CHAPTER 78 Total facial alloplastic augmentation
Historical background
The senior author (E.O.T.) is widely recognized for his unique and bold contribution to the development of reproducible and more anatomically precise alloplastic implants for facial rejuvenation (Terino, 1992). This was a time period when the surgical community was still greatly influenced and biased toward the sole use of autologous craniofacial reconstruction techniques pioneered by the Paul Tessier (Tessier, 1971).
In the 20th century, chin alloplastic augmentation was first described in 1948 (Rubin and Walden, 1955). Gonzalez-Ulloa is credited to be among the first surgeons to describe malar augmentation with alloplastic implants (Gonzales-Ulloa, 1957). In the mid-1960s, Ulrich Hinderer developed unilateral corrective malar silicone implants (Hinderer, 1975).
The evaluation
Patient evaluation for total alloplastic facial augmentation includes the following:
• What problem does the patient want you to solve?
• Get the patient’s verbal description of his/her “ideal scene” appearance of facial change.
• Patient “homework assignment”: bring magazine photos of specific “do’s and don’ts” on desired anatomic part changes.
• Have older patients bring a variety of earlier personal photos.
• Use computer face photos (five views) and imaging technology to do the consultations.
• Use an anatomic facial zone model and facial type analysis.
• Use a personality profile test of the surgeon’s choosing to objectably predict patient satisfaction, an extremely important consideration after downplayed or ignored to the risk of the surgeon.
Applied anatomy for total alloplastic facial augmentation
Interrelationships of the facial promontories
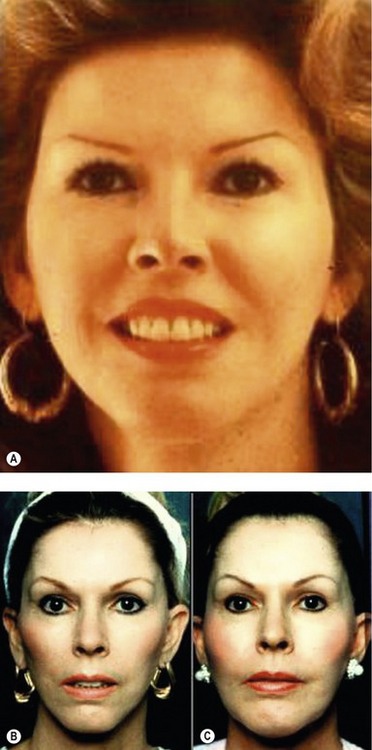
These are three major promontories of volume and mass. In order of importance, they are the nose, the two malar zygomatic eminences, and the chin–jaw line (Fig. 78.1). The supraorbital ridges, constitute a fourth promontory, which are of lesser significance (and will not be discussed in this chapter).
By altering the interrelationships of the three major prominentories, a surgeon can uniquely create or restore facial harmony, balance, and beauty. By mathematical law, the diminution or enhancement of any one of the three promontories directly and inversely affects the aesthetic importance of the others. Facial aesthetics is the art and science of achieving beauty by creating a balance in all three elements of facial skeletal anatomy. One important method by which the aesthetic surgeon can accomplish this balance is by properly employing alloplastic implants (Fig. 78.2). Recent advances in applied alloplastic implant technology now make it possible for the surgeon to make subtle or dramatic changes in the facial promontories with ease and predictability.
The restructuring of all these layers still has many limitations. Patients who display round, full, fleshy facial contours with an abundance of subcutaneous fat rarely appear beautiful by contemporary standards. Conversely, there are lean-faced individuals with a tendency to a longer facial contour with inadequate skeletal promontories in the malar or mandibular regions or both. Both extremes of these facial types, as well as innumerable patients who have combinations of volume deficiencies in varying anatomic locations can be significantly improved by rearranging the balance of their skeletal promontories with targeted alloplastic augmentation techniques. Furthermore, contour surgery of the facial skeleton should also be complemented by a wide variety of other sound coordinated facial procedures (Fig. 78.3).
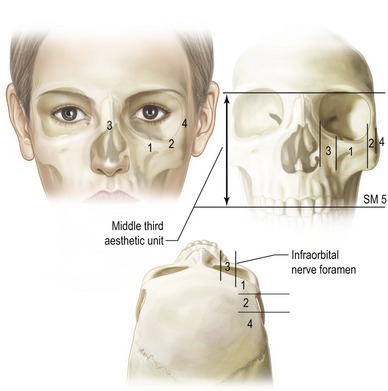
Zonal anatomy of the malar and premandible regions
That part of the facial skeleton which, when appropriately augmented, produces an aesthetic change in the contour of midface can be called the “malar-midface space”. To determine the most aesthetic augmentation to select for that space, it is useful to partition the midface region into five distinct anatomic zones (Terino, 1992) (Fig. 78.4). By understanding these five zones and their interrelationships, the surgeon can vary cheek and/or midface shapes to accommodate each unique patient.
Summary of zones
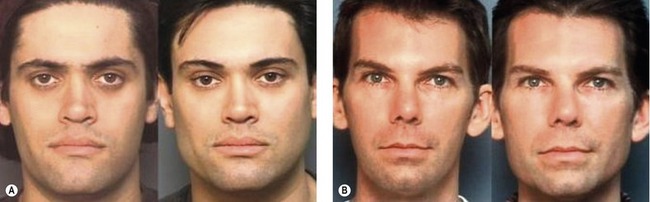
Zone 1, the largest area, includes the major portion of the malar bone and the first third of the zygomatic arch. Augmentation of this entire zone produces the greatest volumetric filling of the cheek and also maximizes the projection of the maxillary eminence (Fig. 78.5).
Zone 2, the second most important site, overlies the middle third of the zygomatic arch. Enhancement of this zone along with zone 1 increases accentuation of the cheek bone laterally, giving a broader dimension to the upper third of the face, and creating a high, arched appearance. This change of contour is particularly useful for individuals with a narrow upper face or a long-face syndrome. When, however, zones 1 and 2 are augmented in excess, an abnormal and unattractive protuberance may result (Fig. 78.6).
Zone 3 is the paranasal area, which lies medial to the infraorbital foramen and nerve. A line drawn vertically down from the infraorbital foramen marks the medial extent of the usual dissection for malar augmentation. This line also represents the lateral border of zone 3. When paranasal augmentation in zone 3 occurs, medial fullness of the face is created, often in the upper nasolabial area, which can be unattractive or can produce a “chipmunk-cheek” effect. The skin and subcutaneous tissues are thin in that region; consequently, any implant placed there must be carefully sculptured and tapered. Augmentation of zone 3 is indicated for certain reconstructive purposes, following trauma or other heredity deficiencies (Fig. 78.7).
Zone 4 overlies the posterior third of the zygomatic arch. Augmentation in this area is never needed as it would produce an unnatural appearance. Moreover, dissection here may be dangerous, since it is very possible to injure the zygomaticotemporal or orbicularis oculi branches of the facial nerve, and even the capsule of the temporomandibular joint. Infrequently, deformities have been observed that resulted from operations in this area.
Zone 5, the submalar zone or “submalar triangle,” is bounded posteriorly by the tendonous surface of the masseter muscle, and anteriorly by the canine fossa region of the maxilla. The superior boundary of zone 5 is the inferior margin of the malar bone, which constitutes the first two thirds of the zygomatic arch. The medial extent of the submalar space ends at the lateral border of the nasolabial mound and sulcus. Its anterior limit is bounded by the inferomedial portion of the roof of the entire malar-midface space. It contains the overlying facial musculature, fat, skin, and subcutaneous of the midface region. The inferior limit is selected by the surgeon in the natural dissection plane that separates the masseter from the overlying facial musculature according to the desired configuration of midface fullness selected by the patient. This equates to creating certain breast shape by choosing the lower limit of the submammary sulcus.
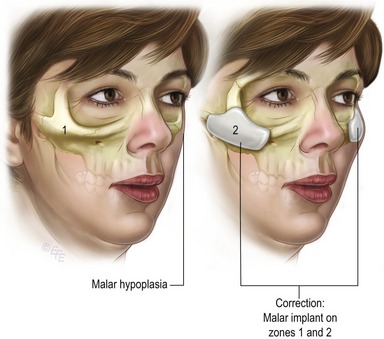
Fig. 78.5 Malar hypoplasia and the resulting malar-midface contour from Zone 1, 2 malar volume enhancement.
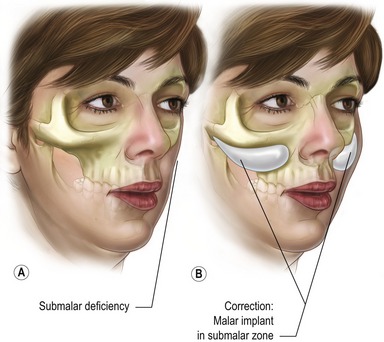
A type 2 facial aesthetic deficiency consists of a soft tissue contour depression specifically in the lower aspect of the midfacial aesthetic unit called the submalar zone 5 (SM5) or submalar “triangle”. This deficiency resides over the masseter tendon and the canine fossa lying under the inferior border of the malar bone and zygomatic arch. A large malar shell implanted over the inferior aspect of the malar bone in zone 1 and extending into the submalar space below the border of the malar bone creates the illusion of a round, full “apple cheek” in females.
By definition, a comprehensive augmentation of the entire malar-midface unit may require an implant shell with maximal transverse dimensions of 5.5 cm across and 4.5 cm vertically. A type 2 face has adequate malar bone prominence, but is deficient in submalar soft tissue volume. This creates a flat, older, midface contour. This frequently occurs in the aging face of both males and females. In a young individual with strongly defined cheekbones and yet deficiencies in the midface soft tissues, a submalar augmentation produces aesthetic softness, and adds youthful fullness to the face. Some people feel strongly that a submalar implant can lift the nasolabial sulcus and give the illusion of facial tightening that will postpone the perceived need for rhytidectomy. The authors have not observed this occurrence. The authors favor volume filling of the midface just posterior to the nasolabial mound, in order to de-emphasize the appearance of fullness and simultaneously correct the soft tissue volume deficiency in the midface.
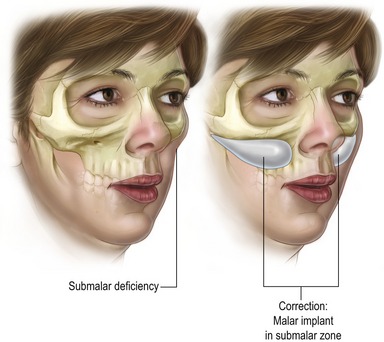
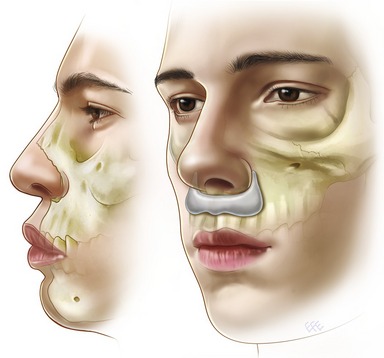
A type 3 facial aesthetic deficiency in a face consists of a very strong malar zygomatic superstructure and a very sunken submalar infrastructure. Such faces often have thin skin and subcutaneous support requiring a generous submalar augmentation with a projecting implant thickness (5–8 mm). This facial type occurs with aging, as well as from heredity (Fig. 78.8). The appearance is that of an emaciated, drawn, haggard and even sick countenance. This can result from soft tissue disease states such as Romberg’s hemi-atrophy and HIV lipodystrophy. The remedy, for any etiology, is the same: a generous volume filling of the submalar zone 5 (SM5) (Fig. 78.9).
Type 5 aesthetic facial deficiency exists as a weakness of facial structure in the suborbital “tear trough” region. This creates a tired and “hollow” appearance around the eyes, especially in the lower orbital region. There may also be a tendency for the eyeball itself to look proptotic due to the “negative vector” orbit (Fig. 78.10).
When this volume deficiency is also accompanied by significant malar-zygomatic hypoplasia the new suborbital tear trough-malar shell (SOTTM) is indicated (Fig. 78.11). Autogenous tissue transplants of fat, muscle, galea and temporalis fascia into this area by a variety of authors have been only partially successful because all autologous grafts, due to unpredictable cell death, demonstrate variable shrinkage and contour irregularities. Their success and complication rate are still debated. More recent techniques for “SOOF” infraorbital dissections which release and elevate the suborbital cheek and malar soft tissue structures beneath the orbital rim and transpose intraorbital fat exist and are more successful in correcting this deficiency but still remain dependent on the locally available tissue mass.
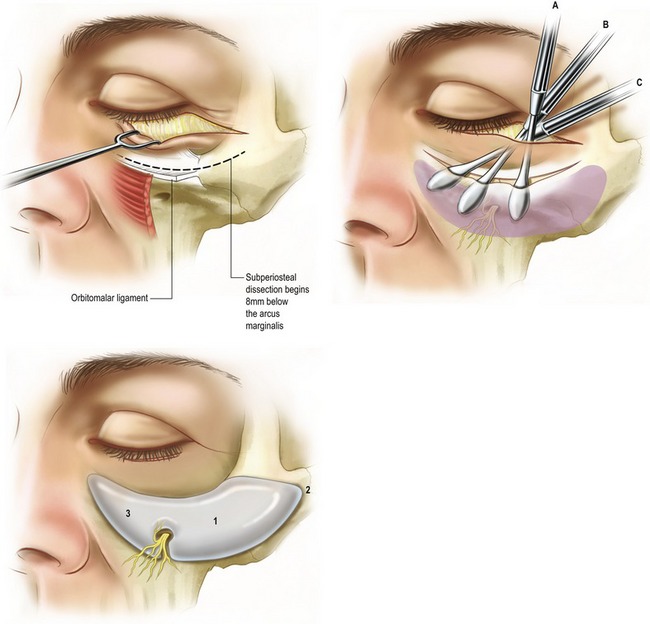
Fig. 78.11 The new suborbital tear trough–malar implant and the technique for insertion around the infraorbital nerve.
Type 6 aesthetic deficiencies are extremely common in all races and are frequently overlooked by aesthetic surgeons. However, mild to moderate forms of premaxillary retrusion can have significant aesthetic improvement from alloplastic augmentation. There are several ways to do this; a silicone rubber implant has been specially designed to fit around the lower pyriform aperture. It is easily placed either directly onto the bone through intraoral or intranasal incisions. Its natural anatomic shape and posterior contour provide stability when positioned properly (Fig. 78.12).
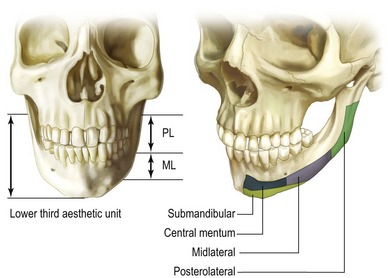
Zonal anatomy of the premandible
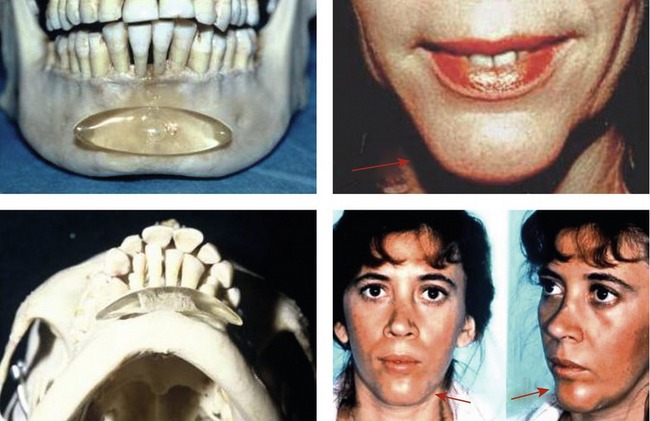
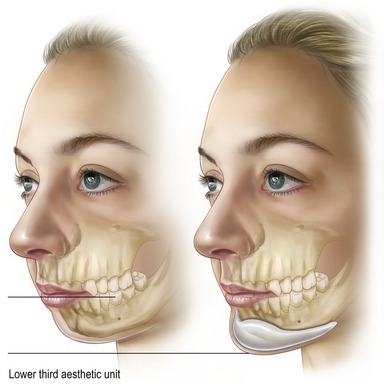
Techniques for chin augmentation have been amplified by extending the shape and size of the traditional, centrally placed implant to provide more lateral and posterior alteration of the chin contour. Oval chin implants have traditionally been placed between the mental foramen. Implants placed only into this central segment often produce an unattractive, round, central protuberance (Fig. 78.13). Moreover, displacement of the origins of the mentalis muscle by traditional chin implant surgery may result in a downward dislocation of the overlying soft-tissue mound and musculature, thereby creating the dreadful “witch’s chin” or “drooping chin” deformity. Furthermore, an adjacent soft tissue sulcus between the central chin mound and the sagging, more lateral jowl elements produce “marionette lines” or the “anterior mandibular sulcus”.
Therefore, to achieve natural chin augmentation, the “premandible space” must be taken into consideration. This region can be configured into four functional anatomic zones (Terino, 2002) (Fig. 78.14).
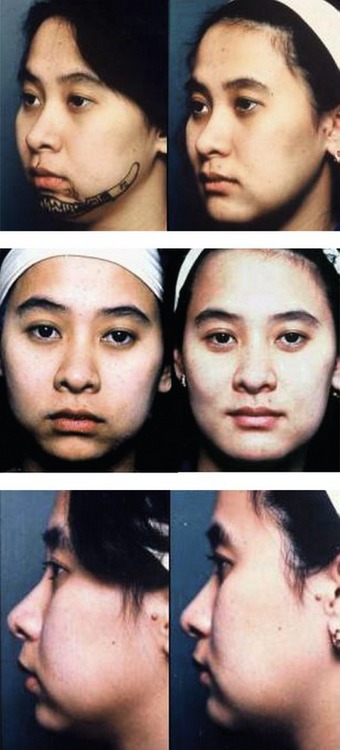
Extending the premandible space laterally into the middle half of the horizontal ramus, and the region of the oblique line, enables the surgeon to define a midlateral zone (ML) of the mandible. Augmentation of this zone, in addition to the central mentum, creates a chin-jawline that has a natural contour (Figs 78.15, 78.16). This embodies the principle of the “extended anatomic contour” implants designed by the senior author (E.O.T.). For maximal aesthetic enhancement, augmentation within the midlateral zone, and even further into the more posterior part of the mandible, creates broadening which appears to shorten the face as well as give greater definition of the mid and posterior aspects of the jaw line. The posterolateral segment of the premandibular space, overlies the posterior half of the horizontal ramus, extending back from the oblique line and including the angle of the mandible and its ascending ramus. Augmentation creates a sculptured enhancement of the posterior jaw line.

Fig. 78.15 Anatomic design implants are contoured posteriorly to securely fit the bony surface like a glove.
The fourth and final premandibular zone resides beneath the inferior border of the mandible and is called the submandibular zone (Fig. 78.17). Traditional chin implants have lacked the ability to extend volume deficient mandibles in a vertical direction. The newer implants, however, have been designed to wrap around the bony margin of the mandible to increase the vertical height of the face from the lower lip to the inferior chin line, thereby augmenting the submandibular zone (Fig. 78.18).
Technical steps of alloplastic facial augmentation
* IMPLANTECH Corporation – Ventura, California.
When placed directly on bone, smooth silicone implants become rapidly fixed and securely surrounded by capsular fibrosis. Because this creates a space well-demarcated, they can be removed readily and exchanged when necessary or desirable. On the other hand, porous implants that permit tissue ingrowth such as high-density polyethylene, e.g. Medpor, fenestrated implants, and implants with Dacron backing have a low but consistent, predictable, and clinically significant incidence of infection (Carboni, Gasparini et al., 2002). They are also significantly more difficult to exchange or modify due to bone sequestration and other locally induced tissue interactions. Perhaps, most pertinent is the recognition that Medpor is also more likely to extrude when placed under thinner tissue coverage (Sevin, Askar et al., 2000).
Preoperative planning
Preoperative planning for all plastic and reconstructive surgery is the critically essential step for achieving successful results. For aesthetic surgery, such planning must include accurate and definitive communication with the patient, whose perceptions and expectations the surgeon must understand completely. For traditional surgery on aging patients, communication about their needs and wishes may be relatively simple. They wish to have their prior youthful contours and facial features restored as completely as possible. With the passing years, individuals accommodate to the slow, gradual changes that take place in the soft-tissue contours of their faces. The limited technical results of routine tissue repositioning and tightening techniques from traditional facial aesthetic surgery may therefore be acceptable to them, because they do produce some significant visible albeit limited postoperative improvements.
Although there currently is an assortment of ever-evolving tools for measuring aesthetic skeletal parameters, precise implementation of facial form still remains challenging, even in the most experienced hands. Therefore, before the surgeon attempts an alloplastic facial contour alteration, it is imperative that he or she knows exactly what facial image the patient desires. The authors request their patients to modify photographs of themselves and bring them in, or to provide, from fashion magazines or other sources, examples of facial contours that they admire, namely, faces that they feel look similar to their own but are more attractive in the pertinent skeletal areas (Fig. 78.19). Although this process may run contrary to standard residency teaching, it creates an understanding of patients’ expectations by providing invaluable visual insights and imagery to discuss. Most patients do have very precise ideas about the images of facial contours they wish to emulate. Therefore, when they do not, it is easy to discover that their expectations cannot be met. In elective operations, surgeons must not undertake what they are not sure they can accomplish especially when the patient’s own visually described goals are poorly defined. Overall, the authors find computer imaging technology to be indispensable in this process.
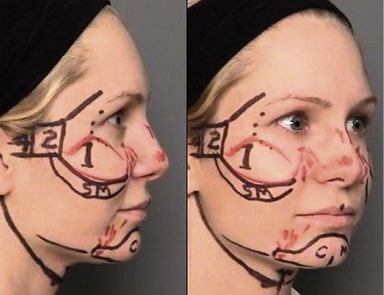
During patient consultations, it is important to determine the desired anatomic zones to augmentation, because, by definition, this is responsible for the patient’s postoperative appearance. Multiple consultations with the patient are important to precisely define the final desired outcome. On the morning of surgery, quality time spent in marking, measuring, and discussing surgical details with the patient is essential. Finally, by drawing the preoperative configurations of the pertinent regional and zonal anatomic landmarks on the patient’s face, the surgeon is provided with guidelines for accurately performing the intraoperative surgical dissection and implant placement (Fig. 78.20).
Suggested operative techniques
With regard to operative technique, the authors offer the following suggestions:
1. Stay directly on the bone and the periosteum. Placement of implants directly on bone creates a firm and secure attachment to the skeleton. Capsular contracture has not been seen with facial anatomic implants.
2. Be gentle in elevating the soft tissues from the malar and premandible regions. When there is adequate infiltration of local anesthetic agents, the tissue planes separate easily and without need for forceful trauma. Excessive trauma may produce mental nerve symptoms, transient or prolonged, but rarely permanent. Paresis or paralysis of the zygomaticus, the orbicularis oculi, and even the frontalis muscle may occur. Such damage is usually temporary, but in rare cases it can be permanent and has never occurred in the authors stories of over 3500 chin implants.
3. Expand the dissection space adequately in either the malar or the premandible regions to accommodate the chosen prostheses comfortably. Elevation of the soft tissues into areas adjacent to bone should be done with a blunt-edged elevator and, again, as gently as possible. Anatomically contoured implants of adequate size and shape present very few problems in malposition or mobility because they fill the space comfortably and hold their position by virtue of their contoured posterior surface and their rapid fixation to bone.
4. Minimize bleeding by using both local and general anesthesia. A “dry operative field” is essential for accurate visualization, precise dissection, and proper placement, the three critical factors in avoiding potential problems with hematoma, seroma, infection, inaccurate placement; and nerve damage. Maintenance of the systolic blood pressure between 90 and 110 provides optimal hemostasis in combination with infiltration of a dilute lidocaine 0.2% solution containing epinephrine (adrenaline), 1 : 800,000. Clonodine, 0.2 mg by mouth, may also be given immediately preoperatively to stabilize the hemodynamics of the patient’s blood pressure and pulse.
| The ideal anesthesia for alloplastic facial contouring is as follows: |
Technical elements
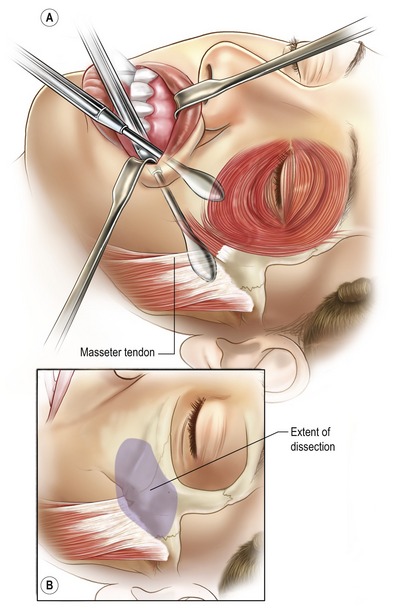
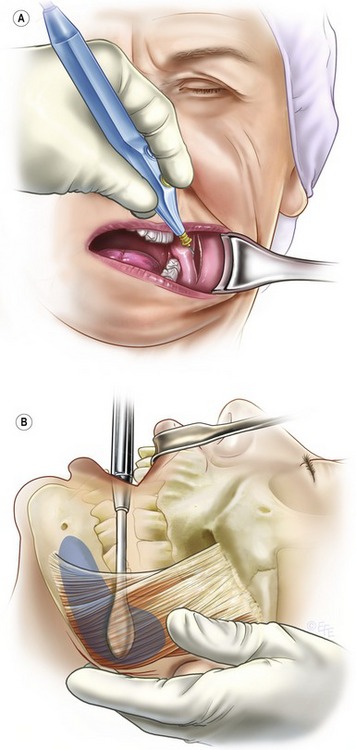
A spatula-shaped elevator with a 1 cm wide blade is placed directly under the periosteum and under the orbicularis oris muscle in a vertical orientation at the inferior base of the maxillary buttress, in the apex of the gingival-buccal sulcus. The overlying soft tissues are swept obliquely upward over the maxillary eminence by maintaining the elevator directly on bone. The elevator should always remain on the bony margin along the inferior border of the malar eminence and zygomatic arch (Fig. 78.21).
Manual palpation of the previously marked zonal design of the malar space anatomy on the skin is performed, while the underlying elevator mobilizes the tissues directly from the bone. This maneuver includes palpating the orbital rim and the upper and lower borders of the zygoma as the elevator dissects the subperiosteal space within these areas (Fig. 78.22).
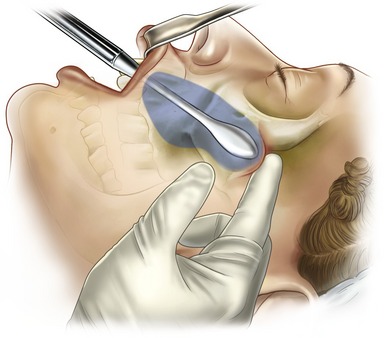
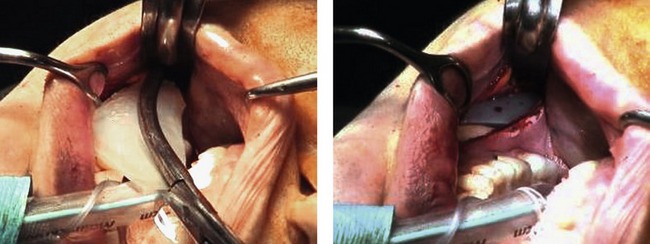
In the submalar zone, the soft tissues are swept off the shiny, white, glistening, fibrous tendon of the masseter muscle in an inferior and outward direction. This opens up the submalar space for approximately 1–2 cm, depending on the desired choice of cheek shape and the corresponding implant necessary to achieve it. When adequate anesthesia techniques are used, the intraoral approach permits excellent visualization of the skeletal anatomy and musculature. This exposure allows accurate implant placement into zones 1, 2, and 5 (SM5). It permits the surgeon to place a spatula elevator above and below the implant to make certain that its edges are not buckled or that the zygomatic extension of the implant is not curled. It is not necessary to visualize the infraorbital nerve, but it is rather easy to do so when required, or when an implant is used for the suborbital region.
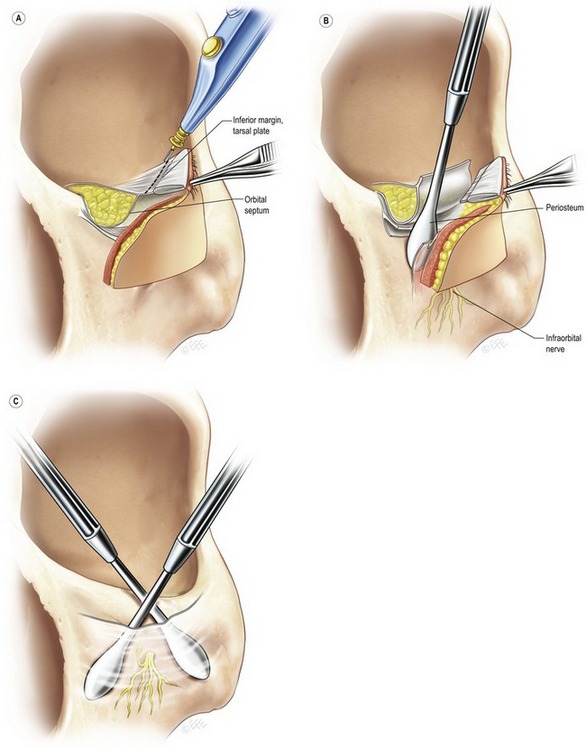
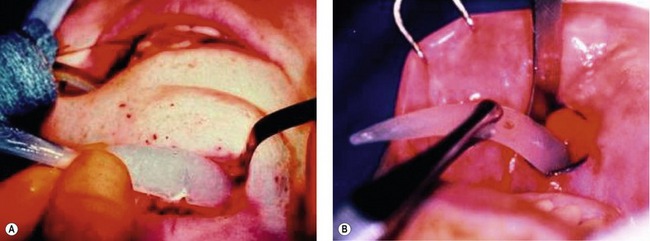
Subciliary blepharoplasty approach
In the standard subciliary blepharoplasty approach, an incision is made 3 mm below the lash line, and limited in its lateral extension to avoid scars in the lateral canthal region. This approach may be used either in conjunction with routine blepharoplasty or as an independent route of entry for a malar implant. When used for implant placement alone, the incision is limited to a length of 10–15 mm. It is designed only in the middle to lateral third of the lower eyelid, in the subciliary region (Fig. 78.23). Moreover, the dissection inferiorly provides a sturdy shelf upon which the implant rests.
The rhytidectomy approach
Zone 1 of the malar region is a safe zone for penetration through the superficial musculo-aponeurotic system (SMAS) into the malar space. There are no named branches of the facial nerve in that region. Once the rhytidectomy flap is elevated over zones 1 and 2, the roof of the malar space can be directly penetrated through the SMAS with a small, sharp elevator onto the malar bone. This may be done either medial or lateral to the zygomaticus origins. The seventh nerve branches leading to the frontalis muscle run more proximal over the middle third of the zygomatic arch, and the motor nerve to the orbicularis oculi is more superior. By creating a transverse aperture that parallels facial nerve fibers, nerve risk is minimal. It is important to remember that dissection backward along the zygomatic arch is necessary to position a malar shell implant comfortably and correctly without a buckling of the lateral tail.
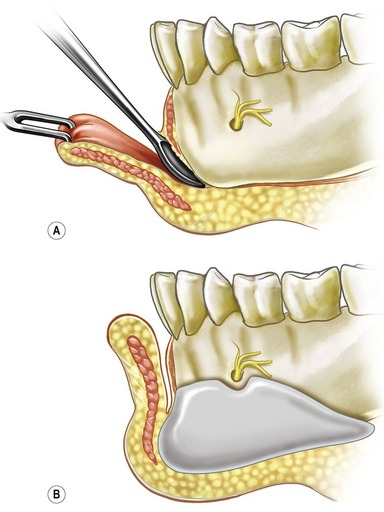
Premandible augmentation technique
Although operations to augment the central mandible for aesthetic purposes have existed for over 50 years (Millard, 1954), and plastic surgeons have well understood the advantages of improved nasomentum profile relationships, it is only within the last 30 years that methods have been developed for augmenting the premandible by extending central chin implants over a larger surface area as well and with using anatomically designed alloplastic devices. These techniques also make it possible to alter the shape and size of the midlateral and posterior aspects of the mandible, and even to lengthen the submandibular segment vertically.
Access to the premandible space can be achieved by either the standard intraoral route or the submental route (Fig. 78.24). These authors use the submental approach exclusively for operations that require additional surgery in the submental and submandibular region, such as liposculpturing and platysmal contouring.
In both approaches, the incisions are transverse and 2 cm long. The intraoral transverse incision is through mucosa only. The mentalis muscles are then divided vertically through their midline raphe to avoid transection of the muscle bellies and total detachment from their bony origins (Fig. 78.25). This aperture provides direct access downward onto the bony plane and eliminates the muscle weakening that occurs with customary transection methods.
In one operation, the senior author inadvertently placed a premandible implant superior to the mental nerves bilaterally. The immediate result was compression symptoms in the form of anesthesia of the lower lip. Unfortunately, other facial procedures performed at the same time (rhytidectomy and blepharoplasty) obscured the diagnosis until the swelling had diminished. The implant was repositioned beneath the nerves on the ninth postoperative day. Replacement of an implant or repositioning can easily be done within the first 10 to 14 days. By applying the basic principles of wound healing taught during residency, the surgeon is able to re-enter the premandible or malar space to replace or reposition implants prior to the rapid increase in wound tensile strength, which occurs from 14 to 21 days after the operation.
Posterolateral implants are placed through a posterolateral incision. The posterolateral incision is transverse and is located approximately 1.5–2 cm anterior and adjacent to the angle of the mandible. Appropriate space for placement is created by making a direct dissection onto bone and subperiosteally beneath the masseter muscle (Fig. 78.26). A curved elevator is used to dissect around the posterior aspects of the ascending ramus in the angle region. In this way, implants designed to fit securely around the angle of the mandible can be accurately positioned (Figs 78.27, 78.28). As with all facial implant incisions, a two-layer closure of muscle and mucosa is optimal.
Complications
The major disadvantages of the use of alloplastic materials are several:
1. Possibilities of severe infection, especially with porous materials which become infiltrated with fibrotic ingrowths or bone sequestrum that complicates ready removal.
2. Contour abnormalities of an unattractive or even disfiguring nature when implants do not have the proper shape, size and positioning.
3. Possibilities for facial nerve and musculature damage due to excessive and inappropriate trauma during dissections to introduce or to remove the implant materials.
4. Complications from the intraoral approach include dysesthesias from damage to the infraorbital nerve or motor dysfunction of the orbicularis oris musculature. Nerve symptoms may be attributed to transection of small branches in the lip during the incision or direct damage to the major nerve bundle during dissection or pressure impingement on the nerve from an implant. These complications, however, are rare and almost nonexistent when the previously stated guidelines to dissection are applied.
5. Use of traditional transverse incisions through the muscle pillars of the zygomaticus produce traumatic transection, resulting in transient and perhaps even permanent damage to muscle function. This can inhibit normal lip elevation.
6. During the subciliary dissection, the infraorbital nerve is also intentionally avoided. An incision is made in the periosteum 3–4 mm anterior to the orbital rim along its lateral aspect, to obviate potential adhesions that may result in ectropion and lower lid contracture. A skin flap should never be used, because it always shrinks and predisposes to eyelid retraction and ectropion. By utilizing a skin-muscle flap approach, however, there should be no trauma to the orbicularis muscle.
7. Excessive muscle damage, with bleeding into lid tissues, stimulates fibrosis and contracture within the middle lamella of the lower eyelid, producing ectropion. Standard lateral canthopexy techniques are used to minimize this possibility. Resection of skin and muscle flap should be conservative, i.e., minimal to no excision, because of additional traction exerted on the lower eyelid from the volume expansion caused by the implant under the malar tissues.
8. Incisions that transact muscle fibers not only lead to inadequate closure but also may create weakness and laxity of the mentalis muscle, thereby contributing to a potential for chin ptosis. Ptosis of the mentalis musculature and soft-tissue mound of the central mentum is described in the literature as one of the controversial aspects of alloplastic implants. Indeed, the possibility for deformities, such as central drooping and a “witch’s chin” does exist. They can be prevented, however, by using the previously described vertical entrance wound and securely approximating the mentalis muscle pillars during closure. The mentalis muscle can easily stretch to accommodate the introduction easily large, extended anatomic implants.
9. Central implants except for large customized “square front” implants almost always create a central mound deformity with an adjacent “anterior mandibular prejowl sulcus” and potential “witch’s chin” or “drooping” appearance.
Pearls & pitfalls
Pearls
• Infection and cellulitis around facial implants made of silicone rubber (Silastic) can almost always be resolved by antibiotics and/or drainage procedures when necessary.
• Smooth surfaced silicone rubber (Silastic) implants have a thin overlying capsule immobilizing them. They are easy to insert and easy to remove or replace.
• Implants placed in a subperiosteal location directly on bone or a stable base such as the masseter muscle will be fixed and mobile. Non-subperiosteal placement will result in mobility.
• Bone remodeling or erosion occurs to a degree with all implant materials. With over 50 years of experience to date no significant number of dental problems have been reported and then only for implants with improper placement higher up against tooth roots.
• Except for complete transactions or major damage, nearly all nerve injuries completely recover with time.
Pitfalls
• Not analyzing and discussing with patients their pre-existing asymmetries and the impossibility of predicting total correction thereof.
• Attempting re-operations, improvements or corrections during the interval of 17 days to 1 year following initial procedures when reactivation of scar contracture is restimulated and/or density of scar adherences can predispose to nerve damage.
• Letting a patient convince the surgeon that the implants are too big or out of a desired position; i.e. before 6 months to 1 year when nearly all swelling has suspended.
• Making a subperiosteal implant space too big or too small.
• “Forcing” a dissection in areas around the mental or infraorbital nerves and especially in the midface submalar and malar zygomatic areas when trying to expand the space more lateral and posterior where the main trunks and branches of the facial nerve reside.
Carboni A, Gasparini G, et al. Evaluation of homologous bone graft versus biomaterials in the aesthetic restoration of the middle third of the face. Minerva Chir. 2002;57(3):283–287.
Gonzales-Ulloa M. [Selective regional plastic restoration by means of esthetic unities]. Rev Bras Cir. 1957;33(6):527–533.
Guerrero-Santos J. The role of the platysma muscle in rhytidoplasty. Clin Plast Surg. 1978;5(1):29–49.
Hinderer UT. Malar implants for improvement of the facial appearance. Plast Reconstr Surg. 1975;56(2):157–165.
Millard DR, Jr. Chin implants. Plast Reconstr Surg. 1954;13(1):70–74.
Rubin LR, Walden RH. A seven year evaluation of polyethylene in facial reconstructive surgery. Plast Reconstr Surg. 1955;16(5):392–407.
Sevin K, Askar I, et al. Exposure of high-density porous polyethylene (Medpor) used for contour restoration and treatment. Br J Oral Maxillofac Surg. 2000;38(1):44–49.
Terino EO. Alloplastic facial contouring: surgery of the fourth plane. Aesthet Plast Surg. 1992;16(3):195–212.
Terino EO. Three-dimensional facial contouring: alloplastic augmentation of the lateral mandible. Facial Plast Surg Clin North Am. 2002;10(3):249–264.
Tessier P. The definitive plastic surgical treatment of the severe facial deformities of craniofacial dysostosis. Crouzon’s and Apert’s diseases. Plast Reconstr Surg. 1971;48(5):419–442.