CHAPTER 106 TRAUMA REHABILITATION
In 2002, unintentional injury was the most common cause of death between the ages of 1 and 44 years. There were 161,000 total injured deaths (56 per 100,000 population) that year. It was the fifth leading cause of death for all ages, after heart disease, malignant neoplasms, cerebrovascular events, and chronic respiratory disease. For males, it is the third leading cause of death, and seventh overall for females.1 Motor vehicle collision (MVC) was the most common cause of death related to trauma.
There were many more nonfatal than fatal injuries. In 2004, there were 29,654,475 (∼10,000/100,000) in the United States—involving all races, ages, and both sexes. Falls were most common (2756/100,000), followed by transportation-related injuries (1545/100,000). Violent nonfatal injuries occurred at a rate of 755/100,000.1
TRAUMA REHABILITATION TEAM
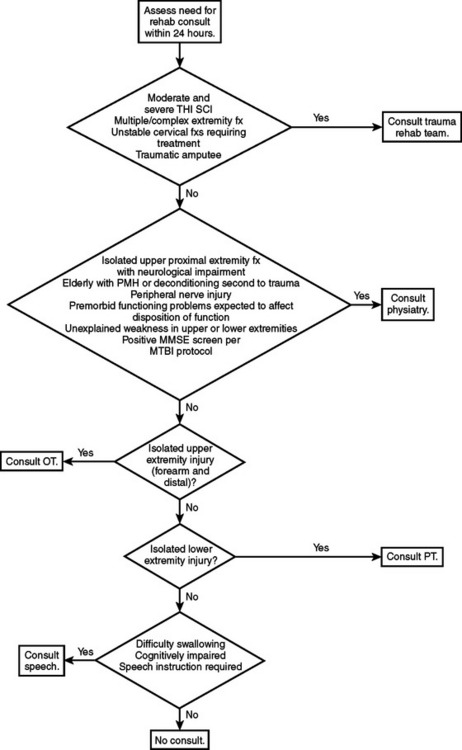
The case manager usually has a background in social service or nursing. Case managers play an integral role by assisting patients and their families with social and discharge planning issues. These managers are responsible for securing durable medical equipment, such as wheelchairs and modified commodes, for patients who are being discharged to home. See Figure 1 regarding rehabilitation screening of trauma patients.
ASSESSMENT OF PATIENTS WITH SPINAL CORD INJURY
Epidemiology of Traumatic Spinal Cord Injury in the United States
The incidence of SCI is estimated to be approximately 40 new cases per million population per year, or roughly 11,000. The estimated prevalence in the United States is 250 million persons.2 SCI primarily affects young adults. The average age at the time of injury is 37.6 years. The percentage of persons older than 60 years at injury has increased from 4.7% in 1980 to 10.9% since 2000. Of the SCI reported to the national database, 79% has occurred among males. Since 2000, MVC have accounted for 47.5% of SCI cases reported. Falls are the next most common cause of SCI, followed by acts of violence and recreational activities. Since 2000, the most frequent neurological category is incomplete tetraplegia (34.5%), followed by complete paraplegia (23.1%), complete tetraplegia (18.4%), and incomplete paraplegia (17.5%).3
Neurological Classification
Determining the neurological level and completeness of injury is the most accurate way of prognosticating recovery and functional outcome. Using the International Standards of Neurological and Functional Classification of Spinal Cord Injury, the examiner determines the motor and sensory level on the right and left and ascertains whether the injury is complete or incomplete.4
Using standard dermatomes and myotomes defined by the American Spinal Injury Association (ASIA), motor level is defined as the most caudal segment to have a muscle grade of 3. Five muscle groups are tested in the upper extremities, and five muscle groups are tested in the lower extremities. Each muscle group is supplied by two root levels, and each muscle group is graded from 0 to 5. Therefore, if the muscle grade is at least 3 of 5 the proximal root is believed to be intact. The sensory level is defined as the most caudal dermatome to have normal sensation to pin prick and light touch. Specific testing points are defined by ASIA4 (Figure 2).
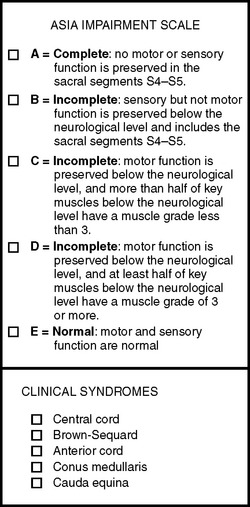
Figure 2 American Spinal Injury Association Impairment Scale.
(Adapted from American Spinal Injury Association: International Standards for Neurological Classification of Spinal Cord Injury, rev. 2006. Chicago, American Spinal Injury Association, 2006.)
In addition to defining the neurological level, the completeness of injury must be determined. See the ASIA impairment scale in Figure 2. A complete injury results in no motor or sensory function preserved in the sacral segments (ASIA A). There are four incomplete levels of ASIA: B, C, D, and E. Incomplete is defined as sparing of sensory and/or motor function below the neurological level that includes the sacral (S4-S5) segments.
Acute Medical Management
All patients with acute traumatic SCI receive methylprednisolone. This is based on the National Acute Spinal Cord Injury Studies (NASCIS), the last being NASCIS 3. This study concluded that patients treated within 3 hours of injury should receive 24 hours of steroids, and those treated in 3–8 hours of injury should receive 48 hours of steroids.5
C1-C3 neurological levels will require ventilatory support. The phrenic nerve (supplied by C3-C5 nerve roots) will be intact in patients with a C5 neurological level and below. As the level descends from mid-cervical to lower cervical, and then to thoracic, there will be greater innervation to abdominal and intercostal muscles—thereby making the work of breathing easier. The primary objective in early pulmonary management in SCI is to minimize secondary complications, including preventing hypoxemia, preventing and treating atelectasis, reducing risk of aspiration, and providing aggressive pulmonary management to compensate for impaired clearing of secretions.6
A bowel program should be established. Initially, a paralytic ileus is common. Patients may be placed on a stool softener and a daily or every-other-day suppository, with digital stimulation. This routine should be established about the same time each day. The goal is to prevent or minimize incontinence between bowel programs.
Deep venous thromboembolism (DVT) prevention is extremely important, as DVT and pulmonary embolism are major causes of morbidity and mortality in the SCI population. Sequential compression devices should be used, with or without elastic stockings, to improve lower extremity venous return. Such methods are contraindicated in patients with severe arterial insufficiency. Pharmacologic prophylaxis should be initiated within the first 72 hours, when not contraindicated. Low-molecular-weight heparin is the current recommendation. Anticoagulation should be continued for 8 weeks in patients with uncomplicated complete motor impairments, and for 12 weeks in complete motor injuries with other risk factors (lower limb fractures, history of thrombosis, cancer, heart failure, obesity, and age over 70). Vena cava filter placement is indicated in SCI patients with a contraindication for pharmacologic prophylaxis.7
ASSESSMENT OF PATIENTS WITH TRAUMATIC BRAIN INJURY
Epidemiology of Traumatic Brain Injury in the United States
There are 1.4 million people who sustain TBI in the United States annually. Approximately 50,000 will die, 235,000 are hospitalized, and 1.1 million are treated and released from the emergency department.8 Between 80,000 and 90,000 people experience long-term disability associated with TBI.9 According to the TBI Model System database, MVCs account for 48.3%—with the next most common cause of TBI being falls, followed by violence. The most common cause of death from MVCs is TBI. Approximately 5.3 million Americans (or about 2% of the population) currently live with disabilities caused by TBI.10
Initial Physiatric Consultation and Early Rehabilitation Intervention
The chart should be thoroughly reviewed, including all associated injuries, comorbid conditions, and diagnostic studies. It is important to document social information, including premorbid vocational and educational status, as well as the family and home situation. Obtaining prehospital records documenting any loss of consciousness and Glasgow Coma Scale (GCS) prehospital and at admission will help determine the severity of brain injury. A GCS of 8 or less is considered severe, a GCS between 9 and 12 is considered moderate, and a GCS of 13–15 is a mild TBI (Table 1).
| Parameter | Score |
|---|---|
| Best Motor Response | |
| Normal | 6 |
| Localizes | 5 |
| Withdraws | 4 |
| Flexion | 3 |
| Extension | 2 |
| None | 1 |
| Best Verbal Response | |
| Oriented | 5 |
| Confused | 4 |
| Verbalizes | 3 |
| Vocalizes | 2 |
| None | 1 |
| Eye Opening | |
| Spontaneous | 4 |
| To command | 3 |
| To pain | 2 |
| None | 1 |
A thorough neurological examination includes a mental status evaluation and assessment of neurological recovery using the Rancho Los Amigos Scale of Cognitive Functioning (Table 2). The Rancho Los Amigos Scale is used for patients with moderate to severe TBI and spans from Level 1 to Level 8. Level 1 indicates no response to any stimuli. Level 8 is when all activities are purposeful and appropriate.11
Table 2 Rancho Los Amigos Scale of Cognitive Functioning
| I | No response to any stimuli. |
| II | Generalized reflex response to pain. |
| III | Localized response. Blinks to light, tracks, inconsistent response to commands. |
| IV | Alert, but confused and agitated. |
| V | Confused, nonagitated. Social, but with inappropriate verbalizations. |
| VI | Inconsistent orientation. Impaired short-term memory. Goal-directed behavior, with assistance. |
| VII | Automatic appropriate behavior in familiar tasks and environment. |
| VIII | Purposeful, appropriate behavior allows functional independence. Social, emotional, intellectual levels may be decreased compared to pretraumatic brain injury. |
Medical Considerations and Complications in Traumatic Brain Injury
Medications can be used, but they provide varied results. Dantrolene acts directly on skeletal muscle and reduces muscle contraction by a direct effect on the excitation-contraction coupling mechanism. Dantrolene is effective for cerebral spasticity. It should not be used for people with liver dysfunction, and all those on Dantrolene should be given liver function tests. Baclofen inhibits monosynaptic and polysynaptic spinal reflexes, and is more effective for spinal spasticity. Sedation is a common side effect, and the dosage should be increased slowly. Tizanidine binds to central alpha2adrenergic receptors, and therefore reduces spasticity by acting centrally. Tizanidine is more effective for spinal spasticity than cerebral spasticity. Hypotension and elevated liver function tests are common side effects. Diazepam and other benzodiazepines are also effective, but are sedating and usually should be avoided. Local injections using Botulinum toxin, phenol, or alcohol can be used for specific muscles. Intrathecal Baclofen may be considered if the previously cited measures do not work.
The risk of seizures is increased by brain injury severity, depressed skull fracture, intracranial hematoma, early seizure, penetrating injury, and prolonged unresponsiveness. According to practice guidelines of the American Academy of Physical Medicine and Rehabilitation, there is evidence for the use of antiepileptic drugs within the first week after TBI. However, there is no good evidence to support their use after the first week of injury.12
ASSESSMENT OF PATIENTS WITH PERIPHERAL NERVE INJURY
Epidemiology of Peripheral Nerve Injuries
The estimated incidence of peripheral nerve injuries in patients admitted to a Level I trauma center, including plexus and root injuries, is about 5%.13 The radial nerve is the most frequently injured nerve in the upper extremity due to mid-shaft humerus fractures, as the radial nerve travels around the spiral groove. Ulnar nerve injuries are associated with elbow fractures, with or without dislocations. The median nerve may also be injured at the level of the elbow or with supracondylar distal humerus fractures. Rarely, there may be peripheral nerve injuries due to forearm fractures—particularly in the rare case of compartment syndrome in the forearm.
Electrodiagnostic Testing and Classification of Peripheral Nerve Injury
A commonly used classification of peripheral nerve injury is the Seddon classification.14 Neurapraxia is the most mild because there is no axonal degeneration (Wallerian degeneration). There is focal demyelination or ischemia causing partial or complete conduction block at the site of injury. The nerve distal to the injured segment functions normally. Recovery is usually good and takes weeks to months, but may be only hours or days if mild and localized. Axonotmesis occurs when there is Wallerian degeneration. For recovery to occur, there must be regeneration of the nerve. Both the axon and the myelin are disrupted. The extent of recovery will depend on the extent of disruption, including the surrounding connective tissue (endoneurium and perineurium) as well as the distance between the site of injury and the muscles it supplies. Neurotmesis is diagnosed when the axon and all connective tissue, including the most external (the epineurium), are disrupted. There will be no spontaneous recovery and only surgery may be helpful.
Many times, electrodiagnostic studies (electromyography [EMG], plus nerve conduction studies) are used to confirm and prognosticate the recovery of a nerve injury. Wallerian (axonal) degeneration takes up to 9 days for motor fibers, and 11 days for sensory fibers, postinjury.15 This information is relevant in performing nerve conduction studies.
ASSESSMENT OF PATIENTS WITH MULTIPLE ORTHOPEDIC INJURIES: THE POLYTRAUMA PATIENT
Orthopedic injuries account for almost half of all trauma-related hospital and inpatient rehabilitation admissions annually in the United States. Patients with multiple orthopedic injuries, or polytrauma patients, account for approximately 10% of inpatient rehabilitation admissions.16 The care of polytrauma patients in an acute care setting is extremely challenging, as they are often victims of high-speed decelerations with significant nonorthopedic-associated wounds. The hospital course of these patients is often complicated by the need for hemodynamic resuscitation, multiple surgical procedures, and the occasional delayed diagnosis of occult injuries. As noted, many of these patients will require intensive inpatient rehabilitation upon discharge. Early involvement of a well-trained physiatrist is critical to ensure the best possible rehabilitative potential and to prevent delays in care and avoidable long-term complications.
Acute Hospital Care
Generally, in-hospital rehabilitation will follow a logical progression from immobilization (occasionally with casts or braces) to passive range of motion exercises. If the patient is cooperative, this is followed by conditioning exercises—especially if the patient experienced significant deconditioning or muscle atrophy. Finally, varying degrees of weight bearing will be allowed—often aided by the use of crutches or walkers. The provision of adequate analgesia is absolutely critical during this early rehabilitative phase. Narcotics or nonsteroidal drugs must be timed properly to have maximum effect during periods of increased activity, yet not be dosed in a fashion to produce lethargy or foster dependency. For patients with low pain tolerances or previous drug dependency, early involvement of a pain management consultant may facilitate and shorten rehabilitation. Lack of appropriate participation in rehabilitation by a patient may be a sign of depression, and if so should trigger involvement of a psychologist or psychiatrist. Patients with significant TBI are particularly challenging because they may not be able to adequately participate in any meaningful active rehabilitation regimens.
1 National Center for Injury Prevention and Control WISQUARS (Web-based Injury Statistics Query and Reporting System) leading causes of nonfatal injury reports, 2006. www.cdc.gov/ncipc/wisquars
2 Cardenas DD, Hoffman JM, Stockman PL. Spinal cord injury. In: Robinson LR, editor. Trauma Rehabilitation. Philadelphia, Lippincott: Williams and Wilkins, 2005.
3 National Spinal Cord Injury Statistical Center: Facts and figures at a glance—June, 2005. www.spinalcord.uab.edu
4 Marino RJ, editor. American Spinal Injury Association: International Standards for Neurological and Functional Classification of Spinal Cord Injury, rev. 2002, Chicago: American Spinal Injury Association, 2002.
5 Bracken MB, Shephard MJ, Holford TR, Leo-Summers L, Aldrich EF, Faz LM, et al. Administration of methylprednisolone for 24 or 48 hours or tirilizad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA. 1997;277:1597-1604.
6 Lanig IS, Peterson WP. The respiratory system in spinal cord injury. Phys Med Rehabil Clin North Am. 2000;11(1):29-43.
7 Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Spinal Cord Medicine: Prevention of Thromboembolism in Spinal Cord Injury, 2nd ed. Consortium for Spinal Cord Medicine, 1999. http://www.pva.org/publications/pdf/DVT.pdf
8 Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention, Nation Center for Injury and Prevention and Control, 2004. http://www.cdc.gov/ncipc/pub-res/TBI_in_US_04/TBI-USA_Book-Oct1.pdf
9 Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: a public health perspective. Head Trauma Rehabil. 1999;14(6):602-615.
10 Traumatic Brain Injury National Data Center The Traumatic Brain Injury Model Systems. West Orange, NJ, Kessler Medical Rehabilitation Research and Education Corporation. www.tbindc.org
11 Nalkmus D, Booth BJ, Kodimer C. Rehabilitation of the Head Injured Adult: Comprehensive Cognitive Management. Downey, CA: Professional Staff Association of Rancho Los Amigos Hospital, 1980.
12 Brain Injury Special Interest Group of the American Academy of Physical Medicine and Rehabilitation. Practice parameter: antiepileptic drug treatment of posttraumatic seizures. Arch Phys Med Rehabil. 1998;79:594-597.
13 Noble J, Munro CA, Prasad VS, Midha R. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma. 1998;45(1):116-122.
14 Seddon HJ. Surgical Disorders of the Peripheral Nerves, 2nd ed. Edinburgh and New York: Churchill Livingstone, 1975.
15 Chaudhry V, Cornblath DR. Wallerian degeneration in human nerves: serial electrophysiological studies. Muscle Nerve. 1992;15(6):687-693.
16 Uniform Data System for Medical Rehabilitation: Annual Inpatient Rehabilitation Facilities Report, 2003–2004. Amherst, NY, Uniform Data System for Medical Rehabilitation, 2004