Chapter 560 Thyroiditis
Lymphocytic Thyroiditis (Hashimoto Thyroiditis, Autoimmune Thyroiditis)
Clinical Manifestations
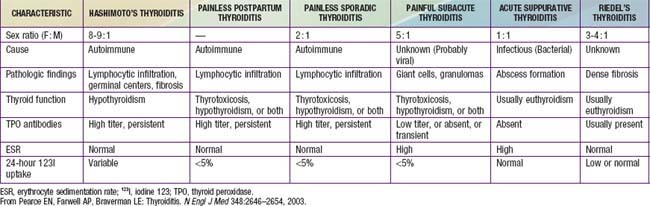
Lymphocytic thyroiditis is also associated with certain chromosomal disorders, particularly Turner syndrome and Down syndrome. In children with Down syndrome, one study reported that 28% had antithyroid antibodies (predominantly anti-TPOs), 7% had subclinical hypothyroidism, 7% had overt hypothyroidism, and 5% had hyperthyroidism. In a study of girls with Turner syndrome, 41% had antithyroid antibodies (again, predominantly anti-TPOs), 18% had goiter, and 8% had subclinical or overt hypothyroidism. Another study of 75 girls with Turner syndrome found that autoimmune thyroid disease increased from the 1st (15%) to the 3rd (30%) decade of life. Boys with Klinefelter syndrome are also at risk for autoimmune thyroid disease. The differential diagnosis is noted in Table 560-1.
Other Causes of Thyroiditis
Specific conditions such as tuberculosis, sarcoidosis, mumps, and cat-scratch disease are rare causes of thyroiditis in children. Other forms of thyroiditis seen in adults, such as painless sporadic thyroiditis and Riedel thyroiditis, are rare in children (see Table 560-1).
Corrias A, Cassio A, Weber G, et al. Thyroid nodules and cancer in children and adolescents affected by autoimmune thyroiditis. Arch Pediatr Adolesc Med. 2008;162:526-531.
Demirbilek H, Kandemir N, Gonc EN, et al. Hashimoto’s thyroiditis in children and adolescents: a retrospective study on clinical, epidemiological and laboratory properties of the disease. J Pediatr Endocrinol Metab. 2007;20:1199-1205.
de Vries L, Bulvik S, Phillip M. Chronic autoimmune thyroiditis in children and adolescents: at presentation and during long-term follow-up. Arch Dis Child. 2009;94:33-37.
Dittmar M, Kahaly GJ. Immunoregulatory and susceptibility genes in thyroid and polyglandular autoimmunity. Thyroid. 2005;15:239-250.
Gopalakrishnan S, Chugh PK, Chhillar M, et al. Goitrous autoimmune thyroiditis in a pediatric population: a longitudinal study. Pediatrics. 2008;122:e670-e674.
Hollowell JG, Staehling NW, Flanders D, et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87:489-499.
Radetti G, Gottardi E, Bona G, et al. The natural history of euthyroid Hashimoto’s thyroiditis in children. J Pediatr. 2006;149:827-832.
Svensson J, Ericsson UB, Nilsson P, et al. Levothyroxine treatment reduces thyroid size in children and adolescents with chronic autoimmune thyroiditis. J Clin Endocrinol Metab. 2006;91:1729-1734.
Wang SY, Tung YC, Tsai WY, et al. Long-term outcome of hormonal status in Taiwanese children with Hashimoto’s thyroiditis. Eur J Pediatr. 2006;165:481-483.
Yoshida A, Hisatome I, Taniguchi S, et al. Pendrin is a novel autoantigen recognized by patients with autoimmune thyroid diseases. J Clin Endocrinol Metab. 2009;94:442-448.