Total Shoulder Arthroplasty
Chris A. Sebelski and Carlos A. Guanche
Clinical Evaluation
History
The most common complaint in patients with advanced osteoarthritis (OA) of the shoulder is pain—more specifically, night pain. Most often, the pain is insidious in its onset, although an occasional patient will report acute symptomatology only to discover severe osteoarthritic changes in the glenohumeral (GH) joint. In many cases night pain is a major problem; specifically, difficulty with lying on the affected side is a common complaint.1
A careful history should be taken with respect to prior injuries and prior surgical procedures. For a total shoulder replacement to be viable and functional, an intact rotator cuff is necessary. In certain patients with long-standing rotator cuff disruption, the initial clinical signs are progressive pain that comes with the developing secondary arthropathy.2
Another area of concern is whether the patient has undergone any prior stabilization procedures. The reason this is important to remember is that preferential wear of certain parts of the glenoid can occur in long-standing cases that have undergone excessive capsular-tightening procedures.3 Most commonly, this is posterior wear. In addition, in certain types of stabilization procedures, a variety of bony transfer procedures are performed, including a lateralization of the lesser tuberosity and a transfer of the coracoid transfer. As a result, the surgical exposure in these cases can be difficult because of the distorted anatomy.
Physical Examination
The most important predictor of the outcome of a total shoulder replacement is the preoperative range of motion (ROM).4,5 ![]() It is therefore incumbent on the physician to document all directions of the patient’s motion and to discuss the implications of lack of mobility on the overall outcome. Another important aspect is the integrity of the rotator cuff; a successful standard replacement depends very heavily on the presence of an intact cuff. The supraspinatus, infraspinatus, teres minor, and the subscapularis should all be carefully examined. If any doubt exists as to the function of the cuff, magnetic resonance imaging (MRI) is indicated. In cases in which a rotator cuff disruption coexists with severe OA, a determination should be made as to the possibility of repairing the cuff. In those cases in which significant chronicity of the cuff is noted, either by history or MRI examination, a simple hemiarthroplasty or a reverse total shoulder replacement (in cases in which pseudoparalysis of the arm exists) should be considered.6
It is therefore incumbent on the physician to document all directions of the patient’s motion and to discuss the implications of lack of mobility on the overall outcome. Another important aspect is the integrity of the rotator cuff; a successful standard replacement depends very heavily on the presence of an intact cuff. The supraspinatus, infraspinatus, teres minor, and the subscapularis should all be carefully examined. If any doubt exists as to the function of the cuff, magnetic resonance imaging (MRI) is indicated. In cases in which a rotator cuff disruption coexists with severe OA, a determination should be made as to the possibility of repairing the cuff. In those cases in which significant chronicity of the cuff is noted, either by history or MRI examination, a simple hemiarthroplasty or a reverse total shoulder replacement (in cases in which pseudoparalysis of the arm exists) should be considered.6
Surgical Indications And Considerations
Those patients with refractory pain and limitation of motion that do not respond to conservative methods of treatment (i.e., a trial of physical therapy, antiinflammatory medications, activity modification, avoidance of inciting factors, and intraarticular corticosteroid injections) are candidates for shoulder replacement. Ideally, the patient’s age should also fit within the acceptable parameters for a joint replacement. Although the ideal patient should be over the age of 65 and have a relatively limited activity level, the reality is that many patients do not fit such criteria.
In cases in which the patient’s age is significantly under 65 years or the activity level is not commensurate with their age, avoiding the surgery should be considered (in some of these patients, a case can be made for fusion of the joint). In addition, a spectrum of replacement procedures can be used, including a partial humeral replacement (classically termed a hemiarthroplasty), a hemiarthroplasty with a biologic resurfacing of the joint, and a standard total shoulder replacement; in more severe cases of patients with concurrent unrepairable rotator cuff tears, a reverse total shoulder can be used.
Surgical Procedure
The choice of anesthesia depends on the clinical experience of the surgeon and anesthesiologist. Ideally, the anesthesia would include an interscalene block, either by itself or as a supplement to a general anesthetic. The use of such blocks has been shown to significantly affect the patient’s postoperative course in a very positive manner.7 In cases in which interscalene anesthesia is not used, the preemptive administration of a long-acting anesthetic (Marcaine) is also well-founded in the literature and has been shown to positively affect recovery.8
The standard approach to a shoulder replacement operation includes positioning the patient in a semirecumbent (beach chair) position, with a small bolster under the scapula to effectively stabilize the glenoid for exposure. In addition, the operative shoulder should be examined under anesthesia with all of the directions of motion measured and documented. Finally, it is important to ensure that the operative arm can be extended and rotated appropriately for delivery of the humeral head and subsequent resection during the surgical procedure (Fig. 7-1). This is called the ability to shotgun the arm into this position.
The standard incision is a deltopectoral approach that is typically centered immediately lateral to the coracoid process of the scapula and extends down the proximal arm, avoiding the axilla (Fig. 7-2). It is important to allow for distal exposure of the wound should the need arise for a more complex humeral approach, such as in complications associated with humeral shaft fractures on prosthetic insertion.
The exposure includes identification of the deltopectoral interval with identification of the cephalic vein and subsequent medial retraction. The pectoralis tendon is identified laterally and, in severe cases, released for a distance of 1 to 2 cm for improved GH joint exposure. In addition, the deltopectoral interval is exposed in its entirety from the leading edge of the clavicle to the lower end of the pectoralis muscle. Commonly, significant subdeltoid adhesions need to be released for proper delivery of the humeral head out of the wound.
After complete exposure of the deltopectoral interval, the conjoint tendon is identified and released at its proximal portion for a distance of 1 cm, and the medial retractor is placed behind the tendon. Care should be taken to protect the musculocutaneous nerve when performing this maneuver.
The subscapularis tendon is now identified and released from superior to inferior, beginning at its lateral corner. The tendon is released directly off the lesser tuberosity and retracted medially. The release continues inferiorly, cauterizing the vascular leash consisting of the anterior inferior humeral circumflex vessels and proceeding along the inferior humeral head, while externally rotating the humerus (Fig. 7-3). The extent of the release is variable. However, the requirement is that the entire humeral head can be delivered for resection and that adequate exposure of the glenoid is possible if resurfacing of that portion is being performed.
Once the exposure is complete, a variety of humeral resection techniques can be used, depending on the manufacturer’s individual surgical protocol. The design the author of this chapter uses involves resection of the humeral head at its anatomic base. Before completing this cut, the head must be exposed and all peripheral osteophytes should be removed to appropriately resect the head in an anatomic fashion (Fig. 7-4).
After resection of the head, the humeral canal is prepared for the prosthetic device being implanted. A series of reamers are inserted down the medullary canal, stopping when the appropriate-sized device is used. The size is typically judged from templates that measure the size of the medullary canal based on their radiographic dimension. However, ultimately the choice is made intraoperatively, based on the surgeon’s experience as he or she advances the device into the shaft.
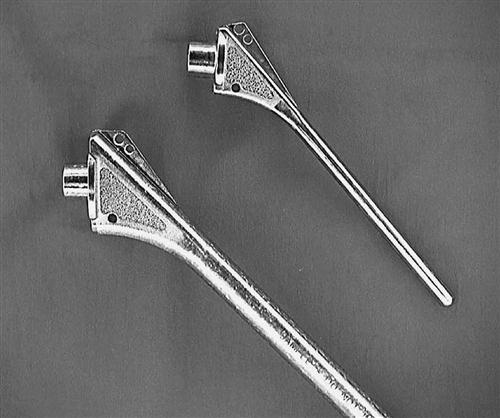
The humeral metaphysis is then prepared with a series of broaches that contour the proximal humerus for insertion of the actual component. The type of implant varies, with two major types being available: (1) cemented and (2) cementless. A cementless device uses the body’s ability to grow bone into some of its surfaces; these surfaces are often prepared with a sintered metal (Fig. 7-5). In a cemented device, the prosthesis is implanted using polymethylmethacrylate cement for immediate fixation of the device. The theoretic advantages of one device over another are beyond the scope of this chapter; the reader is directed to the appropriate references.9–11
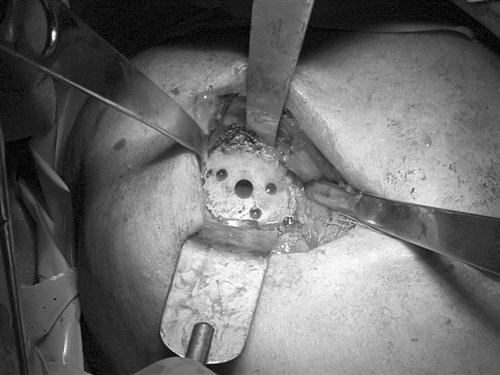
Attention is now directed to the glenoid. It is important to be able to access the entire area of the glenoid from anterior to posterior and superior to inferior to effectively prepare the bony surface for the implant. The capsule of the joint is excised, beginning with the most anterior, superior portion and extending inferiorly and posteriorly as far as necessary to allow for adequate exposure (Fig. 7-6). Once the exposure is gained, the central point of the glenoid is identified; then the surface is prepared for accepting the actual component. Finally, the device is cemented into position using polymethylmethacrylate cement.
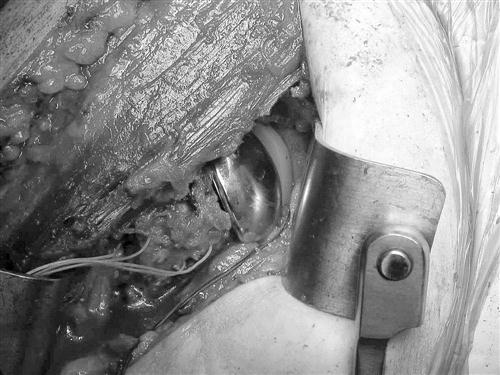
The final decisions that need to be made include choosing the appropriately sized humeral head component to allow a relatively normal passive range of motion (PROM) with minimal to no instability before closure of the subscapularis muscle tendon (Fig. 7-7). Once the appropriate head is chosen and implanted, the subscapularis muscle tendon is reapproximated to the lesser tuberosity with the use of sutures that have been prepositioned through the bone before implantation of the humeral component (Figs. 7-8 and 7-9). The repair of the subscapularis is the critical element that needs attention during the first 6 weeks because of the importance of the subscapularis for component stability and overall shoulder girdle strength. Moreover, a disruption of the repair is notoriously difficult to diagnose in the early phases and extremely difficult to salvage when a chronic diagnosis is made.
The closure is done in layers, with a subcuticular skin closure protected by Steri-Strips being the final step. In some cases a drain may be exteriorized via a separate stab wound incision. This is typically removed on the first postoperative day. The final and perhaps most important part of the surgical procedure occurs at this time. The surgeon takes the arm through a PROM to assess the overall total motion possible without joint instability of disruption of the subscapularis tendon repair. This ROM will be used to guide the limits that will be allowed in the first phases of rehabilitation. Final radiographs are typically obtained immediately postoperatively to ensure an appropriate position of all the components and also to ascertain that no intraoperative complications such as a humeral shaft fracture have occurred (Fig. 7-10).
Therapy Guidelines For Rehabilitation
Total shoulder arthroplasty is performed less frequently than hip or knee total joint replacements in the United States.8 There is evidence that a decreased hospital stay and a higher likelihood of discharge to home may be associated with those patients treated in surgical centers with a higher volume of total shoulder arthroplasties.12,13 No attempts to correlate the patient’s functional limitations and impairments on discharge have been found with length of stay or “successful discharge.” The clinician must use physiologic healing principles to assist in gaining functional return of shoulder ROM following surgical intervention.
Successful rehabilitation of a total shoulder arthroplasty (TSA) depends in large part on the collegial communication between the surgeon and the therapist. Appropriate rehabilitation needs to recognize and address the preoperative history and impairments, the surgical technique, prosthetic type, and the surgeon’s assessment of the tissue status upon finalization of the repair.
The majority of these issues dictate the postoperative precautions and guidelines that are placed upon the rehabilitation timeline to ensure that protection of the position of the prosthesis and the appropriate healing of the subscapularis occurs (Box 7-1).
The patient and therapist must be aware that the primary goal for nontraumatic TSA is pain relief. It appears that the achievement of functional ROM goals are more achievable today than 5 years ago; however, the improvement of ROM is not as well substantiated in the literature as the successful achievement of decreased pain.14 The preoperative diagnosis also impacts the postoperative outcome. Completion of a TSA because of primary OA is more likely to result in functional use of the upper extremity than those completed as a result of trauma, rheumatoid arthritis of the GH joint, capsulorrhaphy, arthropathy, or rotator cuff arthropathy (Box 7-2).15
To prognosticate functional outcomes, including achievement of active ROM against gravity, the clinician should examine the patient’s prior surgical history, duration of impairments before surgery, presence and severity of a preoperative rotator cuff tear,15 the underlying cause for the surgical technique, and finally, the postoperative ROM at the shoulder while under anesthesia. These factors can help the clinician predict the maximal outcome that may be achieved. Both the patient’s status before surgery and the underlying causative factors leading to surgery can be obtained via patient interview. It is rare that the treating physical therapist would have the opportunity to perform a physical examination to potentially address postural deficits preoperatively. The surgical information including comments on ROM and the condition of the repaired tissue may be obtained from communications with the surgeon including the surgical report.
![]() Rehabilitation progression may further be guided by precautions and recommendations directly from the surgeon. In some instances formal physical therapy may not be used depending on the surgeon’s experiences.16 Typically, the patient will present in an abduction pillow or at the very least a shoulder sling. Additional positioning options or passive ROM (PROM) restrictions may be in place for a patient with a history of rheumatoid arthritis. A long history of rotator cuff pathology may require positioning that decreases the mechanical stresses placed on the healing structures.
Rehabilitation progression may further be guided by precautions and recommendations directly from the surgeon. In some instances formal physical therapy may not be used depending on the surgeon’s experiences.16 Typically, the patient will present in an abduction pillow or at the very least a shoulder sling. Additional positioning options or passive ROM (PROM) restrictions may be in place for a patient with a history of rheumatoid arthritis. A long history of rotator cuff pathology may require positioning that decreases the mechanical stresses placed on the healing structures. ![]() An external rotation restriction of less than 30° to 40° is typical for protection of the healing subscapularis muscle and the anterior capsule, which is disrupted during placement of the prosthetic. This restriction may last up to 6 weeks.17–19
An external rotation restriction of less than 30° to 40° is typical for protection of the healing subscapularis muscle and the anterior capsule, which is disrupted during placement of the prosthetic. This restriction may last up to 6 weeks.17–19
The periodization of the rehabilitation program for a TSA must balance protection of the healing tissues, structures with the need for ROM gain to prevent overall stiffness of the shoulder. There are indications that an increased immobilization period increases the risk of a contracture of the deltoid and the rotator cuff. This soft tissue imbalance is theorized to be one of the reasons for revision surgery of a TSA. Other reasons for surgical revision include glenoid loosening, rotator cuff tear, humeral head subluxation, proximal humeral head migration, and GH instability.1,14,20,55![]() The following guidelines should not supersede the communications from the surgeon nor should they override sound clinical judgment to create an independent plan of care based on your patient’s comorbidities, physical health, and functional needs.
The following guidelines should not supersede the communications from the surgeon nor should they override sound clinical judgment to create an independent plan of care based on your patient’s comorbidities, physical health, and functional needs.
Initial Postoperative Examination
Patient examination following surgery typically occurs on day 0 (day of surgery) or on postoperative day 1. The therapist will note IV lines for postsurgical fluid intake, sanguineous drains, postoperative dressing, and the upper extremity in a sling for comfort. Physical examination should include cognitive testing for orientation to name, time, place, and reason and vital sign assessment on the noninvolved extremity in supine, sitting, and standing. Testing specific to the involved upper extremity should adhere to the postoperative restrictions according to the patient’s chart (Box 7-3).
Neural screening should be completed as allowed within the postsurgical restrictions, including myotome, dermatome, and deep tendon reflex (DTR) testing. Active range of motion (AROM) of the cervical spine, thoracic spine, and elbow, wrist, and fingers should be assessed. PROM of the shoulder should be assessed with the patient in supine, understanding that some limitation in mobility may be contributable to the dressing or IV lines. Girth measurements should be noted at the elbow and at the wrist for comparison with the uninvolved extremity. Additionally, the anterior and posterior chest wall should be monitored for ecchymosis.
![]() Functional mobility assessment should be initiated with instructions cautioning against direct pushing or pulling of the involved upper extremity during transferring. Patients must be assessed for independent mobility from supine to sit to stand and vice versa. Once standing is achieved, balance must be assessed for single limb support without loss of balance. Frequently, postoperative day 0 or day 1 will require the patient to use a temporary single upper extremity support (IV pole or single point cane) because of anxiety and a deconditioned state. Monitoring of vitals and orientation during the transfer and gait assessment is necessary due to risk of hypotensive episodes. The clinician should encourage the use of coughing and incentive spirometry throughout the hospital stay because of the greater level of inactivity following surgery intervention.
Functional mobility assessment should be initiated with instructions cautioning against direct pushing or pulling of the involved upper extremity during transferring. Patients must be assessed for independent mobility from supine to sit to stand and vice versa. Once standing is achieved, balance must be assessed for single limb support without loss of balance. Frequently, postoperative day 0 or day 1 will require the patient to use a temporary single upper extremity support (IV pole or single point cane) because of anxiety and a deconditioned state. Monitoring of vitals and orientation during the transfer and gait assessment is necessary due to risk of hypotensive episodes. The clinician should encourage the use of coughing and incentive spirometry throughout the hospital stay because of the greater level of inactivity following surgery intervention.
Phase I: Hospital Phase of Rehabilitation
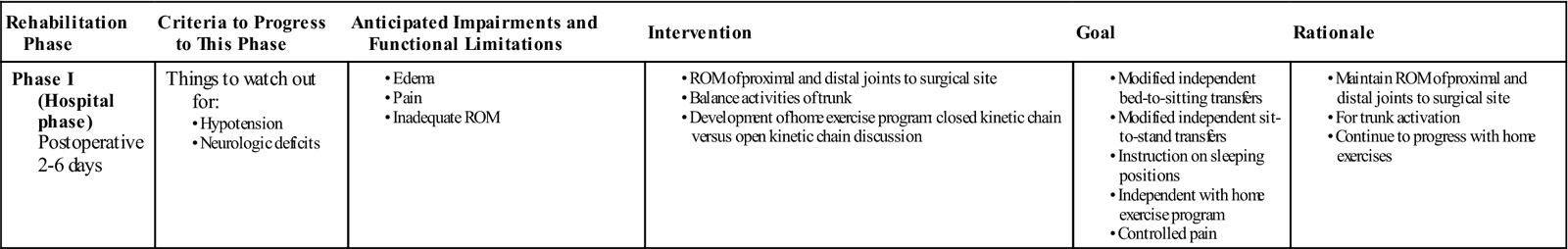
TIME: 2 to 6 days after surgery13
GOALS: Protection of healing structures, pain control, independent functional mobility for transfers, dressing and ambulation, education, and the institution of a home exercise program within the surgical restrictions (Table 7-1)
TABLE 7-1
< ?comst?>
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Treatment during the hospital phase of rehabilitation focuses on the achievement of appropriate pain control, independent functional mobility for transfers, dressing and ambulation, education, and the institution of a home exercise program within the surgical restrictions. Length of hospital stay depends on multiple factors including the volume and experience of the hospital and the surgeon experienced in the total shoulder procedure. Home support, comorbidities, and demographic features play a smaller role. Unlike the total knee arthroplasty where a certain objective measure of knee flexion is often one of the impairment goals for discharge, common discharge goals regarding functional level, pain control, and impairment objective measurements for total shoulder procedures have not been established in the literature.12,13
Typically, PROM is initiated on day 0 or 1, with a progression to self-assisted ROM exercises including pendulum or table top activities.
The home exercise program should be completed multiple times per day for short durations of 5 minutes maximum per bout of exercise.18![]() If there is a strict passive ROM restriction in place, then this will require the education of a caregiver or family member to assist with the execution of the home program. This caregiver must understand all postsurgical restrictions that limit ROM. Self-assisted ROM exercises can be based on patient comfort or surgeon preference.
If there is a strict passive ROM restriction in place, then this will require the education of a caregiver or family member to assist with the execution of the home program. This caregiver must understand all postsurgical restrictions that limit ROM. Self-assisted ROM exercises can be based on patient comfort or surgeon preference.
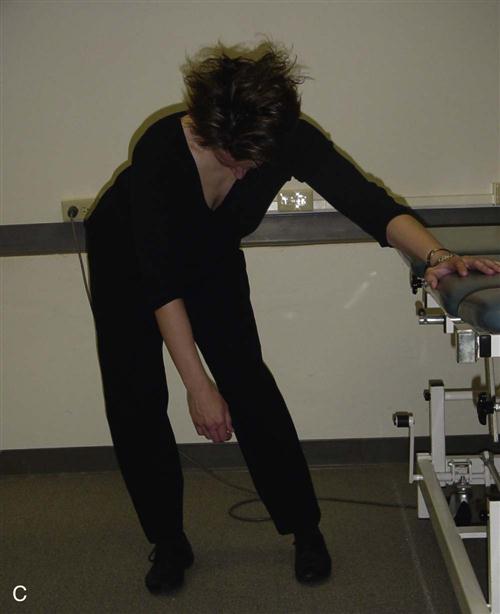
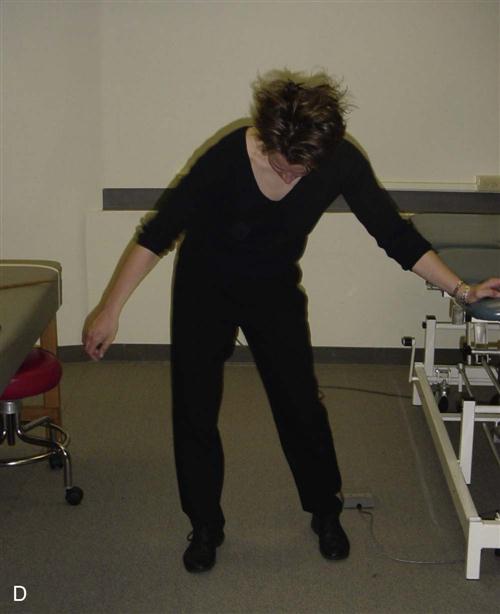
Pendulum exercises involve a static position of forward flexion of the trunk with movement of the hips and trunk to drive the dangling upper extremity into multiple planes of motion (Fig. 7-11). The benefits of this activity for this patient population includes the addition of traction to the joint, stretching of the capsule, and ![]() avoidance of active muscular contraction at the shoulder joint.21 Overall, the goal is prevention of soft tissue contracture and possible modulation of pain via the rhythmic movement of the upper extremity through a PROM.17,22 There are several challenges with the correct performance of this exercise as it applies to the patient with a recent TSA. Frequently, the patient demonstrates inappropriate performance by recruiting excessive muscular action at the deltoid and pectoralis major muscles. The recommended posture for pendulum exercises emphasizes poor mechanical alignment of the scapula on the thorax with promotion of scapular abduction. And lastly, the excessive and unopposed stretching of the recently repaired musculature and tissues from the surgical procedure may actually generate greater pain response.
avoidance of active muscular contraction at the shoulder joint.21 Overall, the goal is prevention of soft tissue contracture and possible modulation of pain via the rhythmic movement of the upper extremity through a PROM.17,22 There are several challenges with the correct performance of this exercise as it applies to the patient with a recent TSA. Frequently, the patient demonstrates inappropriate performance by recruiting excessive muscular action at the deltoid and pectoralis major muscles. The recommended posture for pendulum exercises emphasizes poor mechanical alignment of the scapula on the thorax with promotion of scapular abduction. And lastly, the excessive and unopposed stretching of the recently repaired musculature and tissues from the surgical procedure may actually generate greater pain response.
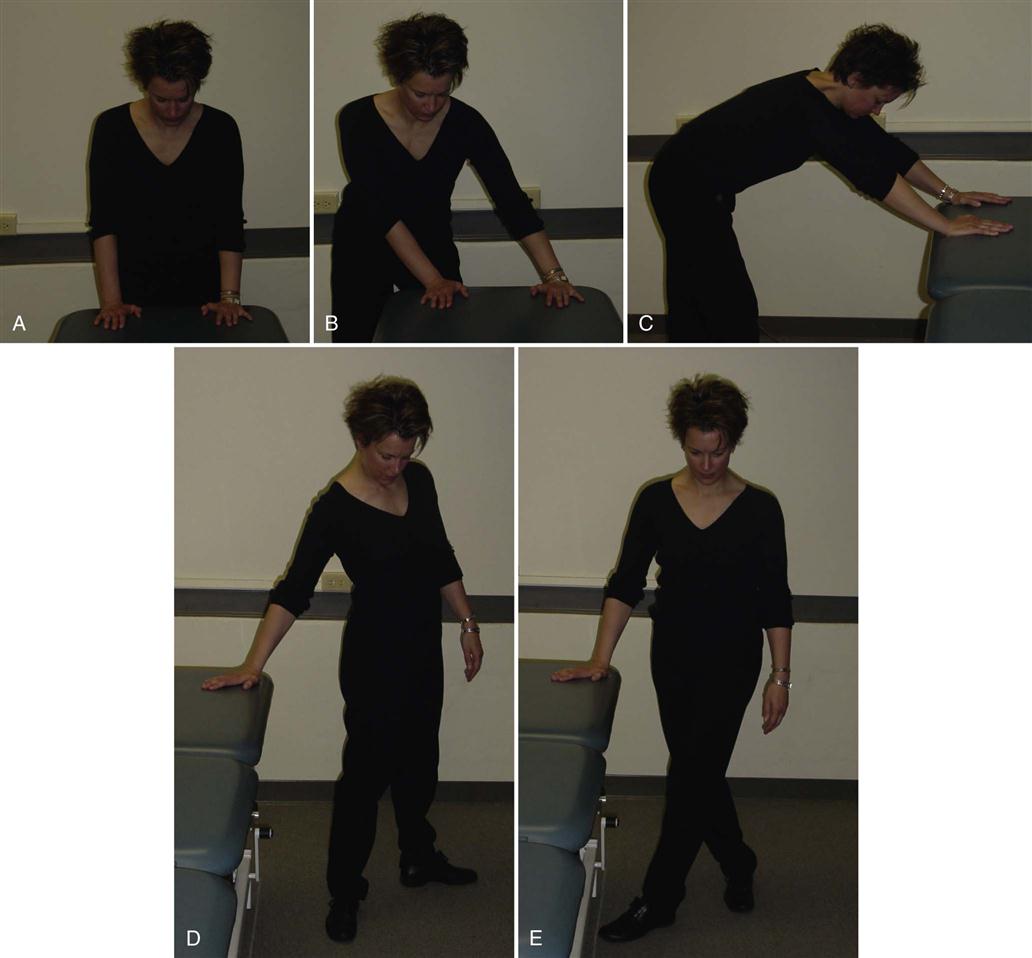
The Neer protocol for TSA23 placed wall slides in the same phase as pendulum activities with literary evidence of low muscular activity about the healing structures.21 Modification of this position to a lower gravitational demanding position would be self-assisted ROM using a table top. This table top modification is frequently used before wall slides during this early intervention phase. The patient stands at a table top with bilateral upper extremities resting at a comfortable placement. The hands maintain a static position and then ROM is attained by the lower extremity stepping into the various planes of motion.17 There are several benefits to this type of exercise prescription. The position of weight bearing promotes ROM gains through planar lower extremity motion. The trunk is moving underneath the scapula, which promotes interaction of the scapula and thorax in preparation for later stages of rehabilitation (Fig. 7-12). The patient is able to control the excursion of the ROM of the shoulder via decreasing the step size. The supported position of the shoulder via the hand decreases the unopposed stress on the healing tissue that may be achieved in the open kinetic chain position of the pendulum. Finally, closed kinetic chain activities at the shoulder reap similar benefits as stated for other extremities including: muscular cocontraction, decrease of shear forces, increased joint compression, and increased stability about the joint.3,24
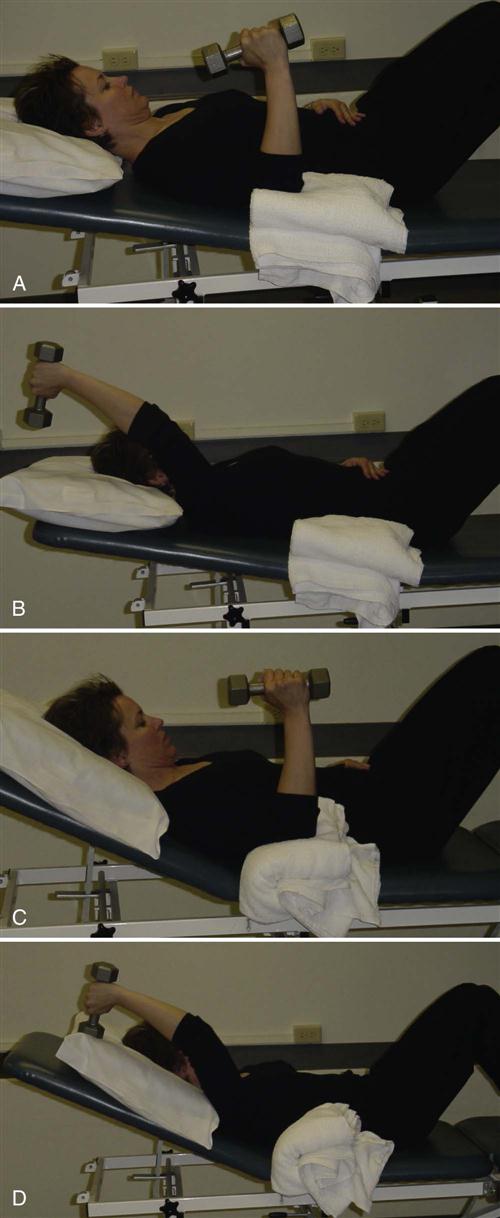
The home exercise program should require AROM of the cervical and thoracic spines through the cardinal planes and active movement of the elbow, wrist, and hand.![]() If the patient is supine then flexion of the elbow should occur only with the humerus supported by a towel underneath it to decrease the strain on the biceps tendon at its insertion. Frequent bouts of exercise for short durations are recommended for the earlier stages of rehabilitation.
If the patient is supine then flexion of the elbow should occur only with the humerus supported by a towel underneath it to decrease the strain on the biceps tendon at its insertion. Frequent bouts of exercise for short durations are recommended for the earlier stages of rehabilitation.
The home exercise program contains education for passive and/or self-assisted ROM at the shoulder, active ROM for proximal and distal structures, and education on sleeping postures. This should include positional support via the use of pillows or an immobilizer to support the healing structures during the night. The encouragement of experimentation to attain the best possible sleeping posture should be discussed. Anecdotally, patients following shoulder surgery feel better sleeping in a semireclined posture with the involved upper extremity supported by pillows or bolsters (Fig. 7-13).

Phase II: Outpatient Rehabilitation–Early Range of Motion 0 to 6 Weeks
TIME: 0 to 6 weeks
GOALS: Protection of healing structures, pain control, uninterrupted sleep pattern, normalized circumference measurements between upper extremities, mobilization of scar, ability to demonstrate normalized posture, and increased ROM (Table 7-2)
TABLE 7-2
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
|
Phase II (ROM) Postoperative 0-6 wk
|
|
|
< ?comen?>< ?comst1?>

< ?comst1?>
< ?comen1?>
Outpatient rehabilitation begins as a progression of the home exercise program given during the hospital stay. It is recommended to incorporate the use of a self-reported outcome measure tool, such as the simple shoulder test (SST) or the disability assessment of shoulder and hand (DASH) to monitor functional changes through rehabilitation.7 It is important to remind the patient that their rehabilitation will continue past discharge from formal physical therapy as functional return may proceed for 1 to 2 years after surgical intervention.25
The focus of the first 6 weeks of rehabilitation is twofold: protection of the healing structures and progression of ROM for prevention of muscular contracture and joint capsule stiffness. A limited amount of literature is available to support the variety of intervention plans employed during this phase.18,26–28 Adherence to postsurgical precautions is paramount. Treatment of the postsurgical impairments of pain, edema, and scar mobility will naturally lead to increased ROM in the shoulder.
Pain control should be assisted via the adherence to medications prescribed by the surgeon and alleviating positions. Use of the sling should be gradually removed as the patient progresses through this phase. Control of pain will also be gained via the interventions to address the postsurgical inflammation and edema, and those interventions to improve the limited functional use of the upper extremity. Edema may be present in the distal upper extremity and ecchymosis may be present in the thorax from the overload of the lymphatic system following surgery. Modality use including ice, elevation, and electric stimulation are appropriate for edema management.29 Diaphragmatic breathing followed by localized lymphatic massage techniques beginning at the proximal segments of the thorax and ipsilateral axilla and progressing distally in sequential order may also be employed for effective management.
Sleeping postures should be recommended to include positional support of the humerus via the use of pillows or a bolster. As mentioned, patients following shoulder surgery may prefer sleeping in a semireclined posture; the therapist should encourage the patient to experiment.
Progression of ROM may be elicited via soft tissue mobilization. Soft tissue mobilization, a form of massage, has the support of an animal model for potential cellular changes.30 Initiation of soft tissue mobilization techniques at the posterior cuff and the deltoid will promote appropriate muscular length. Because of the probable postsurgical hypersensitivity, care should be taken at or near the surgical scar. For each of these techniques, the upper extremity position should be adjusted to ensure the muscle or area of skin being addressed is relaxed and in a protected posture. Initial positioning should address the targeted muscle in a position of a passively shortened length. This will decrease sensitivity and spasm at the introduction of this type of intervention.
![]() The external rotation limitation is in place to promote soft tissue healing and protection of those structures injured during the surgical procedure, specifically the subscapularis muscle. As outlined previously, the subscapularis is taken down and reattached during the arthroplasty procedure.
The external rotation limitation is in place to promote soft tissue healing and protection of those structures injured during the surgical procedure, specifically the subscapularis muscle. As outlined previously, the subscapularis is taken down and reattached during the arthroplasty procedure. ![]() Direct passive ROM to “stretch” this tissue is contraindicated during the early phases of rehabilitation and soft tissue mobilization is an appropriate intervention to address the inflammatory condition of this muscle and prevent adhesion development. The technique of soft tissue mobilization promotes change to the myofascia via proposed realignment of the scar tissue and collagen. Slow, deep strokes to the myofascia of the subscapularis will assist in improvement of external rotation ROM, pain control, and eventual overhead reach.31 The best patient position for improvements to the subscapularis length is approximately 45° of humeral abduction with a neutral rotation of the humerus.
Direct passive ROM to “stretch” this tissue is contraindicated during the early phases of rehabilitation and soft tissue mobilization is an appropriate intervention to address the inflammatory condition of this muscle and prevent adhesion development. The technique of soft tissue mobilization promotes change to the myofascia via proposed realignment of the scar tissue and collagen. Slow, deep strokes to the myofascia of the subscapularis will assist in improvement of external rotation ROM, pain control, and eventual overhead reach.31 The best patient position for improvements to the subscapularis length is approximately 45° of humeral abduction with a neutral rotation of the humerus.
Consideration of the other joints of the shoulder complex should be initiated during this phase. During the hospital stay, the patient had been instructed in cervical and thoracic AROM. Distally, the elbow and hand should be used during daily functional activities, thereby limiting the extent of distal disuse atrophy. Realization of the influence of the scapulothoracic juncture on GH motion can assist with restoration of this motion early in rehabilitation.
Protective posturing from the postsurgical sling typically places the scapula in an abducted and down rotated position. Lack of humeral motion in all of the planes through the initial weeks of rehabilitation leads to further disuse of the scapula and its contribution to shoulder ROM. Scapular mobilization on a stable thorax with the GH joint in its resting position for greatest volume prepares the scapula and its connecting tissue for future shoulder ROM (Fig. 7-14). Because of the typical postural dysfunction of scapular abduction and down rotation, many patients will require facilitation of adduction, upward rotation, and elevation. The lack of a true joint capsule about the scapula places this type of intervention into a mobilization of the myofascial connections. The clinician should recall the scapulohumeral rhythm and carefully monitor the position of the humerus when facilitating positions of the scapula (Box 7-4). For example, scapular mobilizations into upward rotation should only occur with the humerus passively flexed greater than 60° or abducted greater than 30°, as these are the ranges at which the scapula and humerus begin a more associated phase of motion.32

PROM via a family member in a gravity-eliminated position of supine or self-assisted ROM during table top weight bearing will be the primary method to promote ROM during this time frame (see Fig. 7-12). Progression should be dictated by the report of pain. ![]() PROM performed by the therapist, patient, or caregiver should not exceed any precautions or restrictions given by the surgeon. A tip for improved pain tolerance for motion of the upper extremity is to bias toward the plane of the scapula instead of true sagittal plane flexion.33 A recommendation for moving into passive external rotation is the alignment of the humerus perpendicular to the center of the glenoid. This occurs at approximately 30° of abduction and ensures that the capsular structures will relax, achieving a better outcome.18
PROM performed by the therapist, patient, or caregiver should not exceed any precautions or restrictions given by the surgeon. A tip for improved pain tolerance for motion of the upper extremity is to bias toward the plane of the scapula instead of true sagittal plane flexion.33 A recommendation for moving into passive external rotation is the alignment of the humerus perpendicular to the center of the glenoid. This occurs at approximately 30° of abduction and ensures that the capsular structures will relax, achieving a better outcome.18
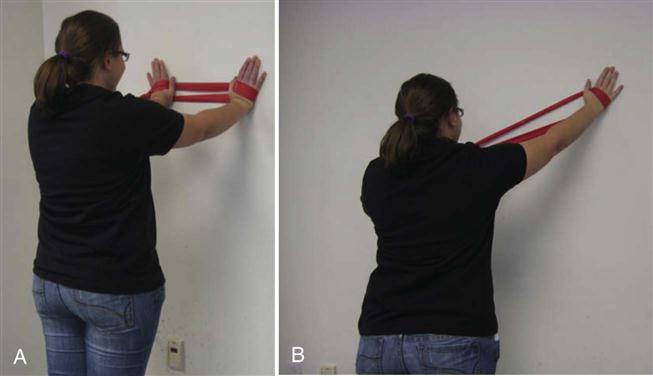
Self-assisted activities for ROM can be varied by direction, surface, and patient position. These types of exercise promote the mobility of the proximal segments over the involved upper extremity in a stable position. The trunk may move away from the upper extremity in various directions to promote the cardinal planes.26 For example, in the early stages when the patient may still be most comfortable in the sling or supported position, relative external rotation and facilitation of scapular control may be achieved via contralateral trunk rotation and a return to neutral.34 In an advanced stage of self-assisted exercises, the involved upper extremity may rest on a stability ball and the patient rolls the stool away from the stability ball in the frontal plane, promoting self-assisted abduction of the involved extremity. Or the patient may progress to gravity-dependent positions using the wall as the support and the trunk moving under the body to facilitate various planes of motions (Fig. 7-15).
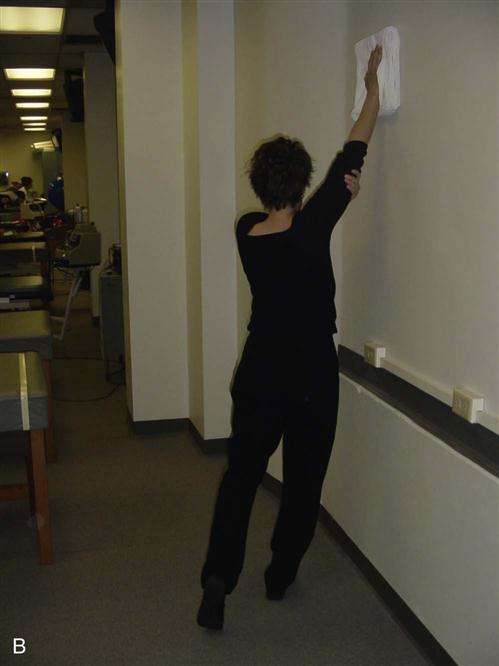
Other self-assisted activities that have been recommended during this time include wand activities and pulley stretches.18,26–28 Examination of pulley and wand activities compared to therapist-assisted exercises35 indicate that therapist activities elicit less muscular activity of the supraspinatus, infraspinatus, anterior deltoid, and trapezius muscles. Therefore, therapist-assisted activities should be used initially during this phase with a progression to wand or pulley activities as pain or surgical restrictions allow (Figs. 7-16, 7-17, and 7-18).18,26–28


Progression from the initial outpatient phase (phase II) to the late ROM phase (phase III) is listed in Box 7-5. ![]() The most significant requirement is physician clearance for AROM, especially into external rotation. Many patients’ restrictions will be lifted between weeks 2 and 6, thereby blurring the activities of phase II and phase III. The therapist should monitor the patient’s ROM to assist with “staging” the patient’s rehabilitation. This is one of the most challenging components of the transition from phase II to phase III. As noted, the passive motion goal of phase II is 40° while the patient will have achieved full PROM at the end of phase III. Additionally at the end of phase III, the patient should have active external rotation ROM of 45°. This ROM measure is the key to successful overhead motion.
The most significant requirement is physician clearance for AROM, especially into external rotation. Many patients’ restrictions will be lifted between weeks 2 and 6, thereby blurring the activities of phase II and phase III. The therapist should monitor the patient’s ROM to assist with “staging” the patient’s rehabilitation. This is one of the most challenging components of the transition from phase II to phase III. As noted, the passive motion goal of phase II is 40° while the patient will have achieved full PROM at the end of phase III. Additionally at the end of phase III, the patient should have active external rotation ROM of 45°. This ROM measure is the key to successful overhead motion.
Recall that optimal GH and scapular mechanics require near normal ROM of external rotation of the GH joint to complete functional tasks, such as touching the back of the head, reaching overhead, and donning/doffing shirts.36 If the GH joint ROM into external restriction is restricted to 45°, then a significant loss of function occurs, dramatically impacting a patient’s quality of life. As the patient will not have near normal external rotation ROM at the end of phase II, it is ill-advised to focus on repetitive or strengthening activities that are overhead because the mechanics will be less than optimal. To prevent complications of overuse or tissue irritation, exercises and activities should be performed with the correct mechanics and without symptoms before progression to the next phase.
Complications
There are several signs and symptoms that should alert the therapist for possible complications (Box 7-6). Each must be examined with close consideration to the context and associated or corroborating signs and symptoms. Sustained edema in the distal upper extremity may be indicative of a systemic issue, such as infection. Excessive external rotation or quick achievement of ROM may indicate compromised muscular integrity. Biceps tendonitis indicates an overuse of the biceps for shoulder motion or stabilization. The biceps has an active role as a humeral depressor and with postsurgical muscular inhibition of the rotator cuff, successful accomplishment of shoulder flexion may rely on the biceps as the primary humeral depressor.37 As a patient successfully progresses through the different stages of rehabilitation, pain is expected to plateau, decrease, or alter to more muscular fatigue or muscular soreness. Progressively increasing pain is often thought of as an indicator of serious pathology.
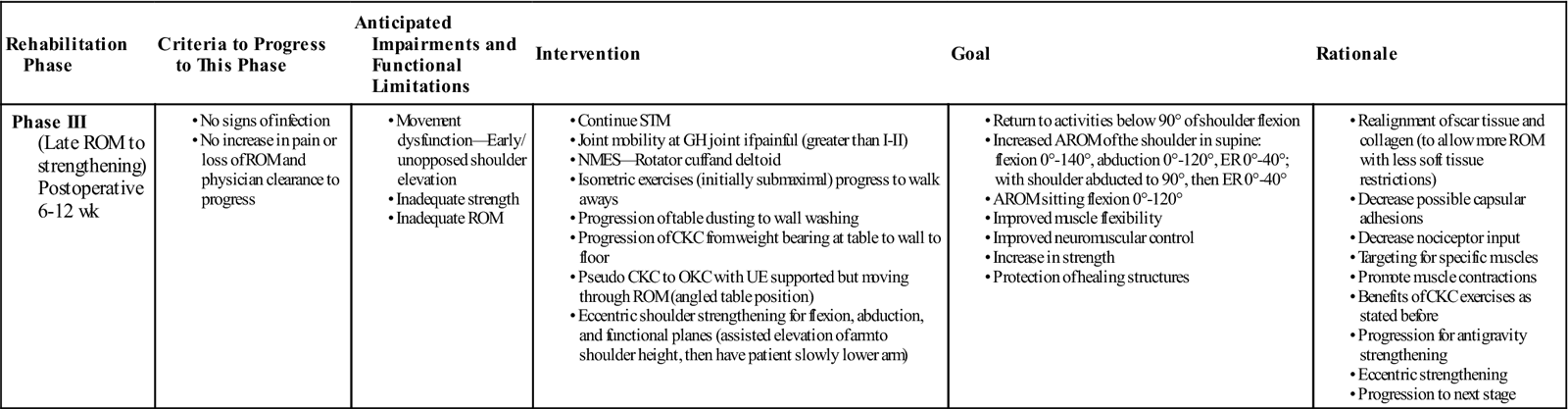
Phase III: Outpatient Rehabilitation—Late ROM and Early Strengthening
TIME: Approximately 6 to 12 weeks
GOALS: Return to everyday activities below 90° of shoulder flexion, increased ROM, improved muscle flexibility, improved neuromuscular control, increased strength, protection of healing structures (Table 7-3)
TABLE 7-3
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
|
Phase III (Late ROM to strengthening) Postoperative 6-12 wk
|
|
|
|
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
As the patient’s ROM progresses, the patient will enter a mixed phase that consists of stretching to gain motion and strengthening to use the range gained. Exercise selection should place the protection of the healing structures as the primary concern. ![]() This may include protection of the anterior joint capsule and the subscapularis via limit of external rotation when the humerus is in 0° of abduction and a limitation of hyperextension of the humerus when in the supine position for resting or exercise positioning.18,26 Communication with the surgeon will assist with determining which restrictions need to be maintained.
This may include protection of the anterior joint capsule and the subscapularis via limit of external rotation when the humerus is in 0° of abduction and a limitation of hyperextension of the humerus when in the supine position for resting or exercise positioning.18,26 Communication with the surgeon will assist with determining which restrictions need to be maintained.
The emphasis of this phase is use of ROM and progression to muscle strengthening. Interventions to address muscular flexibility of the rotator cuff, deltoid, and scapular stabilizers should be continued from the previous phase. Pain has been found to inhibit muscular strength and therefore can be a limitation for achievement of active ROM.6 Consideration that the source of pain may be from structures other than the traumatized muscle tissue will provide options for other interventions. Gentle joint mobilizations (grade I to II oscillatory) to the GH joint may be used to decrease possible capsular adhesions and to alter nociceptive input.18,26
There can be considerable discussion on the most appropriate exercises to initiate strengthening activities following a TSA. The clinician should always consider how mobility is achieved and what movement patterns may be adopted during this time period. As the body transitions from limited mobility and muscular inhibition, the patient is at risk of developing faulty movement patterns that may later impede the ability to achieve active ROM in gravity-resisted positions. It is strongly encouraged to instruct the patient in activities that promote the correct scapulohumeral rhythm for overhead activities. Application of this movement reasoning includes activities that emphasize the separation of scapular and the humeral motion during the initial phases and late phases of flexion and abduction and then emphasize coordination of the motion of the scapula and the humerus during the mid phases of motion.
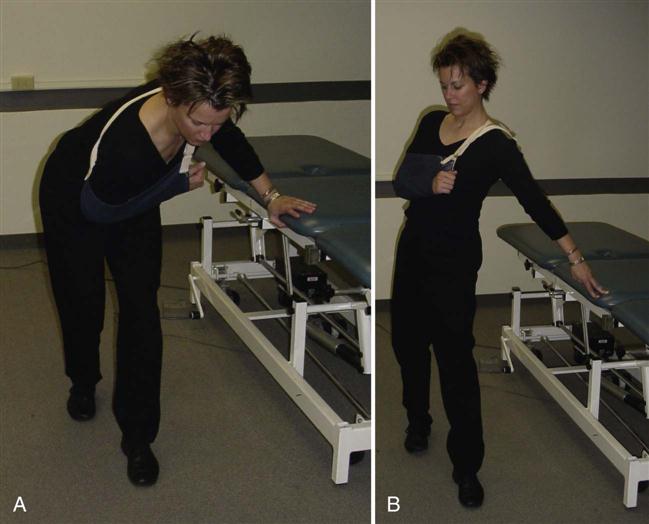
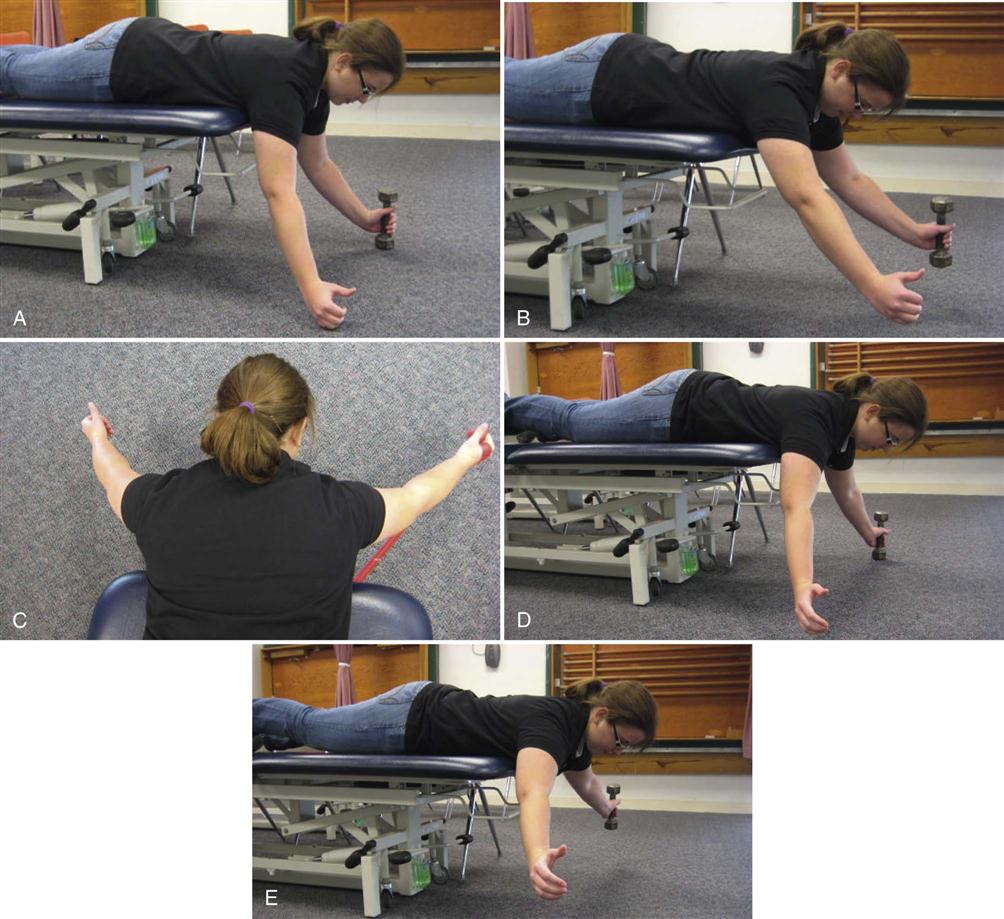
Isometric training is supported for early strength training, especially in the cases where muscular contraction is desired yet the patient lacks sufficient strength for mobility through ROM.26 ![]() The clinician should be aware that significant muscular contraction can be elicited during isometric contraction exercises and therefore these exercises may be inappropriate during a healing phase where maximum tissue protection is required.21 Initiation of isometric training of the deltoids with a contraction of the rotator cuff establishes a muscular cocontraction or force couple that is required for motion (Figs. 7-19 and 7-20).
The clinician should be aware that significant muscular contraction can be elicited during isometric contraction exercises and therefore these exercises may be inappropriate during a healing phase where maximum tissue protection is required.21 Initiation of isometric training of the deltoids with a contraction of the rotator cuff establishes a muscular cocontraction or force couple that is required for motion (Figs. 7-19 and 7-20).
Isometric training of the scapular stabilizers with an eccentric contraction of the deltoid and rotator cuff from a prone position is an option for the introduction of strength training below 90° of shoulder flexion. A slow lowering toward the floor after a passive preposition into horizontal abduction at 90° will activate each of these key muscles. Introduction of concentric flexion and abduction may be introduced by progressively tilting supine positioning toward upright with and without weights (Figs. 7-21 and 7-22).19
If the patient is demonstrating significant difficulty performing an active contraction of targeted muscles in the absence of a neurologic injury, neuromuscular electric stimulation (NMES) may be used. Though specific parameters are outside the scope of this chapter, dual channel stimulation to provide for the deltoid activation and the scapular rotation necessary to achieve shoulder motion greater than 90° is recommended. Scapular rotation may be stimulated via the lateral rotator cuff muscles on the scapula or by stabilizing the scapula by stimulating the muscles with attachments to the medial border of the scapula. Electrode size and placement are key points for effective use of NMES.29
![]() Progression to the final phase requires an improvement in passive and active ROM. The patient must be able to perform all home exercises with the correct form and minimal correction by the therapist (Box 7-7).
Progression to the final phase requires an improvement in passive and active ROM. The patient must be able to perform all home exercises with the correct form and minimal correction by the therapist (Box 7-7).
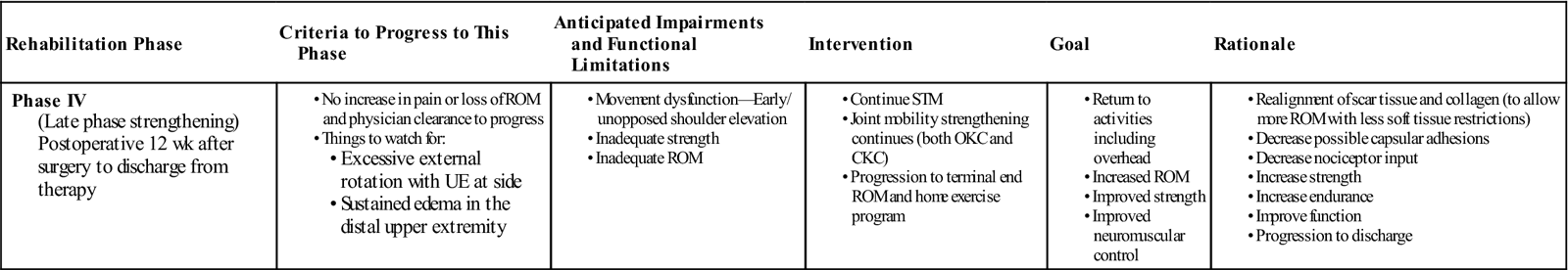
Phase IV: Outpatient Rehabilitation—Late Phase Strengthening
TIME: 12 weeks and more postsurgery
GOALS: Return to normal activities including overhead, increased ROM, improved neuromuscular control and strength. Full potential of function achieved between 6 and 12 months (Table 7-4).7
TABLE 7-4
< ?comst?>
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
The goal of this phase of rehabilitation is strengthening of targeted muscles for use of the AROM gained and to establish a home exercise program that promotes continued strengthening upon discontinuation of therapy. Interventions addressing pain control and edema should be progressively phased out as they are no longer needed. Mobility of the scapula should occur with the humerus positioned into greater ranges of motion into shoulder flexion or abduction or completed in a mobilization with a movement model, with the patient performing the motion and the clinician providing overpressure to engage scapular motion at the appropriate time. The intention of mobilizations to the GH joint should change from addressing pain relief to the residual capsular stiffness or asymmetry through oscillation grades III and IV. Strengthening activities should address the dynamic stabilization system of the shoulder that is necessary for overhead movement.
Several underlying impairments may be responsible for the continued limited ability of the patient to demonstrate appropriate sequential motion when attempting to raise the arm above shoulder height. A number of factors may create barriers to successful progression. These include appropriate and timely surgical intervention, a rehabilitation course that has minimal medical complications, and/or appropriate motivation by the patient. If no barriers are apparent to progress, the primary impairment for limited overhead motion is due to inadequate motor performance of the force couples of the shoulder. The force couple between the deltoid muscles and the rotator cuff musculature is the primary focus.17,27 If the AROM demonstrated in the supine position is approaching the ROM goals for therapy—yet the patient is unable to demonstrate similar range in sitting—then this type of motor control and/or pattern of weakness should be considered (Box 7-8).
Though specific rehabilitation parameters for those patients exhibiting weakness because of neural injury will not be included in this discussion, this impairment should be considered as a possible contributor to a continued movement dysfunction. Typically, a neural injury associated with the trauma that predates the surgery or a neural injury from a recent surgical intervention is difficult to identify because of the amount of surgically induced trauma during the procedure. Neural injury may be identified via atrophic changes to the muscle, inability of the patient to elicit an isometric contraction of the muscle with the humerus positioned in neutral, and possible sensory changes in the upper extremity. Isolated neural injuries following shoulder arthroplasty are considered a low risk because of the transient nature of the injuries and the tendency for resolution without eventual operative intervention.38 When denervation of the shoulder musculature is present before surgery, the patient will most likely be placed in a limited goals category.23 This category and the goals will be discussed later in this chapter.
Evaluation of weakness in patients with adequate innervation of the shoulder musculature should include manual muscle testing and the presence of coordination between the two primary force couples that move the shoulder. As a review, there is a delicate balance that must be maintained to move the shoulder through its full ROM. The muscular contribution to this coordinated effort is via the force couple of the deltoid muscles and the rotator cuff muscles, and the scapular stabilizer muscles with the deltoid muscles. Both of these force couples must have a balanced contraction to facilitate shoulder flexion and abduction without impingement of the humerus at the subacromial arch.39
Strengthening should respect the force couples of the shoulder while addressing both the concentric and eccentric functions of the targeted muscles. The force couple of the shoulder between the deltoid and the rotator cuff can be progressed from earlier examples of exercise (Fig. 7-23) into a standing exercise that maintains humeral external rotation through an isometric contraction and a concentric contraction of the deltoid. An example of an eccentric exercise progression is demonstrated through an alteration of the wand activity. The patient can complete a sitting or standing overhead wand activity initially shown in supine in Fig. 7-24. At the highest point of the wand lift, the patient releases the involved upper extremity from the wand and slowly lowers the involved extremity back toward the waist.40 This type of training can also be initiated for strengthening into abduction.
As a final example, consider that strengthening must also address specific deficits in the targeted muscles. Fig. 7-24 demonstrates an exercise targeting the function of the low trapezius. The exercise emphasizes an isometric contraction of the upward rotation and a concentric action of the low trapezius as a scapular depressor. A movement dysfunction at greater than 120° in either flexion or abduction or inadequate strength as noted in a manual muscle testing would assist in determining the necessity of this exercise.
Return to recreational activities should have been a goal from the initial evaluation. Closer scrutiny to the movements necessary for the patient’s chosen recreation will be strong consideration for formulation of the home program and strengthening program during this final phase. Successful return to recreation has been noted especially with the sports of swimming, tennis, and golf. Though the timeframe of return will vary, successful return has been noted as early as 6 months.4
Caution For Strength Training
Strength training does impart increased loads upon the healing shoulder that the clinician should monitor as the patient progresses through this phase. ![]() Heavier loading of the shoulder or the introduction of activities with increased shear forces is discouraged until significant bone healing is evident, typically around 12 weeks. Changes in the GH translations and loading mechanics can also be attributed to an imbalance of muscular forces either from length or strength impairments and the mobility of the joint capsule.41 The surgical procedure also plays a role in the ability of a patient to participate in heavy loading of the shoulder either for recreation or work demands. With poor methods or inappropriate prosthetic placement in addition to increased loads, the patient may be at risk for uneven wear of the glenoid or loading of the glenoid rim, which may lead to instability or component loosening.17,42
Heavier loading of the shoulder or the introduction of activities with increased shear forces is discouraged until significant bone healing is evident, typically around 12 weeks. Changes in the GH translations and loading mechanics can also be attributed to an imbalance of muscular forces either from length or strength impairments and the mobility of the joint capsule.41 The surgical procedure also plays a role in the ability of a patient to participate in heavy loading of the shoulder either for recreation or work demands. With poor methods or inappropriate prosthetic placement in addition to increased loads, the patient may be at risk for uneven wear of the glenoid or loading of the glenoid rim, which may lead to instability or component loosening.17,42
It is the therapist’s responsibility to ensure that there is appropriate resolution of joint mobility, optimal extremity alignment, and muscular balance. Additionally, the functional tool, the simple shoulder test, can provide guidelines on how much to load the shoulder during the rehabilitation period. It includes the ability to lift 1 lb to shoulder height, ability to lift 8 lb to shoulder level, and carrying an item weighing 20 lb.25,43
Additional assistance for decision-making may be found considering studies of external moments of the shoulder during activities of daily living. The average external moments to reflect loading of the shoulder during several activities of daily living, including picking up a 5-kg box, moving a 10-kg suitcase, and transferring from sit to stand, have been evaluated. The performance of these activities has been found to represent a large proportion of the upper extremity strength in normal men and women.44 Patients who receive a TSA must be considered to possess less than normal strength especially during the rehabilitation process. ![]() Therefore, current caution for heavy loading of the shoulder for strength training demonstrates appropriate concern by the therapist for the external moments created by these lifts thereby protecting the prosthetic and its design. Limiting the intensity prescribed to the patient for strength training exercises should be examined. Discussion with the referring surgeon may give the therapist more specific guidelines for possible lifting restrictions.
Therefore, current caution for heavy loading of the shoulder for strength training demonstrates appropriate concern by the therapist for the external moments created by these lifts thereby protecting the prosthetic and its design. Limiting the intensity prescribed to the patient for strength training exercises should be examined. Discussion with the referring surgeon may give the therapist more specific guidelines for possible lifting restrictions.
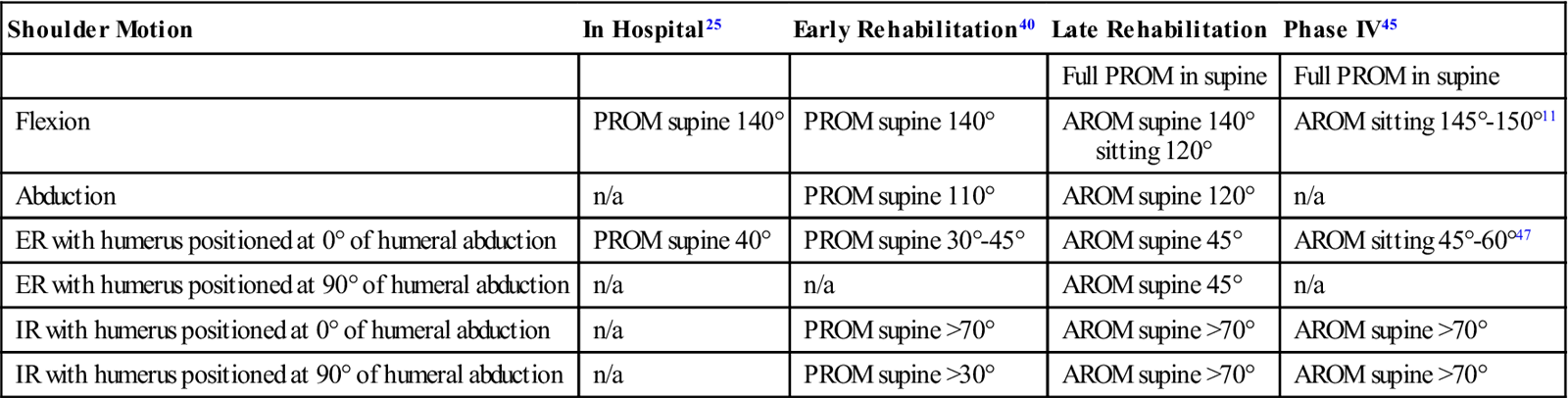
Resolution of functional limitation in activities of daily living and ROM goals should guide the determination of timely discharge. Active ROM goals are listed in Table 7-5. ![]() The therapist should not prognosticate attainment of full ROM following TSA. This has been demonstrated in several studies on total shoulder procedures regardless of the presence or the lack of underlying pathologies or comorbidities.45–50 Additionally, both patient and therapist should be aware that function improvements continue beyond the discharge of therapy up to approximately 1 year after surgery.17
The therapist should not prognosticate attainment of full ROM following TSA. This has been demonstrated in several studies on total shoulder procedures regardless of the presence or the lack of underlying pathologies or comorbidities.45–50 Additionally, both patient and therapist should be aware that function improvements continue beyond the discharge of therapy up to approximately 1 year after surgery.17
TABLE 7-5
Range of Motion Goals to Advance to the Next Phase of Rehabilitation
< ?comst?>
| Shoulder Motion | In Hospital25 | Early Rehabilitation40 | Late Rehabilitation | Phase IV45 |
| Full PROM in supine | Full PROM in supine | |||
| Flexion | PROM supine 140° | PROM supine 140° | AROM supine 140° sitting 120° |
AROM sitting 145°-150°11 |
| Abduction | n/a | PROM supine 110° | AROM supine 120° | n/a |
| ER with humerus positioned at 0° of humeral abduction | PROM supine 40° | PROM supine 30°-45° | AROM supine 45° | AROM sitting 45°-60°47 |
| ER with humerus positioned at 90° of humeral abduction | n/a | n/a | AROM supine 45° | n/a |
| IR with humerus positioned at 0° of humeral abduction | n/a | PROM supine >70° | AROM supine >70° | AROM supine >70° |
| IR with humerus positioned at 90° of humeral abduction | n/a | PROM supine >30° | AROM supine >70° | AROM supine >70° |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Data from Goldberg BA, et al: The magnitude and durability of functional improvement after total shoulder arthroplasty for degenerative joint disease. J Shoulder Elbow Surg 10(5):464-469, 2001; Brems J: Rehabilitation following shoulder arthroplasty. In Friedman R, editor: Athroplasty of the shoulder, New York, 1994, Thieme; Godeneche A, et al: Prosthetic replacement in the treatment of osteoarthritis of the shoulder: early results of 268 cases. J Shoulder Elbow Surg 11(1):11-18, 2002; Gartsman GM, Roddey TS, Hammerman SM: Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am 82(1):26-34, 2000.
Limited Goals Category For Total Shoulder Arthroplasty
The limited goals category following TSA was first mentioned by Neer in 1982.23 Criteria for inclusion into the limited goals category included the status of the rotator cuff and the stability of the implant. Patients were placed into a limited goals category if the rotator cuff was detached and not capable of recovery secondary to denervation or irreversible contracture or if the stability of the implant was problematic as evaluated by the surgeon during the procedure (Boxes 7-9 and 7-10). Specific diagnoses typically associated in this category include: rheumatoid arthritis, massive rotator tear, component position failure, septic arthritis, or neurovascular injury.51
Specific ROM goals are seldom mentioned when preparing a patient for a TSA. This is true whether a patient is placed in the standard goals category or the limited goals category. The primary focus for those patients in the limited goals category is pain relief with a decreased emphasis on ROM gains. This group will achieve less than satisfactory gains in functional ROM.51
Total Shoulder Secondary to Trauma
The goals for a patient with a TSA secondary to trauma are the same as that for a patient with a TSA secondary to degeneration: pain relief and resumption of daily function in both patient populations. The most important preoperative factors that influence postrehabilitation function are the timing of the surgery in relation to the injury and the skill of the surgeon. The outcome worsens the longer the delay is between the date of the trauma and the initiation of surgery. The skill of the surgeon directly relates to the ability to align the humeral tuberosities. Finally, there are improved outcomes with larger surgery centers and higher volume surgeons.52
For patients with a traumatic reason for their total shoulder surgery, rehabilitation may be a longer period of immobilization with passive ROM only. This is to ensure appropriate boney healing. Additional time with significant precautions may exist up to 6 weeks, further delaying the potential resumption of ROM.52 The most common complication following a TSA procedure for a traumatic injury is superior migration of the humeral head, which the clinician may observe as unopposed scapular elevation or “shoulder hike” as described in the next section or in Box 7-11. There are several reasons why this may occur: failure of the rotator cuff muscles, muscular imbalance with inappropriate muscular force couple production at the shoulder, or loosening of the glenoid component.55
Troubleshooting
Shoulder Hike
The most common observable movement dysfunction is unopposed scapular elevation and/or inadequate separation of scapular and humeral motion, or in layman’s language: “a shoulder hike.” This is seen with attempts to raise the arm overhead in either a frontal or sagittal plane of motion. Weakness is only one of the impairments that may contribute to shoulder hiking. Additional impairments contributing to this movement dysfunction include inadequate transverse plane ROM, inadequate length of the scapulohumeral musculature, inadequate mobility of the glenohumeral (GH) joint capsule, and inadequate mobility of the scapula on the thorax. Determination of the primary impairment limiting this motion will guide the plan of care to eliminate the unopposed scapular elevation. For example, if the movement analysis of the patient’s shoulder noted inadequate separation of scapular and humeral motion during the first 30° of shoulder abduction, then the physical examination measures would focus on inadequate GH inferior glide, inadequate strength, or neuromuscular control of the scapular muscles that provide a stabilizing force into scapular down rotation, adduction, or scapular depression or the inadequate length of the scapulohumeral muscles.
Stiffness
Stiffness of the GH joint following TSA presents a complex problem with the origin of the stiffness including: inadequate intraoperative tissue release, an intense postsurgical inflammatory response, or slow progress in rehabilitation. Communication with the referring surgeon and the history of the ROM impairment of the patient before surgical intervention may assist the therapist’s decision-making to decrease the risk of stiffness. Initiating therapy with good pain control immediately postoperatively may prevent the development of pathologic stiffness. Presentation of stiffness later in the rehabilitation process must be evaluated for the primary contributing impairments. Consideration should be given to the GH joint capsule, flexibility of the scapulohumeral muscles, and the separation of scapular motion from humeral motion.
Infection
A patient who has decreasing ROM in conjunction with pain or increasing pain should alert the clinician to possible infection.9 Infection may present in up to 15% of all total shoulder cases53 and may occur more than 1 year following the surgical procedure.5 Though pain and loss of ROM may be the most objective signs during therapy, the therapist should be alert for drainage, warmth at the site, erythema, and effusion. Interviewing questions regarding the presence of night sweats, fever (as noted by taking body temperature), chills, remote sites of infection, or any recent invasive procedures should be asked.10 Early intervention in the acute phase of the infection yields the best result, therefore the therapist should recommend an urgent return visit to the physician for blood laboratory testing.9
Biceps Tendon Tendonitis
Biceps tendon tendonitis is a preventable complication during the rehabilitation process. The biceps has a role in shoulder flexion and is a primary humeral depressor.37 ![]() Following total shoulder surgery, the rotator cuff typically demonstrates muscular inhibition, thus increasing the demand on the biceps as the primary humeral depressor during shoulder motion. Presentation of biceps tendon tendonitis indicates continued overuse of this muscle, therefore implicating inadequate contribution from the rotator cuff muscles. Beyond regional treatment for the inflammation of the biceps tendon such as modalities, active rest, and taping, the rotator cuff muscles should be evaluated for length, neuromuscular control, and strength. The patient will have pain during active ROM, especially with shoulder flexion and shoulder abduction. Limited shoulder extension may be noted secondary to irritation as the biceps tendon is placed at a lengthened position or required to activate eccentrically. Manual muscle testing of the biceps activates this muscle for its role as an elbow flexor and forearm supinator, therefore it may be pain free and strong despite the irritation at the tendon. Attempts at special tests for tendonitis may be inconclusive because of the surgical trauma to the area and the inability of the patient to attain the necessary positions for testing.
Following total shoulder surgery, the rotator cuff typically demonstrates muscular inhibition, thus increasing the demand on the biceps as the primary humeral depressor during shoulder motion. Presentation of biceps tendon tendonitis indicates continued overuse of this muscle, therefore implicating inadequate contribution from the rotator cuff muscles. Beyond regional treatment for the inflammation of the biceps tendon such as modalities, active rest, and taping, the rotator cuff muscles should be evaluated for length, neuromuscular control, and strength. The patient will have pain during active ROM, especially with shoulder flexion and shoulder abduction. Limited shoulder extension may be noted secondary to irritation as the biceps tendon is placed at a lengthened position or required to activate eccentrically. Manual muscle testing of the biceps activates this muscle for its role as an elbow flexor and forearm supinator, therefore it may be pain free and strong despite the irritation at the tendon. Attempts at special tests for tendonitis may be inconclusive because of the surgical trauma to the area and the inability of the patient to attain the necessary positions for testing.
Clinical Case Review
1 SW is a 72-year-old female who slipped and fell 7 days ago sustaining a four-part humerus fracture. Surgical intervention resulted in TSA. She is currently 1 day postoperation and presents in the hospital room with a compression dressing over the surgical site. The surgical team has requested that she be cleared for discharge by this evening if possible. What functional assessments must be completed to ensure a safe discharge home?
Because of her history of falls, the patient’s mobility from bed to chair, sit to stand, and ambulation must be assessed for safety. Following TSA, patients typically self-limit weight bearing through the shoulder. The patient must be assessed for independent mobility with limited use of the involved upper extremity. It would be of great benefit to the patient to integrate the treatment of potential contributing impairments to lesson her fall risk.
2 RP is a 68-year-old male who underwent a right TSA 18 weeks ago. His course has been uncomplicated thus far; however, during observation of shoulder flexion, RP demonstrates a “shoulder hike.” Continued assessment for what impairments needs to occur to alter the treatment plan?
Determination of the primary impairment contributing to this movement dysfunction will guide the plan of care to eliminate the “shoulder hike.” To be most efficient, the clinician must note during which phase of the shoulder motion the “shoulder hike” does occur. For example, if the shoulder hike occurs during the last phase of scapulohumeral rhythm, then there should be a separation of humeral and scapular motion. The resources necessary for this separation to occur must be evaluated for probable impairments. Potential impairments include inadequate GH joint mobility, inadequate humeral depression, inadequate length of the rotator cuff muscles, and inadequate stabilization of the scapula by the lower trapezius.
3 It is 6 weeks after surgery for JK, who had a left TSA secondary to progressive degeneration. Today there is increased swelling noted and you have concerns of a possible infection. What signs and symptoms should you look for? What special questions should you ask?
Loss of ROM with pain or increasing pain would be associated with a potential infection following TSA. Corroborating signs may be drainage and warmth at the surgical site, erythema, effusion, and systemic signs of infection such as fever. Early intervention is necessary, therefore an urgent return to the surgeon should be recommended. Infection risk may extend to 1 year after the operation.
4 AB is a 68-year-old male who is participating in rehabilitation for a total shoulder. His pain complaints have recently moved to the anterior proximal biceps area especially with attempts to move his shoulder into flexion. What may be one of the structures contributing to this pain?
The most likely structure is the proximal biceps brachii tendon. The clinical presentation may also include: contractile pain with a midline resisted test of the shoulder flexors, pain-free contraction for midline resisted tests at the elbow, increased sensitivity to placing the biceps tendon in a lengthened position, and limited or painful shoulder abduction. Presentation of tendonitis indicates overuse of the biceps brachii as a shoulder flexor and humeral depressor, thereby implicating inadequate contribution from the rotator cuff muscles. Beyond the modality intervention for the inflammation of the biceps tendon, evaluation of the function of the rotator cuff should be considered.
5 ML recently underwent a total shoulder surgery. Surgical indications included a significant loss of motion, interrupted sleep, and pain secondary to rheumatoid arthritis of the GH joint. He has many questions regarding his expected ROM. What role does his history play in your discussion of prognosticated ROM?
Because of his medical history of rheumatoid arthritis, ML would have a higher chance of being placed in the limited goals category. A conversation with the surgeon on what ROM was accomplished during the surgical procedure would be necessary to determine the impact of his significant presurgical loss of ROM. A limited goals category means that expected ROM at the shoulder is conservatively estimated to reach: flexion: 75° to 90°, abduction: 70° to 80°, external rotation: 30°, and internal rotation: hand behind back to L5.
6 GR is 3 weeks after surgery on the right. His precautions include PROM for another week. Your treatment plan includes scapular mobilizations to prepare for appropriate scapulohumeral rhythm upon discharge of his PROM precautions. Name three key considerations for this intervention.
Scapular mobilizations are introduced to ensure appropriate mobility of the scapula on the thorax for the scapulohumeral rhythm during active ROM. The rhythm consists of phases when there is movement only by the humerus and not at the scapula and a phase where the scapula and the humerus are both in motion. Therefore, the clinician must consider length and mobility issues that will affect these relationships; namely, the mobility of the scapula and those structures that attach from the glenoid to the humerus (the GH joint capsule and the rotator cuff muscles). The patient should be positioned in a manner that allows the humerus to be passively positioned at greater than 30° of humeral abduction or 60° of humeral flexion before initiating scapular mobility. The length of the rotator cuff muscles must be addressed. Glenohumeral joint mobility must be assessed and treatment initiated if hypomobility is present.
7 MJ’s ROM precautions have been discharged and you wish to introduce him to active overhead activities. What is the primary impairment that must be addressed before initiating independent overhead activities?
Shoulder overhead motion is a complex motion that requires a significant amount of humeral external rotation ROM. This humeral motion is necessary to avoid impingement of the greater tuberosity of the humerus and the undersurface of the acromial arch as the humerus approaches 90° of shoulder motion. As this is the typical osteokinematic motion that is restricted within postsurgical precautions, many patients do not exhibit adequate external ROM to immediately begin overhead motion following discharge of precautions. To avoid the risk of subacromial impingement, external rotation ROM should be achieved first.
8TA is 65-year-old male retired construction worker. You are reviewing his home program before discharge. He comments that the pendulum exercise increases his pain. What should you do?
It is not uncommon for the pendulum exercise to be misinterpreted or performed incorrectly. It was designed to be a passive motion of the involved upper extremity generated by trunk and pelvis motion. You have two immediate choices: reeducate TA on the proper performance of the pendulum exercise and/or instruct him in the alternate of table top exercises. Table top exercises emphasize an active trunk and pelvis over a supported upper extremity thereby mimicking the pendulum exercise without the gravitational traction. The dosage is dependent on the goal of prescribing the exercise. For pain relief, multiple sessions per day with 60 seconds of performance is appropriate. If the goal is to generate ROM, then a numeric prescription is more appropriate such as 3 sets of 15 repetitions each.
9 JJ is a 69-year-old male presenting to you 6 days after a TSA on the right shoulder. He states that he feels better every day but is curious about the discoloration on his chest. During the physical examination, you note large patches of bruising along the right thorax and into the axilla. The wound appears dry and clean with some dried blood along the incision. What are your concerns?
It is not uncommon following total shoulder surgery for bruising to appear and extend into the thorax, trunk, and axilla. Two competing issues would be the presence of petechiae or potential signs of infection. Petechiae are minute hemorrhagic spots that may be present on the chest and are related to injury to the long bone of the humerus. Corroborating signs and symptoms of shortness of breath, increased pain, and traumatic injury would lead to suspicions of fat embolism. For signs of infection, the integumentary integrity of the wound should be checked including drainage, warmth, redness, and/or excessive edema into the axilla or the distal arm. Following major surgery, all patients should be monitored for signs and symptoms of infection including the taking of body temperature. JJ should be educated on these signs and symptoms.
10 MP is a 71-year-old female who is 10 weeks postsurgery. Her chief concern is difficulty with overhead motion. AROM of shoulder flexion is135°. PROM of shoulder flexion is 168°. During your movement analysis, you note inadequate scapular upward rotation during the mid phase of motion (60° to 160°) of shoulder flexion. What are the hypotheses of possible contributing impairments?
Inadequate scapular upward rotation could be a result of weakness of the upper trapezius, lower trapezius, and the serratus anterior because all are upward rotators of the scapula. Other hypotheses include inadequate mobility of the scapula on the thorax because of adaptive shortening of the downward rotators or inadequate motor planning of the force couples of the serratus anterior and trapezius muscles.
11 AB is progressing in therapy and wishes to begin overhead repetitive activities. As a clinician you would stage him as between phases II and III. What is a key measurement in shoulder ROM that assists with recommending overhead motion activities?
External rotation of the shoulder at 0° of humeral abduction and at 90° of humeral abduction should be closely monitored if the patient has had surgical restrictions to avoid external rotation. The end of phase II recommends the patient have 40° of PROM into external rotation. Although 45° of AROM and full PROM into external rotation demonstrate the end of phase III, the clinician must not overemphasize overhead activities until the patient has achieved an adequate amount of external rotation for the movement to be completed without multiple compensations and risk of tissue irritation.
12 YM is nearing discharge. He is 14 weeks after surgery. Though he has been walking in the pool and using various flotation devices, he has not progressed to full, unassisted freestyle swimming. What are the key criteria for successful return to this activity?
YM’s timeline for integumentary healing and bone healing is appropriate. The therapist should be knowledgeable of the stroke mechanics for freestyle swimming, especially the necessary ROM and muscle actions. If the active ROM is appropriate, then the home program will have to emphasize not only traditional strength training parameters but also a timed repetitive component to more aptly mimic the muscle activities during swimming.