Transportation of the acutely ill patient
Introduction
This chapter outlines the nursing care and operational considerations in regard to transportation of the acutely ill person. It will build upon areas elsewhere in this book and will identify the pre-, peri- and post-transportation issues and the care needs of people in transportation. The focus of this chapter will primarily be on secondary rather than primary transportation, as other chapters such as Chapters 1 and 3 make reference to pre-hospital care and the assessment prior to transportation. It links the social trends on movement of people with the need to provide rapid transportation.
Travel trends
• between 1950 and 2005, international tourism arrivals expanded at an annual rate of 6.5 %, growing from 25 million to 806 million travellers
• the income generated by these arrivals grew at an even stronger rate reaching 11.2 % during the same period, outgrowing the world economy to reach around US$680 billion in 2005
• while in 1950 the top 15 destinations absorbed 88 % of international arrivals, in 1970 the proportion was 75 % and decreased to 57 % in 2005, reflecting the emergence of new destinations, many of them in developing countries (United Nations World Tourism Organization 2010, European Travel Commission 2011).
• since 1984, trends in UK travel abroad have risen from 22 million residents to 58.6m in 2009; equally travel to the UK from abroad has also increased since 1984 with 13.6 million overseas residents rising to 28.9m in 2009 (Office of National Statistics 2010)
• the US had 56 million international visitors from 213 countries during 2007, up 10 % from 2006; total arrivals were also up 9 % from 2000, the former record year for total non-resident visitation to the country (International Trade Administration 2008).
Trends in admissions to critical care settings
Critical care admissions data collected by the NHS in England provide some insight into the patterns and reasons for admission to critical care units. Data from the first publication from Hospital Episodes Statistics (HES) in England show that 82 % of critical care records in the period April 2008–March 2009 were available, with 50 % of admissions showing detailed sources (Health and Social Care Information Centre 2009). While 45 % of data does not identify the reason for admission, of the remaining data just over 1 in 4 or 28 % are unplanned admissions with the majority being local admissions resulting in over 36 000 critical care transfers. While tertiary transfers are just fewer than 2900 cases, repatriations from neighbouring hospitals or overseas are recorded in over 3000 transfers. The dataset goes on to show that approximately 1 in 6 patients being admitted into a critical care bed will require a transfer and transportation.
Types of transportation
There are broadly three types of transportation:
• primary transportation refers to the initial response of the acutely ill or injured from the scene of accident or incident to a care facility
• secondary transportation is any onward movements following the primary transportation; also sometimes called tertiary transportation to specialist care or repatriation when it refers to moving someone back to their country of domicile after they become ill or injured abroad
• patient transport refers to general movement; patient transport service (PTS) is used for routine transportation of patients to and from hospital care, such as outpatients appointments or discharge to their place of residence.
In the UK, the development of regional trauma centres and specialist centres, e.g., burn units, neurosurgical units (if not contained within trauma centres), specialist neonatal units (level 1), will mean secondary transfer will probably be necessary. The role of the nurse in the preparation, both pre-transfer and co-ordination of care by communicating with the receiving hospital/centre is key in the safe and effective transfer of the acutely ill or injured person.
Primary transfers
The mode of transport will influence what care is needed pre-transportation. For example, it may be necessary to intubate in advance rather than attempt to intubate in transit because of space, movement and other external factors. The steps required for the pre-hospital care environment are discussed in Chapter 1.
Secondary transfers
Transfers back to the care setting responsible for the person’s on-going condition (including back to their country of domicile), or where rehabilitation is appropriate, are classed as repatriation transfers. Because of the distances involved, the patient’s clinical condition and resources will influence the appropriate mode of transportation. The Association of Anaesthetists of Great Britain and Ireland has developed recommendations that are summarized in Box 4.1.
Factors affecting transfers
A key operational issue that is often overlooked is that unless a local policy dictates otherwise, secondary transfers, i.e., tertiary and repatriations transfers, should not route via the Emergency Department (ED) unless there has been deterioration in the patient’s condition or a new event requiring immediate intervention. Being sent to the ED for registration purposes is poor practice (Box 4.2).
Modes of transportation
While progress in transportation over the last 100 years has increased the mode of transport options, the majority of both primary and secondary transfers have been by road transportation. Historically, ambulances provided a basic collection and removal of the ill or injured person. They now provide a mobile primary response service by providing the initial assessment, stabilization prior to transportation to on-going care at a hospital base. Aircraft and helicopters provide a means of rapid movement of people over long distances, offering significant advances to the survival of injured or ill patients. While each mode of transport has benefits they also have risks, and the choice of mode is as important as the response itself.
Considerations on appropriate transportation
Where any of these factors are compromised then alternatives need to be considered, assuming such supportive resources exist or can be accessed. Holleran & Rhoades (2005) discuss these and similar factors in their work. In some parts of the UK air support may be provided by special request from neighbouring authorities, especially when road transportation in isolated areas or the victim’s condition is serious, rapid transportation to a facility may warrant the use of a primary helicopter. The Intensive Care Society (2002) suggests that for long journeys where road access is difficult, air transport may be quicker; however the perceived speed of air transport must be balanced against organizational delays and inter-vehicle transfers.
Ground transportation
Modern vehicles all have life-saving equipment with automatic external defibrillators, suction, and a wide range of medication to support critical care to obstetric care. These will have 240 volt AC power, a secure critical care trolley and carry a ventilator and syringe drivers. It is more usual to request an ambulance from the local ambulance service to perform the transfer (Box 4.3).
Air transportation
Used to move injured soldiers in World War I in Italy (Bellini 2008), and in common use by World War II, aircraft have advanced over time since then to be pressurized, comfortable and a common mode of general transportation. However, movement by air has limitations and the response will be determined by key factors. Response by air is influenced by whether it is a primary or secondary response. The major advantages of an air response are both speed by the reduction in journey time and the ability to get the acutely ill or injured person from point A to B with minimal changes or delays.
Effect of air pressure on acutely ill
Impact of available oxygen: In the last 100 years there has been a growing understanding of the impact of air travel and the changes in pressure to human physiology. Martin (2001), Rainford & Grandwell (2006) and Holleran (2009) outline in detail how changes in air pressure affect the human body.
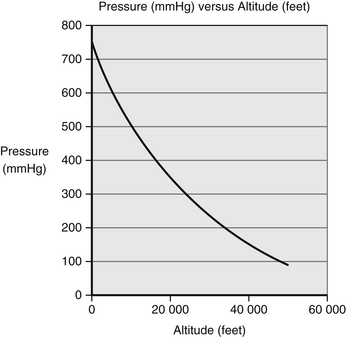
Although the percentage of oxygen in inspired air is constant at different altitudes, the fall in atmospheric pressure at higher altitude decreases the partial pressure of inspired oxygen and hence the driving pressure for gas exchange in the lungs. An ocean of air is present up to 9 000–10 000m, where the troposphere ends and the stratosphere begins. The weight of air above us is responsible for the atmospheric pressure, which is normally about 100 kPa at sea level. This atmospheric pressure is the sum of the partial pressures of the constituent gases, oxygen and nitrogen, and also the partial pressure of water vapour (6.3 kPa at 37°C). As oxygen is 21 % of dry air, the inspired oxygen pressure at sea level (Peacock 1998) (Fig 4.1) is calculated as follows:
Because of the effect of falling barometric pressure, even while pressurized to 2 438 metres (8 000 feet), for the majority of people there are no adverse effects despite the partial pressure of oxygen being at 120 mmHg (16.0 kPa), which corresponds to 75 % of the sea-level value of oxygen at 160 mmHg (21.3 kPa). This means a reduction in arterial oxygen tension from 95 mmHg (12.7 kPa) to between 53–64 mmHg (7.0–8.5 kPa), so oxygen saturation reduces from 97 % saturation on the ground (at sea level) to between 80–92 % at cruising altitude 2 438 metres (8 000 feet) (British Medical Association 2004). This is known as the oxygen disassociation curve and is covered in more detail in Chapter 23.
Impact of pressure on main organs: Boyle’s gas law, where Pressure × Volume = Constant, means that as an aircraft ascends and pressure drops, gas expands. The expansion will be affected by the reduction in air pressure, and at 2 438 metres (8 000 feet) this means an increase in expanded gas of approximately 30 %. Where gas can pass freely there is no problem; however, there can be problems where there is trapped or limited free gas movement, including in any organ which has had surgery in the proceeding 14 days.
At lower flying levels, aircraft cabins, including helicopters, are usually not pressurized. However, they are susceptible to the effects of turbulence, vibration, can be cold, and with helicopters noise. As a result, some equipment, e.g., stethoscopes, is unusable in the air. Sphygmomanometers containing mercury are restricted, so digital sphygmomanometers must be used. Furthermore, temperature affects the ability to record oxygen saturation and a low saturation due to cold peripheral extremities rather than hypoxia should be considered.
On commercial aircraft each airline is responsible for providing medical clearance for its patients prior to flight. The International Air Transport Association (2010) issued medical clearance guidance to airlines and their governing bodies to support suitability to fly. Box 4.4 summarizes the main impact of changes in air pressure on key organs.
Contraindications to air travel
While for most patients in most situations travel by air is acceptable, there are a number of conditions where air travel is contraindicated (World Health Organization 2010). However, while some commercial airlines will accept a number of these conditions, a specialized air ambulance would be an alternative approach with appropriate medical and nursing support (Box 4.5).
Primary response by air
The latter issue of temperature management is usually not an overarching factor as the transfer duration is relatively short time-wise. The majority of journeys are usually less than 30 minutes’ duration and rarely exceed one hour.
Unless these issues adversely affect the movement of the injured or acutely ill patient, air transportation may be the mode of choice, especially in ensuring rapid supportive care. Undoubtedly helicopter primary transfers have saved thousands of lives worldwide since their introduction, especially among the most critically ill (Nicholl et al. 1995, Chipp et al. 2010).
The initial preparation and nursing considerations for a primary transfer will be the same as for a road ambulance transfer. The patient will need to have had a primary survey, most if not all cases will require c-spine immobilization and have adequate airway with venous access should there be a need to rapidly infuse. The level of consciousness and mechanism of injury, or underlying condition may require further preparation of intubation to ensure a patent airway. It is possible to provide infusions in these types of transfers.
A key risk time is the loading and unloading of the patient, and vigilance in ensuring that the patient’s limbs do not get caught in stretchers. It is key that all members follow the lead of the clinical/medical lead especially with monitoring and clinical tubing. Only approved monitoring equipment authorized by the appropriate aviation authorities should be used (Box 4.6).
Secondary repatriation by air
Aircraft in the UK are not usually dedicated to air responses unlike in other parts of Europe, the US and Australasia, although some companies that specialize in air repatriation have adapted and dedicated aircraft. In the UK, the majority of secondary air transfers will be from the Islands and from remote parts of the UK to tertiary services. The Intensive Care Society (2002) recommends that air transportation in a fixed wing aircraft should be considered for distances greater than 150 miles, and helicopter in place of long road journeys or where roads are inaccessible.
Special considerations for transportation by air
The patient is positioned in an aircraft on Joint Aviation Authorities (JAA)/Civil Aviation Authority (UK) CAA approved stretchers, with four-point (over shoulder and abdomen) safety belts. In commercial aircraft and smaller jets, the space above the person is usually restricted. Lastly, because of the gas laws of physics, any equipment that has air in it will expand.
Venous Thromboembolisms: In the 1990s awareness of deep vein thrombosis (DVT), now considered part of venous thromboembolism (VTE), as part of long-haul flying came under scrutiny. The UK House of Lords Science and Technology Committee investigated and produced Air Travel and Health that identified those who are at low, medium and higher risk of developing DVT/VTEs in flight (UK Parliament 2000). A subsequent report (UK Parliament 2007) further looked at DVT/VTEs and other issues raised in the first report. The issues around DVT/VTEs were considered as part of a wider World Health Organization Research Into Global Hazards of Travel (WRIGHT) project that was developed to confirm that the risk of VTE is increased by air travel. The study also determined the magnitude of risk, the effect of other factors on the risk, and the effect of preventive measures on risk (Box 4.7).
While there is still a lack of clarity on how to prevent air-related DVTs, the use of aspirin is yet to be clearly identified as a reputable source. However, the use of low-molecular-weight heparin in the prevention of DVT in higher-risk groups, including those who have previously had a DVT, is well established but it is not clear how it should be used in the prevention of travel-related DVT (British Medical Association 2004, Katsumata et al. 2012).
Special considerations
When preparing all transfers, it is paramount that specialist teams are considered, possibly using retrieval/collection teams if they exist. The suitably qualified (in the relevant specialty) and experienced clinical staff should follow the nationally agreed or professionally developed transfer guidelines (Middleton 2011). This should also include any specific documentation required as recommended.
Transfer of adult intensive care patients
In 1997 there were an estimated 11 000 tranfers (Association of Anaesthetists of Great Britain and Ireland 2009), however figures for the number of such transfers carried out currently are difficult to obtain as there is no national reporting (Intensive Care Society 2011). There are a number of international and national guidance documents (Association of Anaesthetists of Great Britain and Ireland 2009, Clinical Resource Efficiency and Resource Team 2006), which outline the key priorities. While these discuss the operational and skills level of the practitioner (Holleran 2002), there is also a need for nurses to have a suitable level of training to provide effective transfer and transportation support.
The Intensive Care Society (2002) issued guidance that covers an array of core service provision at EDs, consultant cover, transportation guidance on the number of staff and skills set, equipment and preparation, including competence of transport personnel, the role of nursing staff, the role of critical care networks, and the need for dedicated equipment.
While the rate of adverse events by clinically specialized teams is low (Kue et al. 2011), this requires adequate preparation of the team and the equipment. To support practitioners there is a need for adequate preparation (Bambi & Day 2010) and transportation checklists (Intensive Care Society 2002, Nocera 2002) have emerged that support practice around key areas. The Intensive Care Society guidelines include a number of checklists, for example: ‘Is the patient stable for transport’ covering airway, ventilation, circulation, metabolic, neurology, trauma, and monitoring and ‘Are you ready for departure’. These checklists are further supported by detailed guidance in the document.
Transfer of patients with neurological injuries
These types of injuries require rapid discussion, usually consultant-to-consultant prior to transfer. The Association of Anaesthetists of Great Britain and Ireland (2006) developed recommendations for the transfer of patients with brain injuries (Box 4.8).
Transfer of children
• there should be a designated consultant with the responsibility for transfers
• functional mobile equipment and relevant guidelines should be available
• all patient transfers should be accompanied by a trained doctor with a minimum of two years’ experience who has the ability to perform tracheal intubation and is accompanied by a trained assistant, either an ICU nurse or Operating Department Practitioner.
There will be times when a transfer to another care centre is appropriate, and guidelines for the transfer of ambulatory paediatric patients are recommended in these cases (Clinical Resource Efficiency and Resource Team 2001) (Box 4.9). While speedy intervention into paediatric care is important, Killion & Stein (2009) argue that air versus road ambulance transfers have no impact on patient outcome. Further studies in Australia suggest that different approaches can influence transfer time (Soundappan et al. 2007).
Consideration of infection
Infection prevention and control are as applicable within hospital care as well as external to hospital care. A significant amount of meticillin-resistant Staphylococcus aureus and other organisms are transferred into and between care settings from outside of hospital care. Transferring patients between hospitals poses significant risks to established infection control procedures, and each hospital will have localized policies in how patients are accepted and managed on arrival.
The transferring crew must follow universal precautions. The Department of Health in England have issued some guidance on ‘Reducing infection through effective practice in the pre-hospital environment’ (Department of Health 2008a). The document covers a range of topics from hand hygiene, personal protective equipment, aseptic technique and environmental cleanliness, through to the decontamination of ambulance stretcher beds. The nurse and medical escorts must ensure appropriate disposal of infectious clinical equipment.
Conclusion
Health systems, commissioners and providers of health need to be aware of the emerging forces around the movement of people in general to both predict and manage increasing numbers who need care and will require transportation. Nurses, especially those in EDs, critical care areas and those involved in transportation of patients are well placed to assess, plan the pathway of transportation, implement that care and evaluate it. Evaluation needs to be against the three outcome domains for quality (Department of Health 2008b):
1. the anticipated and expected experience: was the experience for the patient as anticipated, was all done to improve that experience?
2. the effectiveness of the need to transport: was the outcome after the transfer anticipated and could only have resulted from the transfer? Was the mode of transport the appropriate one, both for outcome and cost?
3. the safety: was a risk assessment in place to identify potential problems or harms? Did any occur? And what did the nursing intervention in place do to reduce harm?
With a growing body of evidence on the trends, outcomes, experiences and not just data, nurses and healthcare practitioners will be increasingly better placed to influence and improve the effects of care.
References
Association of Anaesthetists of Great Britain and Ireland. Recommendations for the Safe Transfer of Patients with Brain Injury. London: Association of Anaesthetists of Great Britain and Ireland; 2006.
Association of Anaesthetists of Great Britain and Ireland. AAGBI safety guideline – Inter-hospital Transfer. London: Association of Anaesthetists of Great Britain and Ireland; 2009.
Bambi, S., Day, D. The risk of intrahospital transport to patients. ‘Keeping patients safe during intrahospital transport’. Critical Care Nurse. 2010;30(6):14–16.
Bellini, C. An historical perspective of early Italian air medical transport. Air Medical Journal. 2008;27(6):286–292.
British Medical Association. The Impact of Flying on Passenger Health: A Guide oor Healthcare Professionals. London: British Medical Association; 2004.
British Thoracic Society. Managing Passengers with Respiratory Disease Planning Air Travel Summary for Primary Care. London: British Thoracic Society; 2004.
Chipp, E., Warner, R.M., McGill, D.J., et al. Air ambulance transfers of adult patients to a UK regional burn centre: Who needs to fly? Burns. 2010;36(8):1201–1207.
Clinical Resource Efficiency and Resource Team. Ambulatory Paediatrics Guidelines for referrals and transfer. Belfast: CREST; 2001.
Clinical Resource Efficiency and Resource Team. Protocol for the Inter Hospital Transfer of Patients and their Records. Belfast: CREST; 2006.
Department of Health (England). Ambulance Guidelines: Reducing Infection Through Effective Practice in the Pre-hospital Environment. London: Department of Health; 2008.
Department of Health (England). High Quality Care for All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
European Travel Commission. European Tourism in 2010: Trends & Prospects. Brussels: European Travel Commission; 2011.
Health and Social Care Information Centre. Hospital Episode Statistics 2008–2009. London: HSCIC; 2009.
Holleran, R. Challenges in transport nursing. Australian Emergency Nursing Journal. 2002;5(1):7–11.
Holleran, R. ASTNA Patient Transport: Principles and Practice, fourth ed. St Louis: Mosby; 2009.
Holleran, R., Rhoades, C. Ask the experts. Critical Care Nurse. 2005;25(1):58–59.
Intensive Care Society. Guidelines for the Transport of the Critically Care Adult. London: Intensive Care Society; 2002.
Intensive Care Society. Guidelines for the Transport of the Critically Ill Adult, third ed. London: ICS; 2011.
International Air Transport Association (IATA). Medical Manual, third ed. Geneva: International Air Transport Association; 2010.
International Trade Administration (USA). 2007 International Arrivals into the United States. Washington: Department of Commerce; 2008.
Katsumata, Y., Kimura, K., Sano, M., et al. Frequent long-distance flyer’s undesirable mileage: an organized thrombus stuck in PFO. Journal of Thrombolysis. 2012;33(3):296–298.
Killion, C., Stein, H.M. The impact of air transport on neonatal outcomes. Newborn & Infant Nursing Reviews. 2009;9(4):207–211.
Kue, R., Brown, P., Ness, C., et al. Adverse clinical events during intrahospital transport by a specialized team: a preliminary report. American Journal of Critical Care. 2011;20(2):153–164.
Martin, T. Handbook of Patient Transportation. London: Greenwich Medical Media Ltd; 2001.
Middleton, P. Trauma retrieval. In: Smith J., Greaves I., Porter K.M., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford University Press, 2011.
Nicholl, J.P., Brazier, J.E., Snooks, H.A. Effects of London helicopter emergency medical service on survival after trauma. British Medical Journal. 1995;311(6999):217–222.
Nocera, N. The N.E.W.S. Checklist: Enhancing interhospital transfer of trauma patients. Australian Emergency Nursing Journal. 2002;5(1):12–14.
Office of National Statistics. Travel Trends, 2009, edition. London: Office of National Statistics; 2010.
Parliament, U.K. House of Lords Science and Technology Committee Air Travel and Health. London: The Stationery Office; 2000.
Parliament, U.K. House of Lords Science and Technology Committee Air Travel and Health: An Update. London: The Stationery Office; 2007.
Peacock, A.J. Oxygen at high altitude. British Medical Journal. 1998;317(7165):1063–1066.
Rainford, D.P., Grandwell, D.G. Ernsting’s Aviation Medicine, fourth ed. London: Hodder; 2006.
Royal College of Nursing. Royal College of Nursing In-flight Nurses Association Clarification and Guidance on the Management and Administration of Medicines in the In-Flight Setting. London: Royal College of Nursing; 2006.
Soundappan, S.V., Holland, A.J., Fahy, F., et al. To study the appropriateness of, and time taken, to transfer pediatric trauma patients in New South Wales to The Children’s Hospital at Westmead (CHW), a pediatric trauma center. The Journal of Trauma. 2007;62(5):1229–1233.
United Nations World Tourism Organization. World Tourism Barometer. Madrid: UNWTO; 2010.
World Health Organization, Mode of travel: Health considerations. International Travel and Health, 2010 edition, Geneva, World Health Organization, 2010.