are also known as the flexion-dislocation injuries. There is typically little osseous injury except for minor compression failure of the caudal vertebral segment. However, there is severe ligamentous damage involving the dorsal facet capsule complex, ligamentum flavum, and interspinous ligaments, and (depending on the presence of a unilateral or bilateral dislocation) injury to the posterior longitudinal ligament and intervertebral disc14 (Figs. 65-13 and 65-14). A significant number of patients with this injury also have an associated closed head injury.106 Radiographic changes may be minimal in the early stages (flexion sprain) of this injury subtype. MRI is often useful to delineate the full extent of soft tissue disruption (including injury to the disc), although obtaining this study in an awake, alert, and cooperative patient should not delay traction reduction when plain radiographs demonstrate a translational displacement. Some physicians recommend obtaining an MRI before closed or open reduction of this injury subtype.107 All injuries in this family should be considered at risk for further displacement, making surgical stabilization the primary mode of treatment.9,108 After a successful closed reduction, MRI should be obtained to evaluate for the presence of a herniated disc (Fig. 65-15); if present, a ventral decompression and stabilization is the preferred surgical approach. If a closed reduction is not feasible, the surgical approach is predicated on the presence of an extruded disc fragment. If a disc fragment is present, a ventral decompression is required with or without an attempted ventral open reduction followed by a stabilization procedure. Recently, Johnson et al. analyzed the results of 87 patients with either unilateral or bilateral facet dislocations or fracture-dislocations treated with a single-level anterior cervical discectomy and fusion. They, like others, found a 13% incidence of nonunion, and concluded that facet fractures or end-plate fractures were predisposing factors for long-term nonunion.109,110 Paxinos et al. performed biomechanical studies and concluded that an anterior cervical discectomy and fusion with a locked plate was sufficient to stabilize a flexion-distraction stage 3 injury in the lower cervical spine, provided that osteoporosis was not present.105 In the absence of an extruded disc fragment, a dorsal open reduction and stabilization procedure may be performed.
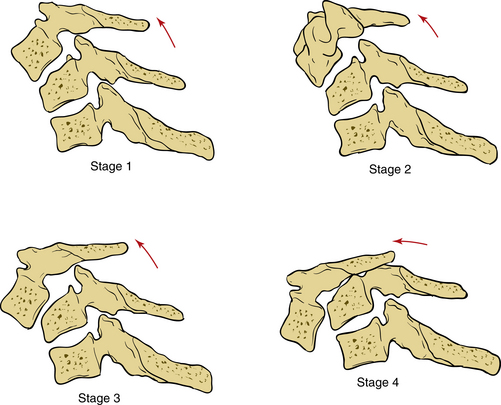
FIGURE 65-13 Distractive flexion injury. Stage 1: flexion sprain injury with facet subluxation in flexion and divergence of spinous processes. There may be some blunting of the anterosuperior vertebral margin (similar to stage 1 compressive flexion injury). Stage 2: unilateral facet dislocation with or without rotary spondylolisthesis. Stage 3: bilateral facet dislocation with up to 50% vertebral body displacement. Stage 4: completely unstable motion segment with full-width vertebral body displacement.
(From Rizzolo SJ, Cotler JM: Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1:57–66, 1993.)
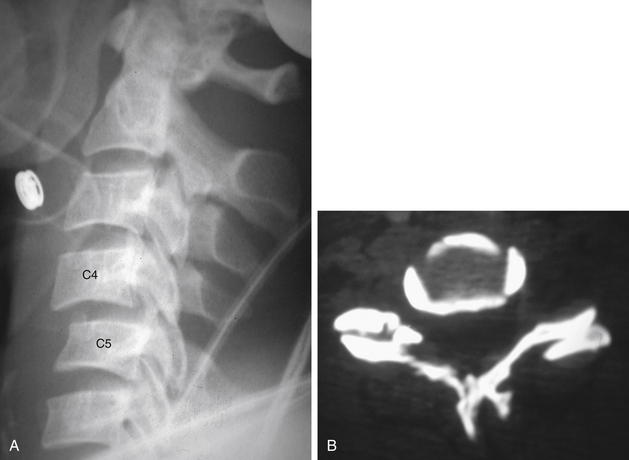
FIGURE 65-14 A, Lateral plain radiograph revealing evidence of a C4-5 unilateral facet dislocation (type II distractive flexion injury). Note the 25% anterior subluxation of C4 on C5. B, Transaxial CT scan revealing a left-sided unilateral facet dislocation. Note that the left C4 inferior articular process is anterior to the left C5 superior articular process.
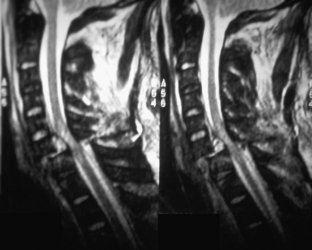
FIGURE 65-15 Sagittal MRI revealing significant cord edema and hemorrhage at the level of a C6-7 bilateral facet dislocation (stage 4 distractive flexion injury). Note the soft tissue density behind the body of C6, which may represent an extruded disc fragment.
Our overall approach has been to treat these injuries as unstable three-column injuries that necessitate a front-to-back fusion. In patients without an extruded disc, dorsal reduction and fixation is first performed; ventral fixation is then performed with an anterior cervical discectomy and fusion. In patients with an extruded disc, the anterior cervical discectomy is performed first. If sufficient reduction is obtained to reduce the facet joint, an anterior cervical fusion is then performed.105 If that is not possible, dorsal reduction and then anterior fusion are performed.111
Vertical Compression
A vertical compression fracture is described as a cervical burst fracture caused by an axial loading mechanism. Osseous failure is considered to be much more significant than damage to the ligamentous structures in this type of injury (Fig. 65-16). Treatment with halo immobilization is usually sufficient, although injuries at the cervicothoracic junction (C7) have a tendency to settle into kyphosis, which may require surgical intervention.96,112–114 Ventral surgical decompression and stabilization is often necessary in patients with an incomplete neurologic deficit.
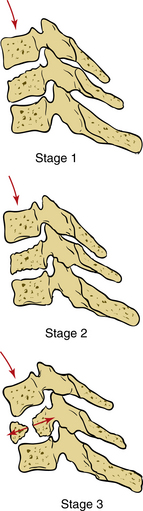
FIGURE 65-16 Vertical compression injury. Stage 1: central “cupping fracture” of the superior or inferior vertebral end plate. Stage 2: fracture of both superior and inferior end plates. Stage 3: displacement and fragmentation of the vertebral body.
(From Rizzolo SJ, Cotler JM: Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1:57–66, 1993.)
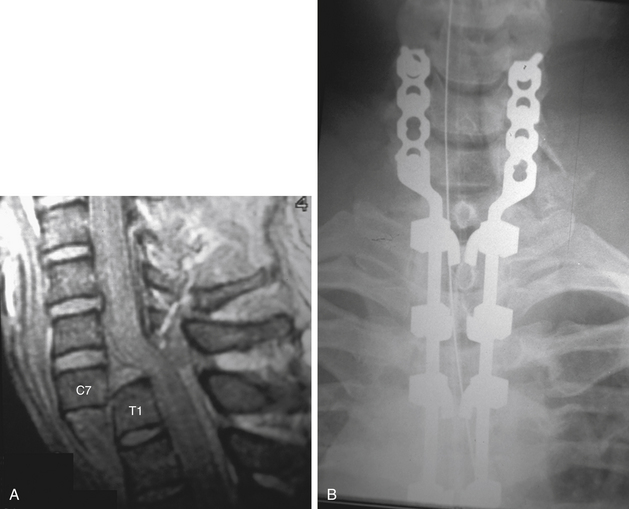
Distractive Extension
Distractive extension injuries are usually caused by forces that place the ventral elements under tension (Figs. 65-17 to 65-20). Ventral disc space widening is the characteristic radiographic finding, although failure may occur in a ventral-to-dorsal direction through the vertebral body. Less severe injuries may have little displacement, making radiographic detection difficult.107 The presence of a ventral avulsion fracture resulting from an avulsion of the anterior longitudinal ligament may provide a clue to this injury type, This injury is especially unstable in a patient with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis, in which two rigid moment arms are joined at an unstable junction. Distractive extension injuries are commonly associated with neurologic impairment. Patients frequently present with neurologic evidence of a central cord syndrome with significant weakness involving the upper extremities and relative sparing of the lower extremities. Spontaneous recovery is common.91 Most distractive extension injuries without disc space disruption are stable and may be treated nonoperatively, with late flexion-extension radiographs to confirm stability. Unstable injuries benefit from a ventral reconstructive procedure with ventral plating acting as a ventral tension band.107
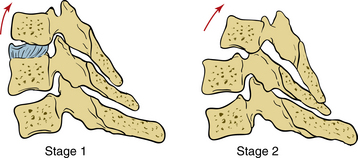
FIGURE 65-17 Distractive extension injury. Stage 1: failure of anterior ligamentous complex, which may present as a widening of the disc space or a nondeforming transverse fracture through the centrum. Stage 2: injury may be identified radiographically by an anterior marginal avulsion fracture of the centrum. Posterior ligamentous disruption may be identified by posterior displacement of the superior vertebra.
(From Rizzolo SJ, Cotler JM: Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1:57–66, 1993.)
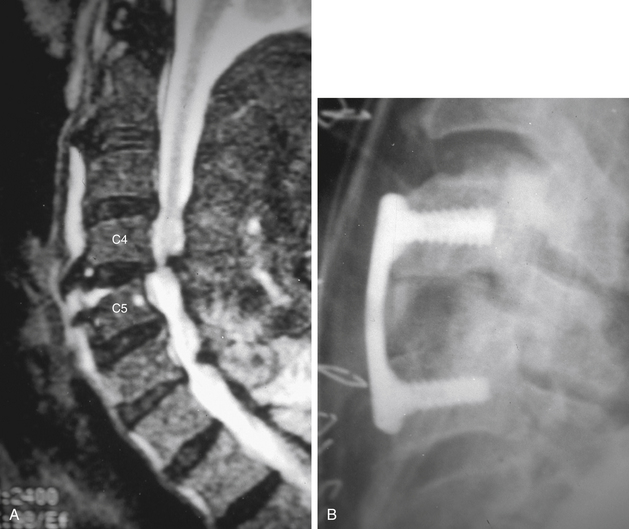
FIGURE 65-18 A, Sagittal MRI revealing a distractive extension injury at the C4-5 level with retrolisthesis of C4 on C5. B, Plain lateral radiograph after an anterior tension band (instrumented fusion) reconstruction of the injury.
Lateral Flexion
Lateral flexion injuries are secondary to asymmetrical compressive loading resulting in unilateral vertebral body compression failure and ipsilateral dorsal arch fracture (Fig. 65-21). As noted previously, this is the least common pattern of lower cervical spine disruption and is often stable, requiring cervical immobilization for 6 to 12 weeks.
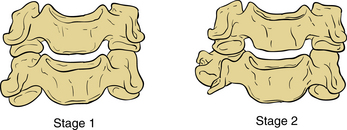
FIGURE 65-21 Lateral flexion injury. Stage 1: asymmetrical compression fracture of the centrum with associated ipsilateral vertebral arch fracture seen on lateral view; no displacement is noted on the anteroposterior (AP) view. Stage 2: displacement is evident on the AP as well as the lateral views. There may also be tension failure of the contralateral ligaments and facet joint.
(From Rizzolo SJ, Cotler JM: Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1:57–66, 1993.)
Summary
Over half of the 50,000 new spinal cord injuries reported annually in the United States occur in the cervical spine. Of these, 11,000 have some degree of permanent deficit. Further advancement and implementation of ATLS protocols may be expected to result in an increased number of multitrauma survivors with a proportionately increased incidence of cervical spine trauma presenting in our emergency departments. These trends and statistics underscore the socioeconomic importance of cervical spine trauma, and they add greater emphasis to the critical nature of early injury recognition, evaluation, and proper treatment.
Anderson L.D., D’Alonzo R.T. Fractures of the odontoid process of the axis. J Bone Joint Surg [Am]. 1974;56:1663-1674.
Daffner R.H. Evaluation of cervical cerebral injuries. Semin Roentgenol. 1992;27:239-253.
Denis F. Spinal instability as defined by the three column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1983;189:65-76.
Jefferson G. Remarks on fractures of the first cervical vertebra. BMJ. 1927;2:153-157.
Levine A.M., Edward C.C. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg [Am]. 1985;67:217-226.
Montane I., Eismont F.J., Green B.A. Traumatic occipitoatlantal dislocation. Spine (Phila Pa 1976). 1991;16:112-116.
Pang D., Wilberger J.E. Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1982;57:114-129.
White A.A.III, Panjabi M.M. Update on the evaluation of instability of the lower cervical spine. Instr Course Lect. 1987;36:513-520.
The complete reference list is available online at expertconsult.com.
1. Alker G. Computed tomography with and without myelography. Philadelphia: JB Lippincott; 1989.
2. Schneider R.C., Thompson J.M., Bebin J. The syndrome of acute central cervical spinal cord injury. J Neurol Neurosurg Psychiatry. 1958;21:216-227.
3. Woodring J.H., Goldstein S.J. Fractures of the articular process of the spine. AJR Am J Roentgenol. 1982;139:341-344.
4. Kirshenbaum K.J., Nadimpalli S.R., Fantus R., et al. Unsuspected cervical spine fractures associated with significant head trauma: the role of CT. J Emerg Med. 1990;8:183-198.
5. Vaccaro A.R., An H.S., Lin S., et al. Non-contiguous injuries to the spine. J Spine Disord. 1992;5:320-329.
6. Clark C.R., Ingram C.M., El Khoury G.Y., et al. Radiographic evaluation of cervical spine injuries. Spine (Phila Pa 1976). 1988;13:742-747.
7. White A.A.III, Panjabi M.M. Update on the evaluation of instability of the lower cervical spine. Instr Course Lect. 1987;36:513-520.
8. Daffner R.H. Evaluation of cervical cerebral injuries. Semin Roentgenol. 1992;27:239-253.
9. Scher A.T. Unilateral locked facet in cervical spine injuries. AJR Am J Roentgenol. 1977;129:45-48.
10. Dunn E.J., Blazer S. Soft tissue injuries to the lower cervical spine. Instr Course Lect. 1987;36:499-512.
11. Herkowitz H.N., Rothman R.H. Subacute instability of the cervical spine. Spine (Phila Pa 1976). 1984;9:348-357.
12. Webb J.H. Hidden flexion injury of the cervical spine. J Bone Joint Surg [Br]. 1976;55:322-327.
13. Mazur J.M., Stauffer E.S. Unrecognized spinal instability associated with seemingly simple cervical compression fractures. Spine (Phila Pa 1976). 1983;8:687-692.
14. Mori S., Nobuhiro O., Ojima T., et al. Observation of “tear drop” fracture-dislocation of the cervical spine by CT. J Jpn Orthop Assoc. 1983;57:373-378.
15. Goldberg A.L., Rothfus W.E., Deeb Z.L. The impact of magnetic resonance on the diagnostic evaluation of acute cervicothoracic spinal trauma. Skeletal Radiol. 1988;17:89-95.
16. Gay J.R., Abbott K.H. Common whiplash injuries of the neck. JAMA. 1953;152:1968-2704.
17. McNab I. Acceleration injuries of the cervical spine. J Bone Joint Surg [Am]. 1964;46:1797-1799.
18. Flohl M. Soft tissue injuries of the neck in automobile accidents: factors influencing prognosis. J Bone Joint Surg [Am]. 1974;56:1675-1682.
19. Joliffe V.M. Soft tissue injury of the cervical spine: consider the nature of the accident. BMJ. 1993;307:439-440.
20. LaRocca H.L. Cervical spine syndrome: diagnosis, treatment and long term outcome. In: Frymoyer J.W., Ducker T.B., Hadler N.M., et al, editors. The adult spine. New York: Raven Press; 1991:1051-1062.
21. Wickstrom J.K., Martinez J.L., Rodriguez R.P.O., et al. Hyperextension and hyperflexion injuries to the head and neck of primates. In: Gurdjian E.S., Thomas L.M., editors. Neckache and backache. Springfield, IL: Charles C .Thomas; 1970:108-117.
22. Wackenheim A. Roentgen diagnosis of the craniovertebral region. Berlin: Springer-Verlag; 1974.
23. Anderson P.A., Montesano P.X. Traumatic injuries of the occipito-cervical articulation. In: Camins M.B., O’Leary P.F., editors. Disorders of the cervical spine. Baltimore: Williams & Wilkins; 1992:273-283.
24. Montane I., Eismont F.J., Green B.A. Traumatic occipitoatlantal dislocation. Spine (Phila Pa 1976). 1991;16:112-116.
25. Anderson P.A., Montesano P.X. Morphology and treatment of occipital condyle fractures. Spine (Phila Pa 1976). 1988;13:731-736.
26. Stroobants J., Fidlers L., Storms J.L., et al. High cervical pain and impairment of skull mobility as the only symptoms of an occipital condyle fracture: a case report. J Neurosurg. 1994;81:137-138.
27. Malham G.M., Ackland H.M., Jones R., et al. Occipital condyle fractures: incidence and clinical follow-up at a level I trauma centre. Emerg Radiol. 2009;16:291-297.
28. White A.A.III, Panjabi M.M. Kinematics of the spine. In In White AA III, Panjabi MM, editors: Clinical biomechanics of the spine, ed 2, Philadelphia: JB Lippincott; 1990:92-97.
29. Dibenedetto T., Lee C.K. Traumatic atlanto-occipital instability: a case report with follow-up and a new diagnostic technique. Spine (Phila Pa 1976). 1990;15:595-597.
30. Eismont F.J., Bohlman H.H. Posterior atlanto-occipital dislocation with fractures of the atlas an odontoid process: report of a case with survival. J Bone Joint Surg [Am]. 1978;60:397-399.
31. Evarts C.M. Traumatic occipito-atlantal dislocation: report of a case with survival. J Bone Joint Surg [Am]. 1970;52:1653-1660.
32. Zigler J.E., Waters E.L., Nelson R.W., et al. Occipitocervico-thoracic spine fusion in a patient with occipitocervical dislocation and survival. Spine (Phila Pa 1976). 1986;11:645-646.
33. Maserati M.B., Stephens B., Zohny Z., et al. Occipital condyle fractures: clinical decision rule and surgical management. J Neurosurg Spine. 2009;11:388-395.
34. DeBeer J.D.V., Thomas M., Walters J., et al. Traumatic atlanto-axial subluxation. J Bone Joint Surg [Br]. 1988;70:652-655.
35. Feiz-Erfan I., Gonzalez L.F., Dickman C.A. Atlantooccipital transarticular screw fixation for the treatment of traumatic occipitoatlantal dislocation: technical note. J Neurosurg Spine. 2005;2:381-385.
36. Gabrielsen T.O., Maxwell J.A. Traumatic atlanto-occipital dislocation. AJR Am J Roentgenol. 1966;97:624-629.
37. Jeszenszky D., Fekete T.F., Lattig F., et al. Intraarticular atlantooccipital fusion for the treatment of traumatic occipitocervical dislocation in a child: a new technique for selective stabilization with nine years follow-up. Spine (Phila Pa 1976). 2010;35:E421-E426.
38. Jevitch V. Traumatic lateral atlanto-occipital dislocation with spontaneous bony fusion: a case report. J Spinal Disord. 1991;4:251-263.
39. Harris J.R.Jr., Carson G.C., Wagner L.K., et al. Radiographic diagnosis of traumatic occipitovertebral dissociation: comparison of three methods of detecting occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162:887-892.
40. Koop S.E., Winter R.B., Lonstein J.E. The surgical treatment of instability of the upper part of the spine in children and adolescents. J Bone Joint Surg [Am]. 1984;66:403-411.
41. Dunbar H.S., Ray B.S. Chronic atlanto-axial dislocations with late neurologic manifestations. Surg Gynecol Obstet. 1961;113:747.
42. Krantz P. Isolated disruption of the transverse ligament of the atlas: an injury easily overlooked at post-mortem examination. Injury. 1980;12:168-170.
43. Alker G., Oh Y., Leslie E., et al. Post mortem radiology of head and neck injuries in fatal traffic accidents. Radiology. 1975;114:611-617.
44. Pennecot G.F., Leonard P., Peyrot Des Gachons S., et al. Traumatic ligamentous instability of the cervical spine in children. J Pediatr Orthop. 1984;4:339-345.
45. Hatchette S. Isolated fracture of the atlas. Radiology. 1941;36:233-235.
46. Hinchey J., Bickel W. Fractures of the atlas: review and presentation of data on eight cases. Ann Surg. 1945;121:826-832.
47. Levine A. Avulsion of the transverse ligament associated with a fracture of the atlas: a case report. Orthopaedics. 1983;6:1467-1471.
48. Lipson S.J. Fractures of the atlas associated with fractures of the odontoid process and transverse ligament ruptures. J Bone Joint Surg [Am]. 1977;59:940-943.
49. O’Brien J.J., Butterfield W.L., Gossling H.R. Jefferson fracture with disruption of the transverse ligament. Clin Orthop Relat Res. 1977;126:135-138.
50. Royster R.M., Dryer D.F., Deeney V.F. Traumatic atlantal anterior arch fracture with associated avulsion fracture of the transverse ligament attachment: a previously undescribed combined entity. Spine (Phila Pa 1976). 1987;12:1058-1060.
51. Wigren A., Sweden U., Amici F.Jr. Traumatic atlanto-axial dislocation without neurological disorder: a case report. J Bone Joint Surg [Am]. 1973;55:642-644.
52. Hamilton A.R. Injuries of the atlanto-axial joint. J Bone Joint Surg [Br]. 1951;33:434-435.
53. Ames C.P., Acost F., Nottmeier E. Novel treatment of basilar invagination resulting from an untreated C-1 fracture associated with transverse ligament avulsion: case report and description of surgical technique. J Neurosurg Spine. 2005;2:83-87.
54. Fielding J.W., Hawkins R.J., Hensinger R.N., et al. Atlantoaxial rotary deformities. Orthop Clin North Am. 1978;9:955-967.
55. Fuentes S., Bouillot P., Palombi O., et al. Traumatic atlantoaxial rotatory dislocation with odontoid fracture: case report and review. Spine (Phila Pa 1976). 2001;26:830-834.
56. Panczykowski D., Nemecek A.N., Selden N.R. Traumatic type III odontoid fracture and severe rotatory atlantoaxial subluxation in a 3 year old child: case report. J Neurosurg Pediatr. 2010;5:200-203.
57. Esses S., Langer F., Gross A. Fracture of the atlas associated with fracture of the odontoid process. Injury. 1981;12:310-312.
58. Segal L., Grimm J., Stauffer E. Non-union of fractures of the atlas. J Bone Joint Surg [Am]. 1987;69:1423-1434.
59. Levine A., Edwards C. Fractures of the atlas. J Bone Joint Surg [Am]. 1991;73:680-691.
60. Plant H. Fracture of the atlas resulting from automobile accidents: a survey of the literature and a report of 6 cases. AJR Am J Roentgenol. 1938;40:867-890.
61. Sherk H.H., Nicholson J.T. Fractures of the atlas. J Bone Joint Surg [Am]. 1970;52:1017-1024.
62. Milward F. An unusual case of fractures of the atlas. BMJ. 1933;1:458.
63. Jefferson G. Remarks on fractures of the first cervical vertebra. BMJ. 1927;2:153-157.
64. Marlin A., Williams G., Lee J. Jefferson fractures in children. J Neurosurg. 1983;58:277-279.
65. Penning L. Paravertebral hematoma in cervical spine injury: incidence and etiologic significance. AJR Am J Roentgenol. 1981;136:553-561.
66. Templeton P.A., Young J.W., Mirvis S.E., et al. The value of retropharyngeal soft tissue measurements in trauma of the adult cervical spine: cervical spine soft tissue measurements. Skeletal Radiol. 1987;16:98-104.
67. Bucholz R., Burkhead W. The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Joint Surg [Am]. 1979;61:248-250.
68. Amling M., Hahn M., Wening V.J., et al. The microarchitecture of the axis as the predisposing factor for fracture of the base of the odontoid process. J Bone Joint Surg [Am]. 1994;76:1840-1896.
69. Levine A., Edwards C. Treatment of injuries in the C1/C2 complex. Orthop Clin North Am. 1986;17:31-44.
70. Anderson L.D., D’Alonzo R.T. Fractures of the odontoid process of the axis. J Bone Joint Surg [Am]. 1974;56:1663-1674.
71. Clark C.R., White A.A.III. Fractures of the dens: a multicenter study. J Bone Joint Surg [Am]. 1985;67:1340-1348.
72. Holsbeeck E.V., Stoffelen D., Fabry C. Fractures of the odontoid process: conservative and operative treatment, prognostic factors. Acta Orthop Belg. 1993;59:17-21.
73. Husby J., Sorensen K.H. Fractures of the odontoid process of the axis. Acta Orthop Scand. 1974;45:182-192.
74. Flanigan W.C., Powell F.C., Elwood P.W., et al. Odontoid fractures in elderly patients. J Neurosurg. 1993;78:32-35.
75. Seimon L.P. Fracture of the odontoid process in young children. J Bone Joint Surg [Am]. 1977;59:943-947.
76. Wisoff H.S. Fracture of the dens in the aged. Surg Neurol. 1984;22:547-555.
77. Pryputniewicz D.M., Hadley M.N. Axis fractures. Neurosurgery. 2010;66(Suppl 3):68-82.
78. Osgood R.B., Lund C.C. Fractures of the odontoid process. N Engl J Med. 1928;198:61-72.
79. Bohler J. Anterior stabilization for acute fractures and nonunions of the dens. J Bone Joint Surg [Am]. 1982;64:18-27.
80. Jeanneret B., Vernet O., Frei S., et al. Atlantoaxial mobility after screw fixation of the odontoid: a computed tomographic study. J Spinal Disord. 1991;4:203-211.
81. Levine A.M., Edwards C.C. Traumatic lesions of the occipitoatlantoaxial complex. Clin Orthop Relat Res. 1989;239:53-68.
82. Bucholz R.W. Unstable hangman’s fractures. Clin Orthop Relat Res. 1981;154:119-124.
83. Chittiboina P., Wylen E., Ogden A., et al. Traumatic spondylolisthesis of the axis: a biomechanical comparison of clinically relevant anterior and posterior fusion techniques. J Neurosurg Spine. 2009;11:379-387.
84. Levine A.M., Edward C.C. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg [Am]. 1985;67:217-226.
85. Levine A.M., Rhyne A.L. Traumatic spondylolisthesis of the axis. Semin Spine Surg. 1991;3:47-60.
86. Mollan R.A.B. Hangman’s fracture: injury. Br J Accident Surg. 1982;14:265-267.
87. Schneider R.C., Livingston K.E., Cave A.J.E., et al. “Hangman’s fracture” of the cervical spine. J Neurosurg. 1965;22:141-154.
88. Termansen N.B. Hangman’s fracture. Acta Orthop Scand. 1974;45:529-539.
89. Francis W.R., Fielding J.W., Hawkins R.J., et al. Traumatic spondylolisthesis of the axis. J Bone Joint Surg [Br]. 1981;63:313-318.
90. Pepin J.W., Hawkins R.J. Traumatic spondylolisthesis of the axis: hangman’s fracture. Clin Orthop Relat Res. 1981;157:133-138.
91. Vaccaro A.R., Madigan L., Bauerle W.B., et al. Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976). 2002;27:2229-2233.
92. Bristol R., Henn J.S., Dickman C.A. Pars screw fixation of a hangman’s fracture: technical case report. Neurosurgery. 2005;56(Suppl 1):E204.
93. Starr J.K., Eismont F.J. Atypical hangman’s fracture. Spine (Phila Pa 1976). 1993;18:1954-1957.
94. Denis F. Spinal instability as defined by the three column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1983;189:65-76.
95. Allen B.L., Ferguson R.L., Lehman T.R., et al. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7:1-27.
96. Capen D.A., Zigler J., Garland D.E. Surgical stabilization in cervical spine trauma. Contemp Orthop. 1987;14:25-32.
97. White A.A.III, Southwick W.O., Panjabi M.M. Clinical stability in the lower cervical spine: a review of past and current concepts. Spine (Phila Pa 1976). 1976;1:15-27.
98. Chen L., Yang H., Yang T., et al. Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine. 2009;10:3-8.
99. Aito S., D’Andrea M., Werhagen L., et al. Neurological and functional outcome in traumatic central cord syndrome. Spinal Cord. 2007;45:292-297.
100. Kasimatis G.B., Panagiotopoulos E., Megas P., et al. The adult spinal cord injury without radiographic abnormalities syndrome: magnetic resonance imaging and clinical findings in adults with spinal cord injuries having normal radiographs and computed tomography studies. J Trauma. 2008;65:86-93.
101. Imajo Y., Hiiragi I., Kato Y., et al. Use of the finite element method to study the mechanism of spinal cord injury without radiological abnormality in the cervical spine. Spine (Phila Pa 1976). 2009;24:E83-E87.
102. Pang D., Wilberger J.E. Spinal cord injury without radiographic abnormalities in children. J Neurosurgery. 1982;57:114-129.
103. Shen H., Tang Y., Huang L., et al. Applications of diffusion-weighted MRI in thoracic spinal cord injury without radiographic abnormality. Int Orthop. 2007;31:375-383.
104. Tewari M.K., Gifti D.S., Singh P., et al. Diagnosis and prognostication of adult spinal cord injury without radiographic abnormality using magnetic resonance imaging: analysis of 40 patients. Surg Neurol. 2005;63:204-209.
105. Paxinos O., Ghanayem A.J., Zindrick M.R., et al. Anterior cervical discectomy and fusion with a locked plate and wedged graft effectively stabilizes flexion-distraction stage-3 injury in the lower cervical spine: a biomechanical study. Spine (Phila Pa 1976). 2009;34:E9-E15.
106. Stauffer E.S. Management of spine fractures C3-C7. Orthop Clin North Am. 1986;17:45-53.
107. Harris J.H. Radiographic evaluation of spinal trauma. Orthop Clin North Am. 1986;17:75-86.
108. Rorabeck C.H., Rock M.G., Hawkins A.J., et al. Unilateral facet dislocation of the cervical spine: an analysis of the results of treatment in 26 patients. Spine (Phila Pa 1976). 1987;12:23-27.
109. Johnson M.G., Fisher C.G., Boyd M., et al. The radiographic failure for single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976). 2004;29:2815-2820.
110. Stauffer E.S., Kelly E.G. Fracture dislocations of the cervical spine: instability and recurrent deformity following treatment by anterior interbody fusion. J Bone Joint Surg [Am]. 1977;59:45-48.
111. Capen D.A., Nelson R.W., Zigler J., et al. Surgical stabilization of the cervical spine: a comparative analysis of anterior and posterior spine fusions. Paraplegia. 1987;25:111-119.
112. Evans D.K. Dislocations of the cervicothoracic junction. J Bone Joint Surg [Br]. 1983;65:124-127.
113. Grady M.S., Howard M.R., Jane J.A., et al. Use of the Philadelphia collar as an alternative to the halo vest in patients with C2-C3 fractures. Neurosurgery. 1986;18:151-156.
114. Panjabi M.M., White A.A.III, Johnson R.M. Cervical spine mechanics as a function of transection of components. J Bone Joint Surg [Am]. 1975;57:582.