Thyroid disease in pregnancy
1. How does normal pregnancy affect maternal thyroid function?
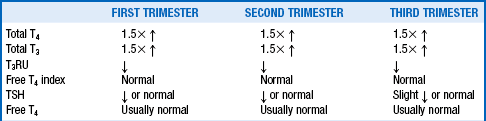
The profound hormonal influences that change the physiology of pregnancy and the increased metabolic demands of the fetus cause significant changes in maternal thyroid function (Table 40-1).
2. Why must thyroid function tests be interpreted cautiously in pregnancy?
The influence of estrogen and human chorionic gonadotropin (hCG) on circulating thyroid hormone levels requires that thyroid function tests in pregnancy be interpreted cautiously. Estrogen increases thyroid-binding globulin (TBG) by two- to threefold beginning a few weeks after conception. The result is an approximately 50% increase in serum total thyroxine (TT4) and total triiodothyronine (TT3) levels because circulating thyroid hormones are highly protein bound. Throughout pregnancy, the range for both hormones should be approximately 1.5 times the nonpregnant range. Measurement of the triiodothyronine (T3) resin uptake (T3RU), which is inversely related to serum thyroid binding capacity, is correspondingly low, so that the calculated free thyroxine (T4) index (FT4I; product of multiplying the total T4 by the T3RU) is usually normal. Although the measured free T4 (FT4) and free T3 (FT3) levels are usually normal in pregnancy, they must be interpreted with caution because the reference ranges provided by manufacturers have been established using pools of nonpregnant sera. These free assays may also be influenced by changes in TBG and albumin unless they are measured by an equilibrium dialysis method or online solid phase extraction–liquid chromatography/tandem mass spectrometry (LC/MS/MS), but these methods are expensive and usually not available. Only 0.03% of serum TT4 content is unbound to serum proteins and is the FT4 available for tissue uptake. Further, the very high TBG levels, the low albumin levels, and the high nonesterified fatty acids characteristic of pregnancy may all affect the FT4 immunoassays. A slightly low FT4 in the late second or third trimester may be normal or may represent true hypothyroidism and should be interpreted in the context of the thyroid-stimulating hormone (TSH) and TT4 levels. If TSH is less than 3.0 mU/L and TT4 is 1.5-fold elevated, it is unlikely that the patient has true hypothyroidism. If possible, pregnancy-specific norms for FT3 and FT4 should be established by the laboratory.
TSH values are also affected by the thyrotropic effect of hCG; in one large series, the 95% confidence limits were as low as 0.03 mU/L in the first and second trimesters and 0.13 mU/L in the third trimester, with an upper limit of normal of less than 3.0 mU/L in the first trimester and less than 3.5 mU/L in the second and third trimesters. Ethnicity-related differences are also significant. Black and Asian women have TSH values that are, on average, 0.4 mU/L lower than in white women. Guidelines from both the American Thyroid Association (ATA) and the Endocrine Society recommend that an upper TSH limit of 2.5 mU/L be used in the first trimester and 3.0 mU/L in the second and third trimesters, especially if thyroid peroxidase (TPO) antibodies are positive and individual laboratories do not offer gestation-specific normal ranges. The TSH must also be interpreted in the context of the actual thyroid hormone levels. If the TT4 and TT3 are less than 1.5-fold elevated compared with the nonpregnancy range and the FT4 and FT3 hormones are not increased, the suppressed TSH may reflect the effect of hCG, but it could also be caused by subclinical hyperthyroidism from Graves’ diseases or a hot nodule. None of these conditions warrants treatment.
3. What particular effects may be seen during the first trimester?
During the first trimester, high hCG levels may stimulate thyroid T4 secretion sufficiently to suppress the serum TSH into the range of 0.03 to 0.5 mU/L in up to 15% of pregnant women. In a study of women with hCG concentrations higher than 200,000 IU/L (which is not uncommon in twin pregnancies), the TSH was less than or equal to 0.2 mU/L in 67% of women. The TSH may be slightly suppressed in the second trimester, but by the third trimester, it is usually within the normal range. The beta subunit of hCG has 85% sequence homology in the first 114 amino acids with TSH and can bind to and stimulate the TSH receptor. Levels of hCG higher than 50,000 IU/L, which may be seen when hCG peaks at the end of the first trimester, can therefore increase the FT4 level enough to suppress the serum TSH. However, the TSH is usually detectable, the TT4 is less than 1.5-fold elevated above the nonpregnancy range, and FT4 is usually within the normal range. A TSH in the high-normal range (> 2.5-3.0) during the first trimester is therefore suggestive of subclinical hypothyroidism.
4. Why must the mother significantly increase thyroid hormone production during pregnancy?
 Maternal plasma volume expands 30% to 40%, requiring a concomitant expansion of the thyroid hormone pool.
Maternal plasma volume expands 30% to 40%, requiring a concomitant expansion of the thyroid hormone pool.
 Placental type 3 deiodinase (D3) activity results in increased maternal T4 metabolism to reverse T3.
Placental type 3 deiodinase (D3) activity results in increased maternal T4 metabolism to reverse T3.
 Transfer of T4 across the placenta to the fetus occurs.
Transfer of T4 across the placenta to the fetus occurs.
 High TBG levels decrease the levels of free hormone.
High TBG levels decrease the levels of free hormone.
 Gastrointestinal absorption of exogenous thyroid hormone may be impaired by iron in prenatal vitamins.
Gastrointestinal absorption of exogenous thyroid hormone may be impaired by iron in prenatal vitamins.
5. What factors may compromise maternal ability to increase thyroid hormone production?
Women with limited thyroid reserve as a result of thyroiditis, partial ablation, or surgical resection may be unable to increase thyroid hormone production during pregnancy and often develop hypothyroidism. Women with inadequate iodine intake may also develop hypothyroidism and a goiter because iodine requirements increase by approximately 40% to 50% in pregnancy.
6. What is the “goiter of pregnancy”?
The goiter of pregnancy has been well described in iodine-deficient areas of the world, but it does not occur in geographic regions that are iodine replete. In fact, one of the first pregnancy tests to be developed in iodine-deficient areas was a loosely braided choker necklace that broke when a woman developed such a goiter. The thyroid gland increased in size with each subsequent pregnancy.
7. Why do iodine requirements increase in pregnancy?
Iodine requirements increase markedly during pregnancy as a result of increased urinary iodine losses secondary to the 50% to 100% increase in glomerular filtration rate (GFR) during pregnancy, the diversion of iodine to the fetus for thyroid hormone synthesis, and increased maternal thyroid hormone requirements.
8. What is the recommended iodine intake during pregnancy, and how can it be met?
The World Health Organization’s recommendations for iodine intake are 250 μg/day during pregnancy and lactation and 150 μg/day in the nonpregnant state. Iodine insufficiency is an increasing problem in the United States as a result of the availability of deiodinated salt and is estimated at 5% to 10%. Because most prenatal vitamins do not contain iodine, women of childbearing age should be instructed to use only iodinated salt or to make sure to ingest a prenatal vitamin containing iodine.
9. What happens if iodine intake is insufficient?
If iodine intake is insufficient, thyroid hormone production drops, resulting in increased secretion of TSH, which then stimulates thyroid gland growth. Thyroid volume commonly increases by 30% or more during pregnancy in iodine-deficient regions and often does not completely regress after delivery. Many European and developing countries with endemic iodine deficiency do not supplement with iodine; therefore, women are at risk of iodine-deficiency goiters during pregnancy. When iodine intake is severely deficient, overt hypothyroidism results both in the mother and the fetus. Endemic cretinism occurs if severe hypothyroidism secondary to iodine deficiency goes unrecognized and untreated at birth.
10. What happens to thyroid gland volume in iodine-replete areas during pregnancy?
In iodine-replete areas, such as the United States, thyroid gland volume may increase by 10% to 15%, primarily as a result of pregnancy-induced vascular swelling of the gland. Although this enlargement can be recognized by ultrasound, it cannot usually be appreciated by palpation. Therefore, any goiter found during pregnancy in an iodine-replete area should be evaluated in the same manner as a goiter occurring outside of pregnancy.
11. Does thyroid hormone cross the placenta?
Thyroid hormone crosses the placenta poorly but significantly, partly because of the high placental activity of the type 3 monodeiodinase (D3) that converts T4 to reverse T3 (rT3) and T3 to T2. However, it is now clear that some T4 does cross the placenta, because fetuses with complete thyroid agenesis have approximately 30% to 40% of the normal amount of thyroid hormone at birth. The amount of maternal thyroid hormone transported across the placenta appears to be protective to the brain, and neurologic development of the newborn usually progresses normally as long as thyroid supplementation is begun immediately after birth. Evidence also suggests that transthyretin, a circulating thyroid hormone binding protein synthesized and secreted by the placenta, may provide a mechanism for delivery of thyroid hormone to the fetus. To date, six thyroid hormone transporters have been identified in placental tissue. However, T3 crosses the placenta poorly, and T3 preparations should not be used in pregnancy.
12. Does iodine cross the placenta?
Iodine easily crosses the placenta for use by the fetal thyroid, which, after 12 to 14 weeks of gestation, takes up iodine even more avidly than does the maternal thyroid.
13. What about thyrotropin-releasing hormone (TRH) and TSH?
TRH, but not TSH, also crosses the placenta and has been used in experimental protocols to attempt to accelerate fetal lung maturity.
14. Summarize the ability of thyroid-related antibodies to cross the placenta.
Immunoglobulin G (IgG) TSH receptor-stimulating antibodies (thyroid-stimulating immunoglobulins [TSI] and TSH receptor antibodies [TRAB]) cross the placenta as early as 18 to 20 weeks of gestation and can occasionally cause fetal or neonatal hyperthyroidism in infants of women with Graves’ disease when antibody levels are at least 2.5-fold elevated. It is recommended that both TSI and TRAB be measured because if either antibody is 2.5 to 3 times normal, surveillance for fetal Graves’ disease is indicated. Although anti-TPO antibodies and antithyroglobulin (TG) antibodies can also cross, they usually have no clinical significance in affecting fetal thyroid function. In rare cases, they may be associated with thyrotropin receptor-blocking antibodies that can cause transient neonatal hypothyroidism.
15. List common medications that cross the placenta.
16. Describe fetal thyroid function and brain development.
At approximately 12 to 14 weeks of gestation, the fetal thyroid gland develops, and the hypothalamic-pituitary-thyroid axis begins to function. Before 16 weeks, however, the fetus relies solely on transplacental delivery of T4. Significant amounts of thyroid hormone cross the placenta in the first trimester and early second trimester before the fetal thyroid begins functioning, and they appear necessary for normal brain development. Thyroid hormones and type 2 deiodinase (D2) have been observed in the fetal cerebral cortex by 5 to 7 weeks. These findings emphasize the importance of maternally derived T4 conversion to T3 in the brain in influencing neuronal and astrocyte proliferation and migration early in pregnancy. Rat studies indicate that fetal brain T3 depends on an adequate supply of T4 and cannot be replenished by T3 alone. In early pregnancy, when adequate fetal thyroid hormone is crucial for normal neurologic development, fetal brain T4 levels reflect maternal levels. Further, T4 is taken up by receptors on fetal brain astrocytes and is deiodinated to produce T3, thus underscoring the importance of maternal T4 in pregnancy.
17. Is fetal thyroid hormone production independent of the mother?
After the first and early second trimesters, the fetal hypothalamic-pituitary-thyroid axis is fairly independent of the mother, with the exception of its dependence on adequate maternal iodine stores. Antithyroid drugs or high levels of TSI or TRAB may, however, affect fetal thyroid function or cause goiter development at this stage. Thyroid hormone and TBG levels increase in the fetus and plateau at about 35 to 37 weeks of gestation. High fetal levels of rT3 and low T3 levels are maintained throughout the pregnancy as a result of the high placental D3 activity. The fetal pituitary-thyroid axis is relatively immature, however, considering the increased fetal TSH levels relative to the low level of T4 production at birth. At the time of labor and in the early neonatal period, there are dramatic increases in T4 levels and the capacity of the liver to convert T4 to T3.
18. What is gestational transient thyrotoxicosis or thyrotoxicosis related to hyperemesis gravidarum?
Gestational transient thyrotoxicosis (GTT) refers to maternal hyperthyroidism caused by elevated levels of hCG, which binds to the TSH receptor and can stimulate thyroid hormone release. Levels greater than 75,000 IU/mL, which may be seen in women with hyperemesis gravidarum, twin gestation, and especially molar pregnancies, can often cause hyperthyroidism. Posttranslational modification of the sialylation of hCG can change its affinity for the TSH receptor and half-life in the circulation, thus resulting in elevated thyroid hormone levels in the first half of pregnancy. A woman who presents with hyperthyroidism, vomiting, and a positive pregnancy test should have a fetal ultrasound examination to exclude a molar pregnancy.
Women with hyperemesis gravidarum (persistent nausea and vomiting accompanied by electrolyte derangements and at least a 5% weight loss) commonly have abnormal thyroid function tests. In one of the largest series yet to be published, half of the 57 women with hyperemesis gravidarum had elevated FT4 levels.
19. What are the most common causes of hyperthyroidism in pregnancy? During what period of gestation is hyperthyroidism most likely to occur?
Hyperthyroidism complicates pregnancy in about 0.2% of women. Graves’ disease, the most common cause of hyperthyroidism in pregnancy, accounts for nearly 85% of the cases. Autoimmune thyroid disease is most likely to manifest in the first trimester or the postpartum period because the immune suppression of pregnancy has been shown to decrease thyroid antibody levels significantly during the second and third trimesters. Other causes include toxic multinodular goiters, solitary toxic adenomas, iodine-induced hyperthyroidism, and subacute thyroiditis. As noted earlier, hCG-induced hyperthyroidism is common in women with hyperemesis gravidarum or hydatidiform moles and also usually manifests in the first trimester.
20. Summarize the diagnostic approach to the pregnant woman with hyperthyroidism.
Normal pregnancy can produce clinical features that mimic hyperthyroidism, such as heat intolerance, mild tachycardia, increase in cardiac output, a systolic flow murmur, peripheral vasodilatation, and a widened pulse pressure. Weight loss may be obscured by the weight gain of pregnancy. As in the nonpregnant state, hyperthyroidism in pregnancy is usually characterized by low serum TSH levels and increased serum levels of FT4. However, in interpreting thyroid tests in pregnant women, it is important to realize that serum TSH levels are also frequently low in normal pregnant women, especially during the first trimester of pregnancy (see Question 2).
21. How can the various causes of hyperthyroidism be differentiated with certainty?
Radioisotope scans are contraindicated during pregnancy; therefore, the differential diagnosis of hyperthyroidism in pregnant women must be based on the history, physical examination, and laboratory testing. An obstetric ultrasound study may be indicated to exclude a hydatidiform mole or to look for twin pregnancies.
22. What findings help distinguish Graves’ disease from GTT?
Although a diffusely enlarged thyroid gland with a bruit in a woman with ophthalmopathy and pre-pregnancy symptoms strongly suggests Graves’ disease, the diagnosis is often less clear because these findings may be absent. If a woman is actively vomiting, the distinction between early Graves’ disease and gestational hyperthyroidism accompanied by hyperemesis gravidarum may be particularly difficult. It is unusual, however, for women to develop hCG-induced hyperthyroidism at hCG levels less than 50,000 IU/mL. Clues pointing to Graves’ disease rather than hCG-induced hyperthyroidism include the presence of a goiter, ophthalmopathy, onycholysis, or preexisting hyperthyroid symptoms antedating the pregnancy. In addition, TSI or TRAB levels are often positive and T3 levels are generally higher in Graves’ disease because hyperemesis gravidarum results in a compromised nutritional state and decreased conversion of T4 to T3 in peripheral tissues.
23. Why is it important to distinguish GTT from Graves’ disease?
It may be difficult to differentiate GTT from other causes of hyperthyroidism because autoimmune hyperthyroidism also commonly manifests during the first trimester of pregnancy, and the biochemical profile of the two conditions is similar. However, it is extremely important to determine whether the thyrotoxicosis results from Graves’ disease or GTT because the latter usually resolves without antithyroid treatment by approximately 18 weeks when hCG levels decline. It is rarely necessary to treat with beta-blocker therapy or antithyroid drugs given that the hyperthyroid state is usually self-limited. Hyperthyroidism is probably not the cause of the nausea. Instead, it appears that hCG mediates both the hyperthyroidism and the nausea by different mechanisms.
24. Why is the woman’s original country of residence significant?
Women who have goiters from areas of endemic iodine deficiency and who move to the United States may develop iodine-induced hyperthyroidism when they suddenly become iodine replete. Hot nodules can also occur and do not improve in later pregnancy with the immune suppression of pregnancy.
25. What are the risks of Graves’ disease to the mother?
Inadequately treated hyperthyroidism in the mother can result in preeclampsia, weight loss, tachycardia, proximal muscle weakness, anxiety, and atrial fibrillation. Left ventricular dysfunction can occur and is usually reversible, but it may persist for several weeks after biochemical hyperthyroidism has been corrected. This cardiac condition may place the pregnant woman at risk for the development of congestive heart failure, especially in the presence of superimposed preeclampsia, infection, anemia, or at the time of delivery. Thyroid storm can rarely occur in these women.
26. What are the risks to the fetus of maternal Graves’ disease?
Inadequately treated maternal hyperthyroidism can result in fetal tachycardia, severe growth restriction, premature births, and a ninefold increased incidence of low birth weight in the infants. Congenital malformations are probably not increased in babies born to mothers with either treated or untreated hyperthyroidism. Inadequately treated maternal hyperthyroidism can cause suppression of the hypothalamic-pituitary-thyroid axis, thus resulting in temporary central hypothyroidism in the neonate and the inability of the neonate to mount an appropriate TSH response.
27. Describe the possible effects on the fetus of high levels of TSH receptor-stimulating antibodies and how they manifest in the fetus,
In about 2% to 5% of cases, fetal or neonatal hyperthyroidism can develop as a result of very high levels of maternal TSH receptor-stimulating antibodies (TSI or TRAB). Because transplacental passage of IgG is limited, this condition rarely occurs unless either the TSI (functional assay measuring cyclic adenosine monophosphate [cAMP]) or TRAB (TSH receptor antibodies by radioimmunoassay) are at least 2.5- to 3-fold elevated in the second and third trimesters. Fetal manifestations include goiter, tachycardia, advanced bone age, and growth restriction, or hydrops. All women with Graves’ disease or a history of Graves’ disease should be tested for TSI and TRAB. Numerous cases of fetal Graves’ disease have been reported in mothers previously treated with ablative doses of iodine-131 (131I) and who are taking thyroid replacement. Therefore, any woman with a history of Graves’ disease should have TSI and TRAB antibodies checked by 22 weeks of gestation. If either antibody is elevated at least 2- to 3-fold, an ultrasound examination should be performed at the time of the fetal anatomy scan at approximately 20 weeks to evaluate for evidence of fetal Graves’ disease and every 4 to 6 weeks or as clinically indicated for the remainder of pregnancy.
28. How are such effects treated?
Hyperthyroidism in the fetus should be confirmed by percutaneous umbilical sampling if the cause of the goiter is in doubt because high doses of maternal PTU can also cause a goiter and render the fetus hypothyroid. Fetal tachycardia is usually present but is not completely specific or sensitive, and growth restriction is usually a late sign of fetal Graves’ disease. Increased central vascularity of the gland may be helpful to suggest that the goiter is secondary to fetal Graves’ disease. Treatment consists of administering high doses of PTU to the mother so that a sufficient amount of medication is delivered into the fetal circulation. There is minimal experience using MMI for the treatment of fetal Graves’ disease, so PTU is usually recommended. Occasionally, mothers are already hypothyroid as a result of previous ablation or surgery or are rendered hypothyroid with these high PTU doses; in these situations, maternal supplementation with T4, which crosses the placenta less well than the PTU, may be required.
29. Why is neonatal hyperthyroidism more common than fetal hyperthyroidism?
Neonatal hyperthyroidism is more common than fetal hyperthyroidism because of the high activity of placental D3, the relatively low serum T3 levels in utero, and the effects of maternal antithyroid drugs on the fetus. TSH receptor-stimulating antibodies, passed transplacentally, remain at high levels after birth and stimulate the neonatal thyroid to produce excess thyroid hormone.
30. How does neonatal hyperthyroidism manifest?
Neonatal hyperthyroidism may manifest as irritability, failure to thrive, hyperkinesis, diarrhea, poor feeding, jaundice, tachycardia, poor weight gain, thrombocytopenia, goiter, and, less commonly, exophthalmos, cardiac failure, hepatosplenomegaly, hyperviscosity syndrome, or craniosynostosis. If the mother had been receiving antithyroid drugs during pregnancy, it may take 5 to 10 days for the neonate to manifest symptoms because of the residual effects of the medication.
31. What is the mortality rate of neonatal hyperthyroidism?
32. How should hyperthyroid infants be treated?
They may require antithyroid medications until the antibody levels wane, which usually occurs by 12 weeks.
33. How can pregnant women with Graves’ disease be safely treated in pregnancy?
Treatment of overt hyperthyroidism (elevated T4 levels) is definitely indicated to decrease morbidity in both mother and fetus. Thionamide therapy and the judicious use of beta-blockers until TT4 or FT4 levels are in the high-normal range or slightly above the normal range for pregnancy comprise the preferred treatment. Unless the patient has severe T3 thyrotoxicosis, the TT3 is usually not routinely monitored because TT3 normalization has been reported to cause hypothyroidism in the infant at birth. Cold iodine should be avoided and radioactive iodine is absolutely contraindicated because they readily cross the placenta and are concentrated by the fetal thyroid after 10 to 12 weeks of gestation. However, pregnant women with thyroid storm can be safely treated with cold iodine after PTU administration along with dexamethasone and judicious use of beta-blockers, similar to nonpregnant women.
34. Should subclinical hyperthyroidism be treated in pregnancy?
No. TSH remains suppressed normally in some pregnant women. In a series of more than 400 women with subclinical hyperthyroidism, pregnancy outcomes in untreated women were no different from those of women without suppressed TSH. Furthermore, such treatment risks the unnecessary exposure of the fetus to antithyroid drugs. Therefore, no matter the cause (Graves’ disease versus hCG mediated versus warm nodule), a suppressed TSH level alone without elevated thyroid hormones should not be treated in pregnancy.
35. Which is preferable in pregnant women, PTU or MMI?
PTU is clearly the preferred drug to treat hyperthyroidism in the first trimester because of the small but real risk of congenital malformations with MMI. MMI has been infrequently associated with a scalp deformity in the infant (aplasia cutis), choanal or esophageal atresia, or omphalocele, with a total malformation rate of 4.1% versus 1.9% in women taking PTU versus 2.1% in controls. Although PTU was thought initially to cross the placenta less well than MMI, this has been challenged; the risk of fetal hypothyroidism is much more directly related to whether the mother’s T4 levels are kept at the upper limit of the pregnancy range than to whether MMI or PTU was used. The Food and Drug Administration (FDA) reported acute fulminant hepatitis in 22 adults who were taking PTU, with 12 adult deaths. The investigators estimated the risk of PTU-related liver injury to be 1:1000 and a 1:10,000 risk for acute liver failure requiring transplant or death. There were 2 reported cases related to pregnancy, and both cases also had evidence of fetal liver injury. Because of this concern, the Endocrine Society and ATA recommendations are that women be switched from PTU to MMI in the second trimester if it can be done effectively and not compromise the optimal titration of antithyroid drugs. The usual conversion of PTU to MMI is about 15:1 (e.g., 150 mg PTU is approximately equal to 10 mg MMI), but maternal FT4 or TT4 levels need to be rechecked and carefully followed because women may respond differently to these antithyroid drugs. If a woman predominantly manifests T3 thyrotoxicosis, PTU may be superior to MMI because PTU also decreases the conversion of T4 to T3.
36. How are PTU and MMI dosed during pregnancy?
Because both PTU and MMI cross the placenta, the lowest possible doses should be given, with a goal of maintaining the mother’s serum FT4 in the high-normal range or the TT4 approximately 1.5 times the nonpregnancy range. The serum TSH level often remains persistently suppressed in women with FT4 and TT4 levels in these ranges and should never be used to titrate the dose of antithyroid drugs during pregnancy. Approximately 1% to 3% of newborns exposed to PTU in utero develop transient neonatal hypothyroidism or a small goiter. This is rare when PTU or MMI doses are titrated to maintain FT4 in the upper limits or slightly above the normal range for pregnancy, but it is more common if the FT4 levels fall into the middle or lower-normal range or if attempts are made to normalize the TSH. If PTU is switched to MMI later in pregnancy, the FT4 or TT4 levels should be rechecked in 2 to 4 weeks and then every 4 to 6 weeks throughout pregnancy to titrate the antithyroid drugs optimally. Although it is unknown whether monitoring liver function tests is beneficial in preventing severe hepatotoxicity, it is reasonable for women on PTU to have liver functions checked on a monthly or bimonthly basis and be advised to report any new symptoms immediately.
Fortunately, antithyroid drug doses can usually be markedly decreased by the second and especially the third trimester because of the decreasing TSI levels that accompany the natural immunosuppression of pregnancy. In fact, many women require minimal or no drug at term, especially if they have small goiters, but it is important to ensure that they are not hyperthyroid at delivery to reduce the risk of hyperthyroid complications to the cardiovascular system. Most women have a rebound in their hyperthyroidism postpartum, and, therefore, postpartum thionamide therapy must be increased.
37. Discuss the role of beta-blockers during pregnancy.
Beta-blockers are indicated to treat symptomatic hyperadrenergic signs and symptoms until antithyroid drug therapy has rendered the patient euthyroid. However, beta-blockers should be discontinued when the patient becomes euthyroid because long-term treatment with these drugs has been associated with intrauterine growth restriction. No compelling data indicate that one beta-blocker is safer than another; however, metoprolol and propranolol are usually favored over atenolol.
38. Why is radioactive iodine contraindicated in pregnancy?
Radioactive iodine is contraindicated in pregnancy because, after 12 to 14 weeks of gestation, the fetal thyroid gland has avidity for iodine that is 20 to 50 times that of the maternal thyroid. Accordingly, any dose of radioiodine will be more highly concentrated in fetal thyroid tissue and can easily ablate the fetal gland.
39. Can cold iodine be given during pregnancy?
Cold iodine (e.g., Lugol’s solution or saturated solution of potassium iodide [SSKI]) should also be avoided in pregnancy except in women with thyroid storm. If it must be given after 10 to 12 weeks, the fetus should be monitored for the development of a goiter, and the duration should be limited, if possible, to 3 days.
40. Does surgery have a role during pregnancy?
Surgery is rarely indicated during pregnancy but may be necessary in women who are unable to take antithyroid drugs (i.e., because of agranulocytosis) or who are refractory to high doses of antithyroid medications. If necessary, it is best to perform surgery in the second trimester before fetal viability. The rationale for this timing is the significant increase in the risk of miscarriage in the first trimester and of preterm labor when surgery is performed after 24 weeks.
41. Should a woman be counseled to terminate a pregnancy if she inadvertently receives a 123I scan or an ablative dose of 131I?
A woman who receives 123I for a thyroid scan early in pregnancy can be reassured for the most part because the fetus has not developed the ability to concentrate iodine before 10 weeks and the radiation exposure from this test is low, with a half-life of only approximately 8 hours. An ablative dose of 131I given early in pregnancy, however, is cause for greater concern because the half-life of 131I is 8 days, and the radiation is more destructive to the thyroid gland. Generally, if the dose is given very early, when the fetal thyroid gland is not yet trapping iodine, the relatively low thyroid and total body irradiation dose is probably not sufficient to justify termination of the pregnancy.
42. How may the risk to the fetus be minimized?
It may be useful in this situation to give PTU to block the recycling of 131I in the fetal thyroid gland if PTU can be given within 1 week of 131I treatment. If the fetus does develop hypothyroidism, it can be diagnosed in utero by percutaneous umbilical sampling, and T4 treatment may be given through amniotic fluid injections, although such treatment is still experimental. Certainly, all women of childbearing age, regardless of contraceptive measures, should have a pregnancy test before receiving any dose of 123I or 131I, and efficacious contraception should be ensured.
43. How should women with Graves’ disease be counseled about treatment alternatives before becoming pregnant?
Many experts recommend definitive treatment with 131I (after a negative pregnancy test) in a woman of childbearing age who wishes to become pregnant. In a series of nearly 300 women given radioiodine for thyroid cancer therapy, no significant differences in stillbirths, preterm births, low-birth-weight infants, or congenital malformations were reported in subsequent pregnancies. Effective birth control must be established, and then women should optimally wait for at least 6 months after regaining a stable euthyroid status before trying to conceive. Women with Graves’ disease who undergo ablation therapy with 131I may continue to have high (more than three times normal) TSI or TRAB antibodies for 1 year, and these increase the risk of fetal Graves’ disease. For women with very high TRAB antibodies who wish to become pregnant, surgery is a reasonable option. In women who are stable on low doses of thionamides, these drugs should not be problematic during pregnancy, but it is highly likely that thionamide doses will have be adjusted during pregnancy and the postpartum period. Women requiring high antithyroid drug doses or who have large goiters should be counseled about the benefits of definitive therapy before becoming pregnant.
44. Describe the natural history of Graves’ disease in the postpartum period.
Approximately 70% of women have a postpartum relapse of Graves’ disease, usually within the first 3 months after delivery, as the natural immunosuppression of pregnancy disappears. Antithyroid therapy must almost always be increased during this time.
45. What treatment options can be recommended for women who wish to breast-feed?
Because PTU is more highly protein bound and may cross less efficiently into breast milk than MMI, it was previously recommended that nursing mothers be treated with PTU rather than MMI. However, MMI doses up to 20 mg have been safely used in nursing mothers without any evidence of neonatal hypothyroidism. Therefore, because of the concerns about PTU-induced hepatotoxicity, women are usually counseled that they can safely nurse as long as these MMI doses are not exceeded. Nursing women requiring antithyroid drugs should tell their pediatrician, and thyroid function tests in the neonates may be indicated, especially if the woman is taking more than 300 mg of PTU or more than 20 mg of MMI per day.
46. Can a nursing mother undergo a diagnostic 123I scan if the cause of the hyperthyroidism is in question?
A diagnostic 123I scan can be performed if the woman is willing to interrupt breast-feeding for 2 to 3 days. Both 123I and technetium-99 (99Tc) pertechnetate are excreted into breast milk with an effective half-life of 5 to 8 and 2 to 8 hours, respectively.
47. Can ablative therapy with 131I be offered to nursing women?
Ablative therapy with 131I cannot be offered unless the women is willing to give up nursing altogether, because even a 5-mCi dose requires discontinuation of breast-feeding for at least 56 days. Further, it is recommended that 131I should not be given to women until at least 4 weeks after breast-feeding has ceased, to avoid high levels in breast tissue.
48. Can beta-blockers be used in nursing women?
Beta-blockers can be used if necessary in breast-feeding mothers. However, atenolol may produce higher breast milk concentrations than other beta-blockers, and there are rare reports of neonatal bradycardia in infants of mothers who nursed while taking this drug. The lowest doses of propranolol or metoprolol are preferred.
49. When should a nursing woman take antithyroid drugs?
It is always best if a mother takes antithyroid drugs immediately after nursing, to avoid exposing the infant to peak concentrations of the drug.
50. Does hypothyroidism pose a risk to the pregnant patient, and should all pregnant women be screened?
Hypothyroidism occurs in approximately 2% to 4% of pregnancies, and overt hypothyroidism occurs in approximately 0.5%. Because of maternal and fetal concerns, a case can be made to screen all pregnant women in the first trimester. It has been shown that targeted screening of only high-risk women fails to detect approximately 25% to 35% of women with elevated TSH values. However, there is a lack of consensus about whether all pregnant women should be screened or whether only women with risk factors should be tested (aggressive case finding). It has not been definitively demonstrated that screening all pregnant women and appropriately treating those with abnormal thyroid function decreases adverse pregnancy outcomes. A randomized controlled trial did not clearly show a benefit of screening and treating all women with a TSH level higher than 2.5 mU/L and elevated TPO antibodies. However, in a secondary analysis, the low-risk women in the screening group had a decrease in adverse outcomes compared with low-risk women in the case finding group, but only if all possible adverse outcomes were included as a composite outcome. Certainly, any pregnant woman with the following should be screened: risk factors for hypothyroidism, including a positive family history, use of amiodarone or lithium, a history of any type of thyroid disease, possible iodine deficiency, presence of a goiter, known thyroid antibodies, symptoms suggestive of thyroid disease; autoimmune disorders including type 1 diabetes mellitus; a history of head or neck irradiation; or a history of preterm delivery. Women more than 30 years old or with a body mass index (BMI) of at least 40 kg/m2 also have a higher risk than the normal population. Untreated hypothyroidism, especially when overt, can cause maternal anemia, myopathy, and congestive heart failure. It has also been associated with an increased risk of preterm delivery, pregnancy loss, gestational hypertension, placental abruption, low-birth-weight infants, postpartum hemorrhage, and the possibility of neurodevelopmental delay in the infant. The ATA stated that there are insufficient data for or against screening, and the American College of Obstetrics and Gynecology (ACOG) stated that there are insufficient data to recommend screening. The Endocrine Society stated that their committee was divided in its recommendation; approximately half the members recommended screening, and half stated that there was insufficient evidence for or against screening.
51. Should pregnant women with recurrent pregnancy loss be screened for TPO antibodies, and, if they are found, should thyroid hormone be offered despite a normal TSH?
There are both positive and negative studies suggesting that TPO antibodies may be related to pregnancy loss despite a euthyroid state, but, on balance, there appears to be a positive association. It is not clear whether these women have decreased thyroid reserve as a possible cause because women with positive TPO antibodies are more likely to develop subclinical hypothyroidism later in gestation. It is also unknown whether these antibodies could directly cause miscarriage or are simply markers of other autoimmune diseases that could be associated with pregnancy loss. Evidence indicates that these antibodies may affect trophoblast function. A single randomized controlled trial suggested that treating unselected euthyroid women who were TPO antibody positive with low doses of thyroid hormone could decrease first trimester loss but not loss later in pregnancy. However, many of the losses occurred so early that initiating treatment before the loss would not have been possible, and it is difficult to understand on a mechanistic basis how only several days of treatment could prevent pregnancy loss. This study also demonstrated that delivery at less than 37 weeks of gestation was decreased in the treated group, but gestational ages of the groups were not reported. Therefore, until further studies support or refute this study, it is not recommended that women be checked for TPO antibodies unless thyroid disease is suspected. Women who are TPO antibody positive clearly have approximately a 15% risk of developing subclinical hypothyroidism later in pregnancy and a 50% chance of postpartum thyroiditis; they should be monitored closely for these developments.
52. How do thyroid hormone requirements change during pregnancy?
Thyroid hormone requirements in treated hypothyroid patients often increase during pregnancy, with up to 75% of pregnant women requiring an increase in thyroxine dosage of 25% to 50%. One study confirmed that 85% of pregnant women required an increase in levothyroxine of 47% by 16 weeks of gestation, although most of these women were athyreotic. Because requirements increased as early as 5 weeks of gestation, women who are athyreotic may need to increase their thyroid hormone dosage by 20% to 25% as soon as pregnancy is confirmed.
53. What causes the rapid increase in thyroid hormone requirements in early pregnancy?
The rapid increase in thyroid hormone requirements that occurs in the first trimester may result from the sudden increase in the estrogen-stimulated TBG pool associated with pregnancy. This change can be especially striking in women undergoing assisted reproduction, during which hormonal therapy may stimulate very high estrogen levels.
54. When should the TSH be checked in pregnancy, what doses of thyroid hormone should be prescribed, and at what level of TSH should therapy be directed?
The serum TSH level should be checked as soon as pregnancy is confirmed, and an appropriate increase in levothyroxine dose should be made. One study suggested that athyreotic women requiring full replacement doses should receive a 25% dose increase as soon as pregnancy is confirmed despite a normal TSH. Another trial supported that this can be done by adding 2 tablets of levothyroxine per week to the patient’s regimen. As discussed earlier, the TSH may be mildly suppressed in normal women during the first trimester as a result of the thyrotropic influence of hCG. Therefore, unless a woman is symptomatically hyperthyroid or has frankly elevated serum FT4 levels, the levothyroxine dosage should not be reduced in response to the finding of a low first-trimester TSH level.
Both the Endocrine Society and the ATA support that pregnant women with subclinical hypothyroidism (TSH > 2.5 or 3.0 mU/L but < 10 mU/L; FT4 within the normal range) should be treated if they have positive TPO antibodies. The Endocrine Society also supports treatment in such women without TPO antibodies if the TSH is repeated and found to be greater than 2.5 mU/L in the first trimester or greater than 3.0 mU/L in the second or third trimesters. These women can usually be adequately treated with 50 μg of levothyroxine. The ACOG does not clearly recommend that subclinical hypothyroidism be routinely treated in pregnancy.
Pregnant women with overt hypothyroidism (elevated TSH; FT4 below the normal range) should be given full levothyroxine replacement doses immediately; this can be estimated at 2 μg/kg in pregnancy. The TSH should be checked 4 weeks after a dose change and every 4 weeks throughout midgestation to maintain TSH levels up to 2.5 mU/L while the fetus is dependent on maternal thyroid hormone. TSH can then be followed every 4 to 8 weeks for the remainder of pregnancy to maintain serum TSH levels up to 3.0 mU/L in the second and third trimesters. In women who have had a thyroidectomy for thyroid cancer, the goal of maintaining a suppressed but detectable serum TSH without rendering them thyrotoxic should be adhered to during pregnancy. The thyroid hormone dose should be reduced almost immediately after delivery to avoid hyperthyroidism postpartum, and the TSH should be checked at 6 weeks postpartum. Pre-pregnancy doses may be instituted as soon as the woman has lost the majority of her pregnancy weight gain.
55. When should a pregnant woman take her thyroid hormone?
It is extremely important to advise the pregnant woman to take her thyroid hormone and her prenatal vitamins or iron supplements at different times, because ferrous sulfate can bind to thyroxine and decrease its bioavailability. High doses of calcium and soy can also interfere with thyroid hormone absorption.
56. What is the risk of abnormal fetal and neonatal intellectual development in infants born to mothers who are hypothyroid during the first trimester of pregnancy?
All newborns in the United States are screened for hypothyroidism because it is well established that infants who have severe congenital hypothyroidism but who then receive thyroid hormone therapy at birth appear to have fairly normal intellectual growth and development. Overt hypothyroidism is defined as decreased serum FT4 or TT4 levels (in the context of pregnancy norms) in association with an increased serum TSH. In pregnancy, a TSH level higher than 10 mU/L is also usually treated as overt hypothyroidism regardless of FT4 or TT4 levels. Although overt hypothyroidism is known to have serious effects on the fetus, the fetal effects of maternal subclinical hypothyroidism (TSH > 2.5 mU/L in the first trimester or > 3.0 mU/L in the second and third trimesters, but FT4 within the normal range) is a subject of ongoing debate. Several publications suggested that psychomotor and intellectual development may be impaired in infants born to mothers who were subclinically hypothyroid during the first trimester of pregnancy, although the differences from control subjects in these studies were small and often became insignificant when the infants were tested later in childhood. Some retrospective studies suggested that infants born to mothers with subclinical hypothyroidism have slightly decreased neurodevelopmental testing results. However, in the ongoing CATS (Controlled Antenatal Thyroid Screening) study, the overall outcomes on IQ testing at 3 years of age between universally screened and unscreened pregnancies were not significantly different when treatment was initiated at 12 weeks in the screened group. A multicenter placebo-controlled randomized controlled trial to evaluate the effects of levothyroxine treatment on subclinical hypothyroidism is being conducted by the Maternal Fetal Medicine Unit of the National Institutes of Health (NIH). The primary outcome will be child IQ at 5 years of age, and it is anticipated that the results of this study will be available in 2015.
57. What strategies can reduce the risk to the fetus?
It seems prudent to attempt to identify and appropriately treat hypothyroidism in women of childbearing age who wish to become pregnant (preconception), as well as in pregnant women in the first trimester. However, serum TSH levels in normal women often decline in the first trimester as a result of the influence of hCG. Thus, a TSH level greater than 2.5 mU/L in the first trimester may be inappropriately high, especially when accompanied by TPO antibodies, whereas a TSH level of 0.1 mU/L may be appropriately low because of the thyroid-stimulating activity of high hCG levels.
58. How should a thyroid nodule be evaluated during pregnancy?
The evaluation of a solitary or dominant thyroid nodule in a pregnant woman is similar to that in nonpregnant women. Ultrasound is indicated to evaluate for multiple nodules and for ultrasonographic features suggestive of malignancy (microcalcifications, hypoechoic patterns, irregular margins, nodules that are taller than they are wide, or intranodular vascularity). If the woman has a high or normal serum TSH, fine-needle aspiration (FNA) should be offered for predominantly solid thyroid nodules larger than 1 cm. FNA should also be recommended in women with nodules 5 mm to 1 cm if these women have a high-risk family history (multiple endocrine neoplasia type 2 [MEN 2], familial papillary thyroid carcinoma, familial polyposis, familial medullary carcinoma), a high-risk personal history (rapid onset or growth of nodule, history of head and neck irradiation during childhood, hoarseness, persistent cough), or ultrasound features suggestive of malignancy. Women with complex nodules 1.5 to 2 cm or larger should also receive an ultrasound-guided FNA. Women who have nodules discovered in the last month of pregnancy could reasonably have FNA delayed until after delivery, but it is usually helpful to make the diagnosis of thyroid cancer during pregnancy so that appropriate planning of surgical treatment can be made. Women found to have a thyroid nodule and a suppressed TSH may have a warm or hot nodule. Warm or hot nodules are rarely malignant but are often nondiagnostic on FNA. For that reason, a pregnant woman with a suppressed TSH and a nodule should undergo a radioisotope scan postpartum to determine whether the nodule is warm or cold before obtaining an FNA. FNA specimens should be evaluated with the same criteria as used for nonpregnant patients.
59. What is the likelihood that thyroid nodules discovered during pregnancy are malignant?
Data suggest that thyroid nodules discovered during pregnancy may have a higher risk of being malignant. However, this finding is likely partly the result of selection or sampling bias, because many young women do not have systematic health examinations until they become pregnant. Depending on the patient population, the incidence of biopsied benign nodules is greater than 80%, whereas differentiated thyroid cancer has been found in 5% to 40% of biopsies. Most malignant nodules are papillary thyroid carcinoma. FNA cytology is highly accurate in diagnosing papillary carcinoma, whereas cytology showing follicular or Hürthle cell neoplasms predicts only a 5% to 15% risk of malignancy. When the serum TSH is normal, fewer than 20% of FNA specimens are nondiagnostic.
60. How should a thyroid nodule be managed during pregnancy?
If the cytology suggests or confirms papillary thyroid cancer, the best time to offer a thyroidectomy is in the second trimester, to avoid the risk of miscarriage in the first trimester and preterm labor in the third trimester. The risk of preterm labor or adverse fetal outcomes related to surgery performed in the second trimester is exceedingly rare. If the nodule is less than 2 cm and has not rapidly increased in size, and the patient has no lymphadenopathy, it may be reasonable to postpone thyroidectomy until after pregnancy and administer thyroid suppression therapy in the meantime, with careful attention to avoiding elevated T4 levels. It is appropriate to administer thyroid hormone to achieve a suppressed but detectable TSH level in pregnant women with a recent history of thyroid cancer, thyroid cancer diagnosed in pregnancy, or a highly suspicious thyroid nodule as long as the FT4 or TT4 levels are not increased above the normal range for pregnancy. Disease-specific survival has not been shown to be affected by whether thyroidectomy for a malignant nodule is performed during pregnancy or immediately postpartum as long as the nodule shows well-differentiated thyroid cancer. However, some evidence suggests that recurrence, based on serum TG levels or rising thyroid antibody titers, may be slightly higher in women who wait to have surgery postpartum compared with women who elect to have surgery performed in the second trimester.
61. How common is postpartum thyroiditis? Who is at risk?
Postpartum thyroid dysfunction occurs in approximately 5% to 10% of women, with a much higher incidence in certain populations. In one series, 25% of women with type 1 diabetes mellitus developed postpartum thyroid dysfunction; it is therefore recommended that this population be routinely screened in the postpartum period. In another series of 152 women with TPO antibodies detected at 16 weeks of gestation, postpartum thyroiditis occurred in 50%; of these, 19% had hyperthyroidism alone, 49% had hypothyroidism alone, and the other 32% had hyperthyroidism followed by hypothyroidism. Women with a family history of thyroid disease are also at increased risk and may be candidates for screening with TPO antibodies during pregnancy or with thyroid function tests in the postpartum period. Women known to be TPO antibody positive should have a TSH test performed at 6 to 12 weeks and at 6 months postpartum or as clinically indicated.
62. Characterize the histopathology of postpartum thyroiditis.
The disorder is highly associated with circulating TPO antibodies, and the histology is identical to that of Hashimoto’s thyroiditis with diffuse mononuclear cell infiltration and destruction of thyroid follicles.
63. Summarize the clinical course of postpartum thyroiditis.
64. Describe phase 1 of postpartum thyroiditis.
At 1 to 3 months after delivery, affected women develop hyperthyroidism secondary to immunologically mediated destruction of thyroid follicles, resulting in the release of stored thyroid hormone into the circulation. Such women may experience anxiety, irritability, palpitations, fatigue, and insomnia, but commonly this phase does not come to clinical attention. Symptomatic patients are best treated with low-dose beta-blockers, which must soon be tapered and discontinued as the thyrotoxic phase spontaneously resolves. Use of PTU or MMI is not indicated because the hyperthyroidism in these patients is caused by destruction of their gland and not by increased thyroid hormone synthesis.
65. How can phase 1 of postpartum thyroiditis be distinguished from Graves’ disease?
Occasionally, there is a question about the cause of the hyperthyroidism, because Graves’ disease commonly appears or exacerbates in the first several months postpartum. Distinguishing between the two conditions is facilitated by measurement of a serum thyroglobulin level and TPO antibodies (both are high in postpartum thyroiditis) and TSH receptor-stimulating antibodies (often elevated with Graves’ disease). However, the most definitive test is a 123I-uptake test (low in postpartum thyroiditis and high in Graves’ disease), if the mother is willing to interrupt nursing for 2 to 3 days.
66. Describe phase 2 of postpartum thyroiditis.
More commonly, women present with stage 2 of postpartum thyroiditis, which is characterized by hypothyroidism alone or following transient hyperthyroidism (phase 1), at about 4 to 8 months after delivery. Nonspecific symptoms include fatigue, depression, impaired concentration, poor memory, aches and pains, dry skin, and weight gain, all of which may be overlooked by the clinician. Symptoms may predate the onset of thyroid function abnormalities in women with positive TPO antibodies and may persist for some time after a euthyroid state is achieved.
67. How is phase 2 of postpartum thyroiditis treated?
Women with abnormal thyroid function tests and symptoms consistent with hypothyroidism should be treated with levothyroxine replacement for approximately 6 to 12 months or at least until 1 year after delivery. At that time, discontinuation of levothyroxine therapy can be attempted to identify the 70% to 80% of women who will return to the euthyroid state by 12 months after delivery.
68. Describe the natural history of postpartum thyroiditis.
Most women return to a euthyroid state at 12 to 18 months postpartum. However, thyroid function tests should then be followed at least annually in women who become euthyroid. In a series of 43 patients with postpartum thyroiditis, 23% of the women were hypothyroid at 2 to 4 years, and, in a longer series, approximately 50% of women were hypothyroid 7 to 9 years later. Women with the highest TPO antibody titers and the most severe hypothyroidism appear to be at the highest risk of developing permanent hypothyroidism. If a woman becomes euthyroid within a year postpartum, she has a high likelihood (70%) of developing postpartum thyroiditis after a subsequent pregnancy.
, ACOG Committee Opinion. Subclinical hypothyroidism in pregnancy. Obstet Gynecol 2007;110:959–960.
Alexander, EK, Marqusee, E, Lawrence, E, et al. Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism. N Engl J Med. 2004;351:241–249.
Cooper, DS, GM, et al, American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–1214.
Stagnaro-Green, A, Abalovich, A, et al, American Thyroid Association Taskforce on Thyroid Disease During Pregnancy and Postpartum. Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and Postpartum. Thyroid 2011;21:1081–1125.
Anckaert, E, Poppe, K, Van Uytfanghe, K. FT4 immunoassays may display a pattern during pregnancy similar to the equilibrium dialysis ID-LC/tandem MS candidate reference measurement procedure in spite of susceptibility towards binding protein alterations. Clin Chim Acta. 2010;411:1348–1353.
Azizi, F, Khoshniat, M, Bahrainian, M, Hedayati, M. Thyroid function and intellectual development of infants nursed by mothers taking methimazole. J Clin Endocrinol Metab. 2000;85:3233–3238.
Casey, BM, Dashe, JS, Wells, CE, et al. Subclinical hyperthyroidism and pregnancy outcomes. Obstet Gynecol. 2006;107:337–341.
Cleary-Goldman, J, Malone, FD, Lambert-Messerlian, G, et al. Maternal thyroid hypofunction and pregnancy outcome. Obstet Gynecol. 2008;112:85–92.
Cooper, DS, Rivkees, SA. Putting propylthiouracil in perspective. J Clin Endocrinol Metab. 2009;94:1881–1882.
De Groot, L, Abalovich, M, Alexander, E, et al, Management of thyroid dysfunction during pregnancy and postpartum. an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2012;97:2543–2565.
Garsi, JP, Schlumberger, M, Rubino, C, et al, Therapeutic administration of 131I for differentiated thyroid cancer. radiation dose to ovaries and outcome of pregnancies. J Nucl Med 2008;49:845–852.
Glinoer, D, Rihai, M, Grun, JP. Risk of subclinical hypothyroidism in pregnant women with asymptomatic autoimmune thyroid disorders. J Clin Endocrinol Metab. 1994;79:197–204.
Goodwin, TM, Hershman, JM. Hyperthyroidism due to inappropriate production of human chorionic gonadotropin. Clin Obstet Gynecol. 1997;40:32–44.
Haddow, JE, Cleary-Goldman, J, McClain, MR, (FaSTER) Research Consortium. Thyroperoxidase and thyroglobulin antibodies in early pregnancy and preterm delivery. Obstet Gynecol 2010;116:58–62.
Huel, C, Guibourdenche, J, Vuillard, E, et al. Use of ultrasound to distinguish between fetal hyperthyroidism and hypothyroidism on discovery of a goiter. Ultrasound Obstet Gynecol. 2009;33:412–420.
Kahric-Janic, N, Soldin, SJ, Soldin, OP, et al. Tandem mass spectrometry improves the accuracy of free thyroxine measurements during pregnancy. Thyroid. 2007;17:303–311.
Kempers, MJE, Van Tijn, DA, Van Trotensburg, ASP, et al, Central congenital hypothyroidism due to gestational hyperthyroidism. detection where prevention failed. Clin Endocrinol Metab 2003;88:5851–5857.
Lazarus, JH, Bestwick, JP, Channon, S, et al. Antenatal thyroid screening and childhood cognitive function. N Engl J Med. 2012;366:493–501.
Lockwood, CM, Grenache, DG, Gronowski, AM. Serum human chorionic gonadotropin concentrations greater than 400,000 IU/L are invariably associated with suppressed serum thyrotropin concentrations. Thyroid. 2009;19:863–868.
Luton, D, Le Gac, I, Vuillard, E, et al, Management of Grave’s disease during pregnancy. the key role of fetal thyroid gland monitoring. J Clin Endocrinol Metab 2005;90:6093–6098.
Momotani, N, Yamashita, R, Makino, F, et al. Thyroid function in wholly breast-feeding infants whose mothers take high doses of propylthiouracil. Clin Endocrinol. 2000;53:177–181.
Moosa, M, Mazzaferri, EL. Outcome of differentiated thyroid cancer diagnosed in pregnant women. J Clin Endocrinol Metab. 1997;82:2862–2866.
Nachum, Z, Rakover, Y, Weiner, E, et al, Grave’s disease in pregnancy. prospective evaluation of a selective invasive treatment protocol. Am J Obstet Gynecol 2003;189:159–165.
Negro, R, Formoso, G, Mangieri, T, et al, Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease. effects on obstetrical complications. J Clin Endocrinol Metab 2006;91:2587–2591.
Negro, R, Schwartz, A, Gismondi, R, et al. Increased pregnancy loss rate in thyroid antibody negative women with TSH levels between 2.5 and 5.0 in the first trimester of pregnancy. J Clin Endocrinol Metab. 2010;95:E44–E448.
Negro, R, Schwartz, A, Gismondi, R, et al. Universal screening versus case finding for detection and treatment of thyroid hormonal dysfunction during pregnancy. J Clin Endocrinol Metab. 2010;95:1699–1707.
Panesar, NS, Li, CY, Rogers, MS. Reference intervals for thyroid hormones in pregnant Chinese women. Ann Clin Biochem. 2001;38:329–332.
Patel, J, Landers, K, Huika, L, et al. Delivery of maternal thyroid hormones to the fetus. Trends Endocrinol Metab. 2011;22:164–170.
Pelag, D, Cada, S, Peleg, A, et al. The relationship between maternal serum thyroid-stimulating immunoglobulin and fetal and neonatal thyrotoxicosis. Obstet Gynecol. 2002;99:1040–1043.
Pop, V, Brouwers, EP, Vader, HL, et al, Maternal hypothyroxinaemia during early pregnancy and subsequent child development. a 3-year follow-up study. Clin Endocrinol (Oxf) 2003;59:282–288.
Rushworth, FH, Backos, M, Rai, R, et al. Prospective pregnancy outcome in untreated recurrent miscarriers with thyroid autoantibodies. Hum Reprod. 2000;15:1637–1639.
Sam, S, Molitch, ME. Timing and special concerns regarding endocrine surgery during pregnancy. Endocrinol Metab Clin North Am. 2003;32:337–354.
Sapin, R, D’Herbomez, M, Schlienger, JL. Free thyroxine measured with equilibrium dialysis and nine immunoassays decreased in late pregnancy. Clin Lab. 2004;50:581–584.
Soldin, OP, Tractenberg, RE, Hollowell, JG, et al, Trimester-specific changes in maternal thyroid hormone, thyrotropin, and thyroglobulin concentrations. trends and associations across trimester in iodine sufficiency. Thyroid 2004;14:1084–1090.
Vaidya, B, Anthony, S, Bilous, M, Detection of thyroid dysfunction in early pregnancy. universal screening or target high-risk case finding. J Clin Endocrinol Metab 2007;92:203–207.
Vannucchi, G, Perrino, N, Rossi, S, et al. Clinical and molecular features of differentiated thyroid cancer diagnosed during pregnancy. Eur J Endocrinol. 2010;162:145–151.
Vulsma, T, Gons, MH, de Vijlder, JJ. Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. N Engl J Med. 1989;321:13–16.
Walker, JA, Illions, EH, Huddleston, JF, et al. Racial comparisons of thyroid function and autoimmunity during pregnancy and the postpartum period. Obstet Gynecol. 2005;106:1365–1371.
Yassa, L, Marqusee, E, Fawcett, R, et al. Thyroid Hormone Early Adjustment in Pregnancy (the THERAPY) trial. J Clin Endocrinol Metab. 2010;95:3234–3241.
Yoshihara, A, Noh, J, Yamaguchi, T, et al, Exposure to methimazole during the first trimester of pregnancy increases the risk of congenital anomalies. (Epub ahead of print). J Clin Endocrinol Metab 2012.