Toxoplasmic Chorioretinitis
Clinical Features:
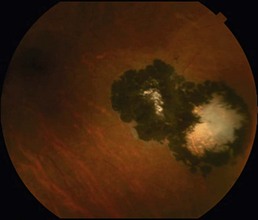
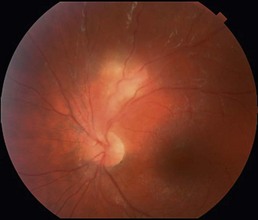
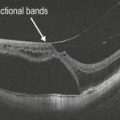
In recurrent cases, there is a characteristic focus of active chorioretinitis with overlying vitritis adjacent to a pigmented chorioretinal scar (Fig. 18.1.1). Associated retinal vasculitis may be present. The disease is almost always unilateral. Primary infection may present with a similar appearance in the absence of a pigmented scar (Fig. 18.1.2). Multifocality and bilaterality are rare except in immunocompromised individuals. In elderly patients, a severe form of toxoplasmosis that is relentlessly progressive, resembling acute retinal necrosis, can occur.
OCT Features:
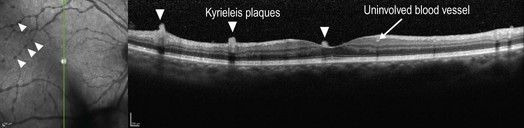
Peripheral lesions are often not amenable to imaging with OCT but if located within or near the macula, OCT reveals thickening and distortion of all the retinal layers and the retinal pigment epithelium (Fig. 18.1.3) within the area of active chorioretinitis. Kyrieleis plaques are a non-specific finding that can be present overlying retinal blood vessels in the setting of vasculitis from toxoplasmic chorioretinitis. These appear as hyper-reflective round outpouchings or plaque-like deposits on the surface of both arteries and veins (Fig. 18.1.4). Choroidal neovascularization can occur secondarily from toxoplasmosis scars and OCT can show associated intraretinal and subretinal fluid.
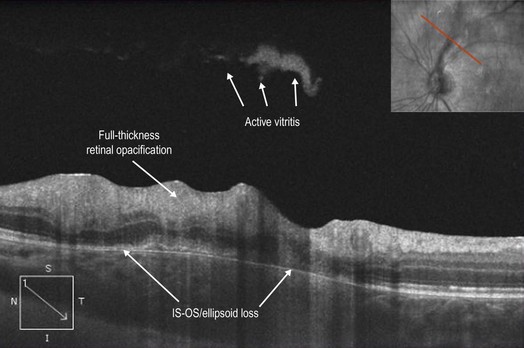
Figure 18.1.3 OCT using enhanced depth imaging protocol (corresponding to Figure 18.1.2) shows distortion and thickening of all retinal layers in the area of active chorioretinitis. The inner retinal layers are more involved and are hyper-reflective. There are patchy areas of IS–OS/ellipsoid zone and retinal pigment epithelium loss. An area of active vitritis is visible.