Controversial whether CTA/MRA is superior to US for TIPS surveillance
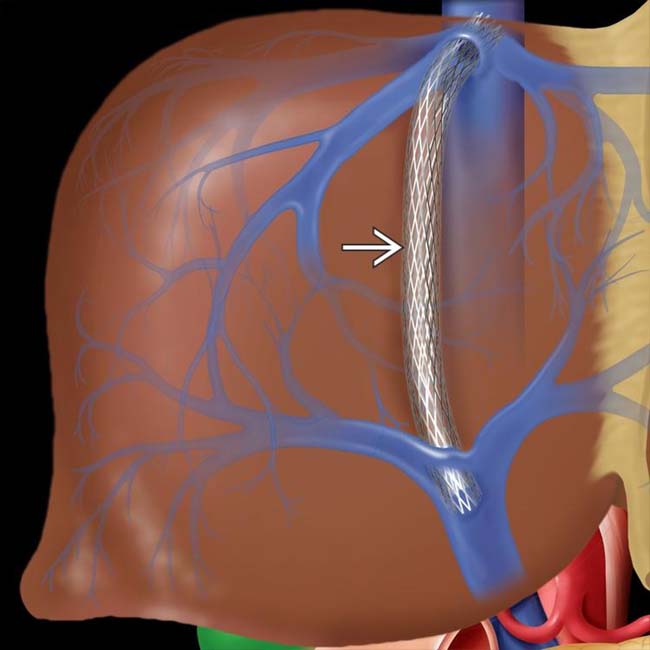
 extends to the right portal vein, adjacent to its junction with the main portal vein.
extends to the right portal vein, adjacent to its junction with the main portal vein.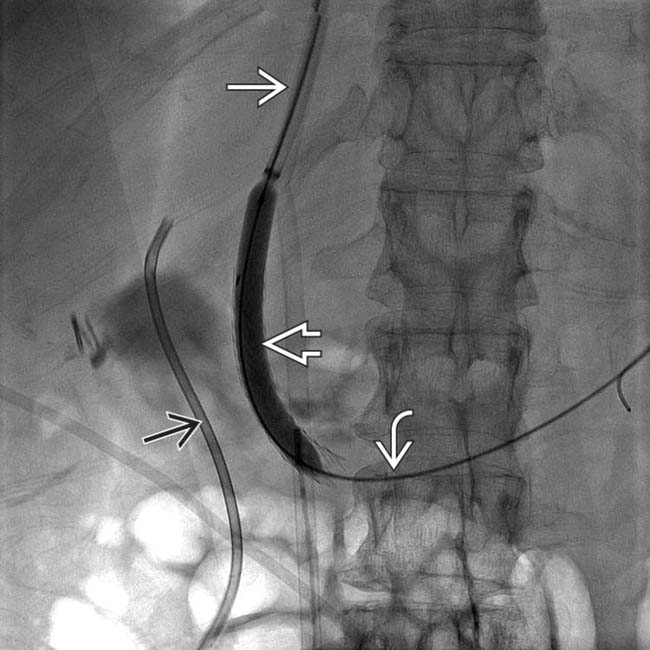
 proceeding down the IVC, then penetrating the liver parenchyma to enter the portal vein
proceeding down the IVC, then penetrating the liver parenchyma to enter the portal vein  . The intraparenchymal tract is dilated with a balloon
. The intraparenchymal tract is dilated with a balloon  . Incidentally noted is a plastic biliary stent
. Incidentally noted is a plastic biliary stent  .
.
 deployed with its distal end in the hepatic vein
deployed with its distal end in the hepatic vein  and its proximal end in the main portal vein
and its proximal end in the main portal vein  .
.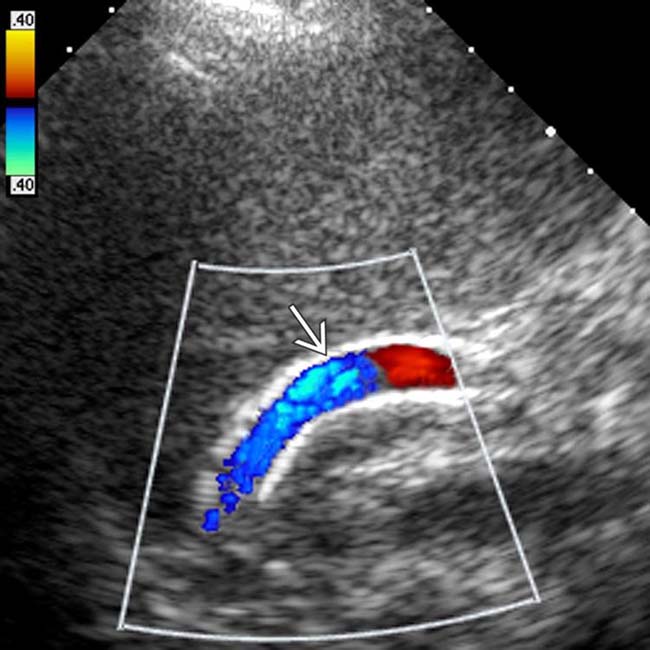
 . Although the stent is highly echogenic, it does not obstruct sonographic visualization. Color Doppler indicates brisk flow toward the heart, the expected finding.
. Although the stent is highly echogenic, it does not obstruct sonographic visualization. Color Doppler indicates brisk flow toward the heart, the expected finding.IMAGING
General Features
Ultrasonographic Findings
• Grayscale ultrasound
• Pulsed Doppler

 .
.
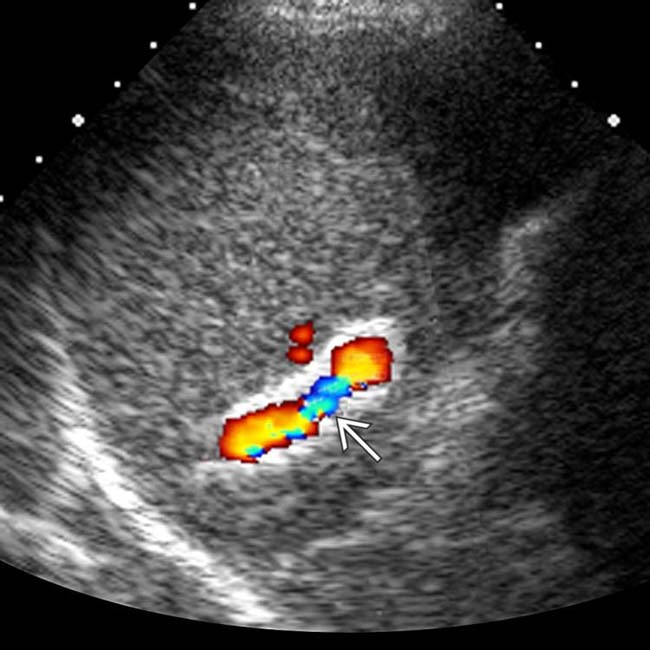
 . A subsequent angiogram revealed a high-grade TIPS stenosis involving the hepatic venous side of the shunt.
. A subsequent angiogram revealed a high-grade TIPS stenosis involving the hepatic venous side of the shunt.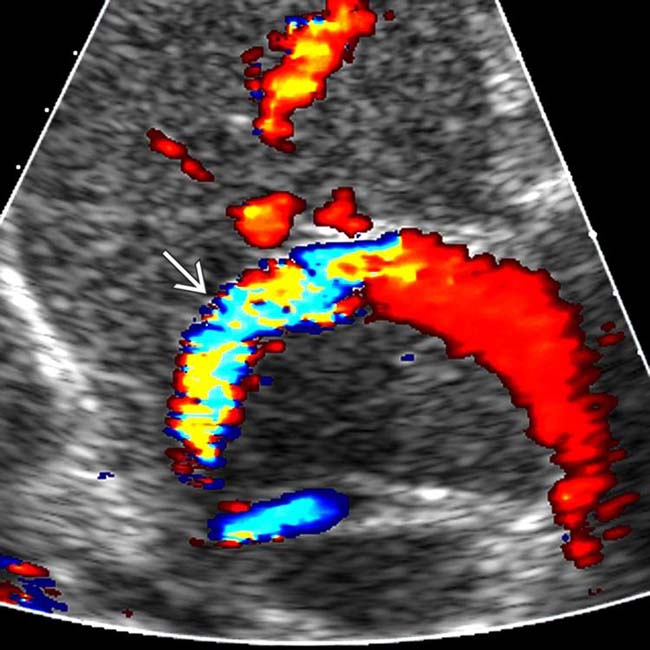
 .
.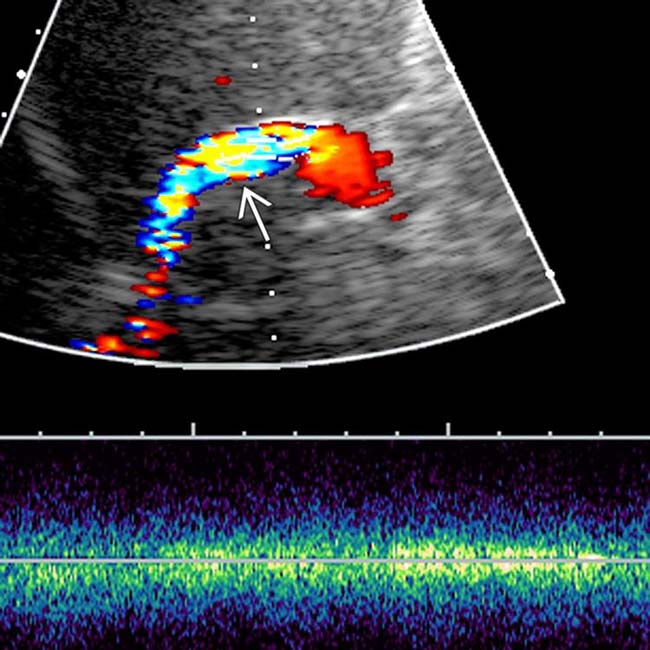
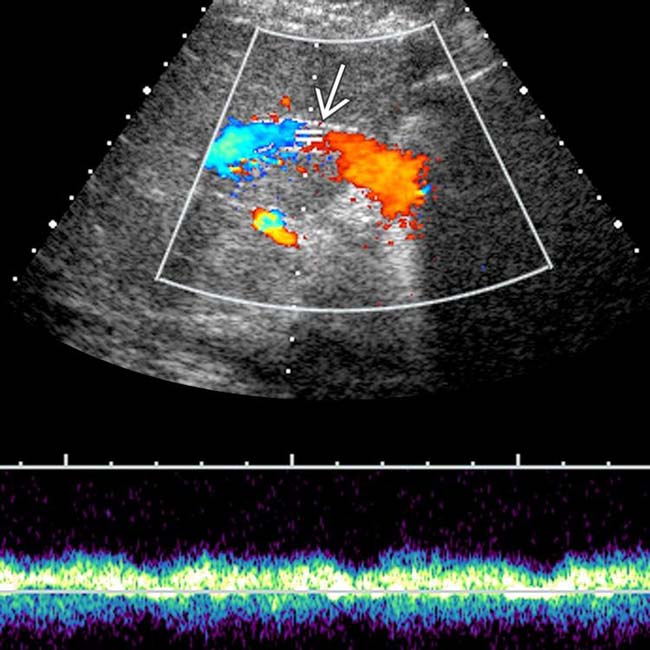
 , findings consistent with mid-shunt stenosis.
, findings consistent with mid-shunt stenosis.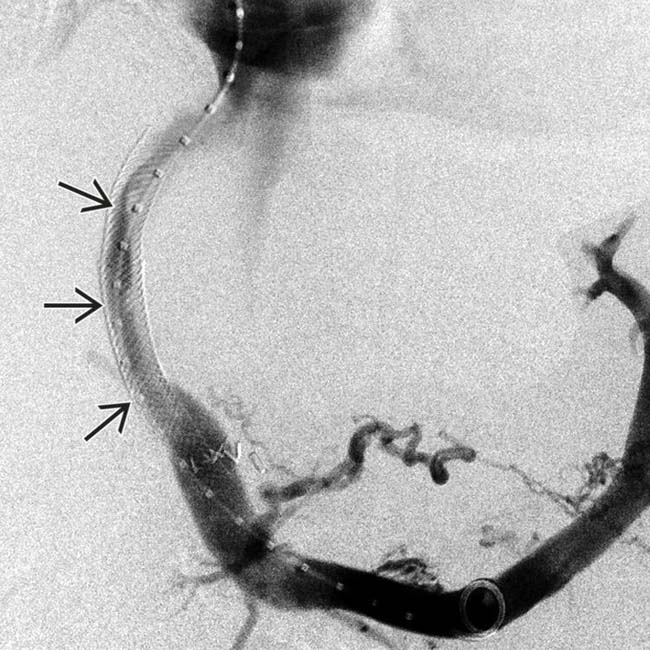
 within the parenchymal portion of the shunt, usually due to intimal hyperplasia.
within the parenchymal portion of the shunt, usually due to intimal hyperplasia.
 at the proximal end of the TIPS.
at the proximal end of the TIPS.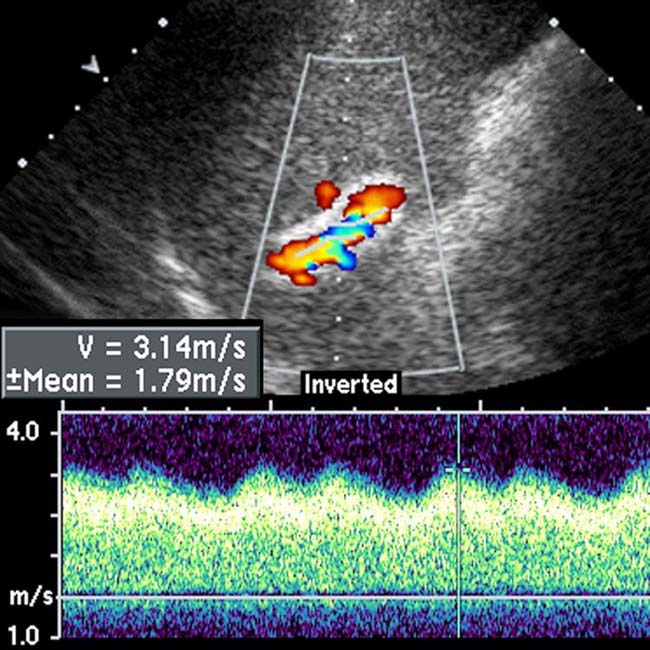
 near the hepatic end of the TIPS.
near the hepatic end of the TIPS.
 . Note the acoustic shadow deep to the stent
. Note the acoustic shadow deep to the stent  , precluding optimal US evaluation for stent patency.
, precluding optimal US evaluation for stent patency.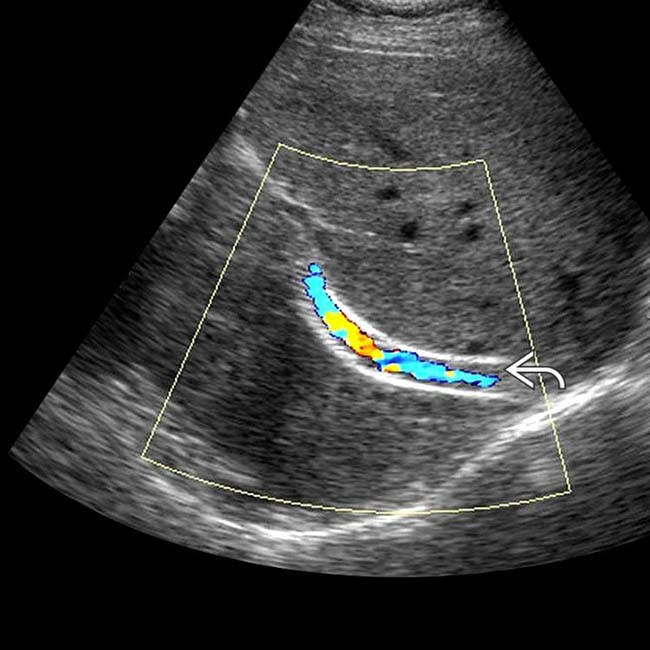
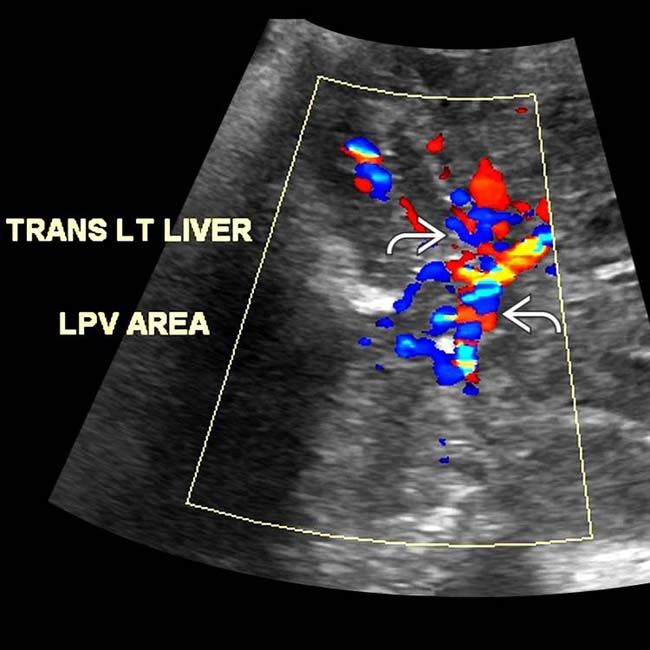
 and turbulent flow, likely due to intimal fibroplasia.
and turbulent flow, likely due to intimal fibroplasia.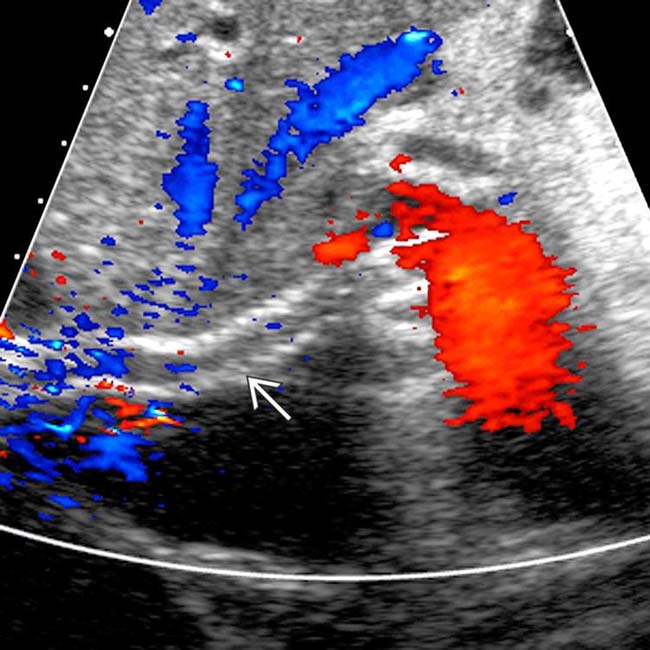
 with complete absence of flow, indicating TIPS occlusion.
with complete absence of flow, indicating TIPS occlusion.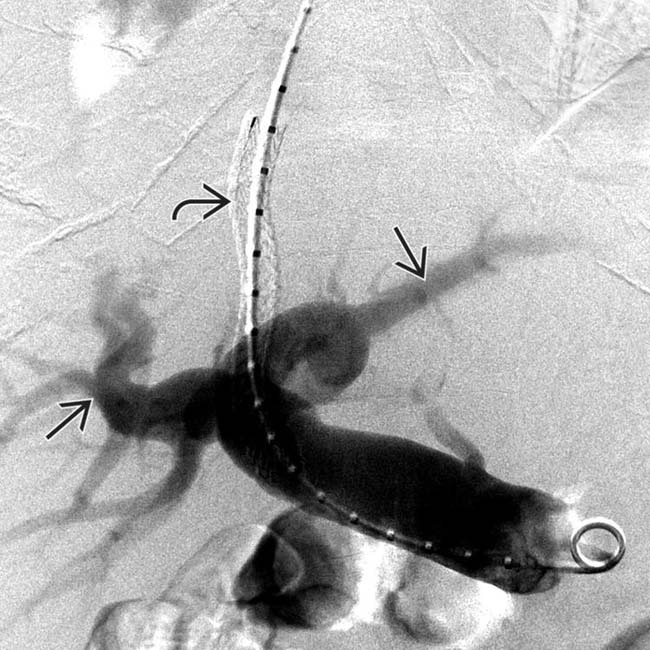
 , but no opacification of the TIPS
, but no opacification of the TIPS  , confirming shunt occlusion.
, confirming shunt occlusion.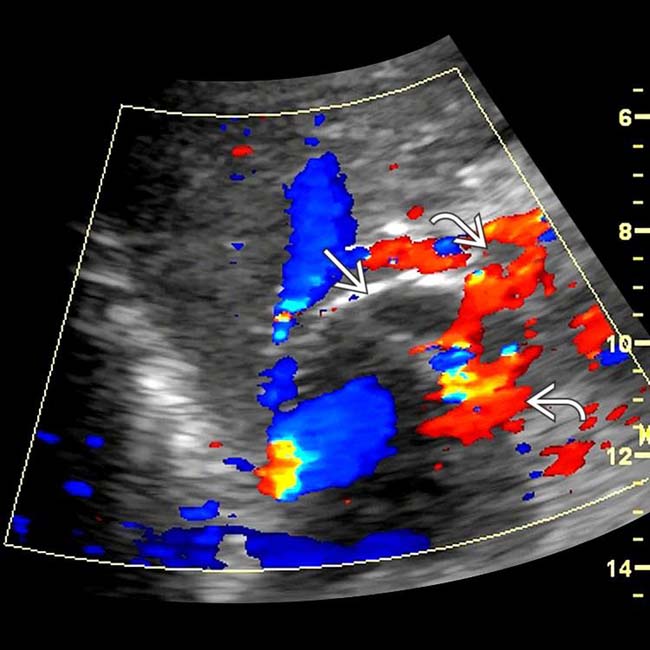
 , the proximal end of which terminates in a markedly distended main portal vein
, the proximal end of which terminates in a markedly distended main portal vein  .
.
 . The liver was very heterogeneous, but no discrete mass was identified.
. The liver was very heterogeneous, but no discrete mass was identified.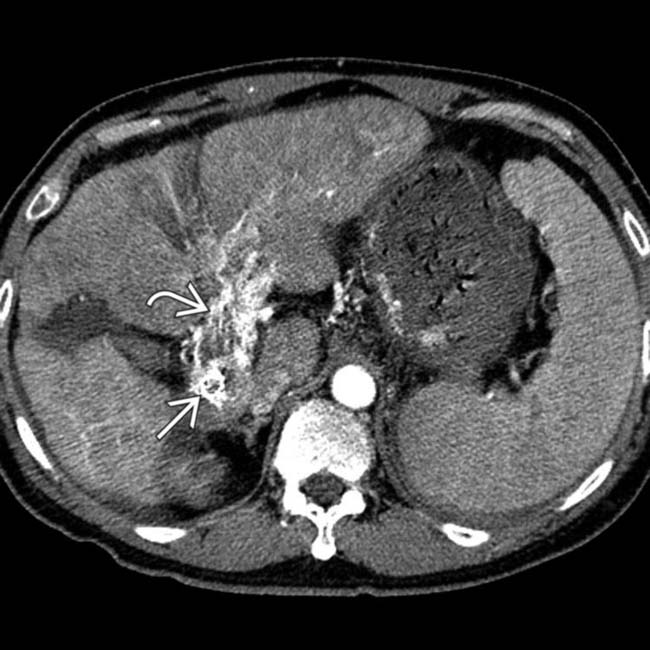
 lying within a massively dilated portal vein that was distended with contrast-enhancing tumor thrombus
lying within a massively dilated portal vein that was distended with contrast-enhancing tumor thrombus  .
.
 and contrast washout from the portal vein tumor thrombus
and contrast washout from the portal vein tumor thrombus  along with the primary HCC that fills the left lobe of the liver
along with the primary HCC that fills the left lobe of the liver  .
.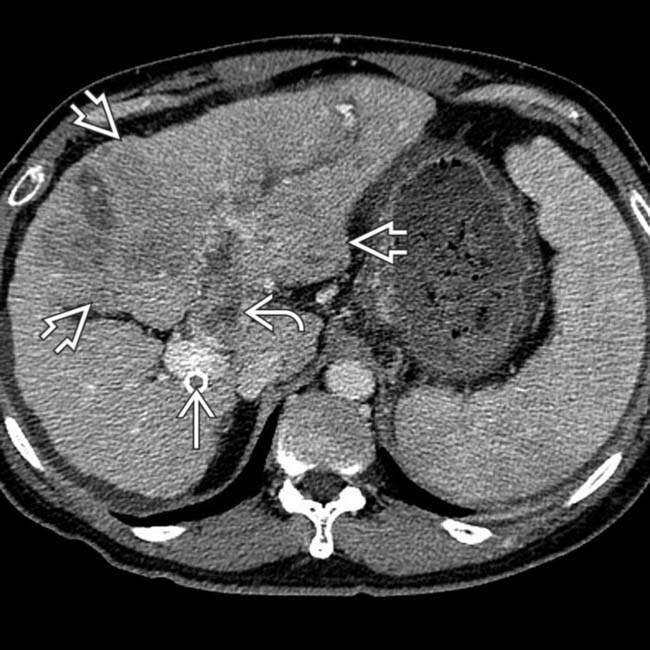
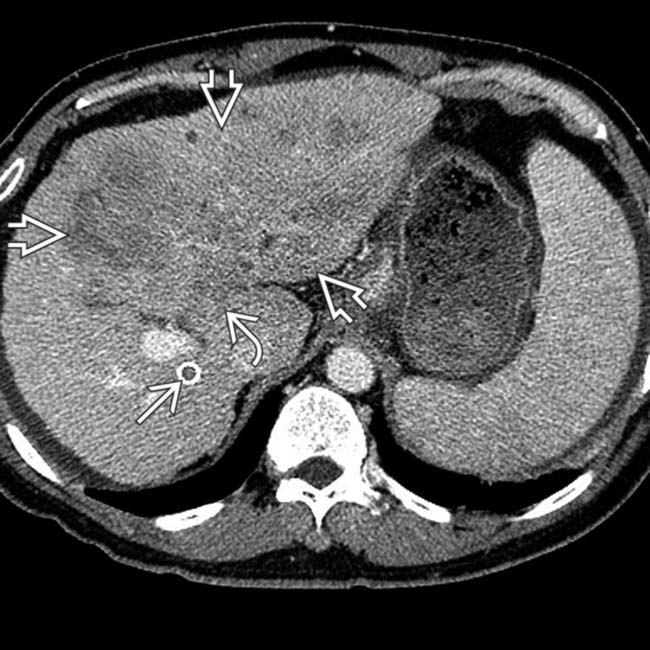
 entering the portal vein, along with the primary HCC
entering the portal vein, along with the primary HCC  and its extension into the left portal vein
and its extension into the left portal vein  .
.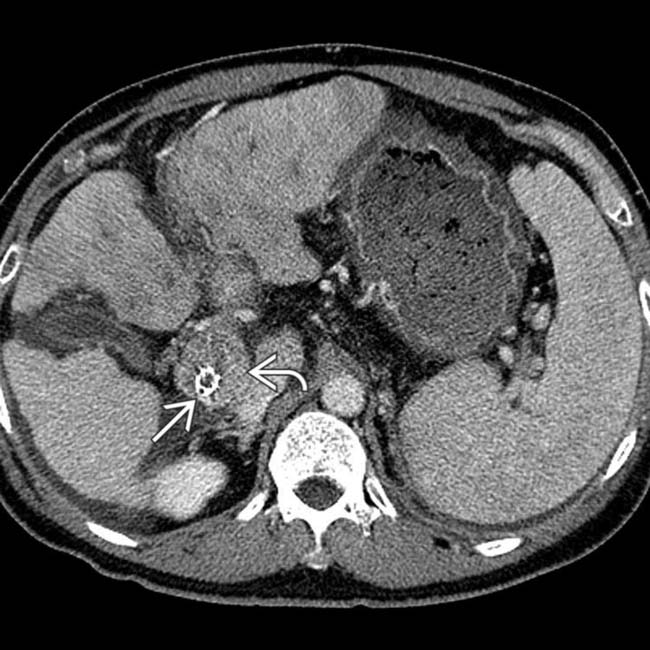
 embedded within a tumor thrombus
embedded within a tumor thrombus  that distends the main portal vein.
that distends the main portal vein.




























































 due to a combination of clot and intimal fibroplasia. The shunt was successfully revised with balloon dilation.
due to a combination of clot and intimal fibroplasia. The shunt was successfully revised with balloon dilation.


