CHAPTER 44 The Role of Arthroscopy in Scaphoid Fractures
Rationale and Basic Science Pertinent to the Procedure
The complex morphology and the small size of the scaphoid bone resulted in the development of numerous sophisticated techniques to achieve an anatomical and stable fixation. In 1984, Herbert and Fischer1 reported their experience using a cannulated screw, which originally was not developed for fixation of scaphoid fractures. In the early 1990s, the first article was published2 describing inserting cannulated screws with a minimally invasive technique. The main principle was to preserve the surrounding ligaments of the carpal bones to avoid a destabilization of the reduction and to protect the fragile vascularization of the scaphoid bone.3
Whipple4,5 first presented a method with percutaneous screw fixation using a modified Herbert screw combined with image intensifier control and arthroscopic examination of the wrist. This method allowed the surgeon to control the reduction and to assess potential associated lesions.
Operative Technique
Under ambulatory conditions, the operation is performed with locoregional anesthesia. The patient is placed in the supine position on a special arm table with a tourniquet on the arm applied as proximal as possible. During the critical parts of the operation, the forearm can be extended using a pad underneath the wrist. Another possibility is to put the wrist under traction with a traction device, which is placed outside the arm table still allowing positioning the image intensifier. A retrograde (from distal to proximal) screw fixation is aimed. First, the fracture is visualized under arthroscopy using standard portals, leaving the forearm free on the table. Next, a 1-mm pin is placed through a small (5-mm) incision to the distal tuberosity of the scaphoid in a retrograde fashion (Fig. 44-1). Then the wrist is put under traction allowing arthroscopic control to verify the exact reduction of the scaphoid.

FIGURE 44-1 Percutaneous retrograde pinning of the scaphoid through a small approach centered on the distal tuberosity.
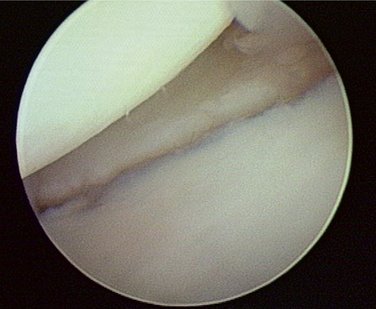
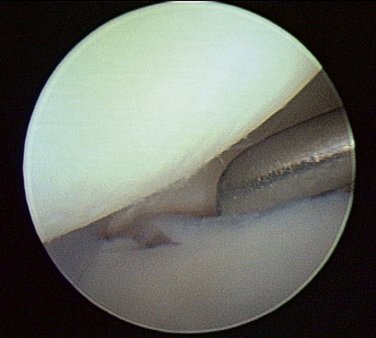
The arthroscope is introduced through a radial midcarpal portal through which the fracture can be assessed easily. If necessary, a débridement of the articulation can be done with the shaver while cleaning the medial surface of the scaphoid. If the fracture is displaced, reduction of the fragments is possible with a little retractor introduced through the STT midcarpal portal. Under arthroscopic control, the fracture fixation pin is slightly pulled back beyond the fracture line, then the fracture is reduced, and the pin is replaced into the proximal fragment (Figs. 44-2, 44-3, and 44-4). As soon as a satisfactory reduction is achieved, the hand is removed from the traction device, and the wrist is positioned on a pad on the arm table.
Under fluoroscopic control, the hole for the screw is tapped. If a resorbable screw is chosen, a double-sized trephine, drilling proximal with a 3-mm part and distal with a 3.5-mm part at the same time, is used. The two different screw threads are separately prepared mechanically to avoid the phenomenon of blockage in torsion with a resorbable screw. This avoids the risk of implant fracture (Fig. 44-5). The screw is inserted over the guidewire. Again under arthroscopic control, the radiocarpal compartment is visualized through the 3,4 portal; this allows the surgeon to verify the absence of an intra-articular penetration of the screw head at the level of the proximal pole (Fig. 44-6).
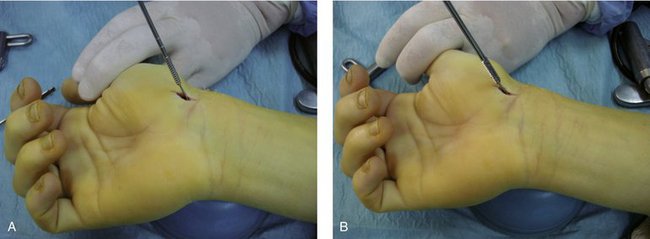
FIGURE 44-5 A, Tapping of the proximal part of the scaphoid. B, Tapping of the distal part of the scaphoid.
The entire radiocarpal compartment is inspected to assess potential associated lesions. Midcarpal exploration allows the inspection of the fracture line to the medial articular surface of the scaphoid and the assessment of the reduction quality. In case of insufficient compression, the screw can be redrilled while visualizing the compressive effect. The scaphotrapeziotrapezoid articulation remains untouched. The resorbable screw has only one size with a long distal part, which allows adaptation to different scaphoid sizes. The surgeon must cut the part that is outside of the bone short at the scaphoid with a mini-oscillating saw (Fig. 44-7). The incisions are closed using Steri-strips. Postoperatively, the wrist is left unprotected; a simple anterior splint can be applied after the first dressing to help with postoperative pain.
Important aspects of the operative technique are as follows:
The risks of the procedure are as follows:
Results
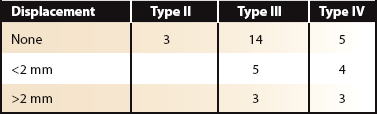
All fractures were acute (type B according to the classification of Herbert and Fischer1); the mean delay from trauma to surgery was 9 days (range 2 to 30 days). There were mainly waist fractures (type III and IV according to Schernberg’s classification6); fractures of the proximal pole were not included (Table 44-1). The fracture was nondisplaced in 22 cases.
Discussion and Review of Literature
Numerous more recent studies have shown the capability of a percutaneous fixation of scaphoid fractures using cannulated screws.2,7–9 The various cannulated screw models underline the interest in this method and create competition with the classic conservative method of forearm immobilization for 3 months. Several studies confirm the increased rate of fracture consolidation with this method.7–10 The time to consolidation in nondisplaced fractures seems to be shorter with percutaneous screw fixation. Shin and coworkers10 reported in their randomized study (percutaneous screw fixations versus conservative treatment) a consolidation time of 4 to 5 weeks after percutaneous screw fixation. With our results with an average radiological consolidation of less than 2 months in nondisplaced fractures, we can confirm this statement.
In various series, return to professional activities was earlier after screw fixation.8,10,11,14,21 In our study, the functional recovery also was exceptionally fast. This also might be due to a patient selection bias because many of our patients have chosen this method with regard to their professional and personal duties. It seems to be more logical to propose the percutaneous screw fixation to a motivated and well-informed patient even more when conservative treatment has the risk to fail (e.g., in unstable fractures). The failure rate in terms of consolidation can be 15% after cast immobilization of 3 months.12,13 In our series, there were no nonunions.
Wrist arthroscopy combined with percutaneous screw fixation allows avoiding certain complications that are relatively frequent in fracture fixation of the scaphoid. Filan and Herbert13 found 14 intra-articular (Herbert) screw penetrations in their series of 431 patients. In our series, after final arthroscopic control of the radiocarpal joint, we had to change three screws because of breakout of the screw tip out of the scaphoid. Arthroscopic midcarpal examination also allows assessing the quality of fracture reduction after screw fixation.
We agree with Whipple16 that direct visual examination of the reduction quality is much more efficient than fluoroscopic evaluation. Direct visual control of fracture compression is an additional security for the surgeon. The possibility to diagnose and treat associated lesions with arthroscopic exploration of the wrist was described by many authors.15,16 Shin and coworkers10 found 11 intracarpal lesions during arthroscopic exploration in a series of 15 displaced scaphoid fractures that were treated with arthroscopic reduction and percutaneous fixation. Most of them were minor lesions, but the authors also found two complex scapholunate lesions that could be treated with reduction and pinning.
Because of the need for reduction, displaced scaphoid fractures usually required classic open reduction.17 The possibility to maintain the reduction by external maneuvers justified the use of percutaneous screw fixation.18 If one could not maintain the reduction, change to an open procedure was indicated.19 In our series we did not have any problems with the reduction, and all the displaced scaphoid fractures could be reduced and maintained under arthroscopic control (Fig. 44-8).
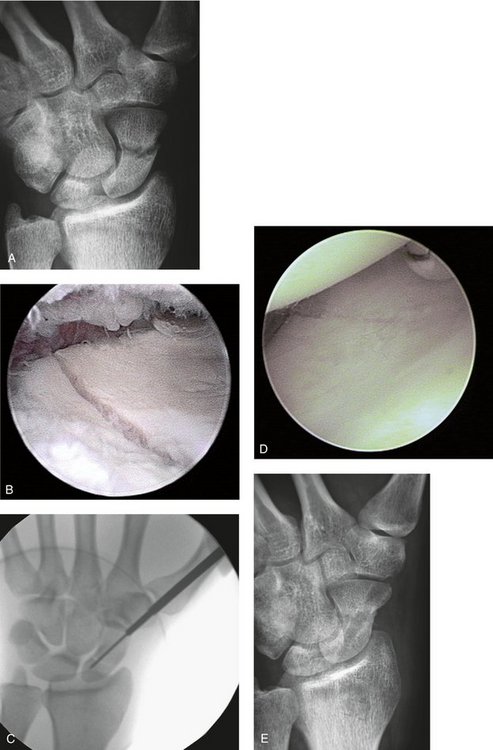
FIGURE 44-8 A, Displaced scaphoid fracture. B, Mediocarpal arthroscopic view showing the rotational displacement between the two fragments. C, Mediocarpal arthroscopic view showing the reduction after disimpaction of the two fragments with the help of a small curet. D, Drilling with fluoroscopic control. E, Radiographic control after 60 days showing the consolidated fracture.
Wrist arthroscopy has found its place for this indication allowing direct and indirect reduction maneuvers. Slade and colleagues20 described in detail their technique of percutaneous arthroscopically assisted fracture fixation from proximal to distal. The guiding pin is placed with the wrist in hyperflexion and hyperpronation after reduction of the geometric axis of the scaphoid under fluoroscopic control. The screws that were used (Acutrak LLC, Hillsboro, OR) are voluminous, and in our opinion penetration of the screw at the proximal pole may cause a significant cartilage lesion at the scaphoid head. In the case of a fracture type I according to Schernberg, the small-sized proximal fragment has to be fixed with a standard screw. Apart from these specific cases, the technique of screw fixation through a volar approach with the assistance of a small elevator through an STT midcarpal portal to align the fragments always allowed us to verify the reduction without major difficulties. The classic disadvantages of the scaphotrapeziotrapezoid articulation with a volar approach have led to a systematic removal of the screw after 1 year to avoid secondary osteoarthritis.20 The advent of resorbable screws may have solved this particular problem.22 We have performed screw removal only in the case of persistent anterior wrist pain. A longer follow-up is necessary to evaluate the potential development of secondary osteoarthritis.
1. Herbert TJ, Fischer WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Am. 1984;66:114-123.
2. Wozasek GE, Moser KD. Percutaneous screw fixation of fractures of the scaphoid. J Bone Joint Surg Am. 1991;73:138-142.
3. Gelberman RH, Menon J. Vascularity of the scaphoid bone. J Hand Surg [Am]. 1980;5:508-513.
4. Whipple TL. Stabilization of the fractured scaphoid under arthroscopic control. Orthop Clin North Am. 1995;26:749-754.
5. Whipple T. Arthroscopic surgery. In: The Wrist. Philadelphia: J.B. Lippincott; 1992.
6. Schernberg F, Elzein F, Gerard Y. Etude anatomo-cliniquedes fractures du scaphoïde carpien. Problème des cals vicieux. Rev Chir Orthop. 1984;70(II suppl):55-63.
7. Ledoux P, Chahidi N, Moermans JP, et al. Percutaneous Herbert screw osteosynthesis of the scaphoid bone. Acta Orthop Belg. 1995;61:43-47.
8. Inoue G, Sionoya K. Herbert screw fixation by limited access for acute fracture of the scaphoid. J Bone Joint Surg Br. 1997;79:418-421.
9. Haddad FS, Goddard NJ. Acute percutaneous scaphoid fixation: a pilot study. J Bone Joint Surg Br. 1998;80:95-99.
10. Shin A, Bond A, McBride M, et al: Acute screw fixation versus cast immobilisation for stable scaphoid fractures: a prospective randomized study. Presented at the 55th American Society of Surgery for the Hand, Seattle, October 5-7, 2000.
11. Gellman H, Caputo RJ, Carter V, et al. Comparison of short and long arm thumb-spica casts for non displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989;71:354-357.
12. Kuschner SH, Lane CS, Brien WW, et al. Scaphoid fractures and scaphoid non-union: diagnosis and treatment. Aust N Z J Surg. 1985;55:387-389.
13. Filan SL, Herbert TJ. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Am. 1996;78:519-529.
14. Bond CD, Shin AY, McBride MT, et al. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83:483-488.
15. Shih JT, Lee HM, Hou YT, et al. Result of arthroscopic reduction and percutaneous fixation for acute displaced scaphoid fractures. Arthroscopy. 2005;21:620-626.
16. Whipple TL. The role of arthroscopy in the treatment of intra-articular wrist fractures. Hand Clin. 1995;11:13-18.
17. Schernberg F. Les fractures récentes du scaphoïde. Chir Main. 2005;24:117-131.
18. Cooney WP, Dobyns JH, Linscheid RL. Fractures of the scaphoid : a rational approach to management. Clin Orthop. 1980;149:90-97.
19. Herbert TJ. Internal fixation of the scaphoid—history. In: Le Scaphoïde. Sauramps; 2004:125-129.
20. Slade JF3rd, Grauer JN, Mahoney JD. Arthroscopic reduction and percutaneous fixation of scaphoid fractures with a novel dorsal technique. Orthop Clin North Am. 2001;32:247-261.
21. Rosati M, Nesti C, Del Grande S, et al. L’osteosintesi con vite cannulata percutanea nelle fratture di scafoide carpale. Riv Chir Mano. 2004;41:149-157.
22. Martinache X, Mathoulin C. Ostéosynthèse percutanée des fractures du scaphoide carpien avec assistance arthroscopique. Chir Main. 2006;25:S171-S177.