CHAPTER 317 Transient Quadriparesis and Athletic Injuries of the Cervical Spine
Epidemiology and Significance
Sporting events rank as the fourth most common cause of spinal cord injury, behind motor vehicle crashes, violence, and falls, and up to 7% of all spinal cord injuries have been reported to be related to athletics.1–4 These injuries most commonly occur in younger patients and are the second most common cause of spinal cord injury in the first three decades of life.4,5
The National Center for Catastrophic Sports Injury Research (NCCSIR) has defined a catastrophic sports injury as “any severe spinal, spinal cord, or cerebral injury incurred during participation in a school/college sponsored sport.”3 Sporting injuries may be broadly classified as either direct or indirect. Direct injuries result from participating in the sport, whereas indirect injuries result from systemic failure caused by exertion while participating in the sport.3,4 Indirect injuries are frequently related to underlying cardiopulmonary conditions, including cardiac arrhythmia, coronary artery disease, and hypertrophic cardiomyopathy. Within each category, injuries can be subclassified as serious, nonfatal, and fatal.6 Serious injuries include significant injuries that do not result in a permanent functional disability, such as a spinal fracture that does not result in neurological deficit. Nonfatal injuries include injuries that are severe and have resulting permanent functional disability.
According to the NCCSIR, the incidence of direct and indirect catastrophic injuries for all sports is about 1 of every 100,000 high school and 4 of every 100,000 college athletes.3 These injuries result in fatality rates of 0.40 of every 100,000 high school and 1.42 of every 100,000 college athletes.3
Cervical spine injuries related to sports have been reported at many different levels of participation, ranging from unsupervised activities to organized contact and collision sports.7 Cervical trauma has the potential to lead to devastating and irreversible neurological consequences for the player-athlete. Improvements in protective equipment, rule changes, and immediate postinjury care have lowered the incidence of complete quadriplegia among high school and college athletes from 2.5 per 100,000 in 1976 to 0.5 per 100,000 in 1991.8
Although athletic injuries have been reported in a variety of sports, including weightlifting, rugby, diving, surfing, skiing, gymnastics, and boxing, football is associated with the greatest number of direct, catastrophic injuries of all team sports.4 Up to 15% of football players experience a cervical spine injury at some point during play or practice, which may include injuries of the spinal column, spinal cord, or nerve roots.4,9 Linemen, defensive ends, and linebackers are disproportionately prone to these injuries. An increased number of cervical injuries are also encountered among players on special teams, in which players are frequently subject to high-speed collisions.10 In addition, up to 50% of football players with a history of neck trauma have been demonstrated to have radiographic changes, including compression fractures, abnormal motion segments, and disk disease.11
Predisposing Factors
Certain conditions may predispose the athlete to injury. Athletes with a congenitally narrow cervical vertebral canal may be at higher risk for transient quadriplegia. The Torg ratio, a radiographic measure comparing the spinal canal diameter to the vertebral body width, was developed as a marker of spinal stenosis, with a ratio of 0.8 or less indicating severe cervical stenosis and suggesting that a participant was at increased risk for neurological injury.9,12,13 However, among 124 professional football players and 100 rookie football players, 32% of the professional football players and 34% of the rookies had a sagittal canal–to–vertebral body ratio of less than 0.80 at one or more levels from C3 to C6.9 Herzog and colleagues have reported that the Torg ratio has a poor positive predictive value for the presence of true spinal stenosis.14 Because of this factor, as well as the fact that the Torg ratio was studied primarily in professional athletes, it is not commonly used today to determine safety for athletic competition.7
A number of syndromic disorders have been reported to predispose to increased risk for cervical injury. Up to 40% of athletes with Down syndrome demonstrate occipitocervical and atlantoaxial instability owing to increased ligamentous laxity, which would be expected to place them at increased risk for cervical spinal cord injury. However, this theoretically increased risk has not been confirmed in reports of children with Down syndrome in sporting activities when compared with age-matched controls.15,16 Patients with achondroplasia often have multiple levels of cervical spine stenosis, which may be particularly prominent at the foramen magnum. Individuals with achondroplasty have been reported to be at increased risk for spinal cord injury with hyperflexion and hyperextension.15 In addition, atlantoaxial instability is associated with type VI mucopolysaccharidosis (Maroteaux-Lamy syndrome), and atlantoaxial rotatory subluxation may be seen in patients with Marfan’s syndrome.16,17
Anatomic Considerations and Biomechanics
A basic understanding of spinal developmental anatomy and biomechanics is important in managing the injured athlete. The first two cervical vertebrae have characteristic patterns of development.18 Three primary ossification sites contribute to the formation of the atlas (C1). These include a single anterior arch and two neural arches, which subsequently fuse to form the posterior arch. Ossification of the anterior arch typically occurs by 1 year of age but is present in up to 20% of cases at birth.18 Although the neural arches develop in the seventh fetal week, they do not fuse with the anterior arch until later in childhood, typically by 7 years of age. Before these arches fuse, forming the complete C1 ring, this apparent lack of fusion may be readily mistaken for a fracture.18–20 Posterior fusion of the neural arches typically occurs by 3 years of age. In the event that the anterior ossification center fails to form, the neural arches may attempt to fuse anteriorly. This anomaly typically can be distinguished from a fracture based on the presence of sclerotic margins.18,21
Development of the axis (C2) is the most complex of all vertebrae.18 At birth, the axis consists of four ossification centers, including two for the neural arches and one each for the body and odontoid process. The ossification center for the odontoid process forms in utero from the fusion of two ossification centers by the seventh fetal month. In addition, between 3 and 6 years of age, a secondary ossification center forms at the tip of the odontoid process (os terminale) and typically fuses by 12 years of age.18 Fusion of the odontoid process to the body of C2 typically occurs by 3 to 6 years of age. A remnant of this fusion line, termed the subdental synchondrosis, may be apparent at up to 11 years of age and may easily be mistaken for a fracture. By 3 years of age, the neural arches typically fuse posteriorly, and between 3 and 6 years of age, these arches fuse with the body and odontoid process.18
The vertebrae of the subaxial cervical spine share a similar developmental pattern.18 Each vertebra develops from three primary ossification centers, one for the body and one each for two neural arches. Typically, by 2 to 3 years of age, the neural arches fuse, and over the next 3 years, the arches fuse with the body. Secondary ossification centers contribute to the formation of the transverse and spinous processes and may also be present at the superior and inferior edges of the bodies. Secondary ossification centers may be mistaken for fractures because they may remain unfused into the third decade of life.
The craniocervical junction is vulnerable to traumatic injury, and an appreciation of the bony and ligamentous anatomy of this region is important for understanding the mechanisms of injury.18 The cephalad edge of C1 is connected to the foramen magnum by paired anterior and posterior atlanto-occipital membranes. The anterior aspect of the dens is attached to the anterior arch of C1 by the atlantoaxial ligament. The posterior longitudinal ligament extends in a cephalad direction as the tectorial membrane and provides attachment of the cervical spine to the foramen magnum. The transverse ligament extends laterally from tubercle to tubercle along the inner aspect of the anterior arch of C1 and provides approximation of the atlas to the dens. The apical ligament extends from the tip of the odontoid process to the anterior edge of the foramen magnum. The alar ligaments extend between the sides of the dens and the tubercles on the medial aspects of the occipital condyles. Because the alar ligaments serve to limit the degree of contralateral rotation, a tear produces an increased range of motion to the contralateral side and may result in rotational instability.
Cervical spine injury patterns and vulnerabilities vary between the immature and mature spine.18 The adult cervical spine has a fulcrum of motion centered at the C5-C6 level. In contrast, the pediatric cervical spine has a fulcrum of motion that is centered at C2-C3,18,22,23 resulting in a greater risk for occipitocervical and high cervical injuries. This more cephalad fulcrum predisposes children to injuries in the occiput to C3 region. In addition, the pediatric cervical spine in general is predisposed to instability by a number of factors, including a relatively large head, hypermobility owing to increased ligamentous laxity, incomplete ossification of the dens, relatively weak neck muscles, and shallow facet joints.18,19,23–25 As the cervical spine matures, its fulcrum gradually descends to the C3-C5 level in 8- to 12-year-old children, and ultimately descends to the C5-C6 level in adolescents and adults.
Mechanisms of Injury
Lateral Bending
When excessive lateral bending forces are applied to the cervical spine, exiting nerve roots may be subjected to considerable compressive and tractional forces.26 Although a connective tissue layer surrounds the exiting cervical nerve roots and provides some degree of protection, these roots remain vulnerable and are common sources of symptoms in the injured athlete. When nerve roots are subjected to tractional forces, the force is distributed along the length of the root. However, once the elastic limit of the nerve and associated connective tissue is reached, partial or complete disruption may occur. A stinger, an example of neurapraxia (see later), is a common example of a neurological sporting injury that results from excessive traction on neural tissue.
Axial Loading
Axial loading refers to compressive forces applied along a vector parallel to the axis. Resulting fractures commonly affect the region of the fulcrum, C5-C6 in adults and C2-C3 in children. These injuries are typically stable because it is uncommon for pure axial forces, in the absence of rotational or sheer forces, to produce dislocation.27
Considerable attention has been directed toward addressing excessive axial loading forces in athletics because it remains a common mechanism of cervical injuries. About half of the 209 football injuries resulting in permanent quadriplegia between 1971 and 1975 were attributed to axial loading forces.1 The cervical spine loses considerable buffering capacity when the head is lowered. In the lowered position, the cervical spine loses the lordotic contour that provides maximal ability of the vertebral bodies, disks, and cervical soft tissues to absorb and dissipate force. The result is a biomechanically compromised cervical spine that is vulnerable to angulation or hyperflexion to release energy. The result is often intervertebral disk space injury, vertebral body fractures, or ligamentous injury. Biomechanical studies suggest that the axial load limits of the cervical spine in young adults is between 3340 and 4450 Newtons, which can be readily approached with a fast walk when the head is lowered.28,29
Axial loading injuries are often avoidable and have received the most attention in football, where they can occur when an athlete intentionally uses the crown of the helmet as a point of contact (“spearing”). On this basis, most professional, college, and high school football leagues have banned both deliberate spearing and the use of the top of the helmet as the initial point of contact when making a tackle. After these rule changes, a marked decrease in cervical spine injury rates occurred.30
Rotation
Because of the oblique relationship of the superior and inferior articulating processes of the cervical facets, lateral bending forces in the cervical spine are typically associated with a rotational force. Most rotational motion in the cervical spine is facilitated by the atlas and axis. Extremes of rotation at this interface can produce neurological and vascular compromise. For example, with leftward rotation of the atlas, the right transverse foramen of the atlas moves in a posterior direction. With extremes of rotation, increased stretch is applied to the vertebral arteries and spinal nerves. In severe cases, this may result in compromised brainstem or spinal cord circulation and has most commonly been described in wrestlers.31–35
Dislocation and Subluxation
In a study examining the incidence of quadriplegia in athletes, Eismont and associates demonstrated a higher likelihood of quadriplegia in patients with cervical stenosis following cervical fracture-dislocation.36 Other authors have also described minor trauma, such as falls or minor motor vehicle collisions, that could cause permanent quadriplegia in people with marked developmental cervical stenosis, although the degree of stenosis that should be considered critical is controversial.4,37
Transient Quadriplegia and Common Neurological Syndromes Associated with Athletics
A classification system has been proposed for the evaluation and treatment of athletes with cervical spine injuries, which divides injuries into three categories.38 Type 1 injuries are those in patients who suffer permanent spinal cord dysfunction. These include patients with a complete spinal cord injury or incomplete lesions (e.g., anterior cord syndrome). Type 2 injuries are transient spinal cord injuries, such as spinal concussion or neurapraxia. Type 3 injuries consist of disorders involving radiologic abnormalities without neurological deficit. A brief overview of these injuries is provided next.
Transient Quadriparesis
Several terms have been used interchangeably to describe the condition of acute, transient sensory changes of at least two extremities and may also include motor deficit. These terms have included transient quadriplegia, spinal cord concussion, and cervical cord neurapraxia.4,39 Various mechanisms for these deficits have been proposed, including axial loading, hyperflexion, hyperextension, or a combination of the three.10,39
The features of transient quadriparesis have been recognized for more than 130 years. In 1879, Obersteiner was the first to report this neurological phenomenon and referred to it as a spinal cord concussion.40 In the 1940s, it was suggested that the injury is due to spinal cord neural transmission failure,41,42 and in the 1960s, Penning proposed that the mechanism of injury is related to sudden spinal cord compression between the posterior inferior cervical vertebral body and the subjacent spinal lamina.43
Episodes of neurapraxia typically occur acutely in association with a traumatic event and may include both sensory changes, such as burning pain, numbness, and tingling, and motor changes, which may range from weakness to paralysis. Although it is more common for there to be complete recovery within a few minutes, events may gradually resolve over a period of up to 48 hours.44 Except for burning paresthesia, pain in the neck is usually not present at the time of injury, and there is complete return of motor function and full, pain-free motion of the cervical spine. Routine radiographs of the cervical spine are typically negative for fractures or dislocations, although it is not uncommon for radiographs to show developmental spinal stenosis, congenital fusion, cervical instability, or intervertebral disk disease.10,45
It is difficult to estimate the true prevalence of cervical neurapraxia owing to underreporting of its occurrence and its transient presence.4 In 1986, Torg and Pavlov studied 39,377 players during the 1984 National Collegiate Athletic Association (NCAA) college football season and reported the incidence of transient paresthesia in all four extremities to be 6 per 10,000 athletes, whereas the incidence of paresthesias associated with transient quadriplegia was 1.3 per 10,000 athletes.39 In addition, Torg and colleagues reported the overall recurrence of cervical neurapraxia in athletes who returned to play to be 56%, with increased recurrence risk being correlated with decreased sagittal canal diameter.46
The question of return to play in patients with neurapraxia is highly controversial.4 In Torg’s study, 63 of the 109 (58%) athletes returned to contact sports in this study after one episode of neurapraxia, although the risk for permanent quadriplegia was not definitively related to the development of neurapraxia.46,47 These data, however, have been contradicted by other groups.48 The ultimate answer to this question will rely on a multi-institutional collaborative effort because the number of athletes who suffer transient quadriparesis (1 in 200,000) is so low that most small studies do not provide accurate statistical power.10 Despite this, some groups have developed guidelines for management of neurapraxia, with the caveat that each patient must be dealt with on a case-by-case basis.29
Spinal Cord Injury without Radiographic Abnormality
The phenomenon of spinal cord injury without radiographic abnormality (SCIWORA) has been well described18,49 and consists of spinal cord injury in the setting of no apparent abnormalities on conventional radiography or computed tomography (CT). SCIWORA has been more commonly appreciated in children, possibly owing to the increased ligamentous laxity of the pediatric spine. In SCIWORA, substantial spinal cord injury may exist without apparent radiographic abnormality. This is thought to result from transient ligamentous deformation of the cervical spine, but the mechanism by which this produces SCIWORA remains unclear.18 Because the spinal cord is less elastic than the spinal column, the spinal cord may be more vulnerable to injury with deformation.18,22,50–54 Spinal ischemia may also account for SCIWORA, either through direct injury of spinal vessels or through hypoperfusion of the spinal cord.50,55
Stingers
A stinger is typically characterized by unilateral upper extremity burning dysesthesia that may be associated with motor weakness. The C5 and C6 nerve roots are most commonly affected, which can result in weakness of the deltoid and biceps muscles as well as a stinging sensation extending from the neck to the fingertips. Stingers are typically self-limited and resolve within minutes to hours, but less commonly symptoms may persist longer.56 Stingers disproportionately affect athletes participating in contact sports, and among these players, the incidence may be as high as 50%.57 Meyer and colleagues studied 266 college football players and reported a lower mean Torg ratio among players with a history of stingers compared with players lacking such a history.58
Stingers may result from direct traumatic injury to the cervical nerve roots or brachial plexus or may result from traction injury to these neural structures from hyperextension of the cervical spine.56 Stingers may also present concurrently with spinal cord injury. Thus, the examiner of a patient suffering a suspected stinger should assess the level of involvement based on the symptoms and findings. Nerve root involvement is suggested by pain in a dermatomal pattern that may include deficits of the muscles innervated by the corresponding nerve root. In contrast, involvement of more than one dermatome or weakness of more than one major muscle group is more consistent with brachial plexus involvement. Spinal cord injury should be suspected if the symptoms are bilateral, involve one or both of the lower extremities, include long tract signs, or affect bladder or sexual function. Although not typically diagnostic until at least 3 weeks after injury, electromyography can be useful in distinguishing among nerve root, plexus, and spinal cord injuries.
On-Field Evaluation and Management of the Athlete with Suspected Cervical Injury
Consideration of the mechanism of injury is an important step in the on-field assessment of the injured athlete. An athlete suffering from a major spinal injury may not immediately present with focal neurological signs or symptoms, and in these cases, initial assessment of the cervical spine may be difficult.1 While still on the field, the prevention of further injury is the single most important objective.44
Several groups have attempted to determine the optimal position for the cervical spine to allow the maximal amount of space for the spinal cord. The head and neck should be held in neutral position to immobilize the spine during the primary survey. De Lorenzo and colleagues, used MRI to assess the position of the cervical spine that maximizes cross-sectional area of the spinal canal versus the spinal cord.59 Maximal area was produced when the neck was in slight flexion, which corresponded to raising the occiput by about 2 cm. Because they can serve as sites of neutral traction, protective gear such as shoulder pads, helmet, and chin strap should not be removed.44
Following this, the physician, in sequence, should assess respiration, circulation, and level of consciousness.44 Patients with impaired mental status tend to have the highest risk for injury and should be immobilized immediately. Once the initial survey has been completed, the patient should be transferred to a rigid spine board. The transfer can be performed using a log-roll, or using a scoop-stretcher, which lifts the athlete up while the spine board is slid underneath.
Physical examination should include a thorough examination of the nervous system, including reflexes and rectal tone. Unexplained hypotonia or hypertonia or any abnormal neurological examination findings in the setting of minor trauma are relative indications for imaging of the cervical spine. The most common symptoms of pediatric cervical spine injury are neck pain and torticollis.60
If the patient is medically unstable, cross-table lateral radiography may be performed until the patient’s condition permits complete evaluation of the cervical spine.61 The false-negative rate for a single cross-table lateral radiograph ranges from 21% to 26%; therefore, complete evaluation with either conventional radiography or CT may be necessary. CT with multiplanar reformatting has a crucial role in the assessment of cervical spine injury. CT delineates the bone detail of the cervical spine and demonstrates fractures and the extent of bone injury far better than does MRI.62 MRI is helpful in the evaluation of trauma-related spinal cord injury. MRI facilitates evaluation of the extradural spaces and of the integrity of the spinal ligaments. Increased interspinous distance, divergence of the articular processes, and widening of the posterior aspect of the disk space are indicative of cervical spine instability.
Return to Play
The decision about whether the injured athlete can return to playing sports is complex and must be considered on an individual basis, after the extent of the spine injury as well as all other injuries are assessed.63 There are often significant extrinsic pressures on the health care providers to clear an athlete to play, particularly when their livelihood is related to the sport. Because resumption of play may put the patient at risk for catastrophic injury in the future, the decision must be made with complete objectivity.
Watkins proposed a point grading system to quantitatively assess player risk with return to play following cervical injury.29 Cantu and colleagues recommend that before return to play, the athlete should have no neck tenderness or spasm, neck or arm pain, numbness, paresthesias, or weakness, either at rest, with full range of motion, or on axial compression.1 Vaccaro and associates recently reviewed and published absolute and relative contraindications to play following cervical spine injury.7
Case 317-1
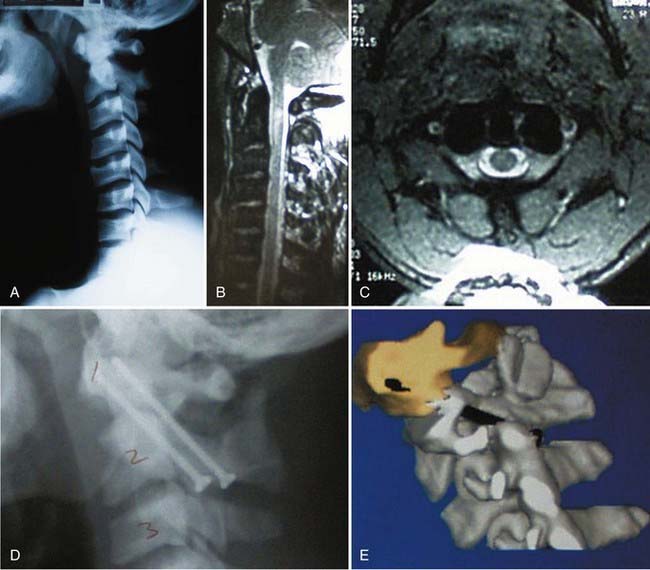
A 24-year-old professional football player suffered quadriplegia following a tackle during play. Neurological function gradually improved over about 5 hours, with a residual severe central cord syndrome. Radiographic imaging demonstrated lack of apparent cervical fracture or dislocation (Fig. E317-1A). MRI revealed rupture of the transverse ligament and abnormal T2 signal in the spinal cord at the level of C2 (Fig. E317-1B and C). C1-2 transarticular screw fixation was performed for stabilization (Fig. E317-1D and E). At last follow-up, he continued to have only mild hand weakness.
Case 317-2
A 20-year-old college-level football player presented after an episode of transient quadriplegia following a head-down tackle. He had persistent neck and left shoulder pain and paresthesias. Radiographic cervical spine imaging did not demonstrate any fractures or dislocations (Fig. E317-2A). MRI showed a C3-4 disk protrusion eccentric to the left side with associated cord T2 signal change (Fig. E317-2B and C). MRI STIR sequences were negative, suggesting lack of ligamentous injury. He underwent a C3-4 anterior cervical diskectomy and fusion with allograft and plating (Fig. E317-2D). His symptoms continued to gradually improve, and he subsequently returned to playing football.
Bailes JE, Maroon JC. Management of cervical spine injuries in athletes. Clin Sports Med. 1989;8:43-58.
Boden BP. Direct catastrophic injury in sports. J Am Acad Orthop Surg. 2005;13:445-454.
Boden BP, Tacchetti RL, Cantu RC, et al. Catastrophic cervical spine injuries in high school and college football players. Am J Sports Med. 2006;34:1223-1232.
Brigham CD, Adamson TE. Permanent partial cervical spinal cord injury in a professional football player who had only congenital stenosis. A case report. J Bone Joint Surg Am. 2003;85:1553-1556.
Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg. 2001;36:1107-1114.
Cantu RC. Cervical spine injuries in the athlete. Semin Neurol. 2000;20:173-178.
Cantu RV, Cantu RC. Guidelines for return to contact sports after transient quadriplegia. J Neurosurg. 1994;80:592-594.
Clancy WGJr, Brand RL, Bergfield JA. Upper trunk brachial plexus injuries in contact sports. Am J Sports Med. 1977;5:209-216.
Dickman CA, Zabramski JM, Rekate HL, Sonntag VK. Spinal cord injuries in children without radiographic abnormalities. West J Med. 1993;158:67-68.
Eismont FJ, Clifford S, Goldberg M, Green B. Cervical sagittal spinal canal size in spine injury. Spine. 1984;9:663-666.
Gill SS, Boden BP. The epidemiology of catastrophic spine injuries in high school and college football. Sports Med Arthrosc. 2008;16:2-6.
Herzog RJ, Wiens JJ, Dillingham MF, Sontag MJ. Normal cervical spine morphometry and cervical spinal stenosis in asymptomatic professional football players. Plain film radiography, multiplanar computed tomography, and magnetic resonance imaging. Spine. 1991;16:S178-S186.
Hill SA, Miller CA, Kosnik EJ, Hunt WE. Pediatric neck injuries. A clinical study. J Neurosurg. 1984;60:700-706.
Levitz CL, Reilly PJ, Torg JS. The pathomechanics of chronic, recurrent cervical nerve root neurapraxia. The chronic burner syndrome. Am J Sports Med. 1997;25:73-76.
Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539-560.
Maroon JC, Bailes JE. Athletes with cervical spine injury. Spine. 1996;21:2294-2299.
Meyer SA, Schulte KR, Callaghan JJ, et al. Cervical spinal stenosis and stingers in collegiate football players. Am J Sports Med. 1994;22:158-166.
Pang D, Wilberger JEJr. Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1982;57:114-129.
Torg JS, Corcoran TA, Thibault LE, et al. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. J Neurosurg. 1997;87:843-850.
Torg JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal cord with transient quadriplegia. J Bone Joint Surg Am. 1986;68:1354-1370.
Torg JS, Quedenfeld TC, Moyer RA, et al. Severe and catastrophic neck injuries resulting from tackle football. J Am Coll Health Assoc. 1977;25:224-226.
Torg JS, Truex RCJr, Marshall J, et al. Spinal injury at the level of the third and fourth cervical vertebrae from football. J Bone Joint Surg Am. 1977;59:1015-1019.
Torg JS, Truex RJr, Quedenfeld TC, et al. The National Football Head and Neck Injury Registry. Report and conclusions 1978. JAMA. 1979;241:1477-1479.
Torg JS, Vegso JJ, Sennett B, Das M. The National Football Head and Neck Injury Registry. 14-year report on cervical quadriplegia, 1971 through 1984. JAMA. 1985;254:3439-3443.
Vaccaro AR, Klein GR, Ciccoti M, et al. Return to play criteria for the athlete with cervical spine injuries resulting in stinger and transient quadriplegia/paresis. Spine J. 2002;2:351-356.
1 Cantu RC. Cervical spine injuries in the athlete. Semin Neurol. 2000;20:173-178.
2 Cantu RC. Functional cervical spinal stenosis: a contraindication to participation in contact sports. Med Sci Sports Exerc. 1993;25:316-317.
3 Center NSCIS. Spinal Cord Information Network: Facts and Figures at a Glance. University of Alabama at Birmingham. http://www.ncddr.org/rpp/hf/hfdw/mscis/nscisc.html, 2003. Available at
4 Gill SS, Boden BP. The epidemiology of catastrophic spine injuries in high school and college football. Sports Med Arthrosc. 2008;16:2-6.
5 Molsa JJ, Tegner Y, Alaranta H, et al. Spinal cord injuries in ice hockey in Finland and Sweden from 1980 to 1996. Int J Sports Med. 1999;20:64-67.
6 Boden BP. Direct catastrophic injury in sports. J Am Acad Orthop Surg. 2005;13:445-454.
7 Vaccaro AR, Klein GR, Ciccoti M, et al. Return to play criteria for the athlete with cervical spine injuries resulting in stinger and transient quadriplegia/paresis. Spine J. 2002;2:351-356.
8 Clarke KS. Epidemiology of athletic neck injury. Clin Sports Med. 1998;17:83-97.
9 Torg JS, Truex RJr, Quedenfeld TC, et al. The National Football Head and Neck Injury Registry. Report and conclusions 1978. JAMA. 1979;241:1477-1479.
10 Boden BP, Tacchetti RL, Cantu RC, et al. Catastrophic cervical spine injuries in high school and college football players. Am J Sports Med. 2006;34:1223-1232.
11 Albright JP, Moses JM, Feldick HG, et al. Nonfatal cervical spine injuries in interscholastic football. JAMA. 1976;236:1243-1245.
12 Torg JS, Quedenfeld TC, Moyer RA, et al. Severe and catastrophic neck injuries resulting from tackle football. J Am Coll Health Assoc. 1977;25:224-226.
13 Torg JS, Truex RCJr, Marshall J, et al. Spinal injury at the level of the third and fourth cervical vertebrae from football. J Bone Joint Surg Am. 1977;59:1015-1019.
14 Herzog RJ, Wiens JJ, Dillingham MF, Sontag MJ. Normal cervical spine morphometry and cervical spinal stenosis in asymptomatic professional football players. Plain film radiography, multiplanar computed tomography, and magnetic resonance imaging. Spine. 1991;16:S178-S186.
15 Birrer RB. The Special Olympics athlete: evaluation and clearance for participation. Clin Pediatr. 2004;43:777-782.
16 McCormick DP, Niebuhr VN, Risser WL. Injury and illness surveillance at local Special Olympic Games. Br J Sports Med. 1990;24:221-224.
17 Pizzutillo PD. Spinal considerations in the young athlete. Instr Course Lect. 1993;42:463-472.
18 Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539-560.
19 Herman MJ, Pizzutillo PD. Cervical spine disorders in children. Orthop Clin North Am. 1999;30:457-466. ix
20 Ogden JA. Radiology of postnatal skeletal development. XI. The first cervical vertebra. Skeletal Radiol. 1984;12:12-20.
21 Ogden JA. Skeletal injury in the child. In Spine, 2nd ed, Philadelphia: Saunders; 1990:571.
22 Kokoska ER, Keller MS, Rallo MC, Weber TR. Characteristics of pediatric cervical spine injuries. J Pediatr Surg. 2001;36:100-105.
23 Roche C, Carty H. Spinal trauma in children. Pediatr Radiol. 2001;31:677-700.
24 McGrory BJ, Klassen RA, Chao EY, et al. Acute fractures and dislocations of the cervical spine in children and adolescents. J Bone Joint Surg Am. 1993;75:988-995.
25 Reynolds R. Pediatric spinal injury. Curr Opin Pediatr. 2000;12:67-71.
26 Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg. 2001;36:1107-1114.
27 Torg JS, Vegso JJ, Sennett B, Das M. The National Football Head and Neck Injury Registry. 14-year report on cervical quadriplegia, 1971 through 1984. JAMA. 1985;254:3439-3443.
28 Ladd AL, Scranton PE. Congenital cervical stenosis presenting as transient quadriplegia in athletes. Report of two cases. J Bone Joint Surg Am. 1986;68:1371-1374.
29 Watkins RG. Neck injuries in football players. Clin Sports Med. 1986;5:215-246.
30 Hill SA, Miller CA, Kosnik EJ, Hunt WE. Pediatric neck injuries. A clinical study. J Neurosurg. 1984;60:700-706.
31 Feipel V, Salvia P, Klein H, Rooze M. Head repositioning accuracy in patients with whiplash-associated disorders. Spine. 2006;31:E51-E58.
32 Logan PM, O’Rourke K, Gibney RG. Case of the month: atlanto-axial rotatory fixation. Br J Radiol. 1995;68:93-94.
33 Weinstein SM, Cantu RC. Cerebral stroke in a semi-pro football player: a case report. Med Sci Sports Exerc. 1991;23:1119-1121.
34 Wennemer HK, Borg-Stein J, Gomba L, et al. Functionally oriented rehabilitation program for patients with fibromyalgia: preliminary results. Am J Phys Med Rehabil. 2006;85:659-666.
35 Ylinen JJ, Julin M, Rezasoltani A, et al. Effect of training in Greco-Roman wrestling on neck strength at the elite level. J Strength Cond Res. 2003;17:755-759.
36 Eismont FJ, Clifford S, Goldberg M, Green B. Cervical sagittal spinal canal size in spine injury. Spine. 1984;9:663-666.
37 Firooznia H, Ahn JH, Rafii M, Ragnarsson KT. Sudden quadriplegia after a minor trauma. The role of preexisting spinal stenosis. Surg Neurol. 1985;23:165-168.
38 Maroon JC, Bailes JE. Athletes with cervical spine injury. Spine. 1996;21:2294-2299.
39 Torg JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal cord with transient quadriplegia. J Bone Joint Surg Am. 1986;68:1354-1370.
40 Obersteiner H. Uber erschutterung des Ruckenmarks. Wein Med Jahrb. 1879;34:531.
41 Denny-Brown D, Russell WR. Experimental cerebral concussion. J Physiol. 1940;99:153.
42 Groat RA, Rambach WAJ, Windle WF. Concussion of the spinal cord: an experimental study and a critique of the use of the term. Surg Gynecol Obstet. 1945:63-74.
43 Penning L. Some aspects of plain radiography of the cervical spine in chronic myelopathy. Neurology. 1962;12:513-519.
44 Bailes JE, Maroon JC. Management of cervical spine injuries in athletes. Clin Sports Med. 1989;8:43-58.
45 Boden BP, Tacchetti RL, Cantu RC, et al. Catastrophic head injuries in high school and college football players. Am J Sports Med. 2007;35:1075-1081.
46 Torg JS, Corcoran TA, Thibault LE, et al. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. J Neurosurg. 1997;87:843-850.
47 Cantu RV, Cantu RC. Guidelines for return to contact sports after transient quadriplegia. J Neurosurg. 1994;80:592-594.
48 Brigham CD, Adamson TE. Permanent partial cervical spinal cord injury in a professional football player who had only congenital stenosis. A case report. J Bone Joint Surg Am. 2003;85:1553-1556.
49 Pang D, Wilberger JEJr. Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1982;57:114-129.
50 Akbarnia BA. Pediatric spine fractures. Orthop Clin North Am. 1999;30:521-536. x
51 Dickman CA, Zabramski JM, Rekate HL, Sonntag VK. Spinal cord injuries in children without radiographic abnormalities. West J Med. 1993;158:67-68.
52 Kewalramani LS, Tori JA. Spinal cord trauma in children. Neurologic patterns, radiologic features, and pathomechanics of injury. Spine. 1980;5:11-18.
53 Kriss VM, Kriss TC. SCIWORA (spinal cord injury without radiographic abnormality) in infants and children. Clin Pediatr. 1996;35:119-124.
54 Leventhall H. Birth injuries of the spinal cord. J Pediatr. 1960;56:447-453.
55 Choi JU, Hoffman HJ, Hendrick EB, et al. Traumatic infarction of the spinal cord in children. J Neurosurg. 1986;65:608-610.
56 Levitz CL, Reilly PJ, Torg JS. The pathomechanics of chronic, recurrent cervical nerve root neurapraxia. The chronic burner syndrome. Am J Sports Med. 1997;25:73-76.
57 Clancy WGJr, Brand RL, Bergfield JA. Upper trunk brachial plexus injuries in contact sports. Am J Sports Med. 1977;5:209-216.
58 Meyer SA, Schulte KR, Callaghan JJ, et al. Cervical spinal stenosis and stingers in collegiate football players. Am J Sports Med. 1994;22:158-166.
59 De Lorenzo RA, Olson JE, Boska M, et al. Optimal positioning for cervical immobilization. Ann Emerg Med. 1996;28:301-308.
60 Gerbino PG. Does football cause an increase in degenerative disease of the lumbar spine? Curr Sports Med Rep. 2002;1:47-51.
61 Buhs C, Cullen M, Klein M, Farmer D. The pediatric trauma C-spine: is the “odontoid” view necessary? J Pediatr Surg. 2000;35:994-997.
62 Graber MA, Kathol M. Cervical spine radiographs in the trauma patient. Am Fam Physician. 1999;59:331-342.
63 Jagannathan J, Dumont AS, Prevedello DM, et al. Cervical spine injuries in pediatric athletes: mechanisms and management. Neurosurg Focus. 2006;21:E6.