Thoracic Trauma
Epidemiology
Thoracic injury directly accounts for 20 to 25% of deaths from trauma, resulting in more than 16,000 deaths annually in the United States. The most common cause of injuries leading to accidental death in the United States is motor vehicle collisions (MVCs) in which immediate deaths are often caused by rupture of the myocardial wall or the thoracic aorta. Early deaths (within the first 30 minutes to 3 hours) resulting from thoracic trauma are often preventable. Causes of these include tension pneumothorax, cardiac tamponade, airway obstruction, and uncontrolled hemorrhage. Because these problems are often reversible or may be temporized nonoperatively, it is vital that emergency physicians be thoroughly familiar with their pathophysiology, clinical presentation, diagnosis, and treatment.1
Approximately 75% of patients with thoracic trauma can be managed expectantly with simple tube thoracostomy and volume resuscitation. Therefore initial care and disposition of these patients is usually performed by emergency physicians. Definitive care of these patients is often multidisciplinary in nature, involving trauma surgeons, cardiothoracic surgeons, and intensivists. Improvement in the understanding of the underlying physiologic mechanisms involved, the advancement of newer imaging modalities, minimally invasive approaches, and pharmacologic therapy contribute to decreasing the morbidity and mortality of these injured patients. The role of multidetector helical computed tomography (CT) scanning in the evaluation of trauma patients continues to expand. Although CT scans provide much greater diagnostic sensitivity than plain radiography, the precise indications for CT scanning in trauma patients remain unclear. Concerns regarding cost, contrast-induced nephrotoxicity, and cumulative radiation exposure to the thorax have been mounting.2
Injuries to the lung parenchyma are common in severely injured patients and include contusion, laceration, and hematoma.1 Hemothorax and pneumothorax are also common injuries in patients with thoracic trauma. Treatment of these injuries has changed during the past decade primarily because of advances in diagnostic imaging techniques and an increased understanding of the pathophysiology.
Chest Wall Injury
Among victims sustaining thoracic trauma, approximately 50% will have chest wall injury: 10% minor, 35% major, and 5% flail chest injuries.1 Chest wall injuries are not always obvious and can easily be overlooked during the initial evaluation.
Rib Fracture
Simple rib fractures are the most common form of significant chest injury, accounting for more than half the cases of blunt trauma.1 The susceptibility to rib fracture increases with age. The importance of this injury is not the fracture itself but rather the associated potential complications, particularly pneumothorax, hemothorax, pulmonary contusions, and post-traumatic pneumonia. Rib fractures in children signify serious trauma to the thorax and have a high incidence of underlying injury.
Anatomy and Pathophysiology
The true danger of rib fracture involves not the rib itself but the potential for penetrating injury to the pleura, lung, liver, or spleen. Fractures of ribs 9 to 11 are associated with intra-abdominal injury. Patients with right-sided rib fractures are almost three times more likely to have a hepatic injury, and patients with left-sided rib fractures are almost four times more likely to have a splenic injury.3 Fractures of ribs 1 to 3 may indicate severe intrathoracic injury. The presence of two or more rib fractures at any level is associated with a higher incidence of internal injuries. Elderly patients with multiple rib fractures have a greater incidence of pneumonia and a higher mortality compared with patients younger than age 65 years.4–6 To prevent a minor injury from developing into a serious complication, these fractures should be diagnosed rapidly and treated expectantly.
Diagnostic Strategies
Although clinical impression and physical findings are sensitive, they are not specific and are therefore unreliable for making an accurate diagnosis. Chest x-ray films often do not demonstrate the presence of rib fractures but are of greatest value in suggesting significant intrathoracic and mediastinal injuries. Although the upright posteroanterior chest radiograph has a higher yield in detecting rib fractures or their complications compared with other views, CT scans are significantly more effective than chest x-ray examination in detecting rib fractures (Fig. 45-1).7 Rib series and expiratory, oblique, and cone-down views should not be used routinely. However, if simple rib fractures are strongly suspected or recognized on a clinical basis, there is no need to routinely obtain a CT scan unless other intrathoracic pathology needs to be studied.
Management
The greater the number of fractured ribs, the higher the mortality and morbidity rates. Patients with three or more fractured ribs, despite the lack of other traumatic injuries, should likely be hospitalized to receive aggressive pulmonary therapy and appropriate effective analgesia. Elderly patients with six or more fractured ribs should be treated in intensive care units owing to high morbidity and mortality. Older patients will probably require narcotic preparations, but care should be taken to avoid oversedation because of the potential for respiratory failure.8
Multiple rib fractures in trauma patients are associated with significant morbidity and mortality. Intercostal nerve blocks with a long-acting anesthetic such as bupivacaine with epinephrine may relieve symptoms up to 12 hours with excellent results. Such nerve blocks are achieved by administration of 1 or 2% lidocaine or 0.25% bupivacaine along the inferior rib margin several centimeters posterior to the site of the fracture. One rib above and one rib below the fractured rib should also be blocked for optimal analgesia. Other alternatives for hospitalized patients include patient-controlled analgesia, parenteral opiates, and thoracic epidural analgesia.9
Clinical Course
Most rib fractures heal uneventfully within 3 to 6 weeks, and patients should expect a gradual decrease in their discomfort during this period. Analgesics are usually necessary during the first 1 or 2 weeks. However, in addition to the complications of hemopneumothorax, atelectasis, pulmonary contusion, and pneumonia, rib fractures can result in post-traumatic neuroma or costochondral separation. These unusual complications are painful and heal slowly. Special attention should be paid to patients with displaced rib fractures, who may develop delayed hemorrhage resulting in death, typically from intercostal artery tears that clot off and then rebleed.10 In these patients, admission and close observation for these delayed sequelae are typically warranted.
Sternal Fracture
Anatomy and Pathophysiology
The natural history of a nondisplaced sternal fracture is contrary to intuition. It had been thought that the magnitude of the forces required to fracture the sternum must be associated with significant trauma to the mediastinal structures. However, isolated sternal fractures are relatively benign, with low mortality (<1%) and low intrathoracic morbidity.11
Cardiac complications, such as myocardial contusion, occur in 1.5 to 6% of cases. There is no association between sternal fracture and aortic rupture. Spinal fractures are seen in less than 10% of cases and rib fractures in 21%.12 Although sternal fractures may occur in the context of major blunt chest trauma, the presence of a sternal fracture does not imply other major life-threatening conditions. However, associated mediastinal injuries should be considered.
Diagnostic Strategies
Most sternal fractures are transverse, and a lateral radiographic view is often diagnostic. These fractures can be missed radiographically because a lateral plain chest x-ray film is not usually obtained during the initial trauma evaluation. Furthermore, plain films are sometimes inconclusive. Even if the sternal fracture is diagnosed by plain radiographs, the extent of the injury is often underappreciated. The advent of helical CT, especially with three-dimensional images of the skeletal system, has resulted in markedly improved diagnosis of sternal fractures. Emerging literature suggests that ultrasound (US) may be more sensitive than plain radiography.13
Although most nondisplaced sternal fractures are not associated with significant intrathoracic injuries, a conservative approach is to obtain a chest CT scan to rule out any other pathology. This may be clinically important in determining the best management of the sternal fracture in terms of conservative management versus surgical fixation.14 Chest CT also helps to rule out any associated mediastinal injuries. A 12-lead electrocardiogram (ECG) should also be obtained during the initial evaluation.
Management
Treatment consists of providing adequate analgesia. In the absence of associated injuries, more than 95% of patients with isolated sternal fractures who can achieve adequate pain control with oral medications can be safely discharged home. However, a small subset of patients have sternal fractures that are displaced or produce overlying bone fragments that may cause severe pain, respiratory compromise, or physical deformity and, if untreated mechanically, result in nonunion. These patients are best referred for operative fixation.15
Flail Chest
Anatomy and Pathophysiology
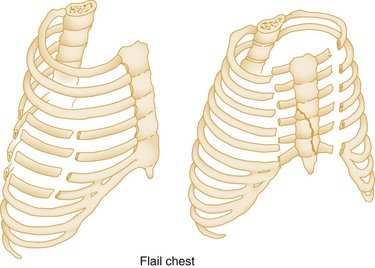
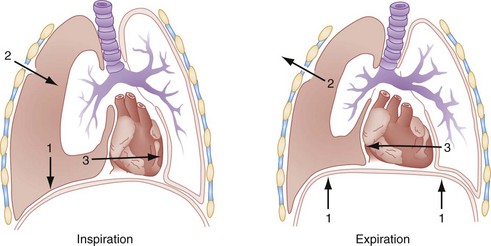
Flail chest results when three or more adjacent ribs are fractured at two points, allowing a freely moving segment of the chest wall to move in paradoxical motion (Fig. 45-2). It can also occur with costochondral separation or vertical sternal fracture in combination with rib fractures. Because of its common association with pulmonary contusion, it is one of the most serious chest wall injuries (Fig. 45-3).
Management
Respiratory decompensation is the primary indication for endotracheal intubation and mechanical ventilation for patients with flail chest. Obvious problems, such as hemopneumothorax or severe pain, should be corrected before intubation and ventilation are presumed necessary. In fact, in the awake and cooperative patient, noninvasive continuous positive airway pressure (CPAP) by mask may obviate the need for intubation.16 In general, the most conservative methods for maintaining adequate oxygenation and preventing complications should be used. Adequate analgesia is of paramount importance in patient recovery and may contribute to the return of normal respiratory mechanics.
Patients without respiratory compromise generally do well without ventilatory assistance. Several studies have found that patients treated with intercostal nerve blocks or high segmental epidural analgesia, oxygen, intensive chest physiotherapy, careful fluid management, and CPAP, with intubation reserved for patients in whom this therapy fails, have shorter hospital courses, fewer complications, and lower mortality rates.17 Avoidance of endotracheal intubation, particularly prolonged intubation, is important in preventing pulmonary morbidity because intubation increases the risk of pneumonia.18
There is also evidence that early operative internal fixation of the flail segment results in a speedier recovery, decreased complications, and better cosmetic and functional results, and that it is cost-effective. Indications for open fixation for flail chest include patients who are unable to be weaned from the ventilator secondary to the mechanics of flail chest, persistent pain, severe chest wall instability, and a progressive decline in pulmonary functions.15,19
The patient with flail chest should be treated in the ED as if pulmonary contusion exists regardless of whether mechanical ventilation is used. The mortality rate associated with flail chest is between 8 and 35% and is directly related to the underlying and associated injuries. However, unilateral flail chest was reported to be infrequently associated with death in one large series.20 Those who recover from flail chest may develop long-term disability with dyspnea, chronic thoracic pain, and exercise intolerance.
Nonpenetrating Ballistic Injury
Many law enforcement officers, emergency medical services personnel, and private security guards wear lightweight synthetic body armor for protection against gunshot injury. In addition, there have been a number of reports of armed robbers wearing such vests in anticipation of exchanging gunfire with police or security personnel.21 These vests are “bullet resistant” rather than “bulletproof,” depending on the weapon being used against them. They are composed of many different combinations of synthetic fibers such as Kevlar.
Another type of nonpenetrating ballistic injury is caused by rubber bullets and beanbag shotgun shells. Rubber bullets have been used for many years by police agencies throughout the world for crowd dispersal and for nonlethal use of force. Beanbag shotgun shells are nylon bags filled with pellets, which are fired from a standard shotgun. Both of these projectiles have the potential to cause serious injury despite their classification of “nonmetal” or “less-than-lethal” use of force.22
Management
It is recommended that all victims of nonpenetrating ballistic injury be observed closely, with overnight observation considered. This is particularly true for injuries over the abdomen, where serial examinations in coordination with CT scanning will help to detect internal injuries that may manifest in a delayed manner.23 Use of protective body armor has resulted in significantly improved survival rates and has dramatically decreased the need for surgical intervention in those protected by it. In addition, “less-than-lethal“ projectiles, such as rubber bullets and beanbag shotgun shells, offer law enforcement an alternative to conventional weapons that are considered “use of deadly force.” However, the possibility of an underlying injury resulting from this form of nonpenetrating ballistic injury should not be underestimated.
Traumatic Asphyxia
Clinical Features
Traumatic asphyxia is characterized by a deep violet color of the skin of the head and neck, bilateral subconjunctival hemorrhages, petechiae, and facial edema. Stagnation develops from capillary atony and dilation, and as the blood desaturates, purplish discoloration of the skin occurs.24 Although the appearance of these patients can be quite dramatic, the condition is usually benign and self-limited if the heavy object was removed before any hypoxic complications such as anoxic encephalopathy occurred.25
Diagnostic Strategies
Disturbance of vision has been attributed both to retinal hemorrhage, which is generally a permanent injury, and to retinal edema, which may cause transient changes in vision. One third of these patients lose consciousness, usually at the time of injury. Intracranial hemorrhages are rare, probably because of the shock-absorbing ability of the venous sinuses, but CT scan of the head should be done in patients with neurologic complaints. Neurologic manifestations typically clear within 24 to 48 hours, and long-term sequelae are uncommon.25
Pulmonary Injuries
Pulmonary Contusion
Pulmonary contusion is reported to be present in 30 to 75% of patients with significant blunt chest trauma, most often from MVCs with rapid deceleration.1 Pulmonary contusion can also be caused by high-velocity missile wounds and the high-energy shock waves of an explosion in air or water. Pulmonary contusion is the most common significant chest injury in children, and it is most commonly caused by an MVC or an automobile versus pedestrian accident.21
Anatomy and Pathophysiology
Pulmonary contusion is a direct bruise of the lung parenchyma followed by alveolar edema and hemorrhage but without an accompanying pulmonary laceration, as first described by Morgagni in 1761.26
Clinical Features
Surprisingly, many of the worst contusions occur in patients without rib fractures. It has been theorized that the more elastic chest wall, as in younger individuals, transmits increased force to the thoracic contents. Although isolated pulmonary contusions can exist, they are associated with extrathoracic injuries in the majority of patients.27
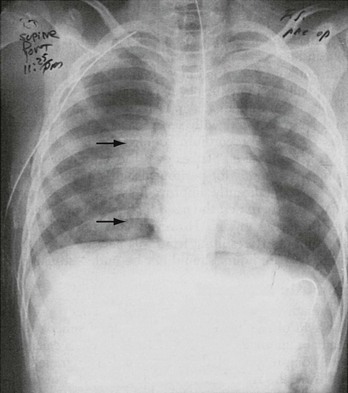
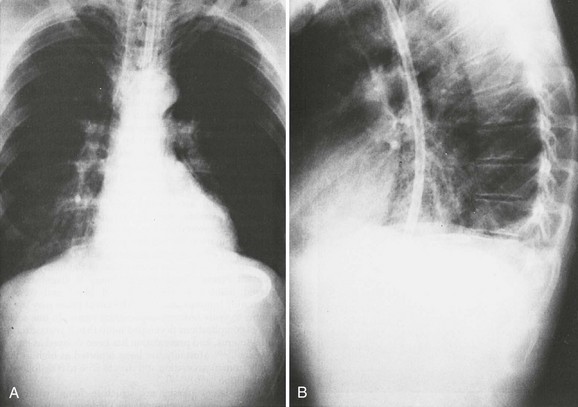
Diagnostic Strategies
Typical radiographic findings begin to appear within minutes of injury and range from patchy, irregular, alveolar infiltrate to frank consolidation (Fig. 45-4). Usually, these changes are present on the initial examination, and they are almost always present within 6 hours. The rapidity of changes on chest x-ray visualization usually correlates with the severity of the contusion. Pulmonary contusion should be differentiated from acute respiratory distress syndrome (ARDS), with which it is often confused because the radiographic appearance of the two conditions may be similar. The contusion usually manifests within minutes of the initial injury, is usually localized to a segment or a lobe, is often apparent on the initial chest study, and tends to last 48 to 72 hours. ARDS is diffuse, and its development is usually delayed, with onset typically between 24 and 72 hours after injury.28
The increased frequency of CT scans for blunt trauma patients has resulted in a corresponding increase in the diagnosis of pulmonary contusion. CT scans have been shown to detect twice as many pulmonary contusions as plain radiographs.7 Some authors suggest that pulmonary contusions visible only on CT scan and not on plain radiographs may not be clinically significant.29
Chest CT scan is particularly valuable to identify a pulmonary contusion in the acute phase after injury because plain chest x-ray films have a low sensitivity.7 Although CT scan may not be necessary to make the diagnosis of a pulmonary contusion that is evident on plain chest radiography, it may be helpful to further define the extent of the contusion and to identify other thoracic injuries. Infectious complications, sternoclavicular joint dislocation, pneumothorax, misplaced endotracheal tube, intraperitoneal air, and vertebral fracture have all been identified by CT scan in the trauma patient. Occult pulmonary contusions are those that are visible only on CT scan, not plain radiographs, and usually involve more than 20% of the lung volume. These “occult” pulmonary contusions are not associated with a worse clinical outcome as compared with blunt trauma patients without pulmonary contusion.29 Patients with pulmonary contusion visible on both conventional chest radiographs and the CT scan frequently have a higher contusion volume and a worse outcome than patients with occult pulmonary contusion. Thus pulmonary contusions that are visible on plain chest radiographs have a higher morbidity and mortality and should therefore receive special medical attention as compared with contusions only seen on the chest CT scan.
Management
Treatment for pulmonary contusion is primarily supportive.29 When only one lung has been severely contused and has caused significant hypoxemia, consideration should be given to intubating and ventilating each lung separately with a dual-lumen endotracheal tube and two ventilators. This allows for the difference in compliance between the injured and the normal lung and prevents hyperexpansion of one lung and gradual collapse of the other.30 As with flail chest, however, intubation and mechanical ventilation should be avoided if possible because they are associated with an increase in morbidity, including pneumonia, sepsis, pneumothorax, hypercoagulability, and longer hospitalization.31 The need for mechanical ventilation increases significantly when the area of pulmonary contusion exceeds 20% of total lung volume.32
Certain patients may benefit from a trial of noninvasive positive-pressure ventilation with BPAP or CPAP to avoid intubation and mechanical ventilation. In those patients most severely injured with extensive pulmonary contusions and the development of ARDS with severe hypoxia refractory to conventional therapy, some small studies suggest a possible role for extracorporeal membrane oxygenation.33
Pneumothorax
Pneumothorax, which is the accumulation of air in the pleural space, is a common complication of chest trauma. It is reported to be present in 15 to 50% of patients who sustain significant chest trauma, and it is invariably present in those with transpleural penetrating injuries.1
Anatomy and Pathophysiology
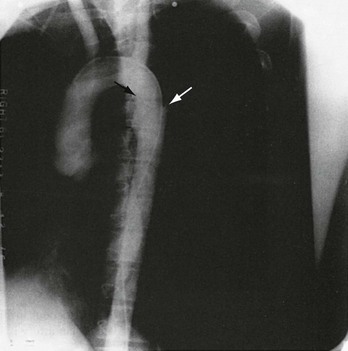
Pneumothorax can be divided into three types depending on whether air has direct access to the pleural cavity: simple, communicating, and tension. A pneumothorax is considered simple (Fig. 45-5) when there is no communication with the atmosphere or any shift of the mediastinum or hemidiaphragm resulting from the accumulation of air. It can be graded according to the degree of collapse as visualized on the chest radiograph. A small pneumothorax occupies 15% or less of the pleural cavity, a moderate one 15 to 60%, and a large pneumothorax more than 60%. Traumatic pneumothorax is most often caused by a fractured rib that is driven inward, lacerating the pleura. It may also occur without a fracture when the impact is delivered at full inspiration with the glottis closed, leading to a tremendous increase in intra-alveolar pressure and the subsequent rupture of the alveoli. A penetrating injury, such as a gunshot or stab wound, may also produce a simple pneumothorax if there is no free communication with the atmosphere (Fig. 45-6).
Communicating Pneumothorax.: A communicating pneumothorax (Fig. 45-7) is associated with a defect in the chest wall and most commonly occurs in combat injuries. In the civilian sector, this injury is typically secondary to shotgun wounds. Air can sometimes be heard flowing sonorously in and out of the defect, prompting the term “sucking chest wound.” The loss of chest wall integrity causes the involved lung to paradoxically collapse on inspiration and expand slightly on expiration, forcing air in and out of the wound. This results in a large functional dead space for the normal lung and, together with the loss of ventilation of the involved lung, produces a severe ventilatory disturbance.
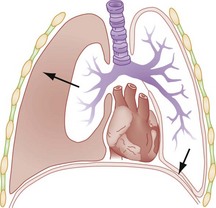
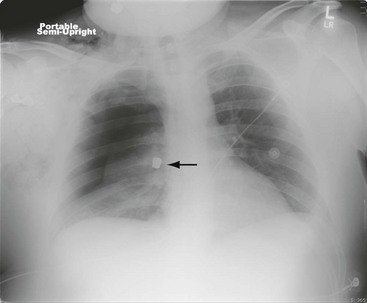
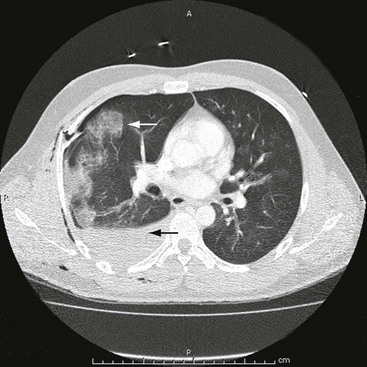
Tension Pneumothorax.: The progressive accumulation of air under pressure within the pleural cavity, with shift of the mediastinum to the opposite hemithorax and compression of the contralateral lung and great vessels, is the constellations of findings in tension pneumothorax (Figs. 45-8 and 45-9). It occurs when the injury acts like a one-way valve, prevents free bilateral communication with the atmosphere, and leads to a progressive increase of intrapleural pressure. Air enters on inspiration but cannot exit with expiration. The resulting shift of mediastinal contents compresses the vena cava and distorts the cavoatrial junction, leading to decreased diastolic filling of the heart and subsequent decreased cardiac output. These changes result in the rapid onset of hypoxia, acidosis, and shock.
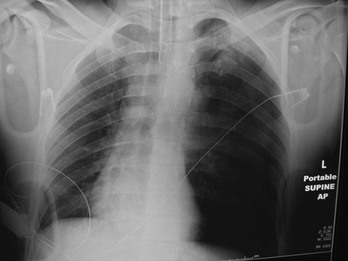
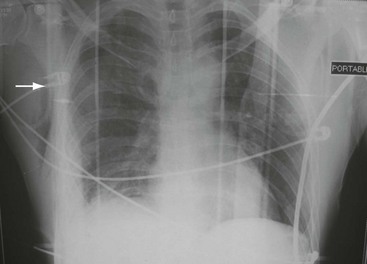
Figure 45-8 Tension pneumothorax seen in intubated patient.
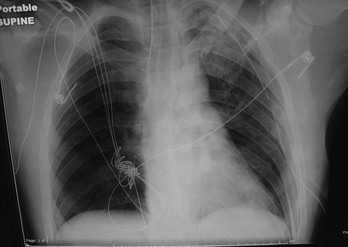
Figure 45-9 Resolution of the tension pneumothorax shown in Figure 45-7 with placement of a left-sided tube thoracostomy.
Diagnostic Strategies
Because intrapleural air tends to collect at the apex of the lung, the initial chest radiograph should be an upright full inspiratory film if the patient’s condition permits. An upright film will often reveal small pleural effusions that are not visible on supine films, and it also allows better visualization of the mediastinum. Although the chest radiograph has traditionally been the preferred initial study for diagnosing a simple pneumothorax, emerging literature suggests that a simple pneumothorax can be identified during the initial US examination of the trauma patient as part of the extended focused assessment with sonography in trauma (E-FAST) examination. Because FAST is becoming part of the routine initial evaluation of trauma patients, evaluation for the presence of a pneumothorax should be included in this rapid bedside examination, especially because this is performed before chest radiography. In fact, several studies have found that the US has greater sensitivity for pneumothorax than chest radiography.34–36
If a pneumothorax is suspected but not visualized on the initial inspiratory film, an expiratory film should be obtained because it makes the pneumothorax more apparent by reducing the lung volume. Notably, as many as one third of initial chest x-ray films will not detect a pneumothorax in trauma patients.7 Although it is not recommended as a primary method of diagnosing pneumothorax, CT is very sensitive in finding small pneumothoraces even in supine patients. When CT scans are obtained to evaluate the abdomen, it may be helpful to take a few low cuts into the chest to exclude the presence of a small pneumothorax.
Occult Pneumothorax
A pneumothorax that is absent on the initial chest radiograph but is identified on subsequent chest or abdominal CT is called an occult pneumothorax. Occult pneumothorax is being diagnosed more frequently given the increased use of CT.37,38 Studies have found rates as high as 75% for diagnosis on CT scan of occult pneumothorax that was absent on initial chest radiographs (Fig. 45-10).7,37–39
Management
In the setting of penetrating trauma in which the patient is asymptomatic and the initial chest x-ray study is negative, the patient can be safely observed and the x-ray examination repeated. Previously, it was thought that if the patient was still asymptomatic and the radiograph negative after 6 hours, the patient could be discharged. Recent experience indicates that 3 hours is probably effective and safe for observation, with repeat x-ray film before discharge for patients with penetrating trauma.40 Patients with blunt trauma in whom clinical suspicion for pneumothorax is high should still undergo a 6-hour delayed chest x-ray examination before discharge. However, if the stable patient undergoes initial screening chest CT that is negative for pneumothorax or hemothorax, the literature suggests that obtaining a delayed chest x-ray film is unnecessary, and these patients may be discharged from the ED.41
Simple Pneumothorax.: Treatment of a simple pneumothorax depends on its cause and size. Most advocate treating a traumatic pneumothorax with a chest tube to correct any respiratory compromise; treatment with a chest tube is generally thought to be safer than observation in these patients. Small pneumothoraces (i.e., <15%), whether spontaneous or traumatic, have been treated with hospitalization and careful observation if the patient is otherwise healthy and symptom free, if the patient does not need anesthesia or positive-pressure ventilation, and the pneumothorax is not increasing in size.
Isolated apical pneumothoraces of less than 25% may be observed in patients with stab wounds. This conservative method seldom has application in multisystem trauma, and a chest tube should be inserted immediately on any signs of deterioration. Some suggest that because it is small and lacks symptoms, occult traumatic pneumothorax found only on CT scan can be managed with observation and does not need treatment. Studies indicate that these injuries can be handled as small but initially detectable pneumothoraces, with observation in hemodynamically stable patients without symptoms. The data regarding the frequency with which patients with occult pneumothorax on mechanical ventilation will require tube thoracostomy are conflicting.42–44 However, an occult pneumothorax may be observed in a stable patient even if he or she is placed on positive-pressure ventilation.44
Any moderate to large pneumothorax should be treated with a chest tube. The indications for tube thoracostomy (chest tube) are listed in Box 45-1. The preferred site for insertion is the fourth or fifth intercostal space at the midaxillary line. If the tube is positioned posteriorly and directed toward the apex, it can effectively remove both air and fluid. This lateral placement of the tube is preferred not only because it is more efficient but also because it does not produce an easily visible cosmetic defect, as does the anterior site at the second interspace at the midclavicular line. With multisystem trauma, an adequate size chest tube (36-F to 40-F in adults and 16-F to 32-F in children) should be used, particularly in cases of major trauma, when hemothorax is likely to occur.
Tube thoracostomy does have some potentially serious complications, including the formation of a hemothorax, pulmonary edema, bronchopleural fistula, pleural leaks, empyema, subcutaneous emphysema, infection, intercostal artery laceration, contralateral pneumothorax, and parenchymal injury.45–47 To reduce the incidence of empyema and pneumonitis, current recommendations include the administration of empirical antibiotics with all tube thoracostomy placements.48 Pneumothoraces that have been present for more than 3 days should be reexpanded gradually without suction to avoid reexpansion pulmonary edema.
Communicating Pneumothorax.: For a patient with a communicating pneumothorax in the out-of-hospital setting, the defect should be covered immediately, which helps convert the condition to a closed pneumothorax and eliminates the major physiologic abnormality. An occlusive dressing of petrolatum gauze can be applied, but care should be taken because this can convert the injury to a tension pneumothorax, especially in patients who are intubated and undergoing positive-pressure ventilation. The wound should never be packed because the negative pressure during inspiration can suck the dressing into the chest cavity. These considerations are not as important once the patient is in the ED, where endotracheal intubation and tube thoracostomy can be performed. Positive-pressure ventilation can then be started without the fear of producing a tension pneumothorax, and the patient can be prepared for definitive surgical repair.
Tension Pneumothorax.: When the diagnosis of tension pneumothorax is suspected clinically, the pressure should be relieved immediately with needle thoracostomy, which is performed by inserting a large-bore (14-gauge or larger) catheter, at least 5 cm in length, through the second or third interspace anteriorly or the fourth or fifth interspace laterally on the involved side. Recent studies have suggested that some catheters may not be of sufficient length to penetrate the pleural space and that the lateral approach may be preferred. This method can be easily performed in the field or ED, allowing vital signs to improve during transport or preparation for a tube thoracostomy.49
Hemothorax
Hemothorax, which is the accumulation of blood in the pleural space after blunt or penetrating chest trauma, is a common complication that may produce hypovolemic shock and dangerously reduce vital capacity. It is commonly associated with pneumothorax (25% of cases) as well as extrathoracic injuries (73% of cases).50
Management
Close monitoring of the initial and ongoing rate of blood loss is performed. Immediate drainage of more than 1500 mL of blood from the pleural cavity is usually considered an indication for urgent thoracotomy. Perhaps even more predictive of the need for thoracotomy is a continued output of at least 200 mL/hr for 3 hours. General considerations for urgent thoracotomy are outlined in Box 45-2.51
Diagnostic Strategies
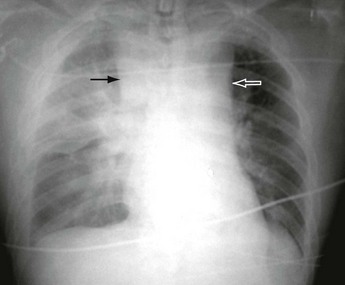
The upright chest radiograph remains the primary diagnostic study in the acute evaluation of hemothorax. A hemothorax is noted as meniscus of fluid blunting the costophrenic angle and tracking up the pleural margins of the chest wall when viewed on the upright chest x-ray film. Blunting of the costophrenic angles on upright chest radiograph requires at least 200 to 300 mL of fluid. The supine view chest film is less accurate, and it may be more difficult to make the diagnosis with the patient in this position. Unfortunately, this is often the only film available because of the patient’s unstable condition. In the supine patient, blood layers posteriorly, creating a diffuse haziness that can be rather subtle, depending on the volume of the hemothorax (Fig. 45-11).With a massive hemothorax, the large volume of blood can create a tension hemothorax, with signs and symptoms of both obstructive and hemorrhagic shock (Fig. 45-12).
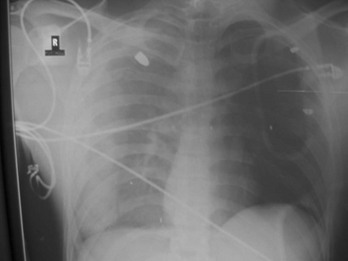
Figure 45-11 Hemothorax secondary to gunshot wound. Note haziness over right hemithorax with bullet seen in right upper lobe.
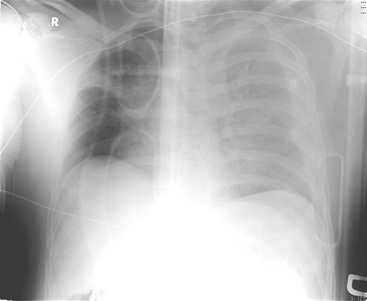
Figure 45-12 Tension hemothorax.
As is the case with pneumothoraces, US has much greater sensitivity than chest radiography in the detection of a small hemothorax, but CT scanning has the highest sensitivity, with some studies reporting up to a 25% incidence of hemothoraces diagnosed by CT that were not detected on chest radiography (Fig. 45-13).7 Perhaps more important, almost half of these occult hemothoraces underwent drainage with tube thoracostomy.52 Furthermore, one drawback of ultrasonography for the identification of traumatic hemothorax is that associated injuries readily seen on chest radiographs in the trauma patient, such as fractures or a widened mediastinum, are not readily identifiable on chest ultrasonography (Fig. 45-14). However, chest radiography and early bedside ultrasonography usually detect clinically significant hemothoraces and should routinely be performed. Delayed hemothorax may be associated with significant morbidity because the residual blood may serve as a nidus for the development of empyema or fibrothorax.
Management
As a result of the increasing frequency of chest CT scans, it has been found that there may be a greater frequency of misplaced thoracostomy tubes than is evident on conventional chest radiographs. Almost 25% of patients in one series subsequently required operative intervention as a result of complications from penetration of the lung parenchyma from tube thoracostomies.53 However, the true incidence of complications that require some surgical intervention remains unknown (Fig. 45-15).
Although beyond the scope of emergency medicine, mention is made of the role of thoracoscopy. Video-assisted thoracic surgery (VATS) is particularly useful for evaluation and evacuation of retained hemothorax, control of bleeding from intercostal vessels, and diagnosis and repair of diaphragmatic injuries.54,55 As surgeons gain more experience with the technique, VATS will likely become more widely used for other indications as well, given the decreased morbidity and length of hospital stay compared with open thoracotomy.56
Tracheobronchial Injury
Tracheobronchial injuries may occur with either blunt or penetrating injuries of the neck or chest. Penetrating injuries tend to be more obvious because of their nature, alerting both the patient and the physician, whereas blunt injuries can be occult. MVCs are the most frequent mechanism causing tracheobronchial injury, accounting for more than half of all cases.57
Although there has been an increase in the occurrence of tracheobronchial disruption, it is still a relatively rare injury, occurring in fewer than 3% of patients with significant chest injury. Its associated mortality rate is reported to be approximately 10%, although mortality rates are significantly affected by associated injuries and the timing of diagnosis and surgical repair.58,59
Clinical Features
Massive air leak through a chest tube, hemoptysis, and subcutaneous emphysema should suggest the diagnosis of major airway damage. Subcutaneous emphysema is typically the most common physical finding.57 Auscultation of the heart may reveal Hamman’s crunch if air tracks into the mediastinum. Hamman’s crunch is a crunching, rasping sound that is synchronous with the pulse and is best heard over the precordium. It is the result of the heart beating against air-filled tissues. Patients with tracheobronchial disruption have one of two distinct clinical pictures. In the first group of patients, the wound opens into the pleural space, producing a large pneumothorax. A chest tube fails to evacuate the space and reexpand the lung, and there is continuous bubbling of air in the underwater seal device.
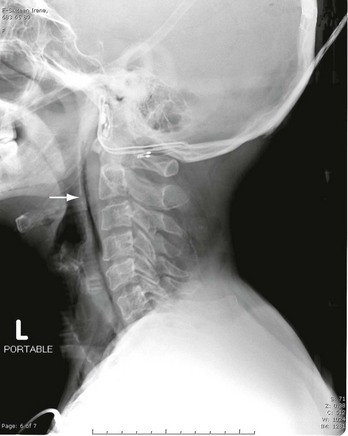
In the second group of patients there is complete transection of the tracheobronchial tree but little or no communication with the pleural space. A pneumothorax is usually not present. The peribronchial tissues support the airway enough to maintain respiration, but within 3 weeks granulation tissue will obstruct the lumen and produce atelectasis. These patients are relatively free of symptoms at the time of injury but weeks later have unexplained atelectasis or pneumonia. Radiographic signs in either group of patients are pneumomediastinum, extensive subcutaneous emphysema (Fig. 45-16), pneumothorax, fracture of the upper ribs (first through fifth), air surrounding the bronchus, and obstruction in the course of an air-filled bronchus.
Diagnostic Strategies
When tracheobronchial injury is suspected, bronchoscopy should be performed. Fiberoptic bronchoscopy is the most reliable means of establishing the diagnosis and determining the site and extent of the injury. However, CT scan has been shown to have high sensitivity in detecting tracheobronchial injury.60 Bronchopleural fistula (a communication between a bronchus and the lung parenchyma) can occur as a complication of tracheobronchial disruption and in some cases has been treated successfully via the fiberoptic bronchoscope. A mediastinal fluid collection, evidence of mediastinitis, or both may be noted on chest CT. However, bronchoscopy is usually preferred to make the diagnosis.
Management
The standard treatment for tracheobronchial injury has been surgery. However, conservative medical treatment of such injuries has been reported for tracheobronchial injury patients who meet strict selection criteria. These include patients without any major symptoms, including esophageal-associated injuries, progressive subcutaneous or mediastinal emphysema, severe dyspnea requiring intubation, difficulty with mechanical ventilation, pneumothorax with an air leak through the chest drains, open tracheal injuries, or mediastinitis.46 In most cases, thoracotomy with intraoperative tracheostomy and surgical repair of the disrupted airway should be performed as soon as possible.
Diaphragmatic Injury
Diaphragmatic rupture is present in 1 to 6% of major thoracic injuries. Diaphragmatic rupture occurs most commonly after blunt thoracoabdominal trauma, such as occurs in MVCs or falls from heights, but can also occur from penetrating trauma.61
Anatomy and Pathophysiology
Diaphragmatic hernia is a herniation of abdominal structures within the thoracic cavity through a defect on the diaphragm. Because of pressure gradients across the diaphragm, these injuries are associated with herniation and a potential risk of strangulation of abdominal viscera, especially the small bowel. Signs and symptoms may not occur during the initial admission and may be delayed for as long as months to years.62 In one study, delayed recognition of incarcerated diaphragmatic hernia after stab wounds to the lower chest and upper abdomen was associated with a mortality rate of 36%.63
In cases of blunt injury, the raised pressure within the abdominal cavity causes the tear of the diaphragm, and a pressure difference of generally 5 to 10 mm Hg forces the abdominal organs through the diaphragmatic defect. Because blunt trauma can cause multiple organ injuries, these coexisting injuries can mask the more silent diaphragmatic injuries, and diaphragmatic rupture may be initially overlooked. Over time, negative intrathoracic pressure generated by inspiration tends to draw abdominal contents into the thorax. This effect is lost with the use of intubation and positive-pressure ventilation. Because there is also a plugging effect of the viscera over the defect, migration of the abdominal organs within the thorax is usually delayed, so these injuries are diagnosed in only 10% of cases in the acute phase.63 An overlooked diaphragmatic injury in the acute phase sometimes manifests as respiratory compromise or a hernia with obstruction, incarceration, or perforation of bowel months or decades later.
Diagnostic Strategies
Chest radiography is the first imaging study to determine the presence of diaphragmatic rupture, but a plain chest radiograph immediately after the accident arouses suspicion about the diagnosis of a ruptured diaphragm in only 20 to 34% of cases. CT examination of the abdomen and chest is a very useful and reliable tool in the evaluation of blunt diaphragmatic injury, but the injury site and type affect its sensitivity.64 CT can demonstrate findings consistent with diaphragmatic injury, such as diaphragmatic discontinuity, intrathoracic herniation of abdominal contents, and waistlike constriction of abdominal viscera (the “collar sign”). An isolated omental herniation is clearly detectable on nonenhanced CT because of its fatty nature and crescent shape, and a CT with intravenous contrast will more clearly reveal the contrast-enhancing omental vessels. If the stomach or intestine is herniated, distended intestinal segments containing air-fluid levels are visualized on the supine position images. It is reported that helical CT can be used to detect 78% of left-sided and 50% of right-sided injuries.65 Albeit highly unusual, efflux of peritoneal lavage fluid through a thoracostomy tube is also diagnostic of a diaphragmatic hernia.
Although magnetic resonance imaging is not useful in most traumatic diaphragmatic hernia cases owing to its relatively long duration and increased sensitivity for motion artifact, it is preferred in selected patients, especially in delayed traumatic diaphragmatic herniation cases from small penetrating injuries. In hemodynamically stable patients with penetrating left thoracoabdominal trauma, the incidence of injury to the diaphragm is very high, and thoracoscopy or laparoscopy is recommended for the diagnosis and repair of a diaphragmatic injury.61,66,67 Patients with right-sided small penetrating lesions typically do not experience herniation because of the protective effect of the dome of the liver on the right side.
Management
Diaphragmatic injuries may be a predictor of serious associated injuries in trauma and a marker of severity,4 but they do not ordinarily require urgent repair. The treatment of choice is surgery. CT scan should identify the site and extent of herniation, herniated organs, complications, and damage to associated organs. Although they are not without complications, laparoscopy and thoracoscopy may be used for diaphragmatic hernia repair.
The incidence of diaphragmatic involvement after penetrating left-sided thoracoabdominal injury is high, making nonoperative, expectant management of these patients potentially unsafe. Mandatory evaluation of the diaphragm with laparoscopy to exclude injury in all asymptomatic, hemodynamically normal patients is recommended.68 In the absence of significant hemoperitoneum or other factors preventing adequate visualization of the diaphragm, laparoscopy or thoracoscopy is a sensitive means of excluding occult diaphragmatic injury in these patients. When significant hemoperitoneum is encountered on laparoscopy or other factors are present that prohibit adequate evaluation of the diaphragm, conversion to an open exploration should be considered to fully visualize the diaphragm at risk and exclude additional injuries.
Cardiovascular Trauma
Epidemiology
Blunt cardiac injury usually results from high-speed MVCs in which the chest wall strikes the steering wheel. Other causes, such as falls from heights, crushing injuries, blast injuries, and direct blows, are less common. The significance of blunt injuries as a cause of myocardial or cardiac contusion was described more than 50 years ago by Bright and Beck.69 Nevertheless, the diagnosis of a blunt injury to the heart remains elusive because of the usual concomitant serious injuries to other body organs and, more important, because there is no gold standard for making the diagnosis.
Anatomy and Pathophysiology
Blunt cardiac trauma may be viewed as part of a continuous spectrum (i.e., myocardial concussion, contusion, infarction, and rupture).70 Myocardial concussion occurs when a blunt injury to the interior chest produces a “stun” response in the myocardium. No permanent cellular injury occurs, but transient clinical effects may result. Myocardial contusion is the least severe form of injury that can be demonstrated pathologically. Cellular injury occurs with extravasation of red blood cells into the muscle wall, along with localized myocardial cellular necrosis. Permanent myocardial damage is rare.71 Traumatic myocardial infarction (MI) results from either direct trauma to the coronary arteries or a severe contusion of the myocardium, leading to irreversible cellular injury and ultimately cell death. Direct injury to the coronary arteries via laceration, thrombosis, or spasm is thought to be the most common mechanism for traumatic MI. Cardiac rupture is obviously the most severe form of blunt cardiac injury.
Myocardial Concussion
The term myocardial concussion or commotio cordis is used to describe an acute form of blunt cardiac trauma that is usually produced by a sharp, direct blow to the midanterior chest that stuns the myocardium and results in brief dysrhythmia, hypotension, and loss of consciousness.72 If the patient survives the initial dysrhythmia, there are no lasting or discernible histopathologic changes, and it is difficult to make the definitive diagnosis of myocardial concussion. This presumptively explains those cases of sudden death after a blow to the chest in which no histopathologic changes in the myocardium are demonstrated at autopsy.72
If prolonged cellular dysfunction occurs, it may result in a nonperfusing rhythm, such as asystole or ventricular fibrillation, and irreversible cardiac arrest. There are a number of documented cases of successful resuscitation with rapid provision of CPR and the use of an automated external defibrillator in children who were struck in the chest while playing Little League baseball.73
Myocardial Contusion
Myocardial contusion has been a diagnosis describing a very poorly understood and nebulous condition. Decades of research and widely varied clinical practice have failed to produce a consensus regarding its diagnosis, complication rate, and proper disposition. The incidence of myocardial contusion varies from 3 to 55% in reported series of severe closed-chest trauma, depending on the criteria used for establishing the diagnosis.74,75
Diagnostic Strategies
Significant controversy exists regarding the importance and manner of establishing the diagnosis of myocardial contusion in otherwise hemodynamically stable patients.76
Even when the diagnosis of a myocardial contusion is considered, confirming the diagnosis without a true gold standard is problematic. Clinical evidence is often nonspecific, especially in the setting of multiple trauma. Patients may have dysrhythmias or ST wave changes caused by significant hypoxia as a result of pulmonary injuries or blood loss, which resolve once the hypoxemia or blood loss has been corrected. Likewise, severe intracranial injury, electrolyte abnormalities, and excessive vagal or sympathetic tone may give rise to dysrhythmias or an abnormal ECG. Under these conditions, ECG abnormalities may not represent true myocardial damage. On the contrary, they may cause one to overlook the potential for traumatic cardiac injury. One large series of blunt trauma patients found that blunt cardiac injury was a significant risk factor for cardiac dysrhythmia.76
Because myocardial contusion cannot be positively identified short of biopsy or autopsy, there is much confusion regarding the role of the various laboratory and imaging studies used to diagnose myocardial injury. Multiple studies using cardiac biomarkers have been unhelpful in establishing or excluding the diagnosis. Furthermore, the vast majority of myocardial contusions probably do not cause clinically significant complications. Based on mechanism alone, the relative risk of a life-threatening dysrhythmia is far too low to warrant routine admission to rule out myocardial contusion in all patients with blunt chest trauma. Several studies suggest that very few patients diagnosed with myocardial contusion develop cardiac complications requiring therapeutic intervention or a change in management. Therefore a routine cardiac workup is not indicated in most blunt thoracic trauma victims.77 The usefulness of diagnostic studies is to identify patients at low risk who can be safely discharged from the ED and not to diagnose the presence of a myocardial contusion.
Electrocardiogram.: The ECG after blunt chest trauma may be normal or may show nonspecific abnormalities. Because of its anterior position in the thorax and proximity to the sternum, the right ventricle is far more likely to be injured than the left ventricle. The standard 12-lead ECG is relatively insensitive to right ventricular damage, as demonstrated by pathologic evidence of cellular damage in patients with normal ECGs. A cardiac contusion usually results in moderate right ventricular damage with only minor electrical changes, which can easily be missed on ECG. Right-sided ECGs (the addition of V4R) have not been found to be of any benefit.78
Little is known about the relative risk of dysrhythmia as a function of the ECG abnormality, and any new ECG finding warrants consideration of further diagnostic studies or admission for further monitoring. A severely injured right ventricle may cause a right bundle branch block, usually transient. Less commonly, various degrees of atrioventricular block have been documented after blunt chest trauma. Sinus tachycardia and ventricular and atrial extrasystoles are the most frequently reported rhythm disorders. More serious arrhythmias, such as atrial fibrillation, ventricular tachycardia, and ventricular fibrillation, occur less often but may acutely compromise the hemodynamic state or even result in sudden death.76
A few cases of delayed life-threatening dysrhythmia have been reported up to 12 hours after injury, and patients may develop less lethal dysrhythmias up to 72 hours after injury. The onset of ECG changes may be delayed up to 48 hours after injury, and all ECG changes usually resolve in 4 to 60 days.76 The presence of ECG abnormalities is neither specific enough to confirm the diagnosis of myocardial contusion nor reliable enough to predict subsequent complications.
Cardiac Enzymes.: Because myocardial contusion is histologically characterized by intramyocardial hemorrhage and necrosis of myocardial muscle cells, similar to those seen in acute MI, cardiac enzymes were the first screening tool used to detect myocardial injury. CK is nonspecifically increased in trauma patients owing to associated skeletal muscle injury, and CK-MB levels have also been found to be falsely elevated and therefore are very nonspecific in multitrauma patients. Thus the use of CK-MB levels is of very limited utility in screening for myocardial contusion and is no longer recommended.79–81
Although serum cardiac troponin is highly specific for myocardial injury in the setting of acute MI, elevated troponin levels have been found to have much lower sensitivity for myocardial contusion, and they may occur in the absence of a significant direct myocardial contusion.81 However, such studies are limited because no true gold standard exists to confirm the diagnosis. Several studies have suggested that the combination of a normal troponin level and a normal 12-lead ECG has a negative predictive value to “rule out” myocardial contusion of 100%, suggesting that these patients do not need any other workup or monitoring specific to possible myocardial contusion.81 If there is concern because of nonspecific ECG abnormalities or an elevated troponin level on initial evaluation in the ED, a secondary measurement after 4 to 6 hours should be performed to reliably exclude myocardial injury.80,81
Echocardiography.: Echocardiography provides a means of direct visualization of cardiac structures and chambers. Because contused myocardium resembles infarcted myocardial tissue both histologically and functionally, two-dimensional echocardiography is useful in diagnosing myocardial contusion by evaluating wall motion abnormalities. It is also useful in identifying associated lesions, such as thrombi, pericardial effusion, and valvular disruption. Furthermore, echocardiography offers the practical advantages of being portable, noninvasive, and easy to use at the bedside. If patients have painful chest wall injuries, transthoracic echocardiography may be limited. In these cases, transesophageal echocardiography (TEE) is an alternative.74
Management
The value of admitting and carefully monitoring patients with suspected mild (i.e., hemodynamically asymptomatic) cardiac contusions is not supported. The latest studies do suggest that troponin levels are very helpful in risk stratification of patients suspected of having myocardial contusion.77,80,81 One such strategy is to perform emergent echocardiography for all severely injured patients with hemodynamic instability who are suspected to have structural damage to the heart and/or great vessels. Elevated troponin levels or ECG abnormalities indicate a higher risk of developing cardiac complications. A similar recommendation exists for severely injured patients with a sternal fracture, although the presence of an isolated sternal fracture is not necessarily a sign of cardiac injury. Increased troponin levels or ECG abnormalities indicate a higher risk of developing cardiac complications. Further investigation, including echocardiography, serial ECGs, and serial troponin levels, is recommended.
On admission, treatment of a suspected myocardial contusion should be similar to that of an MI: intravenous line, cardiac monitoring, and administration of oxygen and analgesic agents. Dysrhythmias should be treated with appropriate medications as per current Advanced Cardiac Life Support guidelines.82 No data exist to support prophylactic pharmacologic agents for dysrhythmia suppression. Measures should be taken to treat and prevent any conditions that increase myocardial irritability (e.g., metabolic acidosis). Thrombolytic agents and aspirin are contraindicated in the setting of acute trauma. In rare instances there may be an acute MI associated with trauma, which can arise from lacerations or blunt injury to the coronary arteries. These cases should be managed by percutaneous coronary intervention (PCI), with cardiothoracic surgery for definitive repair as indicated.
Myocardial Rupture
Epidemiology
High-speed MVCs are responsible for most cases of traumatic myocardial rupture. Myocardial rupture is almost always immediately fatal and accounts for 15% of fatal thoracic injuries. It has been estimated that blunt cardiac rupture accounts for 5% of the 50,000 annual highway deaths in the United States.1 In various series, the incidence of cardiac rupture in cases of blunt chest trauma ranges from 0.5 to 2%.83 The most common cause of death in cases of nonpenetrating cardiac injuries is myocardial rupture. Approximately one third of these patients have multiple chamber rupture, and one fourth have an associated ascending aortic rupture. Bright and Beck reviewed 152 autopsy cases of traumatic cardiac ruptures and found that 20% of patients survived 30 minutes or more, which would have allowed them to reach the operating room had the problem been recognized.69 The first report of successful repair of blunt cardiac rupture was published in 1955 and involved a patient with right atrial rupture.84
Anatomy and Pathophysiology
The chambers most commonly involved in cardiac rupture are the ventricles, with right ventricular rupture being most common. Ruptures of the atria are less common, with right atrial rupture being more common than left. Multiple chamber involvement occurs in 20% of patients.83 Twenty percent of nonsurvivors have concomitant aortic rupture.
Because of the nature of the mechanisms involved in cardiac rupture, associated multisystem injuries are common. More than 70% of reported survivors of myocardial rupture have other major associated injuries, including pulmonary contusions, liver and spleen lacerations, closed head injuries, and major fractures. Twenty percent of nonsurvivors have concomitant aortic ruptures.83
Occasionally, patients survive if the pericardial tear is small or the rupture is small enough to seal itself. A small pericardial laceration may allow partial and intermittent release of tamponade while still controlling bleeding. In one series of patients with confirmed myocardial rupture, 40% of patients had isolated rupture of the right atrium. The overall mortality rate was 81%, with none of the patients with two-chamber rupture, ventricular rupture, or absence of vital signs on arrival at the ED surviving.83
Clinical Features
In a review of survivors of myocardial rupture, common symptoms and signs included hypotension (100%); elevated CVP (95%); tachycardia (89%); distended neck veins (80%); cyanosis of the head, neck, arms, and upper chest (76%); unresponsiveness (74%); distant heart sounds (61%); and associated chest injuries (50%).83–86
The following findings are suggestive of pericardial rupture:
1. Hypotension disproportionate to the suspected injury
2. Hypotension unresponsive to rapid fluid resuscitation
3. Massive hemothorax unresponsive to thoracostomy and fluid resuscitation
4. Persistent metabolic acidosis
5. The presence of pericardial effusion on echocardiography or elevation of CVP and neck veins with continuing hypotension despite fluid resuscitation
Diagnostic Strategies
Early use of ED US may facilitate the early diagnosis of cardiac rupture and pericardial tamponade.87 The combination of shock and jugular venous distention (or an elevated CVP) in a patient with blunt chest trauma should immediately suggest pericardial tamponade. However, in patients with coexistent hemorrhage from other injuries, JVD may be absent. Other considerations include tension pneumothorax, right ventricular myocardial contusion, superior vena cava obstruction, and ruptured tricuspid valve. Sonographic visualization of pericardial fluid in this setting should be followed by emergent thoracotomy (Fig. 45-17).
Management
Cardiopulmonary bypass is commonly required in only 10% of successful repairs of myocardial rupture.83 Therefore, for patients with suspected myocardial rupture, it is appropriate to undertake emergency thoracotomy in institutions that have qualified surgeons but no immediate access to cardiopulmonary bypass.
Prognosis
Reported survival rates for patients with myocardial rupture and an intact pericardium vary widely. Although only a small number of survivors of ventricular rupture had been previously reported,81,82,84 a small case series reported that four out of a total of five patients with blunt cardiac rupture who arrived at the ED with vital signs ultimately survived.85 Most survivors of cardiac rupture are patients with atrial rupture, including one patient with multiple atrial tears. Most undergo surgical repair within 3 or 4 hours of injury. Approximately 60% of successful repairs have been performed more than 60 minutes after injury.
Penetrating Cardiac Injury
Penetrating cardiac injuries are one of the leading causes of death in the setting of urban violence. Patients with penetrating cardiac injury who survive to arrive at the hospital have an overall mortality rate of almost 80%.88 Improvements in emergency medical services systems during the past few years, along with an emphasis on rapid transport, are responsible for an increasing number of cardiac injury patients arriving in impending or full cardiopulmonary arrest at busy urban trauma centers. The proportion of gunshot wounds versus stab wounds varies widely in reported case series, depending on the location of the trauma center.
The right ventricle is affected more often (43%) than the left ventricle (34%) owing to its anterior anatomic location. The left or right atrium is affected in 20% of cases.89 One third of penetrating cardiac wounds affect multiple chambers, and survival is much worse in these cases. In 5% of cases, a coronary artery is lacerated, although these injuries usually involve a distal segment of the artery and rarely produce significant acute MI when they are ligated. More proximal coronary artery lacerations require coronary bypass.90 Rarely, the interventricular septum, a valve, papillary muscle, or chordae tendineae are lacerated, producing an acute shunt or valvular insufficiency. These lesions are poorly tolerated and can quickly produce massive pulmonary edema and cardiogenic shock.
Two conditions may occur after penetrating heart injury: (1) exsanguinating hemorrhage if the cardiac lesion communicates freely with the pleural cavity, or (2) cardiac tamponade if the hemorrhage is contained within the pericardium. Patients with exsanguinating wounds frequently die before they reach medical attention, or they have rapidly progressive hemorrhagic shock on presentation, culminating in cardiac arrest. This presentation is most typically seen in patients sustaining gunshot wounds to the heart. Cardiac tamponade is a life-threatening condition but appears to offer some degree of protection and increased survival in patients with penetrating cardiac wounds. These patients often require immediate resuscitation by ED thoracotomy (EDT) if they meet the criteria listed in Box 45-3.
Acute Pericardial Tamponade
The reported incidence of acute pericardial tamponade is approximately 2% in patients with penetrating trauma to the chest and upper abdomen; it is rarely seen after blunt chest trauma. It occurs more commonly with stab wounds than with gunshot wounds, and 60 to 80% of patients with stab wounds involving the heart develop tamponade.89 Patients with acute pericardial tamponade can deteriorate in minutes, but many can be saved if proper steps are taken.
Anatomy and Pathophysiology
The diagnosis of pericardial tamponade should be suspected in any patient who has sustained a penetrating wound or blunt trauma to the thorax or upper abdomen. One is never certain of the trajectory of the bullet or the length, force, and direction of a knife thrust on initial evaluation. Obviously, wounds directly over the precordium and epigastrium are more likely to produce a cardiac injury resulting in tamponade than those in the posterior or lateral thorax. Nevertheless, it is assumed that a penetrating wound, particularly a gunshot wound, anywhere in the thorax or upper abdomen may have injured the heart. Rapid bedside echocardiography, performed as part of the standard FAST examination, easily detects a pericardial effusion causing cardiac tamponade.91,92
Clinical Features
The physical findings of pericardial tamponade are hypotension, distended neck veins, and, rarely, distant or muffled heart tones.93 This so-called Beck’s triad is sometimes difficult to demonstrate clinically, especially in the midst of a major resuscitation with concomitant hypovolemia, when the neck veins may be flat.91 Although the most reliable signs of pericardial tamponade are an elevated CVP (>15 cm H2O) in association with hypotension and tachycardia, bedside echocardiography performed as part of the FAST examination rapidly identifies pericardial tamponade and has largely replaced the use of CVP measurements to make the diagnosis. Echocardiography also distinguishes pericardial tamponade versus tension pneumothorax when the triad of elevated CVP, hypotension, and tachycardia is present.
Diagnostic Strategies
Ultrasound.: US, which is now widely available in EDs throughout the world, enables rapid, accurate, and noninvasive diagnosis of pericardial tamponade.92,94 This study can be performed at the bedside in the ED during the initial resuscitation of the patient as part of the FAST examination. Although the sonographic definition of tamponade is the simultaneous presence of pericardial fluid and diastolic collapse of the right ventricle or atrium, the presence of pericardial fluid in a patient with chest trauma is highly suggestive of pericardial hemorrhage (see Fig. 45-17). An indirect sonographic sign of tamponade is the demonstration of a dilated inferior vena cava in a hypotensive patient. EDs in which cardiac ultrasonography is performed with subcostal and long parasternal views have reported a sensitivity of 98.1% and a specificity of 99.9% for the detection of pericardial effusion.92,93 Because US is noninvasive and extremely accurate, its immediate availability in the initial phase of a major trauma resuscitation can be very helpful in detecting pericardial fluid before the patient deteriorates hemodynamically.
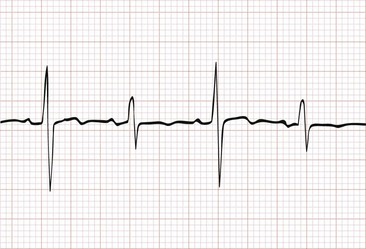
Electrocardiography.: Many ECG changes of pericardial tamponade have been described in the literature, but few are diagnostic, and each is more likely to be seen with chronic rather than acute tamponade. Electrical alternans has been reported to be a highly specific marker of pericardial tamponade. Electrical alternans is an ECG change in which the morphology and amplitude of the P, QRS, and ST-T waves in any single lead alternate in every other beat (Fig. 45-18). The postulated cause is the mechanical oscillation of the heart in the pericardial fluid, which is called the swinging heart phenomenon. In uncomplicated pericardial effusion, the heart swings back and forth but returns to approximately the same position before the next systole. Electrical alternans does not occur in this situation.
Radiography.: The radiographic evaluation of the cardiac silhouette in acute pericardial tamponade generally is not helpful, unless a traumatic pneumopericardium is present. Because small volumes of hemopericardium lead to tamponade in the acute setting, the heart will typically appear normal. This is in contrast to the “water-bottle” appearance of the heart with chronic pericardial effusion. Usually the latter condition is tolerated for a long period.
Management
Out-of-Hospital Care.: Field treatment for cases of pericardial tamponade is essentially the same as that outlined for any victim of major trauma. The diagnosis of tamponade should be suspected by the location of penetrating wounds or by the patient’s poor response to vigorous volume resuscitation. Tension pneumothorax, which is much more common, may mimic certain aspects of acute pericardial tamponade. If the patient is in extremis or the clinical condition rapidly deteriorates, consideration should be given to performing a needle thoracostomy, which, if not therapeutic, suggests pericardial tamponade under the appropriate clinical presentation by virtue of “diagnosis of exclusion.” Expedient transport to the nearest trauma center should be of paramount concern.
Emergency Department.: When the patient arrives in the ED, volume expansion with crystalloid solution via two or three large-bore (14- or 16-gauge) catheters should be established immediately. The presence of a pneumothorax or hemothorax, which is often associated with penetrating cardiac trauma, is treated expeditiously with tube thoracostomy. Bedside echocardiography should be performed as quickly as possible to establish the diagnosis of pericardial tamponade, which then should be followed by emergent surgical repair.
There is increasing controversy regarding the role of pericardiocentesis. In the past, it was recommended that pericardiocentesis be performed for both diagnostic and therapeutic reasons. Aspiration of as little as 5 to 10 mL of blood may result in dramatic clinical improvement. However, it should be emphasized that pericardiocentesis is not a benign or invariably successful procedure. Blood in the pericardial space tends to be clotted, and aspiration may not be possible. Possible complications include the production of pericardial tamponade, the laceration of coronary artery or lung, and induction of cardiac dysrhythmias. Whenever possible, pericardiocentesis should be performed under sonographic guidance because this approach will increase the success rate and decrease the incidence of complications. A pigtail catheter may be introduced into the pericardial space for repeated aspirations while preparations are underway to quickly transport the patient to the operating room for definitive therapy. If pericardiocentesis is unsuccessful or the clinical status deteriorates, and if acute pericardial tamponade remains important in the differential diagnosis, thoracotomy should be performed as quickly as possible.81 Patients with penetrating cardiac injury invariably require surgical repair. The location (operating room vs. ED) and timing (immediate vs. urgent) depend on the patient’s clinical status.
Emergency Department Thoracotomy.: EDT is a drastic, dramatic, and potentially lifesaving procedure in which emergency physicians should be proficient. Although the procedure is not described in detail here, a few technical points merit discussion. A left lateral incision is preferred because it is rapidly accomplished; allows the best exposure of the heart, aorta, and left hilum; and facilitates open cardiac massage and internal defibrillation95 (Fig. 45-19). With right-sided or multiple injuries, it may be necessary to extend the incision across the sternum and right chest wall, creating a “clamshell” incision. The internal mammary arteries need to be ligated if this maneuver restores effective perfusion. After the heart is sufficiently exposed, the pericardium is vertically incised anterior to the phrenic nerve. Release of a tamponade may rapidly restore cardiac output. The heart is then delivered through the pericardium, and penetrating wounds are identified.

Figure 45-19 Emergency department thoracotomy.
There are several alternatives for repairing cardiac wounds. Small wounds can be compressed by digital pressure to control bleeding en route to the operating room. If the injury is quite large, balloon tamponade can be achieved by applying gentle traction on a Foley catheter inserted into the wound with the balloon inflated with saline. This can temporarily stop the hemorrhage to allow suture repair of the injury (cardiorrhaphy) or to gain time while the patient is transferred to the operating room for a more definitive surgical procedure. Lacerations of the atria can be temporarily controlled with a vascular clamp.95
Suture of cardiac wounds over pledgets is the time-honored and effective technique but is technically more difficult and more time-consuming. The use of a monofilament suture, such as 2-0 Prolene, is recommended. Some trauma surgeons recommend stapling cardiac wounds with standard skin staplers because this technique has been shown to be much quicker and equally effective in closing these wounds, and there is also a report on the use of a collagen mesh attached with fibrin glue mesh to rapidly repair a ventricular laceration.96,97
Indications for Emergency Department Thoracotomy.: Although it is often tempting to perform EDT on all traumatic arrest victims in the ED, there are many cases in which patients have virtually no chance of survival.98 In addition, EDT is costly; requires the undivided attention of all personnel in the ED, diverting care from other, more salvageable patients in critical condition; and poses a risk to ED personnel for injury from needle sticks and other blood-contaminated exposures. Consequently, guidelines have been established by the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma (ACSCOT) to withhold EDT or terminate resuscitative efforts on scene.99 These guidelines, along with the most recent Advanced Trauma Life Support text, include withholding EDT for patients in cardiopulmonary arrest secondary to blunt trauma (see Box 45-3).100
However, several recently published case series have questioned whether these guidelines are overly restrictive. One large, multicenter study reported three neurologically intact survivors of EDT who had asystole at ED arrival (all of whom had pericardial tamponade) and five survivors after blunt traumatic arrest who had mild to no neurologic deficits, and another study also reported survivors of EDT who did not meet the traditional survival predictors.101,102 Other authors have noted that some patients who survive EDT may be suitable organ donors.103 Patients with penetrating trauma with signs of life in the field, even if only electrical activity on cardiac monitor or agonal respirations, are candidates for EDT if transport times are less than 10 minutes.102–104
Prognosis
Survival rates after EDT have been correlated with the mechanism and location of injury, field and transport times, the duration of arrest, and the physiologic status of the patient in the out-of-hospital and hospital settings. Although reported survival rates after EDT vary widely, they are consistently higher in victims with isolated cardiac injuries secondary to stab wounds versus gunshot wounds.99–102,104
A meta-analysis of the literature found that EDT had an overall survival rate of 7.4%, with normal neurologic outcomes noted in 92.4% of surviving patients. Survival rates according to mechanism of injury were 9% for penetrating injuries and 1% for blunt injuries. When penetrating injuries were further separated, the survival rates were 17% for stab wounds and 4% for gunshot wounds. The presence of pericardial tamponade is a favorable prognostic finding.105,106
Blunt Aortic Injury
Blunt aortic injury is a life-threatening injury, usually resulting from sudden deceleration, usually from automobile crashes. Other mechanisms of injury include pedestrians struck by automobiles, motorcycle crashes, airplane crashes, and falls from heights.107 In an analysis of automobile crash data, the impact was most often head-on (72%), followed by side impact (24%) and rear impact (4%).108 Despite the improvement in and increased use of restraint systems, the overall incidence of blunt aortic injury associated with fatal automobile crashes has remained unchanged over the past decade.109
Blunt aortic injury includes a spectrum of lesions, ranging from a small intimal tear to frank rupture, which usually cause rapid lethal hemorrhage. The most common sites of injury are the aortic isthmus and the ascending aorta just proximal to the origin of the brachiocephalic vessels.107 Sixty percent to 90% of patients with blunt aortic injury die at the site of accident or within hours of hospital admission.109,110 However, an increasing number of patients arrive at a treatment facility because of improvement in out-of-hospital care, more aggressive resuscitation in the field, and rapid transportation to a trauma center. The early survival rate of such patients depends on the initial resuscitation and/or the timeliness and correct choice of the diagnostic procedures. A rapid and accurate diagnosis is thus mandatory to optimize treatment and maximize patient survival.
Anatomy and Pathophysiology
Blunt aortic injury encompasses various histologic lesions. Minor blunt aortic injuries (grade 1, intramural hematoma or limited intimal flap) and major blunt aortic injuries (grade 2, subadventitial rupture or modification of the geometric shape of the aorta; and grade 3, aortic transection with active bleeding or aortic obstruction with ischemia) can be differentiated by TEE. Whereas minor blunt aortic injuries appear to have a good prognosis, major blunt aortic injuries involve the entire depth of both the intimal and the medial layers and may lead to adventitial rupture, resulting in sudden death at the scene of the accident or during the first hours of hospitalization.111
Rupture of the ascending aorta just distal to the aortic valve likely occurs through a different mechanism. At the time of rapid deceleration and chest compression, the heart is displaced into the left posterior chest, which causes a shearing stress just above the aortic valve. A sudden increase in intra-aortic pressure, “the waterhammer effect,” may also cause an explosive rupture of the aorta at this location. Involvement of the coronary ostia with coronary artery occlusion may occur in association with tears to the ascending arch. The intraluminal pressure tolerance of the aorta may be exceeded in a high-speed motor vehicle crash. It is likely that a combination of the preceding mechanisms accounts for the multiple aortic ruptures that have been found in 20% of traffic accident victims examined at autopsy.109
A total of 80 to 90% of aortic tears occur in the descending aorta at the isthmus, just distal to the left subclavian artery (Fig. 45-20).107,110,111 Less common sites of involvement are the ascending aorta, the distal descending aorta at the level of the diaphragm, the midthoracic descending aorta, and the origin of the left subclavian artery. Although ruptures of the ascending aorta are much less common than those of the descending aorta, they have a 70 to 80% incidence of associated lethal cardiac injuries. This is in contrast to ruptures at the isthmus, which have a 25% incidence of associated cardiac injuries. Lethal cardiac injuries commonly include pericardial tamponade, aortic valve tears, myocardial contusion, or coronary artery injuries. Passenger ejection, pedestrian impact, severe falls, and crush injuries commonly result in ascending thoracic aortic ruptures. Survival long enough to be evaluated in the ED is rare among patients who sustain an ascending aortic rupture.111
Clinical Features
The possibility of aortic disruption is considered in every patient who sustains a severe deceleration injury, because approximately 30% of surviving patients with blunt aortic injury will die within the first 24 hours without treatment.112 This is especially true if the automobile was moving in excess of 45 mph or if there is evidence of severe blunt force to the chest (e.g., from a damaged steering wheel).109 In the case of any moderate- or high-speed motor vehicle accident, it is imperative that paramedics carefully evaluate the extent of damage to the vehicle, the complaints of the victims, and the physical manifestations of blunt chest trauma. This information should be promptly relayed to the emergency physician.
Despite the severe nature of the injury, the clinical manifestations of an aortic rupture are often deceptively meager. Associated pulmonary, neurologic, orthopedic, facial, and abdominal injuries are commonly present. Coexisting injuries can mask the signs and symptoms of an aortic injury or divert the physician’s attention away from the more lethal aortic rupture. The absence of any external evidence of a chest injury does not eliminate the possibility of an aortic tear. One third to one half of patients reported in the literature have no external signs of chest trauma.107,111
Diagnostic Strategies
Chest Radiography.: Radiography of the chest is a valuable tool when aortic rupture is suspected. Many patients have died because the presence and significance of radiographic findings were not appreciated. An increase in the width of the superior mediastinum is the most sensitive sign and is found in 50 to 92% of aortic ruptures (Fig. 45-21).113,114 However, specificity of this radiologic sign is as low as 10%.
Commonly cited guidelines for abnormal mediastinal widening include a mediastinal width greater than 6 cm in the erect posteroanterior film, greater than 8 cm in the supine anteroposterior chest film, or greater than 7.5 cm at the aortic knob or a ratio of mediastinal width to chest width greater than 0.25 at the aortic knob. There is disagreement regarding the reliability of these parameters in confirming or excluding aortic rupture. A subjective interpretation of mediastinal widening is more reliable than direct measurement of mediastinal width.114 Positioning of the patient and the degree of inspiration are important factors in assessing the mediastinum. Every effort should be made to obtain a standard upright inspiratory posteroanterior film, if clinically feasible, before a mediastinum is declared abnormal, to avoid false-positive interpretations.
Current literature is replete with various diagnostic radiologic criteria thought to be sensitive indicators of aortic rupture.115,116 Several authors have shown that an interpretation of widened mediastinum and an obscured aortic knob are the most reliable signs of aortic rupture. The opacification of the clear space between the aorta and the pulmonary artery, displaced nasogastric tube, widened paratracheal stripe, or widened right paraspinal interface is thought to provide the most specific evidence for aortic rupture.113,115,116 Others believe that deviation of the nasogastric tube to the right in combination with depression of the left mainstem bronchus below 40 degrees from the horizontal is the most reliable sign positively associated with the diagnosis.
Although previous reports suggested that a negative chest radiograph is highly predictive of a normal aortogram, several studies have challenged this widely held belief. Between 7 and 44% of patients with blunt aortic injury may have a normal mediastinum on chest radiography117–119; thus the sensitivity of a negative chest radiograph (i.e., normal mediastinum) is limited. These findings have led to the liberal use of helical chest CT scanning in patients with high-speed deceleration mechanisms of injury.118
Chest Computed Tomography Scan.: Chest CT scanning has largely replaced the need for aortography to detect aortic rupture and is now the diagnostic test of choice.120–122 The development of multidetector helical CT scanning in the early 1990s revolutionized trauma radiology with its speed and superior definition, thereby largely negating the negative results obtained with conventional scans. New helical CT scans have almost 100% sensitivity and specificity for rapidly detecting aortic injury while requiring only intravenous contrast administration (Figs. 45-22 and 45-23). A normal aortic contour on CT, even in the presence of a mediastinal hematoma, has been shown to be highly accurate in excluding thoracic aortic disruption (Figs. 45-24 and 45-25).118,119,121
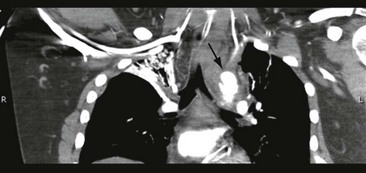
Figure 45-22 Chest computed tomography scan showing aortic intimal tear with surrounding mediastinal hematoma (arrow).
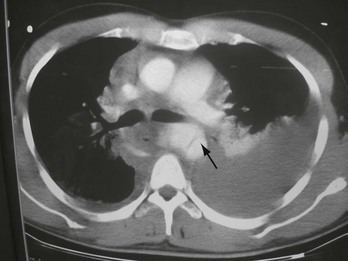
Figure 45-23 Chest computed tomography scan demonstrating periaortic hemorrhage and an intimal flap (arrow).
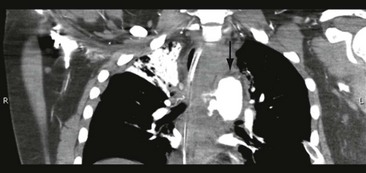
Figure 45-24 Chest computed tomography scan showing aortic injury with active extravasation (arrow).

Figure 45-25 Three-dimensional reconstruction of chest computed tomography scan showing aortic injury (arrow).
A chest CT scan with intravascular contrast offers a number of advantages over aortography. It is noninvasive, provides significantly more information on other thoracic injuries than chest radiography, and can be performed more rapidly than angiography. At most centers, an immediate chest CT scan is readily available. In addition, in the group of patients with a widened mediastinum, CT evaluation may be useful in evaluating not only the aorta but also the spine because spinal fractures may be the cause of a widened mediastinum. It is now recommended that all patients with a mechanism of injury suggestive of potential aortic injury undergo CT evaluation of the mediastinum, irrespective of chest radiographic findings.118
As a result of the improvements in CT scanning technology, more subtle aortic lesions are now being identified, which has led to the term “minimal aortic injury.” A minimal aortic injury is defined as an aortic injury with an intimal flap less than 1 cm, and no or minimal periaortic mediastinal hematoma.123 Up to 10% of patients with blunt aortic injury diagnosed on CT scan may have a minimal aortic injury. It is felt that minimal aortic injuries carry a relatively low risk of rupture. Some centers opt to follow these patients with serial CT scans. If the injury is associated with significant thrombus, periaortic hematoma, lumen encroachment, or pseudoaneurysm, many centers will then proceed to endograft coverage via interventional radiology.123
Transesophageal Echocardiography.: TEE is an alternative method to CT scanning or aortography for establishing the diagnosis of aortic rupture.124–126 It offers a number of advantages over other diagnostic studies: It is fast, does not require intravenous contrast or radiation exposure, provides concomitant evaluation of cardiac function, and can be performed in the ED. Sedation is necessary to avoid hypertension while the probe is inserted. TEE is contraindicated in patients with esophageal injury.
TEE allows identification of an intimal flap, as well as a periaortic hematoma (Fig. 45-26). When only a monoplane TEE is used, the upper portion of the ascending aorta represents a blind zone because of the interposition of the air-filled trachea. However, because the vast majority of injuries are located at the isthmus, TEE is highly accurate, with a reported sensitivity of 87 to 100% and a specificity of 98 to 100%.124–126 When available, TEE offers an alternative to a chest CT scan as a diagnostic screening test for aortic injury.
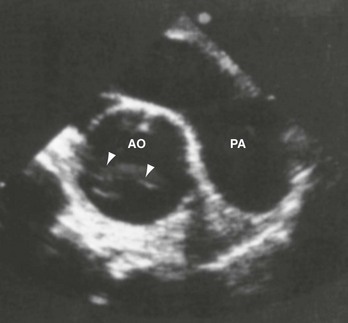
Figure 45-26 Transesophageal echocardiogram shows periaortic hemorrhage and aortic dissection (arrows). AO, aorta; PA, periaortic.
In patients with severe blunt chest trauma, TEE and CT have been found to have similar diagnostic accuracy for the identification of surgical acute traumatic aortic injury. In addition, TEE also allows the diagnosis of associated cardiac injuries and is more sensitive than CT for the identification of intimal or medial lesions of the thoracic aorta.126
Aortic repair may be feasible based on TEE alone, but aortography is still needed when TEE results are equivocal, when TEE is not tolerated or contraindicated, or when other suspected vascular injuries require evaluation by arteriography.111
Intravascular Ultrasound.: Intravascular US has been described in the detection of subtle injuries to the aorta. This modality involves a small US probe that is inserted through the femoral artery and guided up the aorta. Currently, availability is limited to a few trauma centers because the technique requires sophisticated equipment and is performed in the operating room or angiography suite. Preliminary data suggest that intravascular US is extremely sensitive and specific in detecting blunt aortic injury.127,128
Aortography.: Aortography, long considered the gold standard for establishing the diagnosis of aortic disruption, has been replaced almost completely by high-resolution helical CT scanners.129,130 The major objective for patients with a ruptured aorta is the early recognition of the lesion before adventitial disruption and exsanguination. Multiple aortic tears occur in 15 to 20% of cases, necessitating precise anatomic localization of these injuries. Before the widespread availability of helical CT scanners, aortography was recommended not only for patients with a widened mediastinum but also for those who had sustained significant blunt chest trauma and who had any of the radiologic signs previously mentioned. An aggressive approach is particularly warranted in elderly patients.
Aortography should be delayed in patients with more immediate life-threatening injuries to the abdomen, pelvis, and head. In circumstances in which aortography is be delayed, it is important to provide medical management and maintain the systolic blood pressure below 120 mm Hg with antihypertensive agents.128
As surgeons have gained more experience with the diagnostic capabilities of helical CT scanning, the need for preoperative angiography has declined. Aortography should now be reserved for high-risk patients with indeterminate helical chest CT scans.118,130
Management
Out-of-Hospital Management.: In the out-of-hospital care of any patient who has sustained blunt chest trauma, evaluation for possible aortic rupture should concentrate on identifying a mechanism of injury compatible with aortic rupture and treating hypotension, tension pneumothorax, and pericardial tamponade. Immediate communication of the patient’s condition and expeditious transport to a trauma center will increase the patient’s chance for survival.
Emergency Department.: Because of the ever-present risk of sudden free rupture and exsanguination, repair of the lesion should be performed as soon as the diagnosis is made. Management of the patient with multiple injuries who has documented rupture of the thoracic aorta depends on the nature of associated injuries. Surgical repair of the aortic rupture should be delayed in the presence of life-threatening intracranial or intra-abdominal injury or profuse retroperitoneal hemorrhage.118 Consideration for delay of the procedure should be made for patients at high risk for infection (e.g., those who have extensive body surface burns, contaminated large open wounds, established sepsis, or severe respiratory insufficiency caused by thoracic trauma).
Careful regulation of blood pressure is mandatory until definitive surgical repair can be performed. If operative repair is delayed, the systolic blood pressure should be maintained between 100 and 120 mm Hg. The objective of lowering the blood pressure is to decrease the shearing jet effect of an elevated pulse pressure, thus decreasing the possibility of continued adventitial dissection and subsequent free rupture.130
Surgical Techniques
Many surgical techniques have been described since the first successful repair by Passaro and Pace in 1959.131 In those patients who survive operative repair, paraplegia from spinal cord ischemia has been a significant complication, traditionally affecting as many as 10 to 20% of such patients.132,133 The major variable thought to be related to spinal cord ischemia and subsequent development of paraplegia has been aortic cross-clamp times.134 Blunt aortic injury ranges from a simple tear (usually distal to the origin of the subclavian artery) to complex injuries involving the proximal aorta and branch vessels.
Many surgeons have reported the use of cardiopulmonary bypass techniques in surgical repair to allow for distal spinal cord perfusion with significantly reduced incidence of paraplegia.135,136 This is especially true for patients with complex aortic injuries, for which the aortic cross-clamp times are typically prolonged.130
For patients who arrive at the hospital alive but who have descending thoracic aortic injuries, the incidence of mortality during surgery ranges from 20 to 30%, and the paraplegia rate is 5 to 7%.132,135,136 Younger patients have the highest survival rate. Mortality is related to the presence or absence of extensive dissection and to the preoperative condition of the patient.
Endovascular Repair
There is a growing body of evidence demonstrating the safety and efficacy of endovascular repair of traumatic aortic tears.137–141 This involves the use of a stent placed through a femoral or iliac artery approach. Preliminary data indicate that success rates and complication rates are comparable if not better than those of traditional open surgical repairs and that the risk of major surgery and subsequent paraplegia from prolonged aortic clamping is significantly reduced with endovascular repair.142 Emerging literature suggests that endovascular repair with stenting is replacing open repair as the treatment of choice for blunt aortic injury (see Fig. 45-26).143–148
Esophageal Perforation
Perforation of the esophagus has been called the most rapidly fatal perforation of the gastrointestinal tract because death is almost ensured if the diagnosis is delayed more than 24 hours.149 The classic description of esophageal perforation resulting from forceful vomiting was published in 1724 by Boerhaave, and from 1724 to 1941 the occurrence of Boerhaave’s syndrome was almost uniformly fatal.150 In 1941 the first successful surgical treatment, a drainage procedure, was reported, and in 1947 the first successful closure of a ruptured esophagus was described. Since then, improved surgical techniques, a greater physician awareness leading to a more prompt diagnosis, the availability of more effective antibiotics, and better general supportive measures have reduced the mortality to approximately 20%.151 Mortality data cited for perforation are affected by several variables, such as location (with perforations of the thoracic segment having the highest mortality rate), mechanism of injury, time elapsed between injury and diagnosis, the presence of preexisting esophageal disease, and general health of the patient.
Etiology
The most common causes of an esophageal perforation are shown in Box 45-4.
Iatrogenic
Most esophageal perforations are iatrogenic, most commonly as a complication of instrumentation (59% of all patients).152 The rigid endoscope is the most common offender, particularly when general anesthesia is used. Although use of the flexible endoscope has made this complication less likely, the total number of perforations has increased as more procedures are performed. Injuries tend to occur near either the cricopharynx or the cervical esophagus as the endoscope is inserted.152 Endoscopic procedures that are too vigorous in the presence of a corrosive burn or carcinoma are also a common cause of iatrogenic esophageal injury.
Esophageal dilation performed for benign or malignant strictures of the esophagus is the second most common iatrogenic cause of esophageal perforations.153 Increasing the dilator size too rapidly during these procedures may lead to perforation. The preexisting fibrotic process that resulted in the stricture tends to scar the surrounding mediastinal tissues, however, limiting free access to the mediastinum provided by many other perforations. In the ED, nasotracheal or nasogastric intubations are the most common causes of iatrogenic perforation, with the perforation usually occurring in the pyriform sinus. In a closed claims analysis published in 1999, esophageal injuries by anesthesiologists were overwhelmingly associated with difficult intubations.154 Risk factors for a difficult airway include obesity, cervical arthritis, haste, and improper muscle relaxation. Claims involving airways that were classified as “nondifficult” involved other esophageal instrumentation, such as a nasogastric tube, esophageal dilator, or esophageal stethoscope. In all cases, esophageal injuries were more severe than any other type of airway injury sustained during airway maneuvers.
The use of an esophageal obturator airway was also associated with occasional esophageal trauma, specifically midesophageal perforation. Use of the esophageal obturator airway’s successors, the laryngotracheal Combitube and the King airway, do not seem to be associated with trauma more severe than occasional esophageal abrasions or contusions.155
Foreign Bodies
Foreign bodies can cause an esophageal injury by direct laceration, by pressure necrosis, or during endoscopic removal.156 Small perforations tend to seal without sequelae, but pressure necrosis or lacerating injuries provide ample access to the mediastinum.153 Foreign bodies usually lodge in the cervical esophagus, but if a distal stricture is present, this too is a common site. In children younger than 4 years, the cricopharyngeal narrowing is the usual point of foreign body impaction. After age 4 years, most objects pass this region and traverse the remaining normal esophagus. In adults, a foreign body impaction, especially in cases of repeated episodes, raises the possibility of a stricture and warrants further investigation.
In elderly patients, foreign bodies commonly enter the esophagus because of a loss of oral tactile sensation resulting from intoxication or a poorly fitting set of dentures.152 Inadequate dentures may also lead to the swallowing of large pieces of poorly chewed food. Other esophageal foreign bodies include sharp fish or chicken bones and corn chips that may impale the esophageal wall leading to eventual leakage.
Caustic Burns
Caustic burns of the esophagus occur from intentional or accidental ingestion of acid or alkali. There are two peaks of incidence: 1 to 5 years of age, when ingestion is usually of a small amount of material and accidental, and in the teens and 20s, when larger quantities are ingested during suicide attempts. Symptoms include hematemesis, respiratory distress, vomiting, drooling, or the presence of oropharyngeal lesions on physical examination.157 Perforation usually occurs during the latent granulation stage of the disease, approximately 4 to 14 days after ingestion.
The liquefaction necrosis classically resulting from strong alkali burns (pH >12) is more likely to cause esophageal perforation than the coagulation necrosis resulting from strong acid burns (pH <2). Individuals ingesting alkali substances with a pH less than 11.5 rarely sustain injuries more serious than superficial mucosal burns. Acid ingestions cause damage more frequently in the stomach than in the esophagus.157
In treating a patient who has ingested a caustic substance, decontamination should involve only the rinsing of the mouth. Dilution of the substance with milk or water has been suggested; however, further liquid ingestion should be avoided if there is suspicion of perforation. Emesis, gastric lavage, and charcoal should be avoided.154
Endoscopy within the first 6 to 18 hours may be used to determine the extent of the injury and to guide therapy. Antibiotics are reserved for patients with evidence of perforation, and steroids are suggested by some authors if the burns are circumferential or transmural. Other authors have shown that in the setting of large alkali ingestions, corticosteroids not only did not prevent the formation of esophageal stenosis but also increased the risk of other complications.157
Although admission after significant ingestion is the rule, some authors suggest that in the setting of accidental ingestion in children and in the absence of symptoms, endoscopy and admission may not be indicated.158,159 Esophagoscopy is commonly undertaken to ascertain the presence or absence of esophageal injury. Advancing the esophagoscope beyond the first burn in the esophagus increases the risk of perforation and is a common iatrogenic cause of esophageal perforation.
Penetrating and Blunt Trauma
Because of its well-protected position posteriorly, esophageal trauma occurs in approximately 5% of patients with injuries to the neck, but only 1% of blunt trauma victims, and it is usually not an isolated injury.152 Cervical esophageal injuries are the most common because of a lack of protection by the bony thorax, and the trachea is the most common associated site of injury.152 In some cases, the esophageal injury may be overlooked initially because of the dramatic presentation of a patient with a tracheal injury.
Typical symptoms seen in cervical esophageal injuries include neck pain, dysphagia, cough, voice changes, and hematemesis. Physical findings may include neck tenderness, resistance to flexion, crepitus, or stridor.152,158 In one large series, the most common life-threatening problem in the ED was compromise of the airway. Most of these cases were handled with rapid sequence intubation, but a significant number (12%) of patients required cricothyroidotomy.152
If the patient’s condition is stable, a preoperative esophagogram with a water-soluble agent should precede any endoscopy. Although chest and neck radiograph and CT also may be used to diagnose this injury, emergent bedside flexible endoscopy seems to be the test of choice to confirm negative findings on esophagography (especially in the setting of penetrating trauma).160 Operative repair is indicated in most of these injuries (>90%) and should be done as quickly as possible to avoid the development of fistulae, mediastinitis, or abscess formation.158
Blunt traumatic injuries to the esophagus occur much less often than penetrating injuries. The pathophysiology and prognosis of blunt injuries to the esophagus are similar to those of spontaneous rupture or emesis. In some cases, rupture of the cervical esophagus has been reported in association with cervical spine fracture.161
Spontaneous Rupture
In vitro, a tear similar to that seen in cases of Boerhaave’s syndrome requires a force of 3 to 6 psi, which may be generated in vivo by gastric pressure caused by the reverse peristalsis (seen with emesis) pushing against a closed cricopharyngeal muscle. The role of preexisting gastrointestinal disease in spontaneous rupture of the esophagus is unclear. Some authors emphasize its importance, whereas others report that 80% of esophageal ruptures occur in a previously normal esophagus.160 Less pressure is required to perforate a diseased esophagus. Approximately 25% of patients with Boerhaave’s syndrome have no history of emesis.152 Increases in intra-abdominal pressure resulting from blunt trauma, seizures, childbirth, laughing, straining at stool, and heavy lifting have all been reported to cause this injury.
Diagnostic Findings
The diagnosis of esophageal perforation is aided by consideration of clinical circumstances. In patients with classic Boerhaave’s syndrome, emesis is followed by severe chest pain, subcutaneous emphysema, and cardiopulmonary collapse. Development of these signs and symptoms after instrumentation of the esophagus or removal of an esophageal foreign body is relatively straightforward. One third of cases of perforated esophagus are atypical, however. Only a careful history and physical examination supplemented by appropriate laboratory and diagnostic studies enable the clinician to diagnose a subtle case at an early stage. In considering any of the diagnoses listed in Box 45-5, a perforated esophagus should also be considered.
Clinical Features
The most reliable symptom of an esophageal injury is pleuritic pain localized along the course of the esophagus that is exacerbated by swallowing or neck flexion (Fig. 45-27). Pain may be located in the epigastrium, substernal area, or back; usually worsens over time; and may migrate from the upper abdomen to the chest. As the infectious process worsens, dyspnea usually ensues.
The early physical signs of an esophageal perforation are sparse. As air and caustic contaminated material move through the esophageal tear into the mediastinum and pleural space, and before any subcutaneous air is palpable at the root of the neck, the mediastinal air may impart a nasal quality to the voice. Mediastinal air may surround the heart and produce a systolic crunching sound (Hamman’s crunch). As air and fluid move into the pleural space, signs of a hydropneumothorax or an empyema may develop. Eventually the air travels into the subcutaneous tissues, dissecting into the neck, where subcutaneous emphysema may first become evident. This classic sign is present in only approximately 60% of patients, however, and in the absence of a tracheal injury, it may occur in only 30%.162 As the infectious and inflammatory process advances, the patient’s general appearance and vital signs begin to manifest the signs of cardiopulmonary collapse and sepsis with fever, cyanosis, hypotension, anuria, and eventually death.
Diagnostic Strategies
Lateral views of the cervical spine may reveal air or fluid in the retropharyngeal area that is characteristic of a cervical esophageal perforation but also is found when perforations in the lower parts of the esophagus release air or fluid that dissects superiorly (Fig. 45-28). Most patients exhibit one or more of these abnormalities at some point in the course of the illness, but radiographic evidence of the perforation may be absent early.
Endoscopy, similar to contrast studies, is not an infallible aid in establishing the presence or absence of an esophageal perforation. The size and location of the perforation and the skill of the endoscopist are important factors in the low incidence of false-negative studies.164 If the accuracy of the endoscopy is in doubt, an esophagogram should be performed. Helical CT with dilute oral contrast has been reported as a safer, faster, and less manpower-intensive diagnostic examination.165 Some of the abnormalities that may be seen on CT scan include extraluminal air, periesophageal fluid, esophageal thickening, and extraluminal contrast. These CT findings may be the first clue to the correct diagnosis of esophageal perforation.
Management
Early diagnosis can best be accomplished if one is aware of the pathophysiology and clinical settings in which esophageal perforations occur. Time is crucial in minimizing the mortality and morbidity of this condition. If the diagnosis is strongly suggested or confirmed, management should include broad-spectrum antibiotics (covering oral flora), volume replacement, and airway maintenance.163–165 An emergency surgical consultation should be obtained because prognosis worsens as time passes, with mortality almost doubling in the first 12 hours.
Although operative therapy is standard, nonoperative therapy is an option for patients with well-contained perforations, with minimal mediastinal involvement, and without evidence of sepsis.165 In such cases the patient is placed on nothing-by-mouth (NPO) status for at least 72 hours, broad-spectrum antibiotics are initiated, and usually total parenteral nutrition treatment is begun. The use of nasogastric tubes should be discouraged because they may increase gastroesophageal reflux and worsen the contamination of the mediastinum.164,165
References
1. Khandhar, SJ, Johnson, SB, Calhoon, JH. Overview of thoracic trauma in the United States. Thorac Surg Clin. 2007;17:1.
2. Brenner, DJ, Hall, EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277.
3. Shweiki, E, Klena, J, Wood, GC, Indeck, M. Assessing the true risk of abdominal solid organ injury in hospitalized rib fracture patients. J Trauma. 2001;48:684.
4. Bergeron, E, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478.
5. Holcomb, JB, McMullin, NR, Kozar, RA, Lygas, MH, Moore, FA. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549.
6. Brasel, KJ, Guse, CE, Layde, P, Weigelt, JA. Rib fractures: Relationship with pneumonia and mortality. Crit Care Med. 2006;34:1642.
7. Traub, M, et al. The use of chest computed tomography versus chest x-ray in patients with major blunt trauma. Injury. 2007;38:43.
8. Sirmali, M, et al. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24:133.
9. Todd, SR, et al. A multidisciplinary clinical pathway decreases rib fracture-associated infectious morbidity and mortality in high-risk trauma patients. Am J Surg. 2006;192:806.
10. Simon, BJ, Chu, Q, Emhoff, TA, Fiallo, VM, Lee, KF. Delayed hemothorax after blunt thoracic trauma: An uncommon entity with significant morbidity. J Trauma. 1998;45:673.
11. Knobloch, K, et al. Sternal fractures occur most often in old cars to seat-belted drivers without any airbag often with concomitant spinal injuries: Clinical findings and technical collision variables among 42,055 crash victims. Ann Thorac Surg. 2006;82:444.
12. Brookes, JG, Dunn, RJ, Rogers, LR. Sternal fractures: A retrospective analysis of 272 cases. J Trauma. 1993;35:46.
13. You, JS, Chung, YE, Kim, D, Park, S, Chung, SP. Role of sonography in the emergency room to diagnose sternal fractures. J Clin Ultrasound. 2010;38:135–137.
14. Kehdy, F, Richardson, JD. The utility of 3-D CT scan in the diagnosis and evaluation of sternal fractures. J Trauma. 2006;60:635.
15. Richardson, JD, Franklin, GA, Heffley, S, Seligson, D. Operative fixation of chest wall fractures: An underused procedure? Am Surg. 2007;73:591.
16. Xirouchaki, N, et al. Noninvasive bilevel positive pressure ventilation in patients with blunt thoracic trauma. Respiration. 2005;72:517.
17. Pettiford, BL, Luketich, JD, Landreneau, RJ. The management of flail chest. Thorac Surg Clin. 2007;17:25.
18. Gunduz, M, Unlugenc, H, Ozalevli, M, Inanoglu, K, Akman, H. A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 2005;22:325–329.
19. Lafferty, PM, Anavian, J, Will, RE, Cole, PA. Operative treatment of chest wall injuries: Indications, technique, and outcomes. J Bone Joint Surg Am. 2011;93:97–110.
20. Borman, JB, Aharonson-Daniel, L, Savitsky, B, Peleg, K, Israeli Trauma Group. Unilateral flail chest is seldom a lethal injury. Emerg Med J. 2006;23:903.
21. Eckstein, M, Cowen, AR. Scene safety in the face of automatic weapons fire: A new dilemma for EMS? Prehosp Emerg Care. 1998;2:117.
22. de Brito, D, Challoner, KR, Sehgal, A, Mallon, W. The injury pattern of a new law enforcement weapon: The police bean bag. Ann Emerg Med. 2001;38:383.
23. Olivas, T, Jones, B, Canulla, M. Abdominal wall penetration by a police “bean bag.”. Am Surg. 2001;67:407–409.
24. Byard, RW, Wick, R, Simpson, E, Gilbert, JD. The pathological features and circumstances of death of lethal crush/traumatic asphyxia in adults—a 25-year study. Forensic Sci Int. 2006;159:200.
25. Balci, AE, et al. Blunt thoracic trauma in children: Review of 137 cases. Eur J Cardiothorac Surg. 2004;26:387.
26. Morgagni, JB. Epistola. 1761;54:140.
27. Wanek, S, Mayberry, JC. Blunt thoracic trauma: Flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20:71.
28. Kwon, A, et al. Isolated computed tomography diagnosis of pulmonary contusion does not correlate with increased morbidity. J Pediatr Surg. 2006;41:78.
29. Cohn, SM, Dubose, JJ. Pulmonary contusion: An update on recent advances in clinical management. World J Surg. 2011;34:1959–1970.
30. Adoumie, R, Shennib, H, Brown, R, Slinger, P, Chiu, RC. Differential lung ventilation. J Thorac Cardiovasc Surg. 1993;105:229.
31. Deunk, J, et al. The clinical outcome of occult pulmonary contusion on multidetector-row computed tomography in blunt trauma patients. J Trauma. 2010;68:387–394.
32. Hamrick, MC, Duhn, RD, Ochsner, MG. Critical evaluation of pulmonary contusion in the early post-traumatic period: Risk of assisted ventilation. Am Surg. 2009;75:1054–1058.
33. Mielck, F, Quintel, M. Extracorporeal membrane oxygenation. Curr Opin Crit Care. 2005;11:87.
34. Kirkpatrick, AW, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: The Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma. 2004;57:288.
35. Blaivas, M, Lyon, M, Duggal, S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12:844.
36. Volpicelli, G. Sonographic diagnosis of pneumothorax. Intensive Care Med. 2011;37:224–232.
37. Hill, SL, Edmisten, T, Holtzman, G, Wright, A. The occult pneumothorax: An increasing diagnostic entity in trauma. Am Surg. 1999;65:254–258.
38. Ball, CG. 2005 Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J Trauma. 2005;59:917–924.
39. Neff, MA, Monk, JS, Jr., Peters, K, Nikhilesh, A. Detection of occult pneumothoraces on abdominal computed tomographic scans in trauma patients. J Trauma. 2000;49:281.
40. Kiev, J, Kerstein, MD. Role of three hour roentgenogram of the chest in penetrating and non-penetrating injuries. Surg Gynecol Obstet. 1992;175:249.
41. Magnotti, LJ, et al. Initial chest CT obviates the need for repeat chest radiograph after penetrating thoracic trauma. Am Surg. 2007;73:569.
42. McGillicudy, D, Rosen, P. Diagnostic dilemmas and current controversies in chest trauma. Emerg Med Clin North Am. 2007;25:695.
43. Yadav, K, Jalili, M, Zehtabchi, S. Management of traumatic occult pneumothorax. Resuscitation. 2010;81:1063–1068.
44. Mowery, NT, et al. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011;70:510–518.
45. Sethuraman, KN, et al. Complications of tube thoracostomy placement in the emergency department. J Emerg Med. 2011;40:14–20.
46. Givens, ML, Ayotte, K, Manifold, C. Needle thoracostomy: Implications of computed tomography chest wall thickness. Acad Emerg Med. 2004;11:211–213.
47. Inaba, K, et al. Optimal positioning for emergent needle thoracostomy: A cadaver-based study. J Trauma. 2011;71:1099–1103.
48. Luchette, FA, et al. Practice management guidelines for prophylactic antibiotic use in tube thoracostomy for traumatic hemopneumothorax: The EAST Practice Management Guidelines Work Group. Eastern Association for Trauma. J Trauma. 2000;48:753.
49. Eckstein, M, Suyehara, D. Needle thoracostomy in the prehospital setting. Prehosp Emerg Care. 1998;2:132.
50. Meyer, DM. Hemothorax related to trauma. Thorac Surg Clin. 2007;7:47.
51. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons Committee on Trauma. Practice management guidelines for emergency department thoracotomy. J Am Coll Surg. 2001;193:303.
52. Stafford, RE, Linn, J, Washington, L. Incidence and management of occult hemothoraces. Am J Surg. 2006;192:722.
53. Landay, M, et al. Lung penetration by thoracostomy tubes: Imaging findings on CT. J Thoracic Imaging. 2006;21:197.
54. Casos, SR, Richardson, JD. Role of thoracoscopy in acute management of chest injury. Curr Opin Crit Care. 2006;12:584.
55. Paci, M, et al. The role of diagnostic VATS in penetrating thoracic injuries. World J Emerg Surg. 2006;1:3.
56. Manlulu, AV, Lee, TW, Thung, KH, Wong, R, Yim, AP. Current indications and results of VATS in the evaluation and management of hemodynamically stable thoracic injuries. Eur J Cardiothorac Surg. 2004;25:1048.
57. Kiser, AC, O’Brien, SM, Detterbeck, FC. Blunt tracheobronchial injuries: Treatment and outcomes. Ann Thorac Surg. 2001;71:2059.
58. Balci, AE, Eren, N, Eren, S, Ulku, R. Surgical treatment of post-traumatic tracheobronchial injuries: 14-year experience. Eur J Cardiothorac Surg. 2002;22:984.
59. Gómez-Caro, A, et al. Role of conservative medical management of tracheobronchial injuries. J Trauma. 2006;61:1426.
60. Scaglione, M, et al. Acute tracheobronchial injuries: Impact of imaging on diagnosis and management implications. Eur J Radiol. 2006;59:336.
61. Hanna, WC, Ferri, LE. Acute traumatic diaphragmatic injury. Thoracic Surg Clin. 2009;19:485–489.
62. Leppaniemi, A, Haapiainen, R. Occult diaphragmatic injuries caused by stab wounds. J Trauma. 2003;55:646.
63. Reber, PU, et al. Missed diaphragmatic injuries and their long term sequelae. J Trauma. 1998;44:183.
64. Eren, S, Kantarci, M, Okur, A. Imaging of diaphragmatic rupture after trauma. Clin Radiol. 2006;61:467.
65. Sadeghi, N, Nicaise, N, DeBacker, D, Struyven, J, Van Gansbeke, D. Right diaphragmatic rupture and hepatic hernia: An indirect sign on computed tomography. Eur J Radiol. 1999;9:972.
66. Madden, MR, et al. Occult diaphragmatic injury from stab wounds to the lower chest and abdomen. J Trauma. 1989;29:292.
67. Murray, JA, et al. Occult injuries to the diaphragm: Prospective evaluation of laparoscopy in penetrating injuries to the left lower chest. J Am Coll Surg. 1998;187:626.
68. Friese, RS, Coln, EC, Gentilello, LM. Laparoscopy is sufficient to exclude occult diaphragm injury after penetrating abdominal trauma. J Trauma. 2005;58:789.
69. Bright, EF, Beck, CS. Nonpenetrating wounds of the heart: A clinical and experimental study. Am Heart J. 1935;10:293.
70. Rudusky, BM. Classification of myocardial contusion and blunt cardiac trauma. Angiology. 2007;57:610.
71. Koehler, SA, et al. Cardiac concussion: Definition, differential diagnosis, and cases presentation and the legal ramification of a misdiagnosis. Am J Forensic Med. 2004;25:205.
72. Maron, BJ, Gohman, TE, Kyle, SB, Estes, NA, 3rd., Link, MS. Clinical profile and spectrum of commotio cordis. JAMA. 2002;287:1142.
73. Elie, MC. Blunt cardiac injury. Mount Sinai J Med. 2006;73:542.
74. Sybrandy, KC, Cramer, MJ, Burgersdijk, C. Diagnosing cardiac contusion: Old wisdom and new insights. Heart. 2003;89:485.
75. Lindstaedt, M, et al. Acute and long-term clinical significance of myocardial contusion following blunt thoracic trauma: Results of a prospective study. J Trauma. 2002;52:479.
76. Ismailov, RM, Ness, RB, Redmond, CK, Talbott, EO, Weiss, HB. Trauma associated with cardiac dysrhythmias: Results from a large matched case-control study. J Trauma. 2007;62:1186.
77. Nagy, KK, et al. Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. World J Surg. 2001;25:108.
78. Walsh, P, et al. Use of V4R in patients who sustain blunt chest trauma. J Trauma. 2001;51:60.
79. Swaanenburg, JC, Klaase, JM, DeJongste, MJ, Zimmerman, KW, ten Duis, HJi. Troponin I, troponin T, CKMB-activity and CKMB-mass as markers for the detection of myocardial contusion in patients who experienced blunt trauma. Clin Chim Acta. 1998;272:171.
80. Edouard, AR, et al. Incidence and significance of cardiac troponin I release in severe trauma patients. Anesthesiology. 2004;101:1262.
81. Velmahos, GC, et al. Normal electrocardiography and serum troponin I levels preclude the presence of clinically significant blunt cardiac injury. J Trauma. 2003;54:45.
82. American Heart Association. 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Chicago: American Heart Association; 2010.
83. Brathwaite, CE, Rodriguez, A, Turney, SZ, Dunham, CM, Cowley, R. Blunt traumatic cardiac rupture: A 5-year experience. Ann Surg. 1990;212:701.
84. DesForges, G, Ridder, WP, Lenoci, RJ. Successful suture of ruptured myocardium after nonpenetrating injury. N Engl J Med. 1955;252:567.
85. Lu, LH, et al. Blunt cardiac rupture with prehospital pulseless electrical activity: A rare successful experience. J Trauma. 2005;59:1489.
86. Namai, A, Sakurai, M, Fujiwara, H. Five cases of blunt traumatic cardiac rupture: Success and failure in surgical management. Gen Thorac Cardiovasc Surg. 2007;5:200.
87. Teixeira, PG, et al. Blunt cardiac rupture: A 5-year NTDB analysis. J Trauma. 2009;67:788–791.
88. O’Connor, J, Ditillo, M, Scalea, T. Penetrating cardiac injury. J R Army Med Corps. 2009;155:185–190.
89. Asensio, JA, et al. One hundred five penetrating cardiac injuries: A 2-year prospective evaluation. J Trauma. 1998;44:1073.
90. Asensio, JA, et al. Penetrating thoracoabdominal injuries: Ongoing dilemma—which cavity and when? World J Surg. 2002;26:539.
91. Kirkpatrick, AW, Ball, CG, D’Amours, SK. Acute resuscitation of the unstable adult trauma patient: Bedside diagnosis and therapy. Can J Surg. 2008;51:57.
92. Ma, OJ, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38:879.
93. Beck, CS. Acute and chronic compression of the heart. Am Heart J. 1937;14:515.
94. Ciccone, TJ, Grossman, SA. Cardiac ultrasound. Emerg Med Clin North Am. 2004;22:621.
95. Asensio, JA, et al. Penetrating cardiac injuries. Surg Clin North Am. 1996;76:685.
96. Toda, K, Yoshitatsu, M, Izutani, H, Ihara, K. Surgical management of penetrating cardiac injuries using a fibrin glue sheet. Interact Cardiovasc Thorac Surg. 2007;6:577.
97. Evans, BJ, Homick, P. Use of a skin stapler to repair penetrating cardiac injury. Ann R Coll Surg Engl. 2006;88:413.
98. Eckstein, M. Termination of resuscitative efforts: Medical futility for the trauma patient. Curr Opin Crit Care. 2001;7:450.
99. Hopson, LR, et al. Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest. J Am Coll Surg. 2003;196:475–481.
100. Kortbeek, JB, et al. Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008;6:1638–1650.
101. Moore, EE, et al. Defining the limits of resuscitative emergency department thoracotomy: A contemporary Western Trauma Association perspective. J Trauma. 2011;70:334–339.
102. Seamon, MJ, et al. Emergency department thoracotomy: Survival of the least expected. World J Surg. 2008;32:604–612.
103. Schnuriger, B, et al. Organ donation: An important outcome after resuscitative thoracotomy. J Am Coll Surg. 2010;211:450–455.
104. Stratton, SJ, Brikett, K, Crammer, T. Prehospital pulseless, unconscious penetrating trauma victims: Field assessments associated with survival. J Trauma. 1998;45:96.
105. Rhee, PM, et al. Survival after emergency department thoracotomy: Review of published data from the past 25 years. J Am Coll Surg. 2000;190:288.
106. Soreide, K, Petrone, P, Asensio, JA. Emergency thoracotomy in trauma: Rationale, risks, and realities. Scand J Surg. 2007;96:4.
107. Parmley, LF, Mattingly, TW, Manion, WC, Jahnke, EJ, Jr. Nonpenetrating traumatic injury of the aorta. Circulation. 1958;17:1086.
108. Fabian, TC, et al. Prospective study of blunt aortic injury: Multicenter trial of the American Association for the Surgery of Trauma. J Trauma. 1997;42:374.
109. Schulman, CI, et al. Incidence and crash mechanisms of aortic injury during the past decade. J Trauma. 2007;62:664.
110. Conroy, C, et al. Motor vehicle-related cardiac and aortic injuries differ from other thoracic injuries. J Trauma. 2007;62:1462.
111. Neschis, DG, Scalea, TM, Flinn, WR, Griffith, BP. Blunt aortic injury. N Engl J Med. 2008;359:1708–1716.
112. Duwayri, Y, Abbas, J, Cerilli, G, Chan, E, Nazzal, M. Outcome after thoracic aortic injury: Experience in a level-1 trauma center. Ann Vasc Surg. 2008;22:309.
113. Lee, FT, Jr., et al. Reevaluation of plain radiographic findings in the diagnosis of aortic rupture: The role of inspiration and positioning on mediastinal width. J Emerg Med. 1993;11:289.
114. Woodring, JH, King, JG. Determination of normal transverse mediastinal width and mediastinal-width to chest-width ratio in control subjects. J Trauma. 1989;29:1268.
115. Mirvis, SE, et al. Value of chest radiography in excluding traumatic aortic rupture. Radiology. 1987;163:47.
116. Heystraten, FM, et al. Chest radiography in acute traumatic rupture of the thoracic aorta. Acta Radiol. 1988;29:411.
117. Demetriades, D, et al. Routine helical computed tomographic evaluation of the mediastinum in high-risk blunt trauma patients. Arch Surg. 1998;133:1084.
118. Nagy, K, et al. Guidelines for the diagnosis and management of blunt aortic injury: An EAST Practice Management Guidelines Work Group. J Trauma. 2000;48:1128.
119. Bruckner, BA, et al. Critical evaluation of chest computed tomography scans for blunt descending thoracic aortic injury. Ann Thorac Surg. 2006;81:1339.
120. Plurad, D, Green, D, Demetriades, D, Rhee, P. The increasing use of chest computed tomography for trauma: Is it being overutilized? J Trauma. 2007;62:631–635.
121. Chen, MY, et al. The trend of using computed tomography in the detection of acute thoracic aortic and branch vessel injury after blunt thoracic trauma: Single-center experience over 13 years. J Trauma. 2004;56:783.
122. Melton, SM, et al. The evolution of chest computed tomography for the definitive diagnosis of blunt aortic injury: A single-center experience. J Trauma. 2004;56:243.
123. Malhotra, AK, et al. Minimal aortic injury: A lesion associated with advancing diagnostic techniques. J Trauma. 2001;51:1042.
124. Goarin, JP, et al. Evaluation of transesophageal echocardiography for diagnosis of traumatic aortic injury. Anesthesiology. 2000;93:1373.
125. Cinnella, G, Dambrosio, M, Brienza, N, Tullo, L, Fiore, T. Transesophageal echocardiography for diagnosis of traumatic aortic injury: An appraisal of the evidence. J Trauma. 2004;57:1246.
126. Vignon, P, et al. Comparison of multiplane transesophageal echocardiography and contrast-enhanced helical CT in the diagnosis of blunt traumatic cardiovascular injuries. Anesthesiology. 2001;94:615.
127. Patel, NH, Hahn, D, Comess, KA. Blunt chest trauma victims: Role of intravascular ultrasound and transesophageal echocardiography. J Trauma. 2003;55:330.
128. Azizzadeh, A, et al. The utility of intravascular ultrasound compared to angiography in the diagnosis of blunt aortic injury. J Vasc Surg. 2011;53:608–619.
129. Fishman, JE. Imaging of blunt aortic and great vessel trauma. J Thorac Imaging. 2000;15:97.
130. Fabian, TC, et al. Prospective study of blunt aortic injury: Helical CT is diagnostic and antihypertensive therapy reduces rupture. Ann Surg. 1998;227:666.
131. Passaro, E, Jr., Pace, WC. Traumatic rupture of the aorta. Surgery. 1959;46:787.
132. Miller, PR, et al. Complex blunt aortic injury or repair: Beneficial effects of cardiopulmonary bypass use. Ann Surg. 2003;237:877.
133. Carter, Y, et al. Anatomical considerations in the surgical management of blunt thoracic aortic injury. J Vasc Surg. 2001;34:628.
134. Nzewi, O, Slight, RD, Zamvar, V. Management of blunt thoracic aortic injury. Eur J Vasc Endovasc Surg. 2006;31:18–27.
135. Whitson, BA, Nath, DS, Knudtson, JR, McGonigal, MD, Shumway, SJ. Is distal aortic perfusion in traumatic thoracic aortic injuries necessary to avoid paraplegic postoperative outcomes? J Trauma. 2008;64:115.
136. Crestanello, JA, et al. The effect of perfusion techniques on the incidence of paraplegia after the repair of traumatic thoracic aortic transections. Mayo Clin Proc. 2006;81:625.
137. Agostinelli, A, et al. Immediate endovascular treatment of blunt aortic injury: Our therapeutic strategy. J Thorac Cardiovasc Surg. 2006;131:1053.
138. Kasirajan, K, Hefferman, D, Langsfeld, M. Acute thoracic aortic trauma: A comparison of endoluminal stent grafts with open repair and nonoperative management. Ann Vasc Surg. 2003;17:589.
139. Orford, VP, et al. Blunt traumatic aortic transection: The endovascular experience. Ann Thorac Surg. 2003;75:106.
140. Dunham, MB, et al. Endovascular stent grafts for acute blunt aortic injury. J Trauma. 2004;56:1173.
141. Kato, M, Yatsu, S, Sato, H, Kyo, S. Endovascular stent-graft treatment for blunt aortic injury. Circ J. 2004;68:553.
142. Bent, CL, et al. Endovascular management of acute blunt traumatic thoracic aortic injury: A single center experience. J Vasc Surg. 2007;46:920.
143. Riesenman, PJ, et al. Outcomes of surgical and endovascular treatment of acute traumatic thoracic aortic injury. J Vasc Surg. 2007;46:934.
144. Patel, HJ, Hemmila, MR, Williams, DM, Diener, AC, Deeb, GM. Late outcomes following open and endovascular repair of blunt thoracic aortic injury. J Vasc Surg. 2011;53:615–621.
145. Starnes, BW. Treating blunt aortic injuries with endografts: Pros and cons of a meta-analysis. Semin Vasc Surg. 2010;23:176–181.
146. Propper, BW, Clouse, WD. Thoracic aortic endografting for trauma: A current appraisal. Arch Surg. 2010;145:1006–1011.
147. Neschis, DG, Scalea, TM. Endovascular repair of traumatic aortic injuries. Adv Surg. 2010;44:281–292.
148. Barnard, J, Humphreys, J, Bittar, MN. Endovascular versus open surgical repair for blunt thoracic aortic injury. Interact Cardiovasc Thorac Surg. 2009;9:506–509.
149. Brinster, CJ, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004;77:1475.
150. Derbes, VS, Mitchell, RE, Jr. Hermann Boerhaave’s Atrocis, nec descripti prius, morbi historia, the first translation of the classic case report of rupture of the esophagus, with annotations. Bull Med Libr Assoc. 1944;43:217.
151. Wang, HE, Mann, NC, Mears, G, Jacobson, K, Yealy, DM. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378–385.
152. Wu, JT, Mattox, KL, Wall, MJ. Esophageal perforations: New perspectives and treatment paradigms. J Trauma. 2007;63:1173.
153. Gander, JW, Berdon, WE, Cowles, RA. Iatrogenic esophageal perforation in children. Ped Surg Int. 2009;25:395–401.
154. Domino, KB, Posner, KL, Caplan, RA, Cheney, FW. Airway injury during anesthesia: A closed claims analysis. Anesthesiology. 1991;91:1703.
155. Weissberg, D, Refaely, Y. Foreign bodies in the esophagus. Ann Thorac Surg. 2007;84:1854.
156. Loop, FD, Groves, LK. Esophageal perforations: Collective review. Ann Thorac Surg. 1970;10:571.
157. Mamede, RCM, De Mello Filho, FV. Treatment of caustic ingestion: An analysis of 239 cases. Dis Esophagus. 2002;15:210.
158. Swann, LA, Munter, DW. Esophageal emergencies. Emerg Med Clin North Am. 1996;14:557.
159. Lamireau, T. Accidental caustic ingestion in children: Is endoscopy always mandatory? J Pediatr Gastroenterol. 2001;33:81.
160. Vassiliu, P, Baker, J, Henderson, SO, et al. Aerodigestive injuries of the neck. Am Surg. 2001;67:75.
161. Pineau, BC, Ott, DJ. Isolated proximal esophageal injury from blunt trauma: Endoscopic stricture dilatation. Dysphagia. 2003;18:263.
162. Ahmed, N, Massier, C, Tassie, J, Whalen, J, Chung, R. Diagnosis of penetrating injuries of the pharynx and esophagus in the severely injured patient. J Trauma. 2009;67:152–154.
163. Vallbohmer, D, Holscher, AH, Holscher, M. Options in the management of esophageal perforation: Analysis over a 12-year period. Dis Esophagus. 2010;23:185–190.
164. Srinivasan, R, et al. Role of flexible endoscopy in the evaluation of possible esophageal trauma after penetrating injuries. Am J Gastroenterol. 2000;95:1725.
165. Plott, E, Jones, D, McDermott, D, Levoyer, T. A state of the art review of esophageal trauma: Where do we stand? Dis Esophagus. 2007;20:279.