CHAPTER 31 Thorascopic Spine Surgery
The applications of endoscopic spine surgery have been expanded since the first publications spanning nearly two decades.1–6 Operating techniques have been standardized and unified and today are safe procedures with low complication rates that are comparable to those of open procedures, presuming the existence of adequate training and manual skills of the surgeon.7 Thus, endoscopic operations on the spinal column no longer represent exceptional interventions but have become standard procedures in spine surgery. Thoracoscopic techniques can be used to approach the anterior column of the spine in the area between the third thoracic vertebra and the third lumbar vertebra because endoscopic splitting of the diaphragm also allows the exposure of the upper sections of the lumbar spine. The application potential includes anterior release procedures, with incision and resection of ligaments and intervertebral disks; removal of fragmented disks or sections of vertebrae, including anterior decompression of the spinal canal; replacement of vertebral bodies with biologic or alloplastic materials; and ventral stabilization procedures with implants designed for use in endoscopic spine surgery. In addition, percutaneous endoscopic techniques are used for minimally invasive treatment of degenerative disk disease of the thoracic and lumbar spine.
Indications
Overall, the range of indications for the technique described here can be defined as follows:
Technical Requirements
Image Transmission
The key to any endoscopic technique is image recording and transmission. “You will do what you can see,” and therefore true high-definition video technique has also revolutionized the endoscopic technique, which now provides an endoscopic view comparable to images that the microscope is able to provide. A high-intensity xenon light source is required to illuminate the thoracic cavity. A rigid, long, 30-degree scope enables positioning of the camera far away from the working portal, thus facilitating undisturbed working and variable adjustment of the angle of vision. The intraoperative view is transmitted onto two or three flat screens (Fig. 31-1).
Instruments
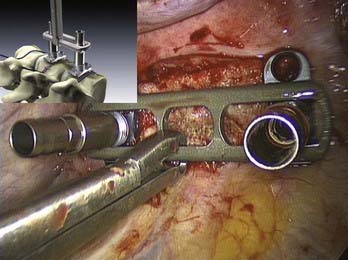
![]() Complete sets of instruments for soft tissue and bone preparation are manufactured by contemporary instrument manufacturers (Fig. 31-2). Instruments should have a nonreflective surface and a depth scale on both sides and be ergonomically designed with big handles for safe control and handling. The technique by which they are used is called the three-point anchoring technique, which means that every sharp and potentially dangerous instrument is guided by both hands; one hand is based on the chest wall, always controlling and sometimes neutralizing unexpected forces and movements of the instrument (see Video 31-9).
Complete sets of instruments for soft tissue and bone preparation are manufactured by contemporary instrument manufacturers (Fig. 31-2). Instruments should have a nonreflective surface and a depth scale on both sides and be ergonomically designed with big handles for safe control and handling. The technique by which they are used is called the three-point anchoring technique, which means that every sharp and potentially dangerous instrument is guided by both hands; one hand is based on the chest wall, always controlling and sometimes neutralizing unexpected forces and movements of the instrument (see Video 31-9).
Implants
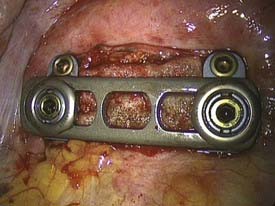
Several implants for anterior instrumentation that can be used for endoscopic, mini-open, or open spine surgery are now available. Most of them are based on the principle of a cannulated screw and plate system, first allowing the implantation of K wires under fluoroscopic control to be used as landmarks, followed by the insertion of screws. Biomechanically tested four-point fixation implants provide adequate angular stability, which is necessary for single anterior instrumentation (Fig. 31-3).13
For vertebral body replacement, bone graft (autograft or allograft) or mechanical devices can be used and filled or surrounded with the autologous bone harvested from the corpectomy site. A wide variety of expandable titanium cages is currently available.14
Preoperative Requirements
Education of the Patient
The patient should be informed about the following approach-specific risks and hazards:
Marking the Portals
![]() As a routine, four portals are used: scope portal, working portal, suction-irrigation portal, and retractor portal (Video 31-2). Their location and, in particular, the position of the working portal are crucial for the endoscopic operation to proceed in the optimal fashion. For this reason, the lesion is first displayed in the lateral projection (with reference to the patient’s body) under precise adjustment of the image intensifier, and a marker is used to draw the injured spinal section onto the lateral thoracic wall (Fig. 31-4). The working portal is drawn in directly above the lesion. The trocar for the endoscope is marked either caudal or cranial to the working portal, depending on the height of the lesion, and following the axis of the spine. The distance from the working portal is approximately two intercostal spaces. The entry points for suction and irrigation and for the retractor are then located ventral from these portals.
As a routine, four portals are used: scope portal, working portal, suction-irrigation portal, and retractor portal (Video 31-2). Their location and, in particular, the position of the working portal are crucial for the endoscopic operation to proceed in the optimal fashion. For this reason, the lesion is first displayed in the lateral projection (with reference to the patient’s body) under precise adjustment of the image intensifier, and a marker is used to draw the injured spinal section onto the lateral thoracic wall (Fig. 31-4). The working portal is drawn in directly above the lesion. The trocar for the endoscope is marked either caudal or cranial to the working portal, depending on the height of the lesion, and following the axis of the spine. The distance from the working portal is approximately two intercostal spaces. The entry points for suction and irrigation and for the retractor are then located ventral from these portals.
Operative Techniques
Approach to the Thoracolumbar Junction
![]() This operation is also performed using single-lung ventilation (Video 31-4).8,11,15,16 Here, too, the approach side is decided by the location of the major vessels, which can be identified from the preoperative computed tomographic scan. In most cases, the best approach to the thoracolumbar junction is from the left. Placement of the trocars and instruments is illustrated in Figure 31-5.
This operation is also performed using single-lung ventilation (Video 31-4).8,11,15,16 Here, too, the approach side is decided by the location of the major vessels, which can be identified from the preoperative computed tomographic scan. In most cases, the best approach to the thoracolumbar junction is from the left. Placement of the trocars and instruments is illustrated in Figure 31-5.
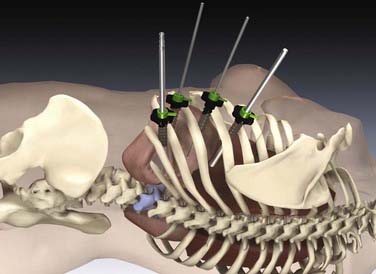
FIGURE 31-5 Placement of the trocars and instruments for an endoscopic intervention at the thoracolumbar spine.
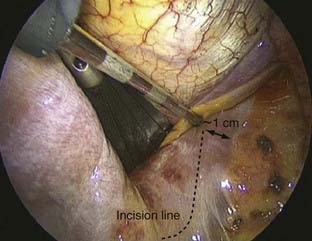
The dome-like diaphragm is firmly connected at its margins with the sternum, ribs, and spine and arches up into the thoracic cavity. Topographically speaking, the attachment sites of the diaphragm to the spine are at the level of the first lumbar vertebra, whereas the lowest point of the thoracic cavity projects with the phrenicocostal sinus at the level of the baseplate of the second lumbar vertebra (Fig. 31-6). This makes it possible to place a trocar intrathoracically in the phrenicocostal sinus, which, after incision of the diaphragm attachment to the spine, provides access to the retroperitoneal section of the thoracolumbar junction down to the baseplate of the second lumbar vertebra. This requires a 4- to 5-cm–long incision following the attachment of the diaphragm; access to the L1-2 intervertebral disk can be obtained with a shorter incision of 2 to 3 cm (Fig. 31-7).15–17
Endoscopic Treatment of Spinal Trauma (Anterior Reconstruction)
Ventral Instrumentation with a Constraint Plate Implant
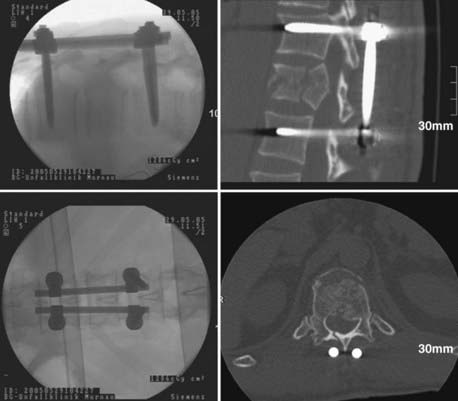
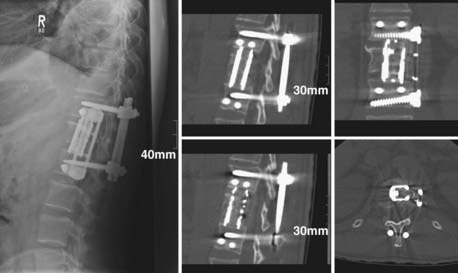
The distance between the screws is defined with a special measuring instrument to select a plate of the correct length. This is introduced lengthwise into the thoracic cavity through the incision for the working portal, laid onto the clamping elements with a holding forceps, and there definitively fixed with nuts with a starting torque of 15 Nm. The plate can be brought into direct bone contact with the lateral vertebral body wall by tightening the bone screws. The ventral screws are inserted after temporary fixation of a targeting device and opening of the cortex. Because of the heart shape of the vertebral body, the ventral screws are usually 5 mm shorter than the dorsal screws. The fixation of the angle-stable implant ends with the insertion of a locking screw that locks the polyaxial mechanism of the dorsal screws (Fig. 31-8).
Special Indications
Removal of Posterior Wall Fragments: Endoscopic Anterior Decompression9
Operative Technique
Case Report
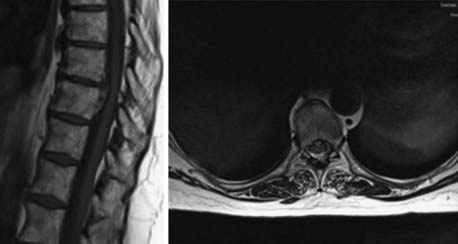
A 43-year-old man was referred to our hospital demonstrating severe back pain at the thoracolumbar junction, weakness of the lower extremities below T12, and moderate bowel and bladder dysfunction. After radiologic diagnostics and neurological examination, the patient was brought to the operating room for dorsal reduction and stabilization by internal fixator followed by thoracoscopic anterior decompression and reconstruction (Figs. 31-9 to 31-11).
Removal of Protruded Herniated Disk: Endoscopic Treatment of Degenerative Disk Disease
Only 0.15% to 1% of all operative procedures due to degenerative disk disease are done to treat thoracic disk protrusion.18–20 As a specialty of the thoracic region, there is a “calcified disk” and an “intradural disk herniation” (Fig. 31-12). These removal procedures are technically demanding. Because of a smaller diameter of the thoracic spinal canal in conjunction with a spinal cord of bigger volume at these levels, there is little space to accommodate disk herniation. In consequence, small disk protrusions might cause significant symptoms. Depending on the localization and expansion of herniation—medial, mediolateral, intraforaminal, or extraforaminal—typical symptoms of thoracic disk herniation can be described.
Operative Treatment Options
The following procedures21 are available, fitting the needed level and herniation site:
![]() Because of the high morbidity of the open transthoracic approach, indications were few. The advent of a tissue-preserving thoracoscopic approach6,12,24 led to greater numbers of indications, centrolateral and lateral disk herniations remaining to be approached posterolaterally. The thoracoscopic approach and operative technique are described here (Video 31-13).
Because of the high morbidity of the open transthoracic approach, indications were few. The advent of a tissue-preserving thoracoscopic approach6,12,24 led to greater numbers of indications, centrolateral and lateral disk herniations remaining to be approached posterolaterally. The thoracoscopic approach and operative technique are described here (Video 31-13).
Operating Room Setup
Positioning the Patient
The side for the approach has to be chosen primarily by the localization of the disk herniation and the adjacent great vessels. In cases of centromedial and right lateral herniation, the approach from the right side is preferred (Fig. 31-13).
Confirmation of the Operative Site
Verification of the level of disease can be demanding before the main procedure is started. Several methods are recommended to ensure that the right intervertebral disk space is addressed. Dickman and Rosenthal12 recommend a preoperative radiograph of the chest to localize the level. Large osteophytes seen on computed tomographic scans or plain radiographs can be used as surgical or radiographic landmarks. After the endoscopic procedure has started, it is recommended that the ribs be counted with use of the C-arm, beginning caudally at the 12th rib. Rib identification should be repeated several times to ensure accuracy. The pleura over the identified rib head is then cauterized. Attention must be paid to the patient with an abnormal number of ribs, because the spinal level could be misidentified.
Operative Technique
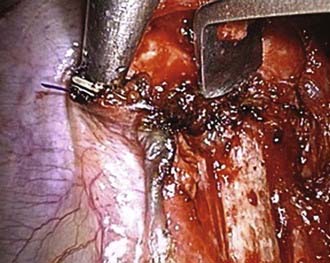
The general principle of the procedure is to resect the rib head of the adjacent rib and expose the pedicle and the affected intervertebral disk (Fig. 31-14). A block-shaped defect will then be created in the adjacent vertebral bodies for removal of soft and calcified disk material away from the dura into the defect. Afterward, the rib head, which usually fits into the defect, is used for a monosegmental fusion procedure to be accomplished by ventral instrumentation.
Technical and Operative Details
Partial corpectomy is performed with a high-speed diamond bur or an osteotome, creating a well-defined, block-shaped central defect involving the upper and lower thirds of the adjacent vertebral bodies. Initially, the posterior vertebral body wall is preserved (Fig. 31-15).
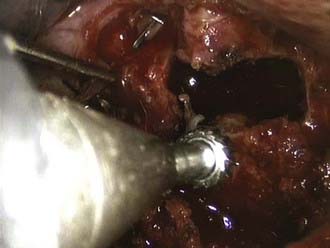
FIGURE 31-15 Partial corpectomy T9 and T10 with a high-speed bur to create a defect in the vertebral bodies in front.
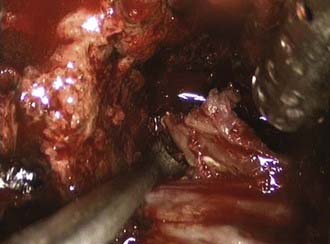
Once the base of the pedicle caudal to the intervertebral disk space is identified, the thickness can be reduced with a diamond bur to weaken the pedicle and to facilitate the transection with Kerrison rongeurs. Dickman12 recommends starting at the upper rim of the pedicle because of less bleeding from the epidural venous plexus. Under direct endoscopic view of the dura, the posterior wall is then dissected off the dura and carefully pushed into the corpectomy site or thinned out with a high-speed diamond bur. The sequestered part of the disk is then removed with dissectors and rongeurs. If there is an intradural calcified herniated disk, the intradural part of the sequestrated disk has to be carefully separated from the arachnoid mater with microdissection (Fig. 31-16). Even if this is not possible without tearing the dura, the base of the calcified disk can be thinned with the diamond bur, leaving only a shell of calcification attached to the dura free to move without bone or soft tissue impingement. Complete decompression of the dural sac across the vertebral body to the level of the contralateral pedicle is confirmed by direct endoscopic view and radiologically by fluoroscopy with use of a nerve hook in an anteroposterior projection. After decompression, the dura is covered with Gelfoam. The corpectomy defect is reconstructed with the rib head harvested at the first step. The size of the graft is determined with an endoscopic measurement of the defect.
Alberico AM, Sahni KS, Hall JAJr, et al. High thoracic disc herniation. Neurosurgery. 1986;19:449-451.
Albrand OW, Corkill G. Thoracic disc herniation. Treatment and prognosis. Spine. 1979;4:41-46.
Awwad EE, Martin DS, Smith KRJr, et al. Asymptomatic versus symptomatic herniated thoracic discs: their frequency and characteristics as detected by computed tomography after myelography. Neurosurgery. 1991;28:180-186.
Beisse R. Video-assisted techniques in the management of thoracolumbar fractures. Orthop Clin North Am. 2007;38:419-429.
Beisse R. Endoscopic surgery on the thoracolumbar junction of the spine. Eur Spine J. 2006;15:687-704.
Beisse R, Muckley T, Schmidt MH, et al. Surgical technique and results of endoscopic anterior spinal canal decompression. J Neurosurg Spine. 2005;2:128-136.
Beisse R, Potulski M, Beger J, et al. Development and clinical application of a thoracoscopic implantable frame plate for the treatment of thoracolumbar fractures and instabilities. Orthopäde. 2002;31:413-422.
Beisse R, Potulski M, Bühren V. Endoscopic techniques for the management of spinal trauma. Eur J Trauma. 2001;27:275-291.
Beisse R, Potulski M, Temme C, et al. [Endoscopically controlled division of the diaphragm. A minimally invasive approach to ventral management of thoracolumbar fractures of the spine.]. Unfallchirurg. 1998;101:619-627.
Beisse R, Trapp O. Thoracoscopic management of spinal trauma. Oper Tech Neurosurg. 2006;8:205-213.
Dickman CA, Rosenthal DJ, Perin NI. Thoracoscopic Spine Surgery. New York: Thieme; 1999.
Horowitz MB, Moossy JJ, Julian T, et al. Thoracic discectomy using video assisted thoracoscopy. Spine. 1994;19:1082-1086.
Kim DH, Jahng TA, Balabhadra RS, et al. Thoracoscopic transdiaphragmatic approach to thoracolumbar junction fractures. Spine J. 2004;4:317-328.
Knop C, Bastian L, Lange U, et al. Complications in surgical treatment of thoracolumbar injuries. Eur Spine J. 2002;11:214-226.
Knop C, Lange U, Bastian L, et al. Biomechanical compression tests with a new implant for thoracolumbar vertebral body replacement. Eur Spine J. 2001;10:30-37.
Le Roux PD, Haglund MM, Harris AB. Thoracic disc disease: experience with the transpedicular approach in twenty consecutive patients. Neurosurgery. 1993;33:58-66.
Mack MJ, Aronoff RJ, Acuff TE, et al. Present role of thoracoscopy in the diagnosis and treatment of diseases of the chest. Ann Thorac Surg. 1992;54:403-408.
Mack MJ, Regan J, Bobechko WP, et al. Applications of thoracoscopy for diseases of spine. Ann Thorac Surg. 1993;56:736-738.
Maiman DJ, Larson SJ, Luck E, et al. Lateral extracavitary approach to the spine for thoracic disc herniation: report of 23 cases. Neurosurgery. 1984;14:178-182.
McAfee PC, Regan JR, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. A prospective multicenter study comprising the first 100 consecutive cases. Spine. 1995;20:1624-1632.
Regan JJ, McAfee P, Mack M. Atlas of Endoscopic Spine Surgery. St. Louis: Quality Medical; 1995.
Rosenthal D, Marquardt G, Lorenz R, et al. Anterior decompression and stabilization using a microsurgical endoscopic technique for metastatic tumors of the thoracic spine. J Neurosurg. 1996;8:565-572.
Rosenthal D, Rosenthal R, Simone A. Removal of a protruded disc using microsurgery endoscopy. Spine. 1994;19:1087-1091.
Stillerman CB, Chen TC, Day JD, et al. The transfacet pedicle-sparing approach for thoracic disc removal: cadaveric morphometric analysis and preliminary clinical experience. J Neurosurg. 1995;83:971-976.
1 Mack MJ, Aronoff RJ, Acuff TE, et al. Present role of thoracoscopy in the diagnosis and treatment of diseases of the chest. Ann Thorac Surg. 1992;54:403-408.
2 Mack MJ, Regan J, Bobechko WP, et al. Applications of thoracoscopy for diseases of spine. Ann Thorac Surg. 1993;56:736-738.
3 McAfee PC, Regan JR, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. A prospective multicenter study comprising the first 100 consecutive cases. Spine. 1995;20:1624-1632.
4 Regan JJ, McAfee P, Mack M. Atlas of Endoscopic Spine Surgery. St. Louis: Quality Medical; 1995.
5 Rosenthal D, Marquardt G, Lorenz R, et al. Anterior decompression and stabilization using a microsurgical endoscopic technique for metastatic tumors of the thoracic spine. J Neurosurg. 1996;8:565-572.
6 Rosenthal D, Rosenthal R, Simone A. Removal of a protruded disc using microsurgery endoscopy. Spine. 1994;19:1087-1091.
7 Knop C, Bastian L, Lange U, et al. Complications in surgical treatment of thoracolumbar injuries. Eur Spine J. 2002;11:214-226.
8 Beisse R. Video-assisted techniques in the management of thoracolumbar fractures. Orthop Clin North Am. 2007;38:419-429.
9 Beisse R, Muckley T, Schmidt MH, et al. Surgical technique and results of endoscopic anterior spinal canal decompression. J Neurosurg Spine. 2005;2:128-136.
10 Beisse R, Trapp O. Thoracoscopic management of spinal trauma. Oper Tech Neurosurg. 2006;8:205-213.
11 Beisse R. Endoscopic surgery on the thoracolumbar junction of the spine. Eur Spine J. 2006;15:687-704.
12 Dickman CA, Rosenthal DJ, Perin NI. Thoracoscopic Spine Surgery. New York: Thieme; 1999.
13 Beisse R, Potulski M, Beger J, et al. [Development and clinical application of a thoracoscopy implantable plate frame for treatment of thoracolumbar fractures and instabilities.]. Orthopade. 2002;31:413-422.
14 Knop C, Lange U, Bastian L, et al. Biomechanical compression tests with a new implant for thoracolumbar vertebral body replacement. Eur Spine J. 2001;10:30-37.
15 Beisse R, Potulski M, Temme C, et al. [Endoscopically controlled division of the diaphragm. A minimally invasive approach to ventral management of thoracolumbar fractures of the spine.]. Unfallchirurg. 1998;101:619-627.
16 Kim DH, Jahng TA, Balabhadra RS, et al. Thoracoscopic transdiaphragmatic approach to thoracolumbar junction fractures. Spine J. 2004;4:317-328.
17 Beisse R, Potulski M, Bühren V. Endoscopic techniques for the management of spinal trauma. Eur J Trauma. 2001;27:275-291.
18 Alberico AM, Sahni KS, Hall JAJr, et al. High thoracic disc herniation. Neurosurgery. 1986;19:449-451.
19 Albrand OW, Corkill G. Thoracic disc herniation. Treatment and prognosis. Spine. 1979;4:41-46.
20 Awwad EE, Martin DS, Smith KRJr, et al. Asymptomatic versus symptomatic herniated thoracic discs: their frequency and characteristics as detected by computed tomography after myelography. Neurosurgery. 1991;28:180-186.
21 Stillerman CB, Chen TC, Day JD, et al. The transfacet pedicle-sparing approach for thoracic disc removal: cadaveric morphometric analysis and preliminary clinical experience. J Neurosurg. 1995;83:971-976.
22 Maiman DJ, Larson SJ, Luck E, et al. Lateral extracavitary approach to the spine for thoracic disc herniation: report of 23 cases. Neurosurgery. 1984;14:178-182.
23 Le Roux PD, Haglund MM, Harris AB. Thoracic disc disease: experience with the transpedicular approach in twenty consecutive patients. Neurosurgery. 1993;33:58-66.
24 Horowitz MB, Moossy JJ, Julian T, et al. Thoracic discectomy using video assisted thoracoscopy. Spine. 1994;19:1082-1086.
25 Beisse R, Potulski M, Beger J, et al. Development and clinical application of a thoracoscopic implantable frame plate for the treatment of thoracolumbar fractures and instabilities. Orthopade. 2002;31:413-422.