Trauma life support
Introduction
Trauma remains the leading cause of death among those under 40 years of age and it is suggested that after cardiovascular disease and cancer, traumatic injury is the leading cause of death across all ages in the developed world (O’ Reilly 2003 Span et al. 2007, Greaves et al. 2009). Injuries kill some 5 million people each year, equating to 9 % of worldwide deaths, and young people between the ages of 15 and 44 account for approximately 50 % of global mortality due to trauma (Middleton 2011). There are an estimated 20 000 cases of serious/multiple injuries in England annually (National Audit Office 2010) resulting in approximately 5400 deaths and a significant proportion of victims suffer permanent disability. It is important to acknowledge that these serious injuries, commonly referred to as ‘major’ trauma, represent a small proportion of workload annually for most Emergency Departments (EDs) – approximated at 0.2 % of normal activity (National Audit Office 2010). In the current economic climate some may question why such an emphasis is placed upon this area of emergency care. The rationale for this may be explained by considering the age group most affected by this epidemic. People under 40 years who may be in gainful employment could work until 65 or more years of age. This employment reflects tax revenue and personal expenditure. This in effect supports the national economy. The loss of those individuals from society from a purely financial perspective is significant. Effective care and treatment may prevent death or disability. It is crucial that quality of care and resources reflect the needs of this demographic. As Cole (2004) notes, the human cost of trauma on society is incalculable.
Reflecting a concept described by the Resuscitation Council (UK) (2010) the ‘chain of survival’ in trauma care is important when attempting to reduce mortality/morbidity from serious injury (Lott et al. 2009). The continuum of care from scene of accident to definitive care should remain intact. Put simply, communication and standards of care are crucial. The Advanced Trauma Life Support (ATLS®) programme (American College of Surgeons 2008), which follows a sequence of priorities of care, with the objective of minimizing mortality and morbidity, has been widely adopted for trauma patients throughout the world. The adoption of this international system offers many benefits for both the practitioner and patient. ATLS is utilized throughout the UK; a practitioner working in London, for example, should expect to be able to operate the same principles of trauma care in Aberdeen. The system in effect is a language – improving communication between professionals.
The initial assessment component of the system comprises:
The application of these components and maintenance of the chain of survival is reliant upon excellent teamwork. The composition of the team will vary from hospital to hospital. The principles however remain unchanged:
• good organization and communication
• excellent cooperation between all medical specialists involved (Lott et al. 2009).
Much of the emphasis on trauma care is on medical assessment and intervention, and defining the role of the nurse within the trauma team can be difficult (Table 2.1 ).
Table 2.1
Nursing roles within the trauma team
| Assessment | Observation of respiratory rate, pulse, BP, capillary refill time, GCS |
| Intervention | Basic airway management, insertion of vascular access, phlebotomy, i.v. fluid/blood product administration, application of splinting |
| Monitoring | ECG/cardiac monitoring, arterial lines, capnography, repetition of observations and documentation |
| Communication | Reassurance and information for the conscious patient, liaison between team members/specialist involvement, communication with tertiary/specialist centres |
| Leadership | Activating trauma team, coordinating nursing care (including care of relatives/significant others) |
Preparation
High-quality care is important in the pre-hospital phase of trauma care and time spent on scene with the patient should be kept to the minimum (Pre-Hospital Trauma Life Support Committee 2002). Much debate remains regarding the extent to which pre-hospital practitioners should instigate advanced trauma interventions – the so-called ‘scoop and run’ versus ‘stay and play’. Smith & Conn (2009) contend that there has been no proven benefit to the patient of advanced interventions, e.g., chest drain insertion or rapid sequence induction and endotracheal intubation. This evidence, however, was specific to urban environments, and its validity to more remote incidents may be questionable. The focus of pre-hospital care should be on airway management, control of haemorrhage, immobilization and transfer of the patient to the nearest and most appropriate facility. In many instances, the ambulance service alerts the ED to the impending arrival of a multiply injured patient. This allows time for appropriate preparation of personnel and environment. Irrespective of the level of staffing, a systematic approach to care should apply on every occasion and it should be constantly monitored to maintain optimum effectiveness and efficiency (Sexton 1997). Equally, safety measures are imperative for both staff and patients to ensure no needless harm is caused (see Table 2.2).
Table 2.2
Safety measures during trauma care∗
| Minimum safety requirements for team members | Gloves Aprons Goggles Lead aprons, where appropriate |
| Patient safety | Effective infection control measures Maintenance of temperature e.g., blankets or provision of Bair Hugger© |
∗It is assumed that all staff have been immunized against hepatitis B
Primary survey
The ATLS approach requires a two-stage approach to the management of the patient. The first stage, or primary survey, follows an adapted ABCDE format similar to the initial assessment applied in medical emergencies (Resuscitation Council (UK) 2010). The adaptation introduces cervical spine control, control of haemorrhage and, importantly, environmental control (American College Surgeons 2008). Environmental control should be interpreted as the prevention of hypothermia. The importance of this will be discussed later in this chapter. It may help to remember the adapted approach as AcBDE. The addition of the letter ‘F’ as Fahrenheit may help some remember the need for temperature control (Table 2.3).
Table 2.3
| Activity | |
| Ac | Airway with cervical spine control |
| B | Breathing |
| C | Circulation and control of haemorrhage |
| D | Disability |
| E | Exposure |
| F | Fahrenheit – control of environment |
The primary survey is a rapid assessment aiming to detect life-threatening problems and dealing with them as they are discovered. Although the survey would appear to occur sequentially, i.e., Ac, B then C etc., in fact in the team context each component may be assessed simultaneously. In many cases in the UK an anaesthetist may assess and manage the airway while another member assesses breathing, another controls haemorrhage, and so on.
Airway with cervical spine control
The management of a patient’s airway takes precedence over all other aspects of patient care. Cervical spine control should be instigated simultaneously. The ability of the patient to answer simple questions confirms that the airway is patent and that sufficient oxygen is perfusing the brain to elicit a reply. A physical examination of the airway should still be undertaken (American College of Surgeons 2008).
If the patient does not respond to a simple question, airway obstruction should be assumed and measures should be taken to relieve this immediately. The most common reason for obstruction in the unconscious patient is partial or complete occlusion of the oropharynx by the tongue. Saliva, vomit and blood may exacerbate the problem. Interventions should begin with the simplest, progressing to the more complex if necessary. A chin lift or jaw thrust should pull collapsed soft tissues out of the airway. Any debris or foreign bodies must be physically removed. Suction can be very effective, using a tonsil tip/rigid (Yankeur) suction catheter. Cole (2004) recommends the tip of the Yankeur suction catheter be kept in sight to ensure it is not inserted too deeply causing the patient’s gag reflex to be stimulated. Equally, blind finger sweeps should not be used as this may further push foreign objects into the airway.
More active measures may be required for those who are unable to maintain their own airway. A nasopharyngeal airway will ensure patency in the conscious patient, without causing a gag reflex. This may be particularly useful for those with a fluctuating conscious level. Caution should be exercised, however, in patients with a head injury. The presence of a fracture of the base of skull precludes the use of this device, as accidental placement of the airway in the cranial vault is a possibility (Greaves et al. 2009). For the unconscious patient, an oropharyngeal (Guedel) airway may be helpful; however, its use increases the risk of vomiting.
A definitive airway should be established if there is any doubt about the patient’s ability to maintain airway integrity (American College of Surgeons 2008). After any intervention the patency of the airway should be re-checked. A cuffed tube placed in the trachea is the gold standard for securing and protecting the airway. However, the laryngeal tube airway and the intubating laryngeal mask airway (LMA) are recent advances in airway management that can facilitate intubation in the patient with a difficult airway (American College of Surgeons 2008, Stoneham et al. 2001).
Breathing
A patent airway does not automatically mean that the patient is able to breathe properly. The patient’s chest should be watched carefully, for the rise and fall of the chest wall, on both sides. The assessor should listen for breath sounds and feel for exhaled breath. If the patient is not breathing or is breathing inadequately, mechanical ventilation using a BVM system with high-flow oxygen should be instituted. This is usually more effective when performed by two people, one to seal the airway and one to squeeze the self-inflating bag.
Efficiency of breathing should be established by applying the acronym RIPPA: Respiratory rate, Inspection, Palpation, Percussion and Auscultation (Table 2.4).
Table 2.4
Assessment of breathing (RIPPA)
| Respiratory rate | Observing rate and peripheral oxygen saturation |
| Inspection | Symmetry of chest expansion, cyanosis, use of accessory muscles, tracheal shift from the midline, engorged neck veins, any sucking chest wounds |
| Palpation | Crepitus, surgical emphysema, sites of tenderness |
| Percussion | This may help determine the presence of haemothorax or pneumothorax |
| Auscultation | Bilateral air entry, presence of abnormal or absence of sounds |
Breathing that is unequal or asymmetrical may indicate bony injury or an underlying pneumothorax. Pulse oximetry is a valuable monitor, as peripheral oxygen saturation is a good measure of breathing efficiency; however, it must be remembered that the reading may not be accurate in a shocked, hypothermic, or burned trauma patient (Casey 2001). Where the patient is intubated, the use of colorimetric carbon-dioxide-measuring devices is regarded as essential to ensure correct tube placement. All trauma patients should receive high-flow oxygen (American College of Surgeons 2008). Metabolic demand following serious injury increases significantly. Inadequate oxygen delivery to cells can result in cell damage. In some cases this can result in an inflammatory response known as systemic inflammatory response syndrome (SIRS) similar to that seen in the septic patient (Adams & Osborne 2009). This can further complicate the condition of a seriously injured patient. A concentration of approximately 95% arterial saturation can be achieved by administering oxygen at 15 L/min through a non-rebreather oxygen mask.
Sucking chest wounds should be covered. Chest decompression will be required immediately in the event of a tension pneumothorax, as this dramatically compromises ventilation and circulation. Equipment for inserting a chest drain should be prepared following a needle thoracentesis. A large flail segment with pulmonary contusion or a massive haemothorax should be treated straight away. If the patient is unable to maintain adequate ventilation unassisted, endotracheal intubation may be required, with mechanical ventilation. After any manoeuvre is used to correct inadequate ventilation, breathing should always be rechecked.
Circulation with haemorrhage control
The most significant contributions to developments in trauma care in recent years have emanated from military medical/nursing care (Champion & Leitch 2012). Conflicts in Afghanistan and Iraq in particular have forced military surgeons to adapt and improve interventions to improve outcomes in the most extreme injuries (Duncan & Moran 2009, Greaves et al. 2009). Many of these developments have made their way into civilian trauma care. Despite improvements in trauma care, uncontrolled bleeding contributes to 30–40% of trauma-related deaths and is the leading cause of potentially preventable early in-hospital deaths (Kauver et al. 2006, Span et al. 2007). Hypotension in the injured patient should be assumed to be due to haemorrhage until proven otherwise (Duncan & Moran 2009). Although assessment of circulation and control of bleeding would usually follow assessment of airway and breathing where assessment is sequential, there are occasions where control of haemorrhage may take precedence. Catastrophic haemorrhaging, i.e., rapid bleeding likely to result in imminent death, for example, following stab injury, should be dealt with immediately. The military adapt the ATLS protocol to <C>AcBCDE, where <C> represents control of catastrophic haemorrhage (Greaves et al. 2009, Sapsford 2008). This may take the form of direct pressure and elevation where possible. In specific circumstances, however, particular measures may need to be taken that were previously unavailable or avoided in civilian trauma care. Two specific interventions include the judicious use a tourniquet, and the use of haemostatic agents, e.g., Celox®.
Determination of the patient’s circulatory status should be made by assessing:
• skin colour and general appearance – check for the presence of pallor, diaphoresis (sweating) and temperature of extremities
• pulse – rate, depth and volume. Tachycardia in the presence of a normal blood pressure (normotension) may be the only indication of hypovolaemia in the injured patient. The absence of a pulse following serious injury is a very poor prognostic indicator. Very few patients recover from a cardiac arrest in this situation. The most recent ATLS guidelines recommend that where a patient suffering penetrating trauma has no cardiac output that no resuscitation effort should be made (American College of Surgeons 2008)
• conscious level – the reduction in cellular perfusion in hypovolaemia results in anxiety in the early stages or confusion/agitation in later stages. These are important signs, and the nurse communicating with the patient may be in the ideal position to observe any alteration in this.
Fluid resuscitation (the replacement of fluid in the presence of hypovolaemia) is the subject of much debate and research in recent years. To facilitate fluid administration at least two short, wide-bore cannulae are inserted (14–16 gauge) into large veins as proximal in peripheries as possible, e.g., antecubital fossa. Lines should not be placed in injured extremities if they can be avoided. It is important to remember that the rate of intravenous (i.v.) infusion is not determined by the size of the vein, but by the internal diameter of the cannula, and is inversely affected by its length. Where venous access proves difficult or impossible alternatives include venous cut down or intraosseous cannulation (Hunt & Hunt 2011).
The ATLS system currently advocates the principle of fluid challenge. According to this protocol an initial fluid bolus of two litres of warmed Hartmann’s solution is administered through a blood-giving set (American College of Surgeons 2008). The patient’s response to this ‘fluid challenge’ is then determined to decide whether further fluid/blood product is required. Patients will either respond:
• rapidly – patients return to a normal cardiovascular state and remain normal
• transiently – patients return to a normal cardiovascular state for a brief period, but begin to deteriorate thereafter
• minimal or no response – patients fail to respond or respond to a minimal extent.
There is evidence to suggest that in some circumstances fluid resuscitation should be related to pulse pressures, e.g., the presence of a radial pulse. This equates to a systolic blood pressure of at least 70 mmHg (Duncan & Moran 2009; Geeraedts et al. 2009; Greaves et al. 2009). This approach is known as permissive hypotension. The rationale behind this approach is that the systolic blood pressure of >70 mmHg would be sufficient to perfuse vital organs, but importantly would not be a pressure high enough to disrupt a newly formed clot at the site of bleeding. Fluid is given in 250 mL boluses to maintain a palpable radial pulse. This is particularly important in so-called ‘incompressible’ bleeding, e.g., intra-abdominal or pelvic bleeding. The exception to this approach would be the presence of a significant head injury. In this situation higher minimum pressures are required to maintain cerebral perfusion pressure (Greaves et al. 2009).
It is an obvious statement that the best replacement for lost blood is blood itself, however, blood is a valuable and scarce commodity that takes time to cross match and prepare. O-negative blood can be used and should be stored in small quantities in the ED for such cases. Patient blood samples should be taken early, as infusion of large quantities of O-negative blood can cause difficulties with grouping and cross-matching later. In the interim, intravenous fluids in the form of crystalloids or colloids can be administered. There has been debate in the past regarding which fluid was optimal. Crystalloids are cheaper than colloids, and are more effective in restoring intravascular volume (Schierhout & Roberts 1998). Hartmann’s solution is a good option; however 0.9 % sodium chloride (‘normal’ saline) is an acceptable alternative (American College of Surgeons 2008). It is important to remember that for every millilitre of estimated blood volume lost, three millilitres of crystalloid should replace it. Neither fluid can enhance oxygen-carrying capacity or enable coagulation. The volume of fluid should therefore be cautious to avoid haemodilution and subsequent coagulopathies.
Occult bleeding, for example, from fractured long bones, can be the cause of hypovolaemia. Haemorrhage control therefore should take into account the need for interventions such as traction of long bones or pelvic splinting (Geeraedts et al. 2009).
Cardiac monitoring provides circulatory information from the heart rate and rhythm. It also provides an indicator of hypoxia, hypoperfusion, myocardial contusion, or hypothermia in the form of arrhythmias or ectopic beats. Pulseless electrical activity (PEA) is suggestive of profound hypovolaemia, cardiac tamponade, or tension pneumothorax (Resuscitation Council (UK) 2010) and has a poor prognosis unless the cause can be found and treated immediately.
Urinary catheters and nasogastric tubes should be considered part of the resuscitation of the patient. Urine output is a sensitive measure of renal perfusion and an invaluable way to assess success of the resuscitation. A urinary catheter attached to a urometer should be inserted, providing no contraindications exist, such as blood at the urinary meatus, scrotal haematoma or a high-riding prostate, which would indicate urethral damage (American College of Surgeons 2008, Greaves et al. 2009). A urometer will ensure that accurate hourly measurements of urine output can be taken. If urethral catheterization is contraindicated due to urethral damage, a suprapubic catheter should be inserted by a suitably skilled team member. A urinary output of more than 50 mL/h in an adult is a good indicator of satisfactory tissue perfusion. The urine that is voided initially should be tested for blood and saved for microscopy and subsequent possible drug analysis.
Disability: neurological status
A simple and rapid assessment of neurological status should take place during the primary survey. The evaluation should establish level of consciousness, pupil size and reaction. The Glasgow Coma Scale (GCS) is the commonest method used for the assessment of level of consciousness and a sequence of readings will tend to show fairly subtle changes quickly. Continuity in measurement is important and measurements should be made by the same person.
As part of the GCS, painful stimulus is sometimes required. There is much variation in the nature of the stimulus. Some areas advocate the use of a sternal rub, while others suggest pressure over the supraorbital ridge or pinching of the trapezius muscle (Waterhouse 2009). Whatever the stimulus method used, the level should not be so excessive as to cause damage to the skin or underlying soft tissues. Be aware of patients with spinal cord injury and upper limb fractures as they may feel painful stimulus but be unable to respond with limb movement. In all cases painful stimuli should be kept to a minimum.
Exposure/environmental control
At the end of the primary survey, every item of clothing must be removed, without risking any further damage to the patient (American College of Surgeons 2008). It is prudent at this point to log-roll the patient so that the back, which comprises 50% of the body, can be fully examined and the rescue board can be removed, along with any debris or retained clothing. Failure to assess the back of the patient can mean that the assessor misses a life-threatening injury. However, rolling a patient with an unstable pelvic fracture can result in further pelvic haemorrhage, so minimal movement and gentle handling are crucial (Little et al. 2001).
Hypothermia in trauma
Trauma patients are at risk from hypothermia (<35°C). Many have been exposed to cold, wet conditions, and blood loss can contribute further to a drop in core temperature. Hypothermia increases morbidity and mortality by a factor of up to three and must be prevented or reversed (Ireland et al. 2011). Secondary hypothermia should be prevented from occurring in the resuscitation room. This is an important aspect of nursing care that should not be neglected in what can be a busy and distracting environment. Various measures can be used, including:
Full history
An AMPLE history helps plan patient care:
Details regarding the mechanism of injury can indicate the site and seriousness of many potential injuries. This information can help target specific treatment strategies, e.g., a fall of 30 cm is less likely to have significance than a fall of 2 m. In this situation the incidence of spinal injury increases and appropriate measures can be taken (Dickinson 2004).
A clear cervical spine X-ray may provide valuable information about serious injury. However, when appropriate, these and any other X-rays required can be deferred to the secondary survey. A major pitfall in the immediate assessment of cervical spine integrity is a failure to recognize that early imaging on its own is inadequate to safely clear the spine (Little et al. 2001).
Good communication, explanation and gentle handling are important preliminaries to analgesia. Correct immobilization of fractures will also relieve a great deal of pain. Other sources of discomfort should be excluded, e.g., full bladder. Analgesia should not be avoided just because the patient has a head injury, but it should be carefully administered and the patient must be monitored afterwards.
Secondary survey
The primary survey and resuscitation must be completed before the secondary survey begins (Robertson & Al-Haddad 2013). If, at the end of the primary survey, the patient’s condition remains unstable, each step should be repeated until stability is achieved. During the secondary (head-to-toe) survey, less obvious injuries, which may pose a latent threat to life, should be detected.
At this stage assessment of vital signs every five minutes should be initiated:
• temperature – rectal or tympanic membrane
• pulse (radial, femoral or carotid) – rate, rhythm and volume
Vital signs should be monitored by the same person to avoid assessor variability.
Trauma patients are vulnerable to the effects of pressure on their skin, and every effort should be made to prevent any unnecessary risk (Swartz 2000). Patients who arrive in the ED on a spine board should be transferred from it as soon as is safe (Cooke 1998). Wet and soiled linen must be removed as soon as possible.
Head and face
Swelling may prevent adequate examination of the eyes, later, so assess:
• visual acuity – this may be modified to suit the situation using either a specifically designed hand-held Snellen chart, or asking the patient to read printed text at a set distance
• bleeding into the anterior chamber (hyphaema)
• contact lenses (remove before swelling occurs)
• eye movement–this may provide evidence of orbital floor fracture.
Pelvis and genitalia
Patients should be asked about pain and whether they have an urge to pass urine. Male patients should be examined for bruising, blood at the urinary meatus, priapism, and scrotal bruising/oedema. The presence of femoral pulses should be ascertained. If a digital rectal examination was not performed when the patient was log-rolled at the end of the primary survey, it should be carried out now. The assessor should look for blood in the rectum, which may indicate damage to the gut or pelvis. A high-riding prostate may be indicative of urethral injury, and loss of sphincter tone is often associated with spinal injury. Bony fragments may also be felt, indicating pelvic damage.
Extremities
Both arms and legs should be examined for contusion or deformity. Each should be assessed for:
Any injuries should be realigned and splinted. Every time this is done, the limb must be reassessed. Any open wounds should be covered with a sterile dressing. If at any time during the secondary survey a patient’s condition deteriorates, returning to the primary survey with institution or reinstitution of resuscitative measures is essential. The primary and secondary surveys should be repeated to ascertain any deterioration in the patient’s condition.
Trauma in children
Injury following an accident is the second leading cause of death in children (Greaves et al. 2009). The number of childhood deaths has declined over the past 30 years. This has been attributed to effective injury prevention strategies. Nurses may play a key role in this regard with effective advice and health promotion advice. Encouraging parents to provide children with cycle helmets being one such example.
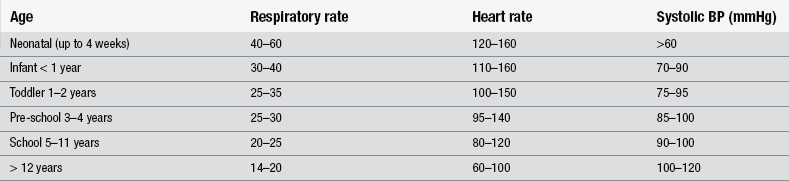
Whilst many of the principles for managing children are the same as for adults, it is essential that team members with paediatric experience are available. The priorities for assessment and management are identical. Some of the approaches to the care of the injured child will need to be modified, due to key differences in managing the seriously injured child (Table 2.5). The differences lie in children’s anatomy, physiology (Table 2.6) and emotional development. It can be difficult for the inexperienced to recognize early problems.
Table 2.5
Considerations required for primary survey in children
| Airway/cervical spine control | Children’s airways are more susceptible to obstruction. Cartilage in the larynx and trachea will be more pliable than in an adult, and the tongue is proportionally larger within the mouth Cervical spine control and assessment is particularly difficult in children, as they may be unable to communicate the presence or absence of any neck tenderness. Immobilization may also cause distress in the conscious child |
| Breathing | As with adults, 100 % oxygen is required via a non-rebreather mask. Signs of respiratory distress may be different, e.g., nasal flaring, intercostals recession, or grunting Tension pneumothorax in children is more common. It is crucial that these are detected and managed rapidly (Greaves et al. 2009) |
| Circulation | A stethoscope should be used to determine pulse rate in children less than 2 years old (RCN 2007) Early close monitoring is essential, as children may compensate for hypovolaemia better than adults, thus potentially hiding early clues of shock Vascular access may need to be via intraosseous routes (Resuscitation Council (UK) 2006) |
| Disability | A modified GCS is available for children under 5 years of age. This modifies the verbal response section, e.g., able to smile/interacts well to irritable or unresponsive |
| Exposure/control of environment | Children are at a higher risk of hypothermia due to their larger body surface area. Exposure for examination/intervention should be therefore kept to a minimum |
Greaves et al. (2009) recommend thorough preparation where the arrival of the injured child can be anticipated. Knowledge of the age of the child allows for a calculation of weight, drug dosages, fluid volumes and endotracheal tube sizes where appropriate. Children can sustain significant injury to the intrathoracic structures without evidence of any skeletal trauma. Children have not had the experience to develop the emotional coping strategies of adults. Particular attention should be paid to psychological considerations. This is particularly important where the child’s has been immobilized to protect their cervical spine. This may be terrifying for a child. If at all possible, someone known to the child is almost always a helpful support in the trauma room and should be given the opportunity to stay throughout the resuscitation.
Trauma in the older person
There are an increasing number of elderly trauma patients, not least because of demographic changes in the population (Greaves et al. 2009) (Table 2.7).
Table 2.7
Considerations required for primary survey in the older person
| Airway/cervical spine control | Degenerative changes make cervical spine injury more likely X-rays may be more difficult to interpret due to co-morbidities, e.g., osteoarthritic changes |
| Breathing | Decreased lung volume and compliance Co-existing respiratory conditions, e.g., COPD will exacerbate any increased requirement for oxygen following injury The thorax becomes less compliant making it more vulnerable to fracture |
| Circulation | Pre-existing cardiac conditions or vascular disease will compromise the body’s ability to compensate for hypovolaemic shock Vasoconstrictor response becomes slower with age. Medication, e.g., beta-blocker, may mask tachycardias or affect compensatory mechanisms to shock |
| Disability | Older patients are more likely to suffer with dementia or mental health problems making assessment of mental status very difficult |
| Exposure/control of environment | Delayed and decreased shivering response, decreased ability to produce heat and a slower metabolic rate will make the older patient more vulnerable to hypothermia. A structural and functional change in the skin increases the risk of the older patient developing pressure ulcers. This is a particularly important aspect of care that falls well within the sphere of nursing responsibility |
Definitive care
Once the trauma patient has been assessed using the ABCDE approach, has been successfully resuscitated and has undergone a head-to-toe assessment to find all injuries, they can be moved on to the next stage of care. Definitive care may be provided in the operating theatre, intensive care unit or a specialist treatment unit (e.g., burns care). Serious injuries are treated and definitive plans for the comprehensive care of the patient are made. It is essential the patient is in the best condition possible to undergo transfer either within the hospital or to another care facility. It is this aspect of trauma care that has seen the most significant recommendation in government policy and approach to major trauma in England. Following the development of a successful trauma network in London, a report from the National Audit Office (2010) has recommended extending the approach nationwide. The report indicates that the creation of trauma networks could improve patient outcome following serious injury.
The system draws on experience from the military and the US where seriously injured patients are met by highly trained specialists and managed in specialist care facilities where their injuries are definitively managed (Miller 2010). The most apt example of this may be the patient with a serious head injury, who is transported by helicopter from the scene of their injury, directly to a facility with a neurosurgical unit. Delay is minimized, optimizing potential recovery. A 20 % reduction in mortality from serious head injury has been demonstrated between the US and UK using this approach (Davenport et al. 2010).
Current recommendations (National Audit Office 2010) divide the UK into geographical regions, and within those regions will be a trauma network. The hospitals providing care are awarded a ‘level’ that determines the ability to manage the various specialities and facilities the seriously injured patient will require. Level 1 trauma centres, for example, will have an ED consultant doctor available 24 hours a day, have a helipad and have all surgical specialities that may be required. Level 2 centres may have 24-hour ED facilities but may lack the specialities required. Level 3 centres may lack the specialities required and the ability to provide 24-hour CT scanning, for example (Miller 2010). Each regional trauma network would have one level 1 centre and several level 2 and 3 centres.
Family members and loved ones should be kept fully informed of the proceedings. The distress experienced by this group of people during resuscitation can be far longer lasting than that experienced by the patient. If possible, someone should be allocated to liaise between the resuscitation room and relatives. Although the nurse may be the ideal person, chaplains, social workers, or staff from other areas of the hospital can often assume this role. Relatives can provide important information, and they should be included in patient care planning. Inviting relatives into the trauma room is appropriate in some instances (Royal College of Nursing & British Association for Accident and Emergency Medicine 1995, Barratt & Wallis 1998, Nykiel et al. 2011, Barratt & Wallis 1998). (See also Chapter 14: Care of the Bereaved.)
Psychological aspects
Most of the resources associated with trauma management in terms of funding, education, and research are directed towards physiological and life-threatening aspects. However, some of the more lasting effects are from the emotional damage trauma has inflicted on patients and their relatives (Larner 2005).
Conclusion
A great deal of progress has been made over the last two decades, but there still remains a great deal to do. In the past, trauma patients have died as the result of relatively simple problems such as hypovolaemia and hypoxia. Many of us are now aware of ways to prevent such deaths. However, it is essential that all those who come into contact with trauma patients have the necessary skills and knowledge. Investment in training of this nature is a small price to pay for a reduction in trauma deaths.
References
Adam, S., Osborne, S. The systemic inflammatory response, sepsis and multiple organ dysfunction. In: Critical Care Nursing – Science and practice. Oxford: Oxford University Press; 2009.
American College of Surgeons. Advanced Trauma Life Support, eighth ed. Chicago: American College of Surgeons; 2008.
Barratt, F., Wallis, D.N. Relatives in the resuscitation room: their point of view. Journal of Accident and Emergency Medicine. 1998;15:109.
Casey, G. Oxygen transport and the use of pulse oximetry. Nursing Standard. 2001;15(47):46–53.
Champion, H.R., Leitch, R.A. Combat casualty management. In: Lenquist S., ed. Medical Incident Response to Major Incidents and Disasters. Berlin: Springer-Verlag, 2012.
Cole, E. Assessment and management of the trauma patient. Nursing Standard. 2004;18(41):45–51.
Cooke, M.W. Use of the spinal board within the accident and emergency department. Journal of Accident and Emergency Medicine. 1998;15:108–109.
Davenport, R., Tai, N., West, A., et al. A major trauma centre is a speciality hospital not a hospital of specialities. British Journal of Surgery. 2010;97(1):109–117.
Dickinson, M. Understanding the mechanism of injury and kinetic forces involved in traumatic injuries. Emergency Nurse. 2004;12(6):30–35.
Duncan, N., Moran, C. Initial resuscitation of the trauma victim. Orthopaedics and Trauma. 2009;21(1):1–8.
Geeraedts, L., Kaasjager, H., van Vugt, A., et al. Exsanguination in trauma; A review of diagnostics and treatment options. Injury: International Journal Care of the Injured. 2009;40:11–20.
Greaves, I., Porter, K., Garner, J. Trauma Care Manual, second ed. London: Hodder Arnold; 2009.
Hoffman, J., Mower, W., Wolfson, A., et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-radiography Utilisation Study Group. New England Journal of Medicine. 2000;343:94–99.
Hunt, P., Hunt, F. Fluid resuscitation therapy. In: Smith J., Greaves I., Porter K., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford Medical Publications, 2011.
Ireland, S., Endacott, R., Cameron, P., et al. The incidence and significance of accidental hypothermia in major trauma: A prospective observational study. Resuscitation. 2011;82(3):300–306.
Larner, S. Common psychological challenges for patients with newly acquired disability. Nursing Standard. 2005;19(28):33–39.
Little, G., Kelly, M., Glucksman, E. Critical pitfalls in the immediate assessment of the trauma patient. Trauma. 2001;3:43–51.
Lott, C., Araujo, R., Cassar, M., et al. The European Trauma Course (ETC) and the team approach: Past, present and future. Resuscitation. 2009;80:1192–1196.
Middleton, P. The Trauma Epidemic. In: Smith J., Greaves I., Porter K., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford Medical Publications, 2011.
Miller, S. How trauma networks can improve patient care. Emergency Nurse. 2010;18(6):14–18.
National Audit Office. Major Trauma Care in England. London: The Stationery Office; 2010.
Nykiel, L., Denicke, R., Schneider, R., et al. Evidence-based practice and family presence: paving the path for bedside nurse scientists. Journal of Emergency Nursing. 2011;37(1):9–16.
Resuscitation Council (UK). European Paediatric Life Support. London: Resuscitation Council (UK); 2006.
Resuscitation Council (UK). Resuscitation Guidelines 2010. London: Resuscitation Council; 2010.
Robertson, L.C., Al-Haddad, M. Recognizing the critically ill patient. Anaesthesia and Intensive Care Medicine. 2013;14(1):11–14.
Sapsford, W. Should the ‘C’ in ‘ABCDE’ be altered to reflect the trend towards hypotensive resuscitation. Scandinavian Journal of Surgery. 2008;97:4–11.
Schierhout, G., Roberts, I. Fluid resuscitation with colloid or crystalloid solutions in critically ill patients. British Medical Journal. 1998;316(7136):961–964.
Sexton, J. Trauma epidemiology and team management. Emergency Nurse. 1997;5(1):14–16.
Smith, R.M., Conn, A. Pre-hospital care: Scoop and run or stay and play? Injury, International Care of the Injured. 2009;4054:S23–S26.
Span, D.R., Cerny, V., Coats, T.J., et al. Management of trauma following major trauma: A European guideline. Critical Care. 2007;11:R17.
Stoneham, J., Riley, B., Brooks, A., et al. Recent advances in trauma management. Trauma. 2001;3:143–150.
Swartz, C. Resuscitation considerations to prevent pressure ulcers in trauma patients. International Journal of Trauma Nursing. 2000;6:16–18.
Waterhouse, C. The use of painful stimulus in relation to Glasgow Coma Scale observations. British Journal of Neuroscience Nursing. 2009;5(5):209–214.