Ophthalmic emergencies
Introduction
A significant proportion, generally around 6 % of the workload of the Emergency Department (ED), is made up of patients with ophthalmic problems (Ezra et al. 2005). Tan et al. (1997) found a lack of basic ophthalmic training for ED Senior House Officers leading to a lack of confidence on their part in the management of eye emergencies. This lack of confidence on the part of junior doctors is reflected in the nursing teams of many EDs, although Ezra et al. (2005) found that nurses were significantly more accurate than junior doctors in their assessment of ED patients, and combined with the apparent health of many ophthalmic patients, can lead to inappropriate management in the ED.
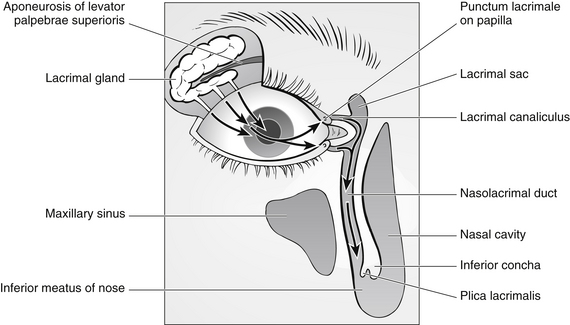
Anatomy and physiology of the eye (Fig. 31.1)
Eyelids
The lids are layered structures covered on their outer surfaces by skin and on their inner surfaces by conjunctiva (Fig. 31.2). In between is subcutaneous tissue, the orbital septum of which thickens within the lids to form fibrous tarsal plates that give structure to the lid. The upper lid contains the levator muscle and the lower contains the inferior tarsal muscle, which retracts it. The lids are maintained in position by the medial and lateral canthal tendons that attach to the periosteum. The lids are closed by the orbicularis muscle.
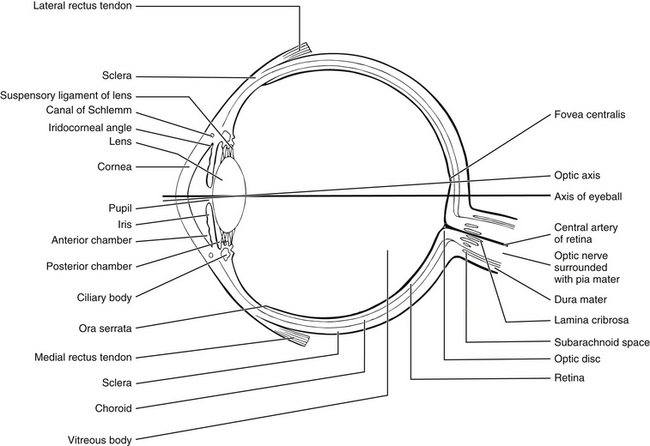
Figure 31.1 Basic structure of the eye.
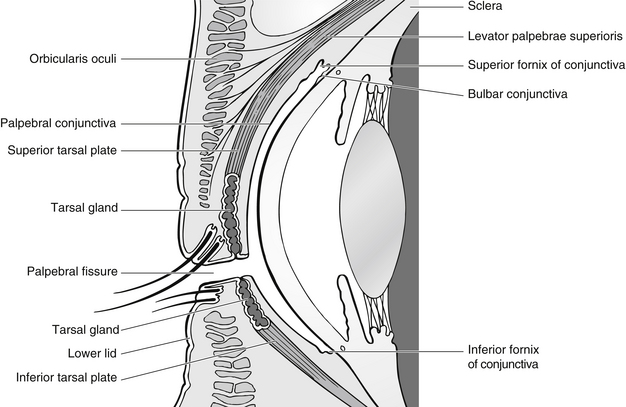
Figure 31.2 Lids and conjunctival fornices.
Lacrimal system
The tear film is composed mainly of watery fluid from the lacrimal gland (99 %), which is situated in the lacrimal fossa of the frontal bone in the orbit. The other important components of the tear film are mucin from the conjunctival goblet cells and oil from the Meibomian (tarsal) glands and the glands of Möll and Zeiss. The tear film is distributed over the surface of the eye by gravity, capillary action of the puncta and canaliculi and the eyelids. The tears leave the eye by evaporation and by way of the puncta, the upper of which takes around 30 % of the unevaporated tears and the lower around 70 %. From the puncta, the tears flow into the canaliculi, into the common canaliculus and then into the lacrimal sac and through the nasolacrimal duct (Fig. 31.3).
Cornea
The transparent cornea forms the anterior one-sixth of the globe. Its curvature is higher than that of the rest of the globe and it is the main structure responsible for the refraction of light entering the eye. It is an avascular structure which is nourished by the aqueous humour, the capillaries at its edge and from the tear film. Microscopically, it consists of five layers:
• the epithelium – consists of five layers of cells centrally, ten or more at the limbus. Running between the cells are the nerve endings of sensory nerve fibres, which are sensitive mainly to pain. The epithelium regenerates by the movement of cells from the periphery towards the middle
• Bowman’s layer – is acellular and consists of collagen fibres
• substantia propria or stroma – comprises 90 % of the thickness of the cornea. It is transparent and fibrous, and is made up of lamellae of collagen fibres arranged parallel to the surface. This arrangement ensures corneal clarity
• Descemet’s membrane – a strong membrane which is the basement membrane of the endothelium
• endothelium – a single layer of flattened cells which plays a major role in controlling the hydration of the cornea by a barrier and active transport method. Loss of endothelial cells leads to corneal oedema and lack of clarity.
The uveal tract
The ciliary body is continuous with the choroid and the margin of the iris. It contains the ciliary muscle used to change the shape of the lens during accommodation. Its outer, pigmented layer is continuous with the retinal pigment epithelium. Its inner, non-pigmented layer produces aqueous humour. The lens attaches to the ciliary body by a suspensory ligament whose fibres are known as zonules.
Assessing ophthalmic conditions
• how long the patient has had symptoms for and whether they are getting worse
• rapidity and mode of onset (Box 31.1)
• is vision reduced and to what degree?
• degree, type and location of pain
• is there any discharge, watering or photophobia?
• has the patient had this, or a similar problem before?
Discussion of systemic problems and medication is important as it can point to possible ophthalmic problems. For example, there is a link between ankylosing spondylitis and uveitis, and a link between rheumatoid arthritis and dry eyes, and there are many ophthalmic side-effects of systemic drugs. The assessing nurse needs to investigate any pre-existing ophthalmic or other medical conditions. Of particular importance are conditions such as glaucoma, iritis (uveitis) and blepharitis; systemic conditions such as diabetes and rheumatoid arthritis; and any drug therapy, as all of these may affect the health of the eye.
Visual acuity
The number for this line is indicated on the Snellen chart, just above or just below the letters. If part of a line only is read, this may be recorded as the line above plus the extra letters, or the line below minus the missed letters. For example, if the patient reads the ‘12’ line except for one letter, at 6 m, it should be recorded as 6/12 – 1.
• using a recognition chart so that the patient may match letters or shapes
• obtaining the services of an interpreter or family member to translate for the patient
• with children, using picture tests such as the Kay picture test and making the procedure into a game – this will usually encourage greater cooperation.
Patients who are in pain should have a drop of topical anaesthetic instilled so that any corneal pain is alleviated and the patient can cooperate more fully with the procedure, thus achieving an accurate visual acuity. Patients sometimes feel that this is a test that they have to pass and ‘cheat’ by looking through their fingers etc. It should be explained that the nurse is attempting to obtain an accurate assessment of their vision and that it is important that they are not tempted to make it seem better than it really is.
Examining the eye
Eye examination must be systematic. It is very easy to assume a diagnosis from the history and, in that way, miss less obvious problems. The eye should be examined from the ‘outside’ – the eye position and surrounding structures – working ‘in’ to consider the globe itself. Considerations for a thorough eye examination are given in Box 31.2.
Equipment to aid assessment
Fluorescein drops or strips that stain damaged epithelial tissue are useful in examining abrasions. The stain is inserted and then the eye is viewed through a cobalt blue filter, as a penlight attachment, slit lamp or ophthalmoscope filter. While slit lamps (a binocular microscope for eye examination) offer the optimum provision for examination, they are expensive and not vital to initial assessment. Topical anaesthetic, such as tetracaine 1 % or oxybuprocaine 0.4 %, should be available in single-dose applications for pain relief and to facilitate examination. Proxymetacaine stings less on initial application and may be preferable, especially in children (Andrew 2006).
Contact lenses
If the patient is wearing contact lenses, the lens should be removed from the injured eye or from both eyes if inflammation or swelling is present. If possible, the patient should remove his own lens; each contact lens wearer develops his own way of doing it.
Removal of lenses
To remove hard lenses, the nurse should stretch the skin of the eyelid by pulling gently in a lateral direction from the outside corner of the patient’s eye. Once the skin is stretched, the nurse should push the upper and lower lids together using a finger from each hand. This movement catches the edges of the lens and breaks its suction to the cornea. Once this happens, the lens will fall out (Fig. 31.4). Alternatively, the nurse could put a (washed) index finger on the lens and gently move away from the cornea. The lids can then be used to lever the edge of the lens away from the cornea, and as the adhesion to the cornea breaks, the lens can be gently removed (Shaw et al. 2010).
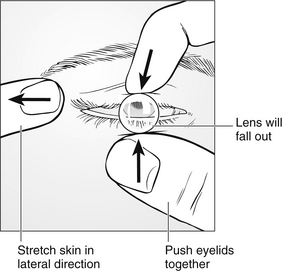
Figure 31.4 Removal of hard contact lenses.
Removal of soft lenses is demonstrated in Figure 31.5.
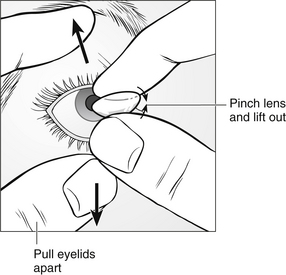
Figure 31.5 Removal of soft contact lenses.
Triage decisions
Similar to other illness and injury, ophthalmic conditions vary considerably in severity and urgency. Using the Manchester Triage Group guidelines (Mackway-Jones et al. 2005) eye complaints can be prioritized as follows:
• priority one (red) – acute chemical eye injury; failure to act to dilute or neutralize chemical agents results in increased tissue damage and can lead to vascular damage and ischaemia and is therefore sight-threatening
• priority two (orange) – severe pain, penetrating eye injury or acute complete loss of vision; these presentations have the potential to be sight-threatening or result in further damage if not treated promptly
• priority three (yellow) – moderate pain, reduced visual acuity or inappropriate (where the history does not explain the findings as this can be an indication of a safeguarding issue)
• priority four (green) – recent mild pain, red eye, foreign body sensation, diplopia, recent problem/injury
• priority five (blue) – chronic complaint without acute exacerbation.
Ocular burns
Ocular burns may be divided most commonly into chemical, thermal and radiation (UV) burns.
Chemical burns
These are the most urgent category of ocular burns and causes may include alkalis, acids or solvents. Alkali burns are caused by substances such as sodium or potassium hydroxide, used as cleaning agents; calcium hydroxide, found in plaster and mortar; and ammonia, which is found in fertilizer and used in liquid form. Alkalis rapidly penetrate corneal tissue, combining with lipids in cell membranes, which results in cell disruption and tissue softening. A rapid rise in the pH in the anterior chamber may damage intraocular structures, and damage to vascular channels leads to ischaemia. Acids are less penetrating, and most damage is done during and soon after exposure. Acid substances combine with tissue, forming barriers against deeper penetration and localizing damage to the point of contact, although they can still be devastating. Acid burns are often due to car battery (sulphuric) acid or more complex organic and inorganic compounds. Solvent burns, although very painful, usually cause only transient irritation and damage. Thermal and/or contusion injuries due to the temperature or pressure of the chemical may be superimposed on the chemical injury (Marsden 1999a).
Primary management
A prompt and effective response to a chemical injury is vital to minimize tissue damage. One of the main determinants of ultimate outcome is duration of contact (Waggoner 1997), and as Glenn (1995) suggested, the initial treatment given by the nurse in the case of chemical eye injury may have more impact on the final vision than any subsequent care by the ophthalmologist.
Irrigation: The initial treatment of acute chemical injury involves copious irrigation to dilute the chemical and remove particulate matter. Irrigation should commence immediately, using whatever source is available and no time should be wasted in trying to find out what chemical was splashed into the eye (Marsden 2009). In a multi-centre trial, Moscati et al. (2007) found no difference in the efficacy of irrigation fluids and therefore, in the ED, the irrigating fluid of choice is normal saline (0.9 %) administered via a giving set to provide a directable and controllable jet. Sterile water is also used. The eyelids should be held open and contact lenses removed. A drop of topical anaesthetic should be instilled prior to irrigation to assist in patient compliance and minimize pain. All aspects of the cornea and conjunctiva (exposed by everting the upper lid) should be thoroughly irrigated. All particulate matter should be removed, by wiping with a cotton-tipped applicator if necessary.
Any delay in irrigation adds to the contact time and increases the risk of more severe injury. It is best to assume that any previous irrigation is inadequate and carry out adequate irrigation when the patient presents, unless a significant time has elapsed (hours) between injury and presentation. Specific irrigation time and fluid volume depend on the nature of the chemical and its physical state as well as the patient’s condition. Waggoner (1997) suggested that it is impossible to over-irrigate a chemically injured eye and recommended irrigation for 15–30 minutes and one to two litres of saline is generally sufficient.
The use of pH paper to check for adequate irrigation may be debated. In alkaline injury in particular, the chemical leaches out of the eye for a number of hours after injury, thus altering the pH. Delay in therapy of a number of hours until the pH is back to normal will delay healing. It is useful though if used before irrigation to determine the type of chemical involved and again later to check any progress in returning to a normal pH. When measured by sensitive experimental methods, normal pH of the conjunctival sac is 6.5–7.6 (Forrester et al. 1996) but when measured by touching pH measuring paper to the conjunctiva, it is most often near 8 (Adler et al. 1968). It must be remembered that a chemical may have a neutral pH and still cause injury. Ultimately then, indicator paper is no substitute for adequate irrigation. Following irrigation, the patient’s visual acuity should be checked.
Acute chemical eye injury is defined by Mackway-Jones et al. (2005) as injury by chemicals occurring in the last 24 hours. While this is true, and places the patient into a red triage category, this should lead to immediate further assessment rather than immediate irrigation. If there is still particulate chemical material in the eye after 24 hours, then it needs irrigation, but small amounts of liquid will have been irrigated by profuse tearing over that period of time and if a period of a few hours has elapsed between chemical exposure and presentation to an ED, and the pH of the conjunctiva is between 7 and 8 at initial assessment, there is little need for irrigation. After irrigation, pH should not be expected to be 7 and is more likely to stabilise around 8 (Sharma et al. 2006).
Ophthalmic management: All but the most trivial chemical injuries should be referred to an ophthalmologist. The eye may look deceptively normal due to tissue blanching and ischaemia, which needs urgent assessment and treatment.
Thermal burns
These usually involve damage to the lids and are often associated with facial burns. Treatment is similar to that of thermal burns elsewhere on the body. Thermal burns range from very mild corneal injury which may be treated as an abrasion, with dilatation of the pupil and chloramphenicol ointment, to devastating injury such as that caused by molten metal which may require reconstruction of the globe and surrounding structures. Thermal burns involving the lids should be referred due to the possibility of aberrant healing, leading to lid closure and mobility problems (see also Chapter 11).
Penetrating trauma
• disruption of the ocular tissues at the time of injury
• scar tissue formation (corneal, disrupting vision, retinal detachment caused by contracting scars inside the eye)
• reaction of the eye to foreign bodies – from organic material introducing infection or inflammation and from the deposition of pigments caused by degrading metal foreign bodies.
Large penetrating eye injuries are very obvious, but small perforations may be easily missed. The eye may look intact if the perforation is small and the wound may be sealed by iris tissue. It is very important, therefore, that a systematic eye examination is carried out and the particular circumstances of the incident are ascertained (Marsden 1996, 2009). Corneal perforations always leave a full-thickness scar, even if it is very small. Scleral perforations may be masked by overlying subconjunctival haemorrhage.
Poor prognostic factors associated with globe loss include a wound larger than 10 mm, injuries that involve the retina, initial visual acuity of less than 5/200 at time of injury, no light perception at the time of injury, pellet mechanism of injury, injuries from blunt objects (Ehlers et al. 2008, Lemley et al. 2008, Abrames & Folio 2012).
Lid trauma
The eyelids must be intact, in the correct position and without any disruption to their structure and function in order that the eyes are protected effectively. Repair of lid trauma may be a planned activity rather than an emergency procedure due to the good vascularization of the lids and associated structures. Lid trauma, unless very superficial, should be referred to ophthalmologists, who are best able to achieve the necessary functional and cosmetic results for the patient.
Major closed trauma
• traumatic mydriasis or miosis
• posterior segment problems such as retinal oedema (commotio retinae), choroidal rupture and retinal detachment
• blow-out fracture of the orbital floor or nasal wall
Patients with reduced vision following blunt trauma should be referred to an ophthalmologist.
Ecchymosis
Ecchymosis is more commonly known as a ‘black eye’. It results from a blow to the orbit that leads to bruising and oedema of the eyelids. In itself, it is a relatively minor injury, treated with ice packs to relieve swelling. The force needed to cause this sort of injury may cause contusion or concussion injuries to any or all of the structures within the eye, as well as orbital rim or floor fractures. It is important, therefore, that the eye and surrounding structures are assessed carefully. The patient may be able to assist in opening the lids enough for the clinician to be able to assess the eye. This kind of injury is common is some sports, such as rugby and squash, however, nearly 90 % of all sports-related eye injuries can be prevented with adequate eye protection (Cass 2012).
Hyphaema
Traumatic hyphaema may only be detectable with a slit lamp, when red blood cells may be seen floating in the anterior chamber, or alternatively it may be visible with the naked eye, when blood may fill the whole of the anterior chamber. Its presence usually indicates significant intraocular trauma (Woodcock 2009). The signs and symptoms of hyphaema are:
• reddish haze present diffusely through the anterior chamber, a settled layer of blood inferiorly or complete filling of the anterior chamber
• pain – due to raised intraocular pressure and other eye injury
Admission may be necessary in the treatment of hyphaema in children, and in the treatment of large hyphaema with raised intraocular pressure in adults, but is rare and generally patients are advised to rest at home. Daily intraocular pressure monitoring by an ophthalmologist is usual, and treatment with agents such as acetazolamide, glycerol or mannitol may be indicated if the intraocular pressure is raised.
Luxation or subluxation of the lens
A patient with a total dislocation of the lens or a partial dislocation (subluxation) can also present to the ED. It may be the result of trauma, hereditary, or associated with certain syndromes, such as Marfan’s syndrome (Shaw et al. 2010). Vision will be disturbed, but the degree of visual disturbance will depend on the degree of dislocation. If 25 % or more of the zonules of the lens are ruptured, the lens is no longer held securely behind the iris. The signs and symptoms of luxation or subluxation of the lens are:
• deepening of the anterior chamber due to tilting of the lens posteriorly – the anterior chamber may be shallow if the lens moves anteriorly
• pupil block – this may occur if the lens occludes the pupil
The patient should be referred to an ophthalmologist. In general, if no complications occur dislocated lenses are best left untreated. If complications do occur, such as raised intraocular pressure, these are treated before lens extraction is attempted, as surgery in these instances is difficult.
Traumatic mydriasis or miosis
This may be present after blunt trauma. Additionally, the pupil may react only minimally to light, or not at all, and may have an irregular shape. This deformity is indicative of complete or partial rupture of the iris sphincter. It may be permanent or transient.
Orbital fractures
Orbital floor fractures
These are often referred to as ‘blow-out fractures’ and are produced by transmission of forces through the bones and soft tissues of the orbit by an object such as a ball or fist. They typically may be found in young patients in their teens and twenties and may not be clinically obvious. Diplopia, nausea, and vomiting with no subconjunctival haematoma in a young patient requires immediate referral (Lynham et al. 2012). Fractures may be complicated by fat and muscle entrapment which limits ocular motility, causing double vision. They are often found by plain X-rays, but CT scans are used to investigate them further. Symptoms resolve without surgery in almost 85 % of patients, as oedematous tissues usually settle, freeing muscles and allowing correct motility (Egging 2009). Visual loss following trauma has a poor prognosis for recovery; however, evolving loss may be indicative of retrobulbar haemorrhage and is potentially treatable (Mackenzie & Gibbons 2011). Signs and symptoms of orbital floor fracture include:
A sentinel presentation is that the patient attends the ED stating that he has had a blow to the eye and when he blew his nose, his eyelids swelled hugely. This indicates a facture between orbit and sinus and air blown into orbital tissues from the sinus. Antibiotics are indicated to prevent orbital infection from contaminated air from the sinus.
Orbital apex trauma and optic nerve injury
Optic nerve injury may occur, often due to traumatic optic neuropathy from indirect trauma (such as fractures of the base of the skull). The nerve may be compressed by haematoma, damaged by foreign body or fracture, resulting in anything from minor trauma to the nerve to transection. Injury to the cranial nerves present in the orbit will present as double vision in injury to the III, IV and VI nerves and as sensory disturbance to the areas supplied by the trigeminal nerve (V). Visual acuity should be checked repeatedly in this group of patients and any reduction should prompt immediate referral to an ophthalmologist (Marsden 2006).
Minor trauma
Corneal abrasion
Eye pain is difficult to control. The pain associated with a breach in the corneal epithelium has a component of ciliary muscle spasm which can be relieved, along with a degree of the patient’s pain, by the use of a dilating drop such as cyclopentolate 1 %. Topical non-steroidal anti-inflammatory (NSAI) drops provide a significant degree of effective pain relief for patients with corneal pain and are usually prescribed four times daily (Brahma et al. 1996).
Any breach in the corneal epithelium places the eye at risk of infection. A prophylactic antibiotic is necessary and chloramphenicol is usually the antibiotic of choice. Short courses of topical chloramphenicol do not appear to cause systemic side-effects (McGhee & Ananstas 1996) and it is considered to be a very safe drug, widely used throughout ophthalmology in the UK. In the treatment of corneal abrasions, this is often prescribed in ointment form, as this provides a lubricant layer over the eye that enables the lid to slide over the damaged epithelium, and is therefore much more comfortable for the patient. As the antibiotic is for prophylaxis rather than treatment of infection and the ointment base is for comfort, there is no need to prescribe a ‘course’ of antibiotics. When the abrasion is healed, the patient will know as the pain will have resolved. At that point, the antibiotic treatment may be stopped. Corneal abrasions generally heal within 48–72 hours. Abrasions which appear slow to heal or involve loose epithelium should be referred to an ophthalmologist.
In some instances, the cornea is at particular risk of infection, slow healing or recurrent abrasion. This is particularly the case in human, animal or vegetable material scratches. It is important, therefore, that the patient uses the antibiotic ointment at night for a period of 3–4 weeks to prevent this occurring. Follow-up visits are not usually necessary unless the abrasion is particularly large, involves the deeper layers of the cornea or the patient is a child. The patient should be reassured that a corneal abrasion usually heals and pain relief occurs within 24–48 hours (Kumar et al. 2012).
Subtarsal foreign body
In this case, the patient often presents with a foreign-body sensation and a history of something falling or blowing into the eye. Management involves everting the upper lid using a moistened cotton-tipped swab. Any foreign material trapped underneath the lid may be wiped off with the swab. The eye should then be stained with fluorescein to rule out any corneal abrasion. If corneal abrasions are present, they are often linear, superficial and quite characteristic of this type of injury. If the corneal injury is minimal, a stat dose instillation of antibiotic ointment is usually sufficient. If larger abrasions are present, they should be treated as corneal abrasions.
Corneal foreign body
These commonly occur from grinding wheels and other industrial machines, from DIY and even windborne materials. The patient may present with a foreign-body sensation, especially when opening or closing the eye. The final resting place of an intraocular foreign body, and the damage caused by it depend on the size, shape and moment of the object at the time of impact and the momentum of the object at the time of impact, and the site of ocular penetration (Scott 2011). Superficial foreign bodies are often easily removed with a moistened cotton bud after instillation of topical anaesthetic. Dry cotton buds should not be used as they can stick to the corneal epithelium, which is moist, and this may result in a large abrasion, complicating the injury.
Eye pads
There is no evidence that padding the eye enhances healing; however, for many patients, padding can make the eye much more comfortable. The decision to pad the eye of a patient with a corneal abrasion should therefore be accompanied by the advice that if the pad makes the eye more comfortable, it can be left in place, without disturbance for 24 hours and then removed and antibiotic treatment commenced. If the pad makes the eye less comfortable, it may be removed and antibiotic ointment commenced immediately. In this way, those patients who can be helped by padding are, and others are not made worse by the indiscriminate application of eye pads (Marsden 2006).
A single pad will not keep the eye closed and further damage to the cornea may be caused by the surface of the pad. If padding is required, the following method should be used. Fold one pad in half and place over the closed eyelids after instilling the necessary medication. Place the second pad, flat, over the first and secure with two or three pieces of tape (Fig. 31.6). It is unnecessary to pad an eye merely because topical anaesthetic has been used. Anaesthetic drops last for only around 20–30 minutes and the risk of the patient sustaining any further injury because of the topical anaesthetic drop is minimal (Cheng et al. 1997).
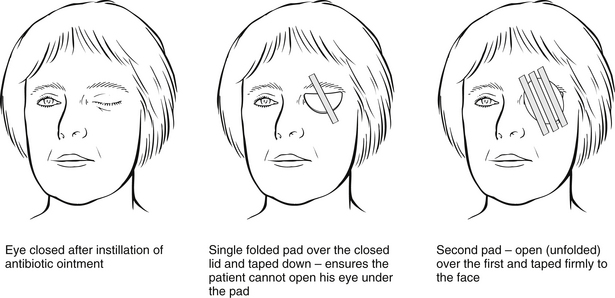
Figure 31.6 Use of eye pads.
The ED nurse should not pad the eye of a patient who is driving home. If the patient leaves the eye pad on and drives anyway, he is breaking the law, invalidating his insurance and is a danger to other road users. A drop of topical anaesthetic will facilitate driving home safely and the patient may then pad the eye at home.
Eye drops
Topical anaesthetic drops are a valuable tool for examination purposes. They ‘magically’ remove all the patient’s pain and he may be very keen to have some to take home so that this pain-free state may continue. Unfortunately, topical anaesthetic drops also inhibit epithelial healing. The patient will be pain-free, but the epithelial defect will not heal (Andrew 2006).
Topical non-steroidal anti-inflammatory drugs (NSAIDs) have been evaluated for use in corneal pain (Brahma et al. 1996) and found to be extremely useful. Their use does not appear to delay healing and no adverse effects have been found. A number of NSAIDs are available in eye drop form, including diclofenac sodium, flurbiprofen sodium and ketorolac trometamol.
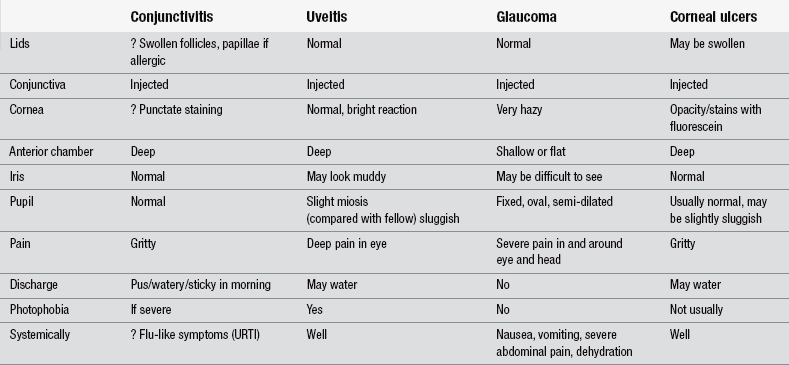
Red eye
Ophthalmic trauma is fairly easy to recognize with the aid of a history and a brief eye examination. However, ophthalmic medical problems are, on the whole, less easily diagnosed and therefore may be dealt with less well than other problems. The differential diagnosis of the red eye (Marsden 2006) is shown in Table 31.1.
Blepharitis
This chronic eyelid condition is very common. The patient is likely to present with gritty, sore eyes and red-rimmed eyelids with crusting, which may be mild to very severe, along the lid margin – the lash line. Treatment involves regular lid cleaning, using a cotton bud dipped in a solution of baby shampoo and water to ‘scrub’ the lid margin along the lash line to remove all the crusts. When the condition is acute, antibiotic ointment should be rubbed into the lid margin after lid hygiene two to four times a day. As this is a chronic condition, lid cleaning should continue even after the symptoms have resolved, or the condition will recur. Occasionally, punctate staining may occur at the corneoscleral junction. This is marginal keratitis, an inflammatory change. The patient should be referred to an ophthalmologist.
Conjunctivitis
Inflammation of the conjunctiva is by far the most common cause of red eyes. Bacterial conjunctivitis in adults is uncommon (Tullo & Donnelly 1995) and most conjunctivitis in adults is viral. Conjunctivitis in children is more likely to be bacterial.
Bacterial conjunctivitis
Health education information, particularly on how to control the spread of infection, should be given and the nurse must ensure that the patient understands how to use his medication before leaving the ED. Information on how to keep the lids clean and free from discharge may be needed, e.g., using cooled, boiled water and cotton wool or tissues, especially by parents of small children who may also need extra help instilling the prescribed medication effectively. Patient education should also, where appropriate, incorporate discussion of cross-contamination through eye makeup, pillows and towels (Egging 2009).
Viral conjunctivitis
Viruses, often types of adenovirus, are by far the most common cause of conjunctivitis in adults (Kaufman 2011). Once again, the patient is likely to complain of a gritty sensation, but the discharge is much less likely to be purulent than profuse watering, with stickiness often only in the morning when the watery discharge has dried and the lids are stuck together. If the lid is everted, the conjunctiva covering it will appear very bumpy rather than smooth. These ‘bumps’ are follicles and are inflamed lymphoid tissue. This roughness of the conjunctiva is what makes the eye feel so gritty and irritable. The patient with viral conjunctivitis often complains of dryness, along with a watery eye. The tears, although profuse, are inadequate in quality and dry up very quickly; the eye responds to the irritation and dryness by producing more. There may be punctate erosions on the cornea when stained with fluorescein.
Allergic conjunctivitis
The second allergic presentation is an acute and frightening atopic reaction that involves massive swelling of the conjunctiva (chemosis) which the patient often describes as ‘jelly’ on the eye. This is usually due to the patient rubbing the eye with an allergen present on the hand or finger. Common allergens include some plant juices and cat hairs, although it is unlikely that the particular allergen will be identified. This condition is completely self-limiting and requires no treatment unless the chemosis is severe and protruding from the closed lids. In this case, lubricant drops may be helpful to prevent drying. Adequate reassurance is needed and, if the reaction is severe, the patient may need to be monitored for systemic effects of the allergen.
Anterior uveitis (also known as uveitis, iridocyclitis, iritis)
Uveitis is an inflammatory condition of part or all of the uveal tract (iris, ciliary body and choroid) (McDonald et al. 2012). It may be associated with systemic disease such as ankylosing spondylitis but which is often idiopathic. It may also occur secondary to trauma. The most common presentation is anterior uveitis (inflammation of iris and ciliary body, also commonly known as iritis). Common presenting symptoms are photophobia, pain due to iris and ciliary spasm, conjunctival redness (injection), which may be more marked around the corneoscleral junction (limbus), and decreased visual acuity. The reduction in vision is due to protein and white blood cells (part of the inflammatory response) in the anterior chamber. The pupil, because of spasm and inflammation, is likely to be small (miosed) compared with the unaffected eye and may react sluggishly. There will be a clear reflection of light when a light is shone onto the cornea, demonstrating the lack of corneal involvement, and there will be no staining with fluorescein. Prompt referral to an ophthalmologist is required and treatment is with topical corticosteroids, and mydriatics to dilate the pupil to reduce inflammation and prevent adhesions of the iris and lens.
Health promotion
Many activities in the home and workplace cause eye injuries, due to equipment, materials, chemicals and radiation. Patients with such injuries should be encouraged to wear eye protection or to check that any equipment already in use is of a suitable standard. All eye protection should conform to British Standard BS 2092 requirements. Children, in particular, are vulnerable to eye injuries. Parents need sympathetic health education to minimize the risks of sight-damaging injury (Kutsche 1994).
References
Abrames, F., Folio, L. CT severity spectrum of penetrating eye injuries from blasts. Military Medicine. 2012;177(2):169–173.
Adler, I.N., Wlodyga, R.J., Rops, S.J. the effects of pH on contact lens wearing. Journal of American Optomotrists Association. 1968;39:1000–1001.
Andrew, S. Pharmacology. In: Marsden J., ed. Ophthalmic Care. Chichester: Wiley, 2006.
Brahma, A.K., Shah, S., Hillier, V.F., et al. Topical analgesia for superficial corneal injuries. Journal of Accident and Emergency Medicine. 1996;13:186–188.
Cass, S.P. Ocular injuries in sports. Current Sports Medicine. 2012;11(1):11–15.
Cheng, H., Burdon, M.A., Buckley, S.A., et al. Emergency Ophthalmology. London: BMJ; 1997.
Egging, D. Ocular emergencies. In Newberry L., ed.: Sheehy’s Emergency Nursing: Principles and Practice, sixth ed, St Louis: Mosby, 2009.
Ehlers, J.P., Kunimoto, D.Y., Ittoop, S., et al. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. American Journal of Ophthalmology. 2008;146(3):427–433.
Ezra, D.G., Mellington, F., Cugnoni, H., et al. Reliability of opthhalmic accident and emergency referrals: a new role for the emergency nurse practitioner? Emergency Medicine Journal. 2005:696–699.
Forrester, J., Dick, A., McMenamin, P., et al. The Eye: Basic Sciences in Practice. London: WB Saunders; 1996.
Glenn, S. Care of patients with chemical eye injury. Emergency Nurse. 1995;3(3):7–9.
Kaufman, H.E. Adenovirus advances: new diagnostic and therapeutic options. Current Opinion in Ophthalmology. 2011;22(4):290–293.
Kumar, K., Dodds, C., Gayer, S. Ophthalmic Anaesthesia. Oxford: Oxford University Press; 2012.
Kutsche, P.J. Ocular trauma in children. Journal of Ophthalmic Nursing and Technology. 1994;13(3):117–120.
Lemley, C.A., Wirostko, W.J., Mieler, W.F., et al. Intraocular foreign bodies. In: Albert D.M., ed. Principles and Practice of Ophthalmology. Philadelphia: Saunders, 2008.
Lynham, A., Tuckett, J., Warnke, P. Maxillofacial trauma. Australian Family Physician. 2012;41(4):172–180.
Mackenzie, N., Gibbons, A. Maxillofacial fractures. In: Smith J., Greaves I., Porter K., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford Medical Publications, 2011.
Mackway-Jones, K., Marsden, J., Windle, J. Emergency Triage, second ed. London: BMJ; 2005.
Marsden, J. Ophthalmic trauma in accident and emergency. Accident and Emergency Nursing. 1996;4(1):54–58.
Marsden, J. Ocular burns. Emergency Nurse. 1999;6(10):20–24.
Marsden, J. Painless loss of vision. Emergency Nurse. 1999;6(9):13–18.
Marsden, J. The care of patients presenting with acute problems. In: Marsden J., ed. Ophthalmic Care. Chichester: Wiley, 2006.
Marsden, J. Ophthalmological emergencies. In: Crouch R., Charters A., Dawood M., Bennett P., eds. Oxford Handbook of Emergency Nursing. Oxford: Oxford University Press, 2009.
McDonald, R.J., Lawlor, M., McCluskey, P.J. Anteriour uveitis: is the cause of a red eye? Medicine Today. 2012;13(2):58–60.
McGhee, C.N., Ananstas, C.N. Widespread ocular use of topical chloramphenicol: is there justifiable concern regarding idiosyncratic aplastic anaemia? British Journal of Ophthalmology. 1996;80:182–184.
Moscati, R.M., Mayrose, J., Reardon, R.F., et al. A multicentre comparison of tap water versus sterile saline for wound irrigation. Academic Emergency Medicine. 2007;14:404–410.
Scott, R. Eye trauma. In: Smith J., Greaves I., Porter K., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford Medical Publications, 2011.
Sharma, A., Smilkstein, M.J., Fraunfelder, F.W. Ophthalmic principles. In Flomenbaum N.E., Goldfrank L.R., Hoffman R.S., et al, eds.: Goldfrank’s Toxicologic Emergencies, eighth ed, New York: McGraw Hill, 2006.
Shaw, M., Lee, A., Stollery, R. Ophthalmic Nursing, fourth ed. Oxford: Wiley Blackwell; 2010.
Tan, M.M.S., Driscoll, P.A., Marsden, J.E. Management of eye emergencies in the accident and emergency department by senior house officers: a national survey. Journal of Accident and Emergency Medicine. 1997;14:157–158.
Tullo, A.B., Donnelly, D. Conjunctiva. In Perry J.P., Tullo A.B., eds.: Care of the Ophthalmic Patient, second ed, London: Chapman and Hall, 1995.
Waggoner, M.D. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Survey of Ophthalmology. 1997;41(4):275–313.
Woodcock, M. Ophthalmic injuries. In: Greaves I., Porter K., Garner J., eds. Trauma Care Manual. London: Hodder Arnold, 2009.