CHAPTER 2 TRAUMA CENTER ORGANIZATION AND VERIFICATION
The development of trauma care has evolved from a synergistic relationship between the military and civilian medical environments for the past two centuries. During the Civil War, military physicians realized the utility of prompt attention to the wounded, early debridement, and amputation to mitigate the effects of tissue injury and infection, and evacuation of the casualty from the battlefield. World War I saw further advances in the concept of evacuation and the development of echelons of medical care. With World War II, blood transfusion and resuscitative fluids were widely introduced into the combat environment, and surgical practice was improved to care for wounded soldiers. In fact, armed conflict has always promoted advances in trauma care due to the concentrated exposure of military hospitals to large numbers of injured people during a relatively short span of time. Furthermore, this wartime medical experience fostered a fundamental desire to improve outcomes by improving practice. In Vietnam, more highly trained medics at the point of wounding and prompt aeromedical evacuation decreased battlefield mortality rate even further.
TRAUMA SYSTEM AND TRAUMA CENTER ORGANIZATION
Trauma System Organization
The organization of trauma systems and trauma centers derives from efforts to match the supply of trauma services accessible to a population in a specific geographical area with the demand for these services in this area. In this process, resources tend to be concentrated in areas of higher patient volume and acuity. At the core of the system organization is the Level I trauma center. Most of these Level I facilities are located at tertiary referral centers within major urban environments. Along with the patient characteristics, these centers foster the development of trauma system infrastructure elements including trauma leadership, professional resources, information management, performance improvement, research, education, and advocacy. By virtue of their inherently academic disposition, Level I centers generally serve as the regional resource for injury care. In addition, due to their size and resourcing, most are capable of managing large numbers of injured patients and have immediate availability of in-house trauma surgeons.1
The next tier of trauma center organization is the Level II trauma center. Like the Level I center, many of these facilities tend to be located in communities of higher population density. The Level II centers aspire to similar standards as the Level I facilities with the exception that their accreditation is not contingent on having graduate medical education, research capacities, or specific volume requirements. Approximately 84% of U.S. residents have access to Level I or Level II trauma centers within 60 minutes of injury through the aeromedical evacuation system.2 The benefits of this concentration of resources in Level I and II trauma centers are found in the association between trauma center volume and decreased average length of stay and improved patient mortality after injury.3 Recent epidemiological studies of trauma patients show that mortality risk is significantly lower when care is provided in a trauma center rather than in a non-trauma center, which supports continued efforts at regionalization.4 It has also been demonstrated that more severely injured patients, with an injury severity score of >15, have lower mortality rates when treated at Level I trauma centers as compared with lower-echelon centers.5
Trauma Center Organization
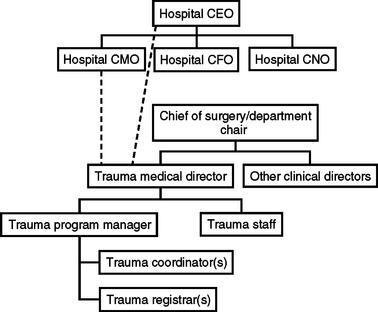
The development and success of a trauma center is contingent upon two basic building blocks: hospital organizational support and medical staff support. First, the hospital and its leadership must have a firm administrative and financial commitment to trauma center development, including incorporating the program into the formal organizational structure at a point commensurate with other clinical care departments of equal organizational stature. Second, medical staff support must be adequate for all levels and types of trauma patient care.6 The basic organizational structure schematic is shown in Figure 1.
Levels of response are guided by patient acuity and level of trauma center resources. Higher patient acuity with more robust resources, as in Level I and II trauma centers, encumbers response from the general/trauma surgeon, emergency physician, anesthesia provider, resident trainees, trauma/emergency nursing, respiratory therapy, radiology technician, security, and religious counsel. The team leader is the surgeon who is ultimately responsible for the patient’s disposition and care, but more importantly, all members of the team work together to streamline patient care according to Advanced Trauma Life Support® guidelines. The trauma service maintains the clinical responsibility for continuity of care in the multidisciplinary environment of injury care. In higher-echelon trauma centers, the trauma service is often a formal clinical service or services under the guidance of trauma staff surgeons. In Level II facilities, these trauma patients are often admitted to the primary surgeon of record and the continuity and oversight to maintain service integrity are provided by the trauma medical director.
The trauma program within a trauma center is a multidisciplinary effort that supports injury care from resuscitation through rehabilitation. Integral staff elements within the trauma program are the trauma medical director, trauma staff, physician specialty staff (orthopedics, neurosurgery, emergency medicine, anesthesia, radiology), trauma program manager/trauma nurse coordinator(s), and trauma registrar(s).6 The key processes that distinguish a trauma center are performance improvement and multidisciplinary peer review.
Trauma Program Manager/Trauma Nurse Coordinator
The position of trauma program manager and trauma nurse coordinator are dual positions or can be coalesced into a single position depending on the size and volume of the trauma program. This position is filled by a highly specialized registered nurse with advanced trauma training who is integral to the development, coordination, implementation, and evaluation of trauma care within the program. This position serves as a key leadership liaison between the staff and process elements within the program (Table 1).
Table 1 Roles of Trauma Program Manager/Trauma Nurse Coordinator
| Role | Definition |
|---|---|
| Clinical | Coordinating continuity and quality of trauma care in multidisciplinary environment |
| Administrative | Helps manage the operational and fiscal activities of the program as well as participates in various committee activities |
| Leadership liaison | Team building |
| Promotes trauma program at local, regional, state, and national levels | |
| Educational | Trains trauma program staff |
| Provides resource plan to train local facilities | |
| Promotes outreach programs | |
| Registry | Oversight of trauma registry data collection and accuracy |
| Performance improvement | Key proponent of trauma program performance improvement process from discovery through loop closure |
| Research | Promotes accurate and reliable data collection and analysis for performance improvement and facilitates clinical research endeavors |
| System advocate | Trauma system development, funding, patient advocate, injury prevention, public education, and outreach |
TRAUMA PERFORMANCE IMPROVEMENT PROCESS
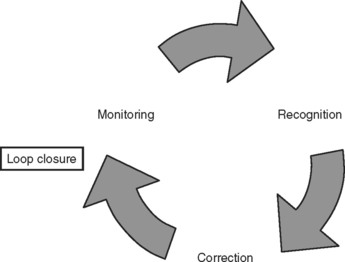
The trauma performance improvement process is perhaps the most important of all trauma program processes for ensuring that the highest quality of care is rendered to each injured patient. The importance of this process is vital from a functional and verification perspective. In fact, more than 50% of verification visit time is spent evaluating patient records and performance improvement. Trauma performance improvement begins with the definition of trauma (ICD-9 codes 800–959.9). This process is based on the tenets of program monitoring, which should be contemporary and based on reliable data. Outliers are identified that serve as indicators of deviation from the standard of care which require further review and discussion. A decision must be made as to whether no action is required or corrective action needs to be instituted in the form of individual counseling, education, policy review, peer review, or multidisciplinary trauma committee review. Once the corrective action has been implemented, the performance indicator returns to the monitoring phase. If performance measures are acceptable, the “loop” is closed (Figure 2).
TRAUMA CENTER VERIFICATION
The basic premise for trauma center verification is to ascertain whether a trauma center meets the guidelines outlined in the Resources for the Optimal Care of the Injured Patient published by the American College of Surgeons Committee on Trauma. Trauma center designation is a process that is geopolitical in origin, and is the ultimate responsibility of the local, regional, or state health care agency with which the trauma center is affiliated. In some states, trauma center designation tasks the regional provision of trauma care to particular hospital facilities, and is required to receive uncompensated care funding from governmental agencies and apply for governmental research grants and support. The designation and verification processes are complementary: designation recognizes capability, whereas verification confirms adherence to established guidelines. Effective trauma centers require both processes to affirm institutional and governmental commitment to the success of the trauma program.7
The verification visit is contingent on approval by the responsible designating authority or in the absence of such an agency, upon request of an individual hospital. Once this occurs, the facility completes the verification application for a site visit followed by completion of pre-review questionnaire (PRQ). A review team is selected, the composition of which may be dependent on the requirements of the designating authority. The verification review consists of a pre-review dinner meeting and an on-site review characterized by a tour of the facility followed by an in-depth chart review and performance improvement process analysis. Other aspects of the trauma program, including prevention, prehospital care, trauma service organization, educational activities, and rehabilitation programs are also evaluated. Trauma center criteria are shown in Table 2.
| Trauma Center Level | Deficiencies by Level and Chapter |
|---|---|
| 1: Trauma Systems | |
| I, II, III | 1.1 There is insufficient involvement by the hospital trauma program staff in state/regional trauma system planning, development, and/or operation (see FAQsa). |
| 2: Description of Trauma Centers and Their Roles in a Trauma System | |
| I, II, III | 2.1 There is lack of surgical commitment to the trauma center. |
| I, II, III | 2.2 All trauma facilities are not on the same campus. |
| I | 2.3 The Level I trauma center does not meet admission volume performance requirements. |
| I, II, III | 2.4 The trauma director does not have the responsibility or authority for determining each general surgeon’s ability to participate on the trauma panel through the trauma POPS program and hospital policy. |
| I | 2.5 General surgeon or appropriate substitute (PGY-4 or-5 resident) is not available for major resuscitations in-house 24 hours a day. |
| I, II | 2.6 The PIPS program has not defined conditions requiring the surgeon’s |
| I, II, III | 2.7 The 80% compliance of the surgeon’s presence rmed or in the monitored by PIPS (15 minutes for Levels I and II; 30 minutes for Level III). |
| I, II | 2.8 The trauma surgeon on call is not dedicated to the trauma center while on duty. |
| I, II | 2.9 A published backup call schedule for trauma surgery is not available. |
| III | 2.10 A Level III center does not have continuous general surgical coverage. |
| III | 2.11 The trauma panel surgeons do not respond promptly to activations, remain knowledgeable in trauma care principles whether treating locally or transferring to a center with more resources, or participate in performance review activities. |
| IV | 2.12 The facility does not have 24-hour emergency coverage by a physician. |
| III, IV | 2.13 Well-defined transfer plans are not present. |
| I, II, III | 2.14 Trauma surgeons in adult trauma centers that treat more than 100 injured children annually are not credentialed for pediatric trauma care by the hospital’s |
| I, II, III | 2.15 The adult trauma center that treats more than 100 injured children annually does not have a pediatric emergency department area, a pediatric intensive care area, appropriate resuscitation equipment, and pediatric-specific trauma PIPS program. |
| I, II, III | 2.16 The adult trauma center that treats children does not review the care of injured children through the PIPS program. |
| 3: Prehospital Trauma Care | |
| I, II, III | 3.1 The trauma director is not involved in the development of the trauma |
| I, II, III | 3.2 The trauma surgeon is not involved in the decisions regarding bypass. |
| I, II, III | 3.3 The trauma program does not participate in prehospital care protocol development and the PIPS program. |
| 4: Interhospital Transfer | |
| I, II, III | 4.1 A mechanism for direct physician-to-physician contact is not present for arranging patient transfer. |
| I, II, III | 4.2 The decision to transfer an injured patient to a specialty care facility in an acute situation is not based solely on the needs of the patient; for example, payment method is considered. |
| 5: Hospital Organization and the Trauma Program | |
| I, II, III | 5.1 The hospital does not have the commitment of the institutional governing body and the medical staff to become a trauma center. |
| I, II, III | 5.2 There is no current resolution supporting the trauma center from the hospital board. |
| I, II, III | 5.3 There is no current resolution supporting the trauma center from the medical staff. |
| I, II, III | 5.4 The multidisciplinary trauma program does not continuously evaluate its processes and outcomes to ensure optimal and timely care. |
| I, II, III | 5.5 The trauma medical director is neither a board-certified surgeon nor an American College of Surgeons fellow. |
| I, II, III | 5.6 The trauma medical director does not participate in trauma call. |
| I, II, III | 5.7 The trauma medical director is not current in Advanced Trauma Life Support®. |
| I, II | 5.8 The trauma director is neither a member nor an active participant in any national or regional trauma organizations. |
| I, II, III | 5.9 The trauma director does not have the authority to correct deficiencies in trauma care or exclude from trauma call the trauma team members who do not meet specified criteria. |
| I, II, III | 5.10 The criteria for graded activation are not clearly defined by the trauma center and continuously evaluated by the PIPS program (see FAQsa). |
| I, II, III | 5.11 Programs that admit more than 10% of injured patients to nonsurgical services do not demonstrate the appropriateness of that practice through the PIPS process (see FAQsa). |
| I, II | 5.12 Seriously injured patients are not admitted to or evaluated by an identifiable surgical service staffed by credentialed trauma providers. |
| I, II | 5.13 There is insufficient infrastructure and support to the trauma service to ensure adequate provision of care. |
| I, II | 5.14 In teaching facilities, the requirements of the Residency Review Committee are not met. |
| III | 5.15 The structure of the trauma program does not allow the trauma director to have oversight authority for the care of injured patients who may be admitted to individual surgeons. |
| III | 5.16 There is no method to identify injured patients, monitor the provision of health care services, make periodic rounds, and hold formal and informal discussions with individual practitioners. |
| I, II | 5.17 The trauma program manager does not show evidence of educational preparation (a minimum of 16 hours of trauma-related continuing education per year) and clinical experience in the care of injured patients. |
| I, II, III | 5.18 There is no multidisciplinary peer review committee chaired by the trauma medical director or designee, with representatives from appropriate subspecialty services. |
| I, II, III | 5.19 Adequate (50%) attendance by general surgery (core group) at the multidisciplinary peer review committee is not documented. |
| I, II, III | 5.20 The core group is not adequately defined by the trauma medical director. |
| I, II, III | 5.21 The core group does not take at least 60% of the total trauma call hours each month. |
| I, II, III | 5.22 The trauma medical director does not ensure and document dissemination of information and findings from the peer review meetings to the noncore surgeons on the trauma call panel. |
| I, II, III | 5.23 There is no Trauma Program Operational Process Performance Improvement Committee. |
a Answers to FAQs can be viewed on the American College of Surgeons website at www.facs.org/trauma/faq_answers.html. FAQ, Frequently asked questions; PIPS, performance improvement and patient safety.
Source: Adapted from Committee on Trauma, American College of Surgeons, Resources for Optimal Care of the Injured Patient: 2006, 5th ed. Chicago, American College of Surgeons, 2006, Chapter 16, pp. 139–141.
The preparation for verification and the verification process itself have demonstrated significant impact on trauma patient care and lowering of injury mortality.8–10
1 Hoyt D, Coimbra R & Potenza B: Trauma Systems, Triage, and Transport. In Moore E, Feliciano D, Mattox K, editors: Trauma. New York, McGraw-Hill, pp. 57–85
2 Branas CC, et al. Access to trauma centers in the United States. JAMA. 2005;293(21):2626-2633.
3 Nathens AB, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285(9):1164-1171.
4 MacKenzie EJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378.
5 Demetriades D, et al. Relationship between American College of Surgeons trauma center designation and mortality in patients with severe trauma (injury severity score > 15). J Am Coll Surg. 2006;202(2):212-215. quiz A45
6 Committee on Trauma, American College of Surgeons. Resources for Optimal Care of the Injured Patient: 2006, 5 ed. Chicago: American College of Surgeons, 2006.
7 Maull KI, et al. Trauma center verification. J Trauma. 1986;26(6):521-524.
8 DiRusso S, et al. Preparation and achievement of American College of Surgeons level I trauma verification raises hospital performance and improves patient outcome. J Trauma. 2001;51(2):294-299. discussion 299–300
9 Ehrlich PF, et al. American College of Surgeons, Committee on Trauma Verification Review: does it really make a difference? J Trauma. 2002;53(5):811-816.
10 Sampalis JS, et al. Trauma center designation: initial impact on trauma-related mortality. J Trauma. 1995;39(2):232-237. discussion 237–239