38 Transversus Abdominis Plane Block
Perspective
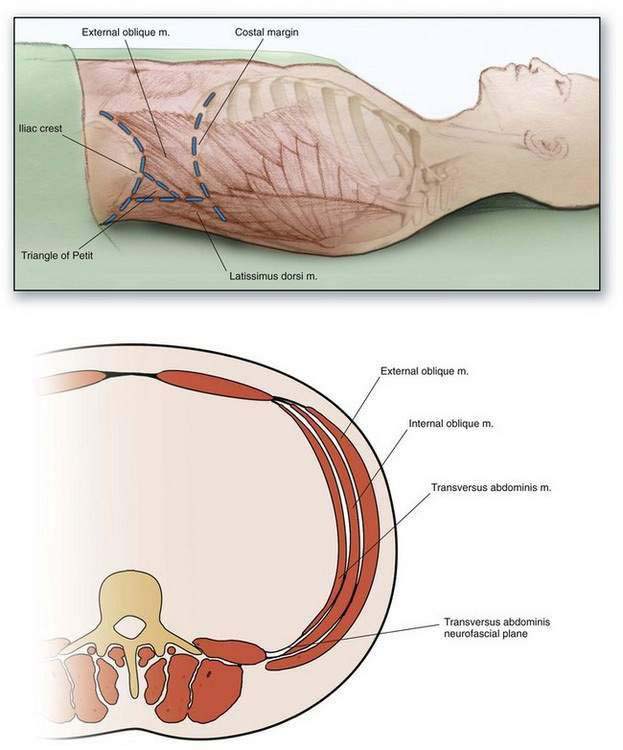
The transversus abdominis plane (TAP) block is used for patients undergoing surgeries involving anterior abdominal wall incisions. The TAP block provides analgesia to the anterior abdominal wall. The lateral abdominal wall comprises three layers of muscle and their associated fascia: the most superficial muscle is the external oblique; deep to this is the internal oblique; and still deeper is the transversus abdominis. The anterior rami of the lower six thoracic and first lumbar nerves provide sensation to the skin, muscles, and parietal peritoneum of the anterior abdominal wall. After exiting the vertebral column’s foramina, these nerves pass through the lateral abdominal wall within the fascial plane between the internal oblique and transversus abdominis muscles (the transversus abdominis neurofascial plane; Fig. 38-1). Injecting local anesthetic into the fascial plane between the internal oblique and transversus abdominis muscles produces the TAP block.
Placement
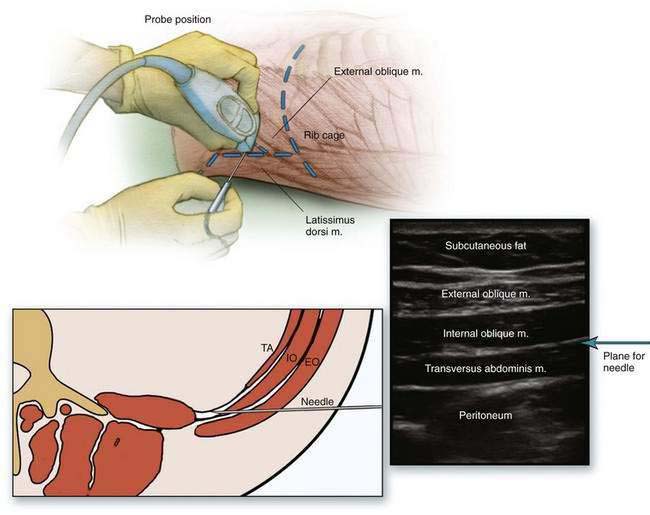
The TAP block is generally placed in a supine patient after the induction of anesthesia and before the surgical incision. After aseptic skin preparation and draping, a 2-inch, 24-gauge, blunt regional anesthesia needle is used for the triangle of Petit approach. A 2-inch, 24-gauge, blunt regional anesthesia or an 18-gauge Tuohy needle can be used for the ultrasonography-guided approach (Fig. 38-2).
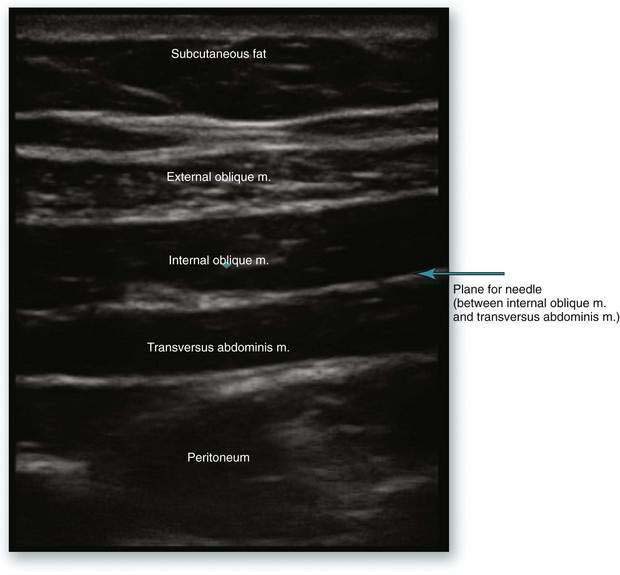
Figure 38-2. Transversus abdominis plane block: sonographic anatomy, showing plane of needle insertion.
Ultrasonography-Guided Approach
The ultrasound probe is placed just superior to the iliac crest in the mid-axillary line, oriented transversely to the abdomen ![]() (see Video 12: Transversus Abdominis Plane Block on the Expert Consult Website) (Fig. 38-3). The three abdominal wall muscle layers are identified: the external oblique muscle superiorly, the internal oblique in the middle, and the transversus abdominis inferiorly. The peritoneum lies deep to the transversus abdominis muscle. The needle is introduced within the plane of the ultrasound probe and maneuvered until it is easily viewed sonographically. The needle is then advanced until the tip lies between the internal oblique and transversus abdominis muscles. After a negative aspiration, the local anesthetic is injected in divided aliquots. The transversus abdominis muscle layer will bulge inferiorly and away from the internal oblique muscle as the local anesthetic expands in the fascial plane.
(see Video 12: Transversus Abdominis Plane Block on the Expert Consult Website) (Fig. 38-3). The three abdominal wall muscle layers are identified: the external oblique muscle superiorly, the internal oblique in the middle, and the transversus abdominis inferiorly. The peritoneum lies deep to the transversus abdominis muscle. The needle is introduced within the plane of the ultrasound probe and maneuvered until it is easily viewed sonographically. The needle is then advanced until the tip lies between the internal oblique and transversus abdominis muscles. After a negative aspiration, the local anesthetic is injected in divided aliquots. The transversus abdominis muscle layer will bulge inferiorly and away from the internal oblique muscle as the local anesthetic expands in the fascial plane.
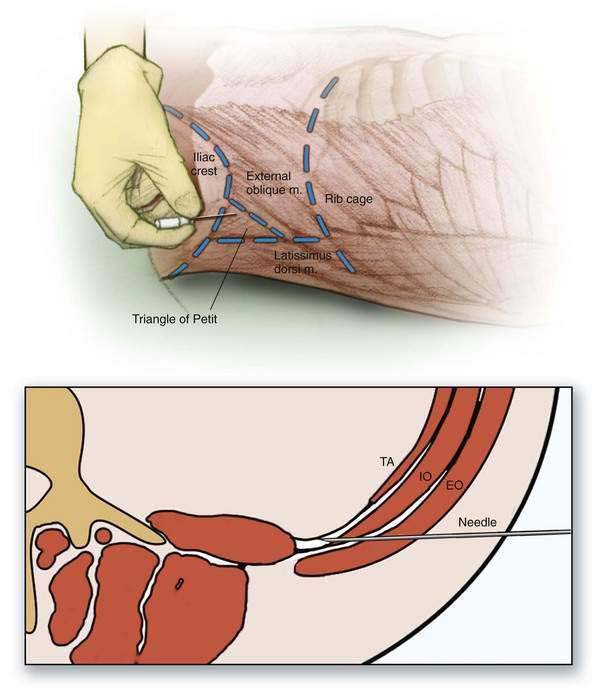
Triangle of Petit Approach
The lumbar triangle of Petit is an anatomic space between the posterior attachment of the external oblique muscle and the anterior attachment of the latissimus dorsi muscle to the iliac crest. It consists of three walls: the iliac crest forms the inferior wall, the external oblique forms the anterior wall, and the latissimus dorsi provides the posterior wall. The floor of the triangle is formed by the external oblique fascia; deep to this is the internal oblique fascia and deeper still is the transversus abdominis fascia. After aseptic skin preparation in a supine patient, the operator’s finger palpates along the cephalad iliac crest from anterior to posterior until a slight irregularity is identified; this marks the attachments of the external oblique and latissimus dorsi muscles. On further posterior movement of the finger, the edge of a muscle is palpated. This is the lateral border of the latissimus dorsi muscle. The area just anterior to the lateral border of the latissimus dorsi muscle is the triangle of Petit. At this point, a blunt regional anesthetic needle is advanced perpendicular to the plane of the triangle of Petit (Fig. 38-4). The needle is advanced until two fascial “pops” are felt. The first pop is felt as the needle penetrates the external oblique fascia, and the second is felt as the needle penetrates the internal oblique fascial layer and enters the plane just external to the transversus abdominis muscle. Local anesthetic is injected after negative aspiration.