Chapter 55 Thrombocytopenia and Platelets
1 What are two principal functions of platelets in effecting hemostasis?
5 How prevalent is thrombocytopenia in critically ill patients, and what are the most common causes of thrombocytopenia in the intensive care unit (ICU)?
9 How is HIT diagnosed?
 The functional assays measure heparin-dependent platelet activation by PF4-heparin antibody in vitro. One of the functional assays, 14C-serotonin release assay (SRA), is considered the gold standard in diagnosis with a positive predictive value of almost 100% (but a negative predictive value of approximately 20%).
The functional assays measure heparin-dependent platelet activation by PF4-heparin antibody in vitro. One of the functional assays, 14C-serotonin release assay (SRA), is considered the gold standard in diagnosis with a positive predictive value of almost 100% (but a negative predictive value of approximately 20%).
 Immunoassays (such as enzyme-linked immunosorbent assay [ELISA]) measure the levels of antibodies in circulation (sensitivity 93%-97%, positive predictive value 93%-100%, specificity 86%-100%, and negative predictive value 88%-95%). ELISA is easy and rapid to obtain, but only 25% of the ELISA-positive specimens are SRA positive.
Immunoassays (such as enzyme-linked immunosorbent assay [ELISA]) measure the levels of antibodies in circulation (sensitivity 93%-97%, positive predictive value 93%-100%, specificity 86%-100%, and negative predictive value 88%-95%). ELISA is easy and rapid to obtain, but only 25% of the ELISA-positive specimens are SRA positive.
11 How is HIT treated?
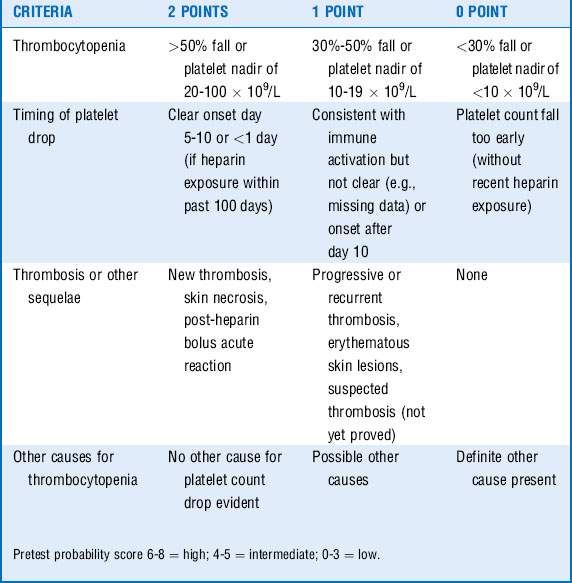
Diagnosis of HIT requires immediate withdrawal of all heparin and treatment with anticoagulation agents. The Warkentin criteria may be used to determine the patient’s pretest probability of HIT (Table 55-1). All patients (with or without thrombosis) with HIT must be anticoagulated, as the risk of thrombosis is >50% without anticoagulation. Do not transfuse platelets unless clearly indicated, as platelet transfusion actually increases the amount of PF4 and may exaggerate the antigen response. If continued anticoagulation is required, a vitamin K antagonist (warfarin) should be initiated after the patient is fully treated with one of the following agents:
 Danaparoid (low-molecular-weight glycosaminoglycan composed of heparan sulfate, dermatan sulfate, and chondroitin sulfate). This drug has mostly anti-factor Xa activity with a limited antithrombin action. Dose is titrated to keep anti-Xa levels between 0.5 and 0.8 units/mL. There is no antidote for bleeding.
Danaparoid (low-molecular-weight glycosaminoglycan composed of heparan sulfate, dermatan sulfate, and chondroitin sulfate). This drug has mostly anti-factor Xa activity with a limited antithrombin action. Dose is titrated to keep anti-Xa levels between 0.5 and 0.8 units/mL. There is no antidote for bleeding.
 Recombinant hirudin (lepirudin [Refludan]) is a 7-kDa peptide that acts directly on circulating and clot-bound thrombin. Anticoagulant effects last about 40 minutes. It is given as a slow bolus (0.4 mg/kg) followed by continuous infusion at 0.15 mg/kg to maintain activated partial thromboplastin time (aPTT) between 1.5 and 2.5 times baseline. This is a good choice for patients who will need to get transitioned to warfarin. Lepirudin does not alter the interpretation of international normalized ratio (INR) as significantly as argatroban.
Recombinant hirudin (lepirudin [Refludan]) is a 7-kDa peptide that acts directly on circulating and clot-bound thrombin. Anticoagulant effects last about 40 minutes. It is given as a slow bolus (0.4 mg/kg) followed by continuous infusion at 0.15 mg/kg to maintain activated partial thromboplastin time (aPTT) between 1.5 and 2.5 times baseline. This is a good choice for patients who will need to get transitioned to warfarin. Lepirudin does not alter the interpretation of international normalized ratio (INR) as significantly as argatroban.
 Argatroban is a 509-Da arginine-based direct thrombin inhibitor that inhibits both soluble and clot-bound thrombin. Half-life is 46.2 ± 10.2 minutes, and steady-state activity is achieved within 1 to 2 hours of continuous infusion. Dose is 2.0 mcg/kg per minute and adjusted to keep aPTT between 1.5 and 3 times baseline (maximum 10 mcg/kg per minute).
Argatroban is a 509-Da arginine-based direct thrombin inhibitor that inhibits both soluble and clot-bound thrombin. Half-life is 46.2 ± 10.2 minutes, and steady-state activity is achieved within 1 to 2 hours of continuous infusion. Dose is 2.0 mcg/kg per minute and adjusted to keep aPTT between 1.5 and 3 times baseline (maximum 10 mcg/kg per minute).
 Fondaparinux is a newer drug that is given via the subcutaneous route. Dose is 7.5 mg once a day.
Fondaparinux is a newer drug that is given via the subcutaneous route. Dose is 7.5 mg once a day.
14 How do you differentiate between thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS)?
16 What are the indications for platelet transfusion?
 Bleeding prophylaxis in a stable oncology patient: 10,000/mm3 (previously <20,000/mm3)
Bleeding prophylaxis in a stable oncology patient: 10,000/mm3 (previously <20,000/mm3)
 Lumbar puncture in a patient with leukemia: 10,000/mm3
Lumbar puncture in a patient with leukemia: 10,000/mm3
 Bone marrow aspiration: 20,000/mm3
Bone marrow aspiration: 20,000/mm3
 Gastrointestinal endoscopy in cancer: 20,000-40,000/mm3
Gastrointestinal endoscopy in cancer: 20,000-40,000/mm3
 Fiberoptic bronchoscopy: 20,000 to 50,000/mm3
Fiberoptic bronchoscopy: 20,000 to 50,000/mm3
 Thrombocytopenia resulting from massive transfusion: 50,000/mm3
Thrombocytopenia resulting from massive transfusion: 50,000/mm3
 Invasive procedures in cirrhosis: 50,000/mm3
Invasive procedures in cirrhosis: 50,000/mm3
 Cardiopulmonary bypass: 50,000 to 60,000/mm3
Cardiopulmonary bypass: 50,000 to 60,000/mm3
 Neurosurgical procedures: 100,000/mm3
Neurosurgical procedures: 100,000/mm3
 Thrombocytopenia and bleeding (intracerebral, gastrointestinal, genitourinary, or retinal hemorrhage): 100,000/mm3
Thrombocytopenia and bleeding (intracerebral, gastrointestinal, genitourinary, or retinal hemorrhage): 100,000/mm3
18 What laboratory test measures platelet function?
Bleeding time is a sensitive indicator of overall platelet function.
19 How are platelet disorders managed?
Key Points Thrombocytopenia and Platelets
1. Thrombocytopenia is a common finding in intensive care unit patients, and the basic rule for management is to treat the underlying cause.
2. Transfuse platelets only if needed (question 16) or if the platelet count is less than 10,000/mm3.
3. HIT is a relatively uncommon but potentially serious complication of heparin administration.
4. Platelet counts should be followed in all patients that are receiving heparin (unfractionated or low molecular weight). A drop in platelet count (>50% from baseline or below 100,000/mm3) is a reason to suspect HIT.
5. Most of the patients who have circulating antibodies to PF4 do not have clinical development of HIT. Therefore screen patients for these antibodies only when clinically indicated.
6. All patients (with or without thrombosis) with HIT (type II) must be anticoagulated, as the risk of thrombosis is >50% without anticoagulation.
1 AuBuchon J.P. Platelet transfusion therapy. Clin Lab Med. 1996;16:797–816.
2 Chong B.H., Eisbacher M. Pathophysiology and laboratory testing of heparin-induced thrombocytopenia. Semin Hematol. 1998;35:3–8.
3 Fuse I. Disorders of platelet function. Crit Rev Oncol Hematol. 1996;22:1–25.
4 Lipsett P.A., Perler B.A. The use of blood products for surgical bleeding. Semin Vasc Surg. 1996;9:347–353.
5 Martel N., Lee J., Wells P.S. Risk for heparin-induced thrombocytopenia with unfractionated and low molecular weight heparin thromboprophylaxis: a meta-analysis. Blood. 2005;106:2710–2715.
6 McCrae K.R., Bussel J.B., Mannucci P.M., et al. Platelets: an update on diagnosis and management of thrombocytopenic disorders. Hematology Am Soc Hematol Educ Program. 2001;2001:282–305.
7 Platelet transfusion therapy. Natl Inst Health Consens Dev Conf Consens Statement. 1986;6:1–6.
8 Priziola J.L., Smythe M.A., Dager W.E. Drug induced thrombocytopenia in critically ill patients. Crit Care Med. 2010;38(6 Suppl):S145–S152.
9 PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group, et al: Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2011;364:1305–1314.
10 Rebulla P. Platelet transfusion trigger in difficult patients. Transfus Clin Biol. 2001;8:249–254.
11 Selleng K., Warkentin T.E., Greinacher A. Heparin induced thrombocytopenia in intensive care patients. Crit Care Med. 2007;35:1165–1176.