Chapter 7 The structured clinical examination
Format
The SCE topics may cover the entire curriculum. You should anticipate at least one paediatric, one medical (including poison/toxins) and one surgical (including trauma) topic. You should also expect at least one skill/equipment station and one administrative scenario. Since 2007 there has been a communication station, with actors playing various roles. Each station has a number of sections the examiners will work through. It is therefore likely that these sections will be presented in combination (e.g. paediatric resuscitation from poisoning while managing distressed parents and considering non-accidental injury). Anything is possible, including being asked to demonstrate use of equipment and/or a skill. If it can happen at work and be assessed in seven minutes, it can be in the SCE!
Preparation
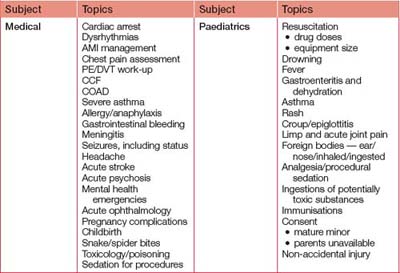
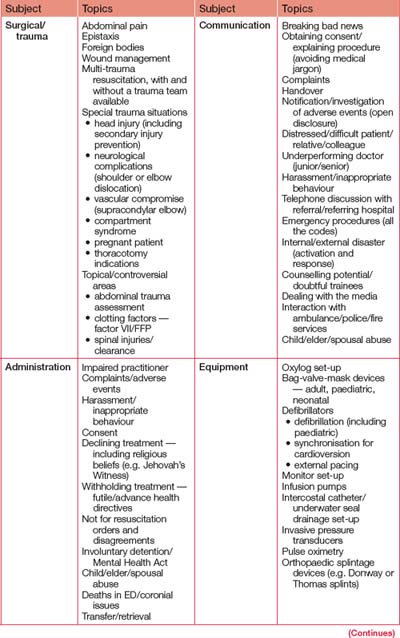
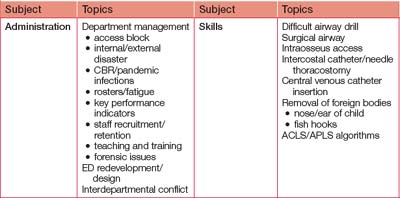
The SCE is relatively easy to prepare for. However, the scope of material that can be used in the exam is enormous. Our suggestion is to practise SCEs from each area of the curriculum, paying particular attention to what is common and what is commonly deadly. Administrative issues and communication feature in many SCEs. Be aware of this when preparing for the SCE. To become familiar with the format, talk to examiners, your DEMT and anyone who has done the exam and read the past papers on the College website. Worked examples for each major area are presented at the end of this chapter, while Table 7.1 outlines a list of key topics to prepare for. Although this list is long, it is not exhaustive. Note that ‘communication’ SCEs may involve junior or senior staff, administration, VIPs, other colleagues and/or relatives. All of the ‘administration’ topics are also well suited to testing communication.
On the day
The SCE itself
Sit comfortably: do not fidget. Answer questions directly and if you do not know an answer, say so. If time permits, the examiners may return to a section where you had a ‘mental blank’. Do not waffle or follow your own agenda: answer the question asked, not what you want it to be. One approach is to begin with a (very) brief synopsis and then expand on the possibilities. If the examiners interrupt you or redirect you along a certain course, comply and do not be concerned —you may already have answered the questions they have to follow and now they want to give you the chance to earn bonus points!
Sample SCEs
SCE 1: administration
Question 1: How would you deal with this letter of complaint? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Acknowledgment (verbal and/or written) | Medical administration Complainant |
|
| Investigation | Medical records Staff involved (medical and nursing) ComplainantCheck daughter not adult (If candidate asks, daughter is 14 years old) |
|
| Response | Timely (< 72 hours ideally) Non-judgemental Apologise sincerely/honestly without admission of liability Verbal better/written if unable |
No denial if apology appropriate |
| Counsel staff Medical defence as appropriate |
||
| Audit/quality | Review ED processes, change as indicated Use as educational exercise Arrange for someone to speak to surgeon about criticising colleagues |
System review |
| Keep records of complaints |
Question 2: The patient and her mother wish to speak to the registrar concerned. Would you agree to this and, if so, under what circumstances? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Specifics of complaint | Appropriate in most cases Helps successful resolution |
Pros and cons |
| Environment | Quiet, uninterrupted area Adequate time set aside Preferably neutral informal environment (Prompt candidate for environment if not given) |
Appropriate environment |
| Doctor concerned | Fully informed pre-meeting Apology honest, sincere Senior staff present +/– mentor Medical defence aware/give consent as appropriate |
Involve administration |
| Hospital | Medical administration aware/give consent |
Question 3: You discuss this complaint with the registrar involved. She promptly bursts into tears and admits to having used pethidine for most of the year. She has become increasingly depressed about her inability to cope. What will you do now? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Complaint-related | Not appropriate for registrar to meet with complainant Manage complaint without this meeting |
Prompt to address |
| Workplace issues | Will need time off — needs sick leave certificate Arrange cover for shifts Maintain confidentiality |
|
| Medical issues | Offer to arrange screening for HIV, Hep B, C etc. Offer medical and drug support services re management/rehabilitation etc. |
|
| Psychiatric issues | Requires urgent objective assessment and management of depression and potential for self-harm May need admission to a psychiatric/drugs of dependency facility Explore psychosocial supports — family/partner/friends etc. |
Appropriate psychological care and follow-up |
| Legal issues | Must be reported to Medical Board Inform medical administration Maintain confidentiality within the hospital |
Appropriate reporting |
| Other | Make aware of AMA/impaired practitioner service; supervised and well-monitored clinical practice; provision of mentors |
Question 4: When would you be happy for this registrar to return to work in ED? (1 minute)
| Expected response | Details and comments | Pass criteria |
| Medical | Appropriate drug-free interval, with ongoing drug screening and dependence help Mentor available |
|
| Psychiatric | Ongoing support and monitoring | |
| Medicolegal | Negotiate with medical administration and medical board regarding restrictions (e.g. cannot write S8 prescriptions) |
SCE 2: medical
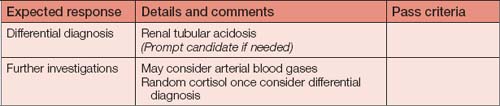
| Expected response | Details and comments | Pass criteria |
| History — presenting complaint/systems review | Symptoms: fever, abdominal pain, change in bowel habit, dysuria, frequency, cough, sputum, fluid intake, postural symptoms, headache | History features |
| Past history | Any previous episodes similar Other medical conditions: particularly immunosuppressive(Prompt candidate: any predisposing factors?) |
|
| Social | Alcohol, medications, drugs Contacts with similar (home/work) Travel |
Medication and contacts history |
| Examination | For cause — all systems potentially relevant | |
| Investigations | Bedside: BSL, urinalysis, ECG Lab: full blood profile (infection), U&Es (renal function, Na, K), Ca, LFT if indicated on history or examination Cultures: urine, blood Radiology: chest X-ray |
BSL, ECG, basic labs |
Question 2: How will you manage him? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Triage | Australasian Triage Scale (ATS) 2 Resuscitation area, team approach |
|
| Resuscitation | ABC — needs O2, IV fluids and monitor response, non-invasive monitoring | Basic description of ABC approach |
| Specific treatment | Depends on what is found, e.g. goal-directed therapy and antibiotics for severe sepsis | |
| Disposition | Depends on findings and response |
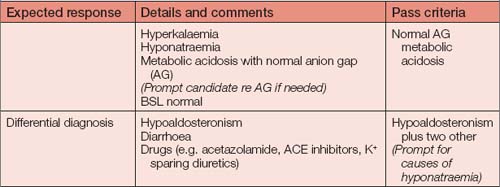
Question 4: You consider hypoaldosteronism as a likely cause. What are the differences between the available steroids? (1 minute)
| Expected response | Details and comments | Pass criteria |
| Hydrocortisone: glucocorticoid and mineralocorticoid action; can still do a short synacthen test Fludrocortisone: both properties but greater mineralocorticoid action Dexamethasone and prednisone: glucocorticoid |
SCE 3: surgical/trauma
| Expected response | Details and comments | Pass criteria |
| Immediately come in | Come in | |
| Prepare department | ED staff — current ED nursing, medical, auxiliary staff; other help as available for this patient and rest of department; activate a trauma call if hospital policy Other staff — surgical team, lab and X-ray (If asked, inform candidate that a lab and radiology with CT capability are on-site) Prepare the resuscitation bay including airway equipment, drugs, warmed fluids, O negative blood |
Consider all aspects |
| Obtain moreinformation if possible | ED staff Ambulance |
• a laceration of the left upper eyelid and a dilated pupil unresponsive to light
• a closed fracture of the left clavicle
• the abdomen is consistent with a gravid uterus at the level of the umbilicus.
Outline your actions from this point. (2 minutes)
| Expected response | Details and comments | Pass criteria |
| EMST/ATLS directed resuscitation | A — confirm ETT placement and that a cervical collar is present B — confirm adequate ventilation bilaterally C — ensure 2 × large bore IV cannulae, administer fluids, assess peripheral pulses and perfusion. Consider wedging to the left while maintaining spinal alignment (pregnant) (When asked, tell candidate she is well perfused) D — clarify GCS pre-intubation, assess other pupil (other pupil is normal — local trauma to left orbit), reflexes, plantar responses, BSL (if/when asked BSL 2 — should treat as soon as known and keep monitoring) E — need to examine back/perineum Keep warm once examined |
Adequate address to life threats Orderly approach |
| Rapid neurological assessment and decision to allow to wake or paralyse/sedate | Cannot leave biting on tube Extensor posturing is an ominous sign; together with the pupil dilatation it suggests imminent coning — traumatic mydriasis of left pupil is a possibility, but should not dissuade against instituting aggressive treatment for raised intracranial pressure Should maintain ETT with sedation/paralysis (Prompt candidate to address if not mentioned) |
Pros and cons |
| Recheck vital signs after immediate management including BSL (if not done already) | As above | BSL earlier or now |
| Secondary survey | Neurology — as much as possible prior to paralysing Secondary survey with full head-to-toe examination when able Assessment of pregnancy will be needed but not an immediate priority; likely 20-week gestation based on fundal height and thus no role for emergency delivery |
Pregnancy acknowledged Gestational age assessment reasonable |
| Ancillary | Orogastric tube Urinary catheter |
Question 3: A secondary survey reveals no other injuries. The patient remains haemodynamically stable: pulse 90–100, systolic BP 100–110. How would you investigate this patient further? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Chest X-ray | Shield abdomen Ensure tubes correctly placed Look for other thoracic abnormalities |
Trauma series |
| Lateral C-spine X-ray | (If asked, plain films show anterior crush # C4) | |
| Pelvis X-ray | Can discuss pros and cons | |
| ECG | Can discuss pros and cons | |
| Labs | Full blood profile, U&Es, BSL Group and hold — blood type as minimum (Rhesus status) ß-HCG (discuss utility if mentioned) |
BSL Rhesus status |
| CT scan of head and cervical spine | Encircling abdominal shield (Prompt discussion about how to clear the thoracolumbar spine) |
CT scan of head and cervical spine |
| Assess pregnancy | Doppler for fetal heart rate initially Ultrasound if available Consider CTG if > 26/40 |
Who and when |
| Abdominal assessment | US/CT/DPL/nothing (Prompt discussion) |
Pros and cons |
Question 4: The retrieval team will be able to transport the patient in approximately 90 minutes. What else needs to be done in the interim? (1 minute)
| Expected response | Details and comments | Pass criteria |
| Bed arranged (if not already) | Liaise with ICU, neurosurgery and obstetric teams at accepting hospital | Arrange bed |
| Packaged for transport | Lines secured Notes copied X-rays — preferably originals — with patient |
Package appropriately |
| Notification of relatives, including prognosis | (If running well on time, state the patient’s identity is currently unknown and ask candidate how they would identify her. Prompt that she has a medic alert bracelet but no wallet) | Notification |
| Registrar education | Importance of BSL (missed) Constructive feedback about trauma management How to use medic alert for patient ID |
SCE 4: paediatrics
| Expected response | Details and comments | Pass criteria |
| Triage | ATS 2/3 | |
| ABC | Exclude immediate life threats and look for other injuries | Basic ABC |
| Specific | Analgesia — discuss options and ask for correct doses (Prompt candidate for estimated weight) Apply sling and ice pack Circulation observations repeated after sling/splint |
Appropriate analgesia options Weight estimate reasonable |
| Disposition | X-ray Orthopaedic consultation Possibility of needing reduction in theatre — issues of consent (need to contact parent/guardian) Consider non-accidental injury (NAI) |
X-ray NAI |
Question 2: X-rays have been performed [give to candidate]. Please describe them. (1 minute

|

Question 3: On re-examination, the pulse in the arm is now absent. What will you do now? (1 minute)
| Expected response | Details and comments | Pass criteria |
| Remove arm from sling and straighten it | Check whether pulse returns as doing it (It does not) |
|
| Expedite orthopaedic review for likely emergent reduction in theatre | Note issues of consent | Urgent orthopaedic review |
Question 4: The orthopaedic surgeon arrives and the pulse is still absent. He instructs that the child be taken immediately to theatre. How will you obtain consent for this procedure? (1 minute)
| Expected response | Details and comments | Pass criteria |
| Surgeon primarily responsible for consent Try all avenues to contact parents Urgent situation (threat to limb) and may need consent from medical administration |
Consent options discussed |
Question 5: The parents arrive just as the child is being taken to theatre. The father starts conversing angrily with the baby-sitter in French. How will you manage this situation? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Determine whether father can speak English | If not, will need an interpreter (baby-sitter no longer appropriate as sole interpreter) Awareness of interpreter service essential (If candidate can speak French, ask them what they would do if it was a language they could not speak) |
Need appropriate communication |
| Defuse situation | Be mindful of potential NAI on part of baby-sitter or parents | |
| Address consent issues | Provide information on procedure (may need to come from surgical team) |
SCE 5: equipment/skills
Question 1: Please set up this ventilator [Oxylog 1000] to ventilate this patient and check that it is working correctly. (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Describe | Ventilator identified Circuit with HME and PEEP valve (Prompt candidate, if necessary) |
Oxylog 1000 |
| Check oxygen source and turn on | Check alarms | |
| Set | Rate 12–14; MV 5–7 L/min; TV 400–500 mL; FiO2no air mix initially PEEP valve set at 5 cmH2O initially (Prompt candidate for rate and minute volume, if necessary) |
Appropriate settings |
| Demonstrate | Working as expected Spirometer use |
Question 2: How would you monitor this patient’s respiratory status over the next two hours? (1 minute)
| Expected response | Details and comments | Pass criteria |
| Clinical | Vital signs — pulse, blood pressure Chest examination — expansion and auscultation findings; frequency/character of secretions |
|
| Monitors | ECG; SaO2; ETCO2 | ECG, SaO2, ETCO2 essential |
| Other | Alarms — peak pressure, supply failure and disconnect ABG — perform serially to optimise ventilation Chest X-ray — repeat if deterioration occurs |
Question 3: Fifteen minutes later, you are called back to the patient because the SaO2has dropped to 70%. Detail the possible causes and your immediate management. (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Possible causes | Probe off (usually obvious) Poor blood flow to probe area O2supply failure or disconnection Leaks (circuit, cuff deflation, high peak pressures) ETT problems — endobronchial migration, dislodgement or blockage Disease complications (e.g. pneumothorax, haemothorax, evolving contusions) Ventilator dysynchrony (Prompt candidate to start from one end and work along) |
At least three of these |
| Action | Assume it is a real problem Disconnect patient from ventilator and hand ventilate with 100% O2 Examine patient — ensure trachea midline, chest expansion, air entry and breath sounds Consider suctioning airway Check monitors — SaO2, ETCO2, airway pressures Check ventilator and O2supply before reconnecting to Oxylog May need extra PEEP May need to involve intensivist — reassess fitness to transfer and need for a better ventilator |
Remove Oxylog from decision |
Question 4: The retrieval service calls to say that it will not be able to collect the patient for another 12 hours. What will you do? (2 minutes)
| Expected response | Details and comments | Pass criteria |
| Consider other transport options | Road/rotary/fixed wing Consider level of escort available and ability to travel by chosen method |
Pros and cons |
| Consider other bed options | Liaise with local intensivist for assistance — may need to admit this patient and transfer out someone more stable Liaise with other nearby hospitals Remain in ED if necessary but negotiate the most appropriate possible staff to care for her |
Other options |
| Other | Continue quality supportive care: • orogastric tube and urinary catheter • fluids • sedation and paralysis • eye, mouth and pressure area care Communicate with relatives Keep in touch with retrieval service and update receiving hospital regularly |
Ongoing patient management |
SCE 6: communication
Information for examiners
The actor who will play Amy’s mother has been briefed with the following background information:
Information for actor playing Amy’s mother
uestion: This is Mrs Jones, the mother of Amy. Please discuss the situation with her.
| Expected response | Details and comments | Pass criteria |
| Introduction | Identify self by name as doctor caring for Amy | Essential |
| Confirm information known | Clarify what the mother knows and her concerns Use non-confrontational manner Preserve Amy’s confidentiality Explain the legal implications of confidentiality as related to minors and adults Clarify the legal status of Amy as a minor or an adult; adult defined from age 16 if living independently or the individual has a child |
Reasonable approach expected Establish rapport Active listening picking up non-verbal cues Body language appropriate Language appropriate — not medical jargon |
| Information released only with consent |
Will be classified as adult Information can be passed on only with the consent of the patient |
Identify status as adult Protect confidentiality |
| Resolution of situation | Empathise with mother’s position Offer to liaise with Amy with intention of creating direct dialogue between them |
Reasonable resolution |