Chapter 41 Threaded Cylindrical Interbody Cage Fixation for Cervical Spondylosis and Ossification of the Posterior Longitudinal Ligament
With advances in neuroimaging using CT and MRI, the diagnosis of cervical disc herniation, spondylosis, and ossification of the posterior longitudinal ligament (OPLL) has become more precise and less invasive in recent years.1 In addition, routine microsurgery with refined drills and implants such as interbody cages has facilitated less invasive and more efficient ventral cervical spine procedures.2,3
Preoperative Workups and Surgical Considerations
The first factor is the frequent association of cervical spondylosis and disc herniation with OPLL and hypertrophy of the posterior longitudinal ligaments,4 causing myelopathy rather than radiculopathy.5–7 Radiologically, OPLL of the cervical spine has been classified into four types: (1) the local, bridge, or circumscribed type, which is located behind the disc space; (2) the segmental type, which usually is limited to the posterior aspect of one or two vertebral levels; (3) the continuous type, which usually extends continuously over several vertebral bodies; and (4) the mixed type, which is a combination of the continuous and segmental types.1
In epidemiologic studies, OPLL of the cervical spine is found in 3.2% of those age 50 years and older in Japan and is relatively common in south Asian countries. It is also found not infrequently in New York, Utah, and Hawaii in the United States and in some European countries. Therefore, understanding of this condition (OPLL) is important in determining surgical strategies to treat patients with cervical discogenic disease.8
The second factor resulting in the need for a different surgical approach in Japan is unique: allografts are not available in Japan. Therefore, autografts or other alternatives have to be used for anterior cervical fusion.9,10
Deciding which surgical strategy—ventral versus dorsal approach—to use can be determined based on the number of spinal levels involved, the extent of OPLL, the presence of canal stenosis, and the alignment of the cervical spine, but more often depends on the surgeon’s experience and philosophy. Generally speaking, the ventral approach is applied to single-level or two-level lesions and the dorsal approach is usually applied to three-level or four-level lesions.3,5,11,12 The surgical techniques of expansive laminoplasty have been well described.13–15
Evolution of Surgical Techniques
Corpectomy with Iliac Bone Graft
From 1980 to 1991, multilevel corpectomy with iliac crest interbody graft was carried out for multilevel OPLL and spondylosis, but graft problems, donor site discomfort, and the necessity of postoperative application of a halo brace were drawbacks of this method. Development of ventral plate fixation dramatically reduced the usage of halo brace application.5,7,11,16
Corpectomy with Vertebral Graft
From 1992 to 1997, limited or keyhole corpectomy with vertebral graft using a Williams microsurgical saw (Ace Medical Co., Los Angeles) was carried out with reasonable results in 60 patients with cervical spondylosis with segmental OPLL. One of the pitfalls of this method is that bone grafts taken from the cervical spine are often more fragile than iliac grafts, especially in heavy smokers and elderly women with osteoporosis.17–19
Microdiscectomy without Grafting
Microdiscectomy for central and paramedian discs and spurs without grafting has been done with reasonable results, but the small opening is often not adequate to decompress lateral spurs or OPLL.20–22 Ventral transuncal foraminotomy was also added to lateral or foraminal discs and spurs with satisfactory results.23,24
Threaded Cylindrical Interbody Cage Fixation
Threaded cylindrical titanium cages were first introduced for posterior lumbar interbody fusion (PLIF) of lumbar spine instability in the early 1990s.25 In 1997, the cylindrical Bagby and Kuslich cervical interbody cage (BAK/C; Spine-Tech, Minneapolis, MN) became available in Japan for ventral cervical fusion.26 However, these instruments were made for macrosurgery and were too large and difficult to use under the operating microscope. Therefore, we developed smaller and more slender instruments, so that the entire procedure of decompression and cage fixation could be done under microsurgical control as a less invasive procedure (M-cage, Ammtec Inc., Tokyo).2,3,27
Modified Keyhole Microsurgical Approach
By using the advantages of keyhole discectomy and limited corpectomy and at the same time avoiding the pitfalls of the aforementioned procedures, a modified keyhole microsurgical technique with interbody cage fixation for cervical spondylosis and OPLL was developed.3,28
Surgical Technique
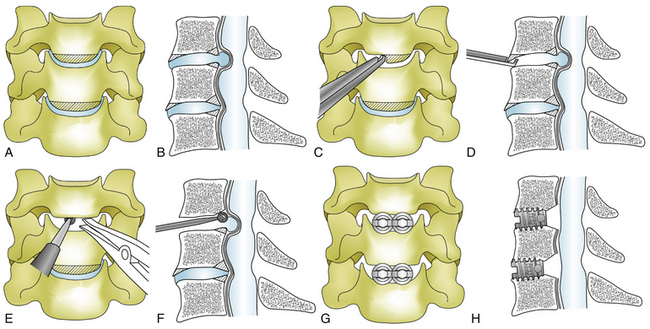
Twin-Cage Method for Cervical Spondylosis and Herniated Disc
In cases of cervical spondylosis and herniated discs, with or without instability, two smaller M-cages of 6, 7, or 8 mm in inner diameter are used side by side in a twin-cage fashion after decompression (Fig. 41-1).
Originally the disc space was opened with a reamer for cage insertion3; however, this reaming was soon abandoned to avoid subsidence of the cages into the vertebrae. Now, by using the spreader efficiently and by drilling the medial portion of the uncinate process after fine adjustment, cylindrical cages, most frequently 7-mm cages, are snugly inserted side by side in a locking fashion. Cages are usually packed with small bone chips of the vertebrae and hydroxyapatite granules (Apaceram, Hoya Corp., Tokyo). The ventral surface of the cages is leveled to the ventral cortex of the vertebral body to avoid subsidence of the cages.
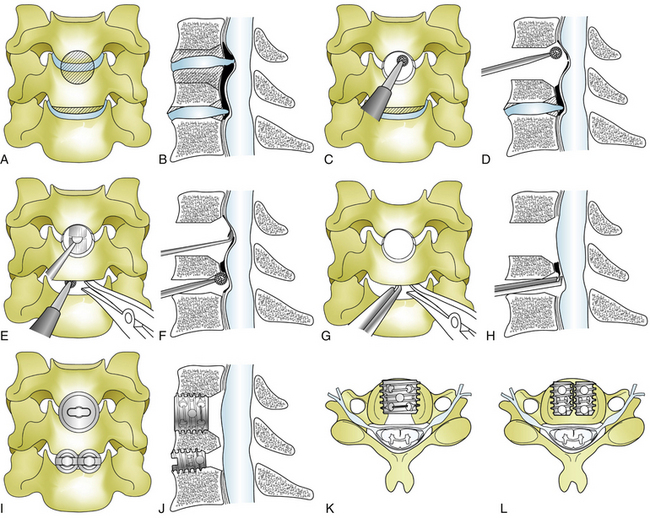
Single-Cage Method for Ossification of the Posterior Longitudinal Ligament
In cases of OPLL, usually of the local or segmental type, some degree of corpectomy is often necessary to remove the ossified ligament that extends behind the vertebrae (Fig. 41-2). For this reason, a larger M-cage of 10, 12, or 14 mm in inner diameter (most frequently 12 mm) is usually used in the single-cage method. After complete discectomy, a Williams microsurgical saw or an ultrasonic bone scalpel (Sonopet, Stryker, Kalamazoo, MI) is used to perform an 8- to 9-mm square corpectomy followed by 10-mm reaming to make a round hole; usually a 12-mm cage packed with bone chips and hydroxyapatite granules is snugly inserted after decompression.3,29
If a Williams saw or Sonopet is not available, a round hole can be made stepwise by using progressively larger reamers. Through this keyhole, the remaining vertebra, spur, and ossified ligament are drilled out with great care, making the OPLL paper-thin by using a high-speed drill with a diamond bur and an ultrasonic bone curette (Sonopet, Stryker). The thinned-out OPLL and hypertrophied ligament, as well as associated disc fragments, are then carefully separated from the dura and excised by using a microdissector, microknife, curettes, and Kerrison rongeurs.
Most of the ossified ligament behind the vertebrae can be removed through this keyhole and through the adjacent disc space above or below the keyhole (see Fig. 41-2). After good hemostasis a cage is inserted with its ventral surface leveled to the ventral cortex of the vertebrae to minimize subsidence. For the past decade, dural ossification has not been removed; instead, it is left alone after good decompression of the dura to avoid leakage of cerebrospinal fluid (CSF). Dural ossification is found in 15.3% of all cases of OPLL, in 10.5% of segmental types, and in 41% of nonsegmental types.30
Surgical Cases
Surgical results were satisfactory (excellent and good) in 88% judging by Odom’s criteria and the Neurosurgical Cervical Spine Scale (NCSS)31; 56% returned to their previous work and 32% to lighter work. No significant difference in surgical results was observed between patients with cervical spondylosis and those with OPLL. The group aged 70 years and older had less favorable results but showed significant neurologic improvement—as much as 72%. The younger group showed satisfactory results in 91%. The most influential factor for poor prognosis was the severity of preoperative neurologic status. Cases with severe myelopathy disclosed satisfactory results in only 65%, and cases with mild to moderate myelopathy disclosed satisfactory results in 93%.27,28
Postoperative wound hematoma and infection were present in less than 1% of patients. Postoperative temporary dysphagia was seen in 2%. No neurologic deterioration was seen, except for one patient with temporary root sign and another with temporary worsening of a long tract sign.
Discussion
Since the ventral approach with interbody fusion for cervical discs was introduced by Cloward and Smith and Robinson in 1958, ventral discectomy with iliac bone graft, with or without the help of an operating microscope, has been the standard procedure with reasonably satisfactory results.32–34
However, postoperative kyphotic deformity, graft collapse, and donor site discomfort cannot be totally disregarded. To avoid these disadvantages, microdiscectomy without bone graft has been advocated by many authors with excellent results.20–22 This method, however, is often not appropriate for spondylosis with prominent bilateral spurs and OPLL. Allografting is one solution to the problems of the autograft, but is reported to have a lower fusion rate compared with autograft. Therefore, ventral plate fixation seems to be necessary for allografting.10 Because allografting is not available in some countries, including Japan, hydroxyapatite, coralline, and titanium threaded cages have been introduced as a substitute for autogenous grafts for cervical interbody fusion.9,26,33,35 Threaded cylindrical cages, which were initially introduced for lumbar interbody fusion,25 have been used for a cervical ventral approach for cervical spondylosis and local and segmental OPLL for the past decade.3,26–28
OPLL of the cervical spine, which was first reported in an autopsy study by Tsukimoto in 1960,36 has been extensively studied for its pathophysiology and surgical management over the past 30 years, especially in Japan.6,13,37–39 OPLL is often associated with cervical spondylosis and disc herniation and is one of the major causes of cervical compressive myelopathy in Japan, but it is also found in other countries to a lesser degree.18 Therefore, it is absolutely vital to establish the precise diagnosis in patients with cervical myelopathy or radiculopathy by using routine radiographs, CT with sagittal reformation, and MRI to make the right and appropriate decision for surgical treatment.
If segmental or local type OPLL is present with cord compression at one or two levels (sometimes at three levels in cases with kyphotic spines), the ventral approach is often selected by surgeons with expertise in microsurgery.12,28 In extensive OPLL of continuous or mixed type with multilevel cord compression over three to four levels, expansive laminoplasty (open-door or double-door) is commonly used because multilevel decompression is readily obtained and the procedure is less risky compared with the ventral approach.13–15
The twin-cage method is more commonly used than the two-levels method to treat single-level cervical spondylosis and herniated discs. In cases associated with OPLL, keyhole corpectomy with the single-cage method with a larger cage is the procedure of choice to access OPLL behind the vertebral body, but more frequently the combined approach, in which the single-cage and twin-cage methods are performed at adjacent levels, is carried out in two-level operations (65%). The three-level cage fixation is relatively rare in cervical spondylosis (2.2%) but is sometimes indicated in cervical OPLL (8.9%). Surgical results are generally satisfactory with rare complications and early ambulation, short hospital stays, and early return to work. Biomechanical testing of cervical interbody cages has indicated better stability with the twin-cage method compared with the single-cage method, and no significant difference in design variations between the cages.40,41 Good bony fusion was observed in 90% at 1-year follow-up.
Epstein N. The surgical management of ossification of the posterior longitudinal ligament in 51 patients. J Spinal Disord. 1993;6:432-455.
Matge G. Anterior interbody fusion with the BAK-Cage in cervical spondylosis. Acta Neurochir (Wien). 1998;140:1-8.
Mizuno J., Nakagawa H. Outcome analysis of anterior decompressive surgery and fusion for cervical ossification of the posterior longitudinal ligament: report of 107 cases and review of the literature. Neurosurg Focus. 2001;10:E6.
Mizuno J., Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6:282s-288s.
Nakagawa H., Mizuno J. Threaded interbody cage fixation for cervical spondylosis and ossification of the posterior longitudinal ligament. In: Benzel E.C., editor. Spine. ed 2. Philadelphia: Elsevier Churchill Livingstone; 2005:363-369.
Nagata K., Sato K. Diagnostic imaging of cervical ossification of the posterior longitudinal ligament. In: Yonenobu K., Nakamura K., Toyama Y., editors. OPLL ossification of the posterior longitudinal ligament. ed 2. Tokyo: Springer; 2006:127-143.
1. Nagata K., Sato K. Diagnostic imaging of cervical ossification of the posterior longitudinal ligament. In: Yonenobu K., Nakamura K., Toyama Y., editors. OPLL: ossification of the posterior longitudinal ligament. ed 2. Tokyo: Springer; 2006:127-143.
2. Nakagawa H., Mizuno J., Chang H.S., et al. Minimally invasive methods in anterior approach for cervical discogenic disease. Jpn J Neurosurg (Tokyo). 1999;8:189-193.
3. Nakagawa H., Mizuno J. Threaded interbody cage fixation for cervical spondylosis and ossification of the posterior longitudinal ligament. In: Benzel E.C., editor. Spine. ed 2. Philadelphia: Elsevier Churchill Livingstone; 2005:363-369.
4. Mizuno J., Nakagawa H., Hashizume Y. Analysis of hypertrophy of the posterior longitudinal ligament of the cervical spine on the basis of clinical and experimental studies. Neurosurgery. 2001;49:1091-1098.
5. Abe H., Tsuru M., Ito T., et al. Anterior decompression for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg. 1981;55:108-116.
6. Nagashima C. Cervical myelopathy due to ossification of the posterior longitudinal ligament. J Neurosurg. 1972;37:653-660.
7. Nakagawa H., Mizuno J. The pathophysiology and management of ossification of the posterior longitudinal ligament. In: Barrow D.L., editor. Perspective in neurological surgery. St. Louis: Quality Medical; 1992:38-48.
8. Matsunaga S., Sakou T. Overview of epidemiology and genetics. In: Yonenobu K., Nakamura K., Toyama Y., editors. OPLL: ossification of the posterior longitudinal ligament. ed 2. Tokyo: Springer; 2006:7-9.
9. Kim P., Wakai S., Matsuo S., et al. Bisegmental cervical interbody fusion using hydroxyatatite implants: surgical results and long-term observation in 70 cases. J Neurosurg. 1998;88:21-27.
10. Martin G.J., Haid R.W., MacMillan M., et al. Anterior cervical discectomy with freeze-dried fibula allograft: overview of 317 cases and literature review. Spine. 1999;24:852-859.
11. Epstein N. The surgical management of ossification of the posterior longitudinal ligament in 51 patients. J Spinal Disord. 1993;6:432-455.
12. Kojima T., Waga S., Kubo Y., et al. Anterior cervical vertebrectomy and interbody fusion for multilevel spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery. 1989;24:864-872.
13. Hirabayashi K., Watanabe K., Wakano K., et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine. 1983;8:693-699.
14. Itoh Y, Nakagawa H, Mizuno J: Minimally invasive expansive laminoplasty: In Mummaneni P, Kanter AS, Wang MY, Haid RW, editors: Cervical spine surgery: current trends and challenges. St. Louis, Quality Medical Publishing [in press].
15. Nakagawa H., Mizuno J., Ohara Y. Expansive open-door laminoplasty. In: Wolfa C.E., Resnick D.K., editors. Neurosurgical operative atlas. New York: Thieme; 2007:97-101.
16. Mizuno J., Nakagawa H., Isobe M. Surgical results of anterior approach in ossification of the posterior longitudinal ligament in the cervical spine. Spinal Surg (Japan). 1997;11:39-46.
17. Isu T., Kaneda K., Kobayashi N., et al. The surgical technique of anterior cervical fusion using bone grafts obtained from cervical vertebral bodies. J Neurosurg. 1994;80:16-19.
18. Nakagawa H., Mizuno J., Tamai K., et al. Anterior approach with autogenous vertebral bone graft in ossification of the posterior longitudinal ligament of the cervical spine. Spinal Surg (Japan). 1995;9:37-42.
19. Williams R.C. Anterior cervical fusion utilizing autogenous bone graft from the cervical vertebrae. Neurosurgery. 1992;11:339-342.
20. Martins A.N. Anterior cervical discectomy with and without interbody bone graft. J Neurosurg. 1976;44:290-295.
21. Murphy M.G., Gado M. Anterior cervical discectomy without interbody bone graft. J Neurosurg. 1972;37:71-74.
22. Nakagawa H., Yamamoto H., Mizuno J., et al. Microdiscectomy and osteophytectomy without bone graft in cervical spondylosis and herniated discs: long term follow-ups. Spinal Surg (Japan). 1992;6:33-39.
23. Hakuba A. Trans-unco-discal approach: a combined anterior and lateral approach to cervical discs. J Neurosurg. 1976;45:284-291.
24. Jho H.D. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg. 1996;84:155-160.
25. Ray C.D. Threaded titanium cages for lumbar interboy fusions. Spine. 1997;22:667-680.
26. Matge G. Anterior interbody fusion with the BAK-Cage in cervical spondylosis. Acta Neurochir (Wien). 1998;140:1-8.
27. Mizuno J., Nakagawa H. Outcome analysis of anterior decompressive surgery and fusion for cervical ossification of the posterior longitudinal ligament: report of 107 cases and review of the literature. Neurosurg Focus. 2001. 10:E6
28. Mizuno J., Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6:282s-288s.
29. Nakagawa H., Kim S.-D., Mizuno J., et al. Technical advantages of an ultrasonic bone curette in spinal surgery. J Neurosurg Spine. 2005;2:431-435.
30. Mizuno J., Nakagawa H., Matsuo N., et al. Dural ossification associated with cervical ossification of the posterior longitudinal ligament: frequency of dural ossification and comparison of neuroimaging modalities in ability to identify the disease. J Neurosurg Spine. 2005;2:425-430.
31. Kadoya S. Grading and scoring system for neurological function in degenerative cervical disease: neurosurgical cervical spine scale. Neurol Med Chir (Tokyo). 1992;32:40-41.
32. Cloward B.B. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602-617.
33. Hacker R.J. A randomized prospective study of an anterior cervical interbody fusion device with a minimum of 2 years of follow-up results. J Neurosurg. 2000;93(Suppl 2):222-226.
34. Smith G.W., Robinson R.A. The treatment of certain cervical spine disorders by anterior removal of interbertebral disc and interbody fusion. J Bone Joint Surg [Am]. 1958;40:607-624.
35. Thalgott J.S., Fritts K., Giuffire J.M., et al. Anterior interbody fusion of the cervical spine with coralline hydroxyapatite. Spine. 1999;24:1295-1299.
36. Tsukimoto H. A case report: autopsy of syndrome of compression of spinal cord owing to ossification within spinal canal of cervical spines. Nippon Geka Hokan (Japan). 1960;29:1003-1007.
37. Hashizume Y., Iijima S., Kishimoto H., et al. Pathology of spinal cord lesions caused by ossification of the posterior longitudinal ligament. Acta Neuropathol. 1984;63:123-130.
38. Mizuno J., Nakagawa H., Iwata K., et al. Pathology of the spinal cord lesions caused by ossification of the posterior longitudinal ligament with special reference to reversibility of the spinal cord lesion. Neurol Res. 1992;14:312-314.
39. Terayama K., Maruyama S., Miyashita R., et al. Ossification of the posterior longitudinal ligament in the cervical spine. Orthop Surg (Japan). 1994;15:1083-1095.
40. Kandiziora F., Pflagmacher P., Schafer J., et al. Biomechanical comparison of cervical spine interbody fusion cages. Spine. 2001;26:1850-1857.
41. Takahashi T., Tominaga T., Yokobori T., et al. In vitro biomechanical evaluation of interbody fusion cage for anterior cervical fusion in a caprine model. Spinal Surg (Japan). 2001;15:1-6.