CHAPTER 23 Total proctocolectomy with ileal-pouch anal anastomosis
Step 1. Surgical anatomy
♦ Chronic ulcerative colitis (CUC) is an inflammatory bowel disease limited to the mucosa of the rectum and colon. Although no etiologic factor has been identified, population studies suggest there is both a genetic and an environmental component contributing to the development of CUC. The disease course is characterized by intermittent flares of disease activity. Medical therapy for the intestinal manifestations of CUC is directed at controlling symptoms by modulating the inflammatory process. To date, no medical therapy is curative. However, surgical removal of the colon and rectum cures the intestinal manifestations of the disease and eliminates or markedly reduces the associated risk of malignancy in long-standing CUC. Surgical intervention for CUC is divided into two broad categories, emergent and elective, that will influence the type of surgery performed. Emergency operations are directed at life-threatening complications of CUC and are not intended as definitive surgical treatment for CUC. Alternatively, elective surgery is intended as a definitive treatment for the intestinal symptoms. In appropriately selected patients, the best surgical option is the total proctocolectomy with an ileal pouch-anal anastomosis (IPAA). The IPAA avoids the need for a permanent stoma while maintaining the normal route of defecation.
♦ This is a technically demanding operation and should be performed by surgeons comfortable with both the technical aspects of the procedure and management of the many possible complications. Traditionally, this complex operation has been performed through a midline laparotomy. However, improved technology and increased surgical experience with advanced laparoscopy have permitted a number of surgeons and centers to offer a minimally invasive approach to the IPAA procedure. Although the initial laparoscopic IPAA experience was characterized by long operative times, experience and new technology have significantly reduced operative times while maintaining the safety and clinical outcomes, making the laparoscopic IPAA comparable to the open procedure.
Step 2. Preoperative considerations
Patient preparation
♦ In chronic ulcerative colitis (CUC) patients with fulminant or toxic disease, the appropriate choice of operation is a total abdominal colectomy with Hartmann pouch and end ileostomy. This operation removes the majority of the diseased organ, allows the patient to be tapered off of all immunosuppressive medications, and regain their health and nutritional status before proceeding to a definitive restorative operation (IPAA).
♦ Prior to proceeding to an IPAA, the diagnosis of CUC or indeterminate colitis needs to be firmly established. Crohn’s disease is a considered a significant contraindication for proceeding to an IPAA.
♦ Patients need to visit with an enterostomal therapist for pre-operative stoma marking and to begin education regarding the care of the stoma. Using a laparoscopic approach for an IPAA results in a significantly shortened length of stay in hospital and decreases the opportunity for education regarding stoma management.
♦ We do not routinely use oral antibiotics nor a mechanical bowel preparation as it tends to cause bowel distension with liquid stool which makes colon manipulation more difficult. Each patient receives one or two tap water enemas the morning of operation.
♦ The operating room requirements for an efficient laparoscopic TPC-IPAA include:
 an electronically controlled operating table with a significant range in side to side tilt and steep Trendlenberg and reverse Trendlenberg capability to facilitate the use of gravity to move the small intestine out of the way of dissection.
an electronically controlled operating table with a significant range in side to side tilt and steep Trendlenberg and reverse Trendlenberg capability to facilitate the use of gravity to move the small intestine out of the way of dissection. a non-skid operating table surface to minimize patient movement on the table during the numerous position changes. This reduces the risk of the patient sliding off of the table as well as shear injury to the patient’s skin which can predispose to pressure related skin breakdown. An alternative approach is to use a “bean bag.”
a non-skid operating table surface to minimize patient movement on the table during the numerous position changes. This reduces the risk of the patient sliding off of the table as well as shear injury to the patient’s skin which can predispose to pressure related skin breakdown. An alternative approach is to use a “bean bag.” a minimum of three video monitors, preferably four, are available for use during the case with two positioned off the shoulders of the patient and one at the foot of the table.
a minimum of three video monitors, preferably four, are available for use during the case with two positioned off the shoulders of the patient and one at the foot of the table. ideally all the equipment should be off the floor attached to ceiling booms which permit easier movement of equipment during the procedure.
ideally all the equipment should be off the floor attached to ceiling booms which permit easier movement of equipment during the procedure.♦ All patients require a padded chest strap placed securing them to the table. They need to be positioned in modified Lloyd-Davies lithotomy with both arms padded, protected, and tucked against their torso. The patient’s legs are placed in leg holder that allows the hips and thighs to be flat with respect to the abdomen but the lower leg to be positioned downward (i.e. Yellofin® Stirrups, Allen® Medical Systems). These leg holders minimize the chance of patient movement on the table during positioning changes as well as permitting access to the perineum for placement of a circular stapler or a vaginal retractor/manipulator.
♦ In patients who have recently received or are currently on steroids, a brief pulse of steroids is appropriate during the peri-operative period.
Room setup and patient positioning
♦ The patient is placed in the modified lithotomy with both arms padded, protected, and tucked against the torso. It is important that the thighs are positioned in such a way that they are level with the abdomen. A chest strap is applied to minimize the risk of the patient shifting on the operating table during frequent position changes during the procedure. Ideally, video monitors are available on movable booms to permit placement above the patient’s left and right shoulders and one in the area between the patient’s legs during different phases of the operation.
Step 3. Operative steps
Laparoscopically-assisted (LA) approach
♦ A diamond configuration for trocar placement is used. Four trocars, three 5-mm and one 10–12-mm are placed.
♦ A 10-12 mm trocar is placed in the future ileostomy site after an open technique is used to enter the abdomen. Pneumoperitoneum is established and laparoscopic exploration of the abdomen is undertaken with a 5 mm 30 degree laparoscope to assess the feasibility of proceeding with a minimally invasive approach.
♦ Extensive adhesions, unanticipated anatomic or inflammatory processes that preclude a minimally invasive should prompt immediate conversion to an open procedure.
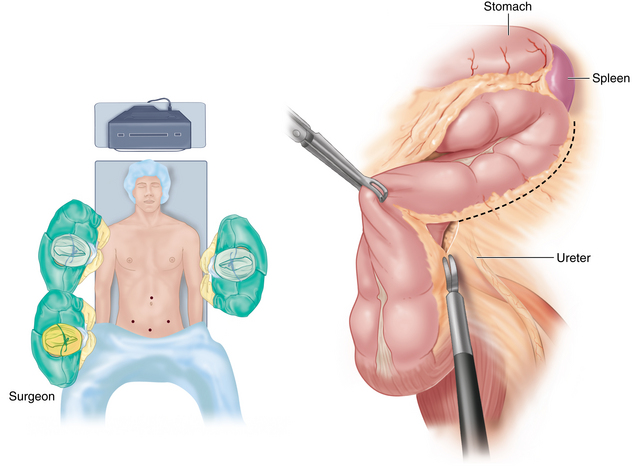
♦ The remaining 5-mm trocars are placed under direct vision in a diamond configuration with one in the left lower quadrant, one in the midline in the suprapubic position, and the last one in the midline above the umbilicus (Fig. 23-1).
♦ During the procedure, the first assistant is always standing across from the surgeon while the camera operator is positioned next to the surgeon. For the majority of the procedure, the camera will be used in supraumbilical trocar.
Left colon mobilization
♦ The patient is placed in maximal Trendelenburg with the left side elevated 30-degrees. The surgeon is positioned on the patient’s right side with the camera operator standing next to the surgeon closest to the patient’s head. The camera is placed in the midline supra-umbilical trocar.
♦ The surgeon will be using the right lower and suprapubic trocars to begin the mobilization of the left colon. The white line of Toldt is incised, reflecting the left colon medially as it is freed from the lateral peritoneal attachments (Figure 23-6). The laparoscopic retractor is used from the right lower quadrant trocar while the dissector is in the suprapubic position.
♦ A critical step during this portion of the operation is identification of the left ureter. It is important to mobilize the colon in the appropriate plane which close to the colonic border as it is quite easy to dissect behind the kidney.
♦ The mobilization of the sigmoid and left colon is considered complete when it is medial to left ureter along its entire course.
♦ The distal aspect of the splenic flexure can be mobilized while the patient is in this position. However, to complete the mobilization the patient is repositioned into reverse Trendelenburg while maintaining the left side elevated.
♦ To facilitate dissecting more proximally on the transverse colon, the surgeon moves between the patient’s leg to utilize the suprapubic and left lower quadrant trocars. The camera operator remains on the patient’s right side while the assistant moves to the right side to use the right lower quadrant trocar site to provide retraction of the omentum upward while the surgeon retracts down into the abdomen.
♦ The splenic flexure is mobilized off Gerota’s fascia and the tail of the pancreas. Once the flexure has been fully mobilized from the lateral aspect, the lesser sac must be completely opened. (Fig 23-3) This ensures that distal transverse colon and splenic flexure can be brought to the umbilicus to facilitate extraction of the specimen if extra-corporeal vessel division is utilized.
Right colon mobilization
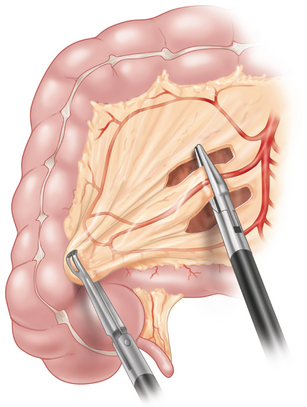
♦ Once the left colon and splenic flexure are mobilized, attention is turned to the mobilizing the right colon, hepatic flexure, and the small bowel mesentery.
♦ The patient is once again placed in maximal Trendelenburg with the right side elevated approximately 30 degrees.
♦ The surgeon and camera operator move to the patient’s left side. The small bowel is retracted into the left upper quadrant.
♦ Using a grasper through the left lower quadrant trocar the terminal ileum and cecum are retracted up and toward the left upper abdomen.
♦ The dissecting instrument is placed through the suprapubic trocar. The peritoneum surrounding the terminal ileum and cecum is incised to reveal the retroperitoneal plane and underlying structures.
♦ Similar to the left side it is extremely important to identify and protect the right ureter.
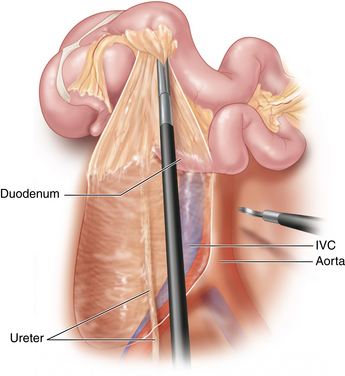
♦ The right colon is dissected free from the lateral peritoneal attachments. Once the lateral attachments are divided attention is turned to completing the mobilization of the small bowel mesentery off of the retroperitoneum (Fig 23-2).
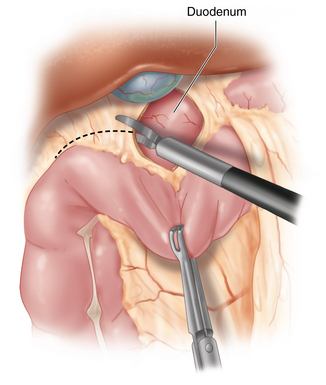
♦ This dissection is considered complete when the mesentery is mobilized off of the duodenum. It is critical to mobilize the small bowel mesentery to this extent to ensure adequate length of the mesentery to allow the ileal pouch to reach the pelvic floor.
♦ After the small bowel and right colon are mobilized, the hepatic flexure must be freed.
♦ The patient is repositioned into reverse Trendelenburg maintaining the right side elevated.
♦ With surgeon and camera operator remaining on the patient’s left, the gastro-colic ligament is grasped near the bowel and elevated toward the abdominal wall. Entering the space between the gastro-colic ligament and the transverse mesocolon will facilitate mobilization of the hepatic flexure, which proceeds laterally. (Fig 23-1)
♦ The duodenum is identified from the superior aspect. With continuous retraction toward the left lower quadrant, the hepatic flexure is freed from the peritoneal attachments to the duodenum and the head of the pancreas.
♦ Similar to the left colon mobilization of the right colon is only considered complete once the entire right colon and proximal transverse colon can be mobilized to the umbilicus.
Proctectomy
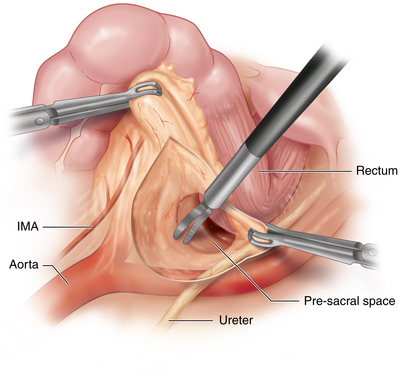
♦ The surgeon moves to the patient’s right side as does the camera operator to begin the dissection. The left pararectal fascia opened after both the left and right ureters are once again identified.
♦ Scoring the fascia to the left of the rectum, the presacral space is entered. This maneuver is repeated on the right side of the rectum. The surgeon alternates dissecting right to left until the two dissection planes meet behind the rectal
Vessel ligation
♦ We routinely use two methods for vessel division.
♦ In a thin patient, the peri-umbilical extraction site can be used. In this situation, a 4-5 cm peri-umbilical incision is made and the entire colon is exteriorized through this incision. The vessels are then divided extra-corporeally.
♦ The alternative method is to use a vessel sealing device intra-corporeally.(Fig 23-5) Ideally, this should be a 5 mm instrument to avoid the need for placement of larger trocars.
Exteriorization, pouch construction, and anastomosis
Once all vessels are ligated, the colon and rectum are removed from the abdomen.
♦ If the vessel were divided via a peri-umbilical incision, this site serves as the extraction site.
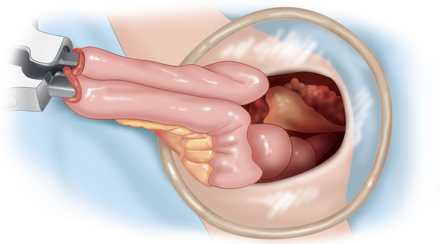
♦ If the vessels were divided intra-corporeally, then a Pfannenstiel incision or a low midline incision may be utilized. The terminal ileum is transected close to the ileal-cecal valve with a linear stapler. The colon specimen is passed off the field and sent to pathology.
♦ Through the extraction incision, the pouch is constructed extra-corporeally, similar to open surgery. The length is assessed by stretching the small bowel downward externally. If the apex of the proposed pouch reached 3-5 cm below the top of the pubic symphasis, then adequate length is present to perform the anastomosis. If not, then different lengthening maneuvers can be performed.
♦ The distal ileum is placed in a J configuration and a linear GIA stapler is inserted through an incision at the apex. The lumen of the pouch is constructed by dividing the two opposing internal walls of J-shaped small bowel loop. Usually, two firings of the linear stapler are used to ensure an adequate small bowel reservoir. The anvil of the circular stapler is secured in the pouch apex.
♦ The pouch is placed back into the abdomen and the extraction site is closed or sealed in a manner that allows pneumoperitoneum to be reestablished.
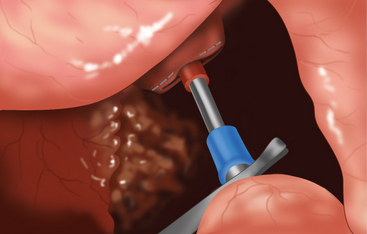
♦ The patient is placed in mild Trendelenburg and under laparoscopic visualization an end-to-end anastomosis (EEA) stapler is inserted through the anus and brought out adjacent to the rectal staple line. The anvil exiting the pouch apex is grasped and connected with the rectal EEA stapler.
♦ Once correct orientation of the pouch and pouch mesentery is confirmed, the stapler is fired. The pelvis is filled with irrigation fluid and under laparoscopic visualization the pouch–anal anastomosis is tested by insufflating the pouch with a proctoscope inserted via the anus.
♦ A closed suction drain is placed through the left 5-mm ports and positioned behind the pouch.
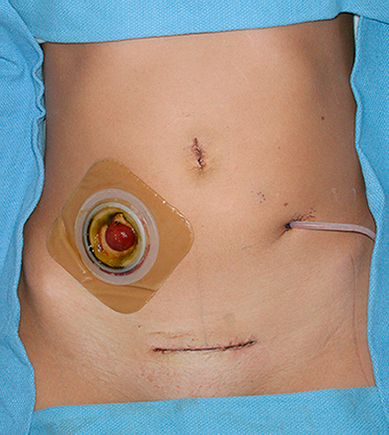
♦ A loop ileostomy is constructed approximately 20-25 cm proximal to the pouch and is brought out the site in the right lower quadrant where the 10-12 mm trocar had been placed. The remaining trocars are removed, the fascia and skin incisions are closed, and the loop ileostomy is matured.
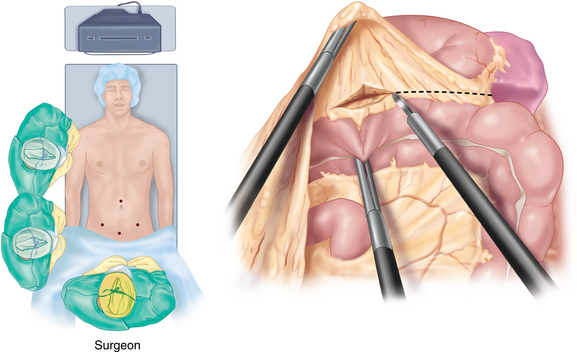
Hand-assisted approach
♦ The surgeon can use their hand to retract the colon and to facilitate the dissection. In essence, the hand access device should be considered a “trocar” for the set-up.
♦ We replace the suprapubic trocar with the hand-access device either using a low midline or Pfannenstiel incision.
♦ The laparoscopic mobilization of the colon is performed by the surgeon who stands between the patient’s legs. The sequence of the colonic mobilization and changes in the patient position during the procedure are the same.
♦ Since the transverse colon and flexure (hepatic and splenic) vessels may not reach the lower abdomen, intra-corporeal vessel ligation is the norm when using a hand-assisted approach.
♦ Once the colon is completely mobilized, the rectal dissection can be performed via a laparoscopic approach as previously describe or through the hand-access device using a traditional open approach.
♦ The pouch can be constructed as previously described and placed down into the pelvis using this incision.
Step 4. Postoperative steps
♦ Only oral gastric tubes are used during the operations and removed at the end of the case.
♦ IV fluids are minimized during the case and in the post-operative period. Fluid boluses are kept to a minimum as increased total body water is associated with delayed return of bowel function and post-operative complications.
♦ Urinary catheters are removed 48 hours after surgery.
♦ All patients are started on a full liquid diet the morning after surgery. This is limited to less than 1 liter intake on the first day. If the full liquids are tolerated, the next day an unrestricted soft diet it begun.
Step 5. Pearls and pitfalls
A minimally invasive approach to a total proctocolectomy with ileal pouch-anal anastomosis is a technically demanding operation that provides a number of short-term benefits for the patient. Using a systematic approach to the mobilization of the colon and rectum permits a high success rate for completing the procedure laparoscopically. Using a hand-access device is an alternative that may permit a minimally invasive approach for a patient not thought to be a laparoscopic candidate, or to reduce the difficulty of the procedure for a less experienced laparoscopic surgeon.
Farouk R, Pemberton JH, Wolff BG, et al. Functional outcomes after ileal pouch: anal anastomosis for chronic ulcerative colitis. Ann Surg. 2000;231;6:919-926.
Larson DW, Cima R, Dozois EJ, et al. Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch anal anastomosis a single institution case-matched experience. Ann Surg. 2006;243(5):667-672.
Larson DW, Dozois EJ, Piotrowicz K, et al. Laparoscopic-assisted vs. open ileal pouch–anal anastomosis: functional outcome in a case-matched series. Dis Colon Rectum, 48. 2005:1845-1850.
Larson DW, Nelson H. Laparoscopic colectomy for cancer. J Gastrointest Surg. 2004;8(5):636-642.
Larson DW, Young-Fadok TM. Laparoscopic ileal pouch: anal anastomosis. Rochester, NY: Mayo Clinic. 2002.