Chapter 19 The Neurologic System
A. Mental Status Examination
5 What are the snouting, rooting, and sucking reflexes?
 Snouting is the labial pouting/pursing elicited by pressing a tongue blade on the patient’s lips.
Snouting is the labial pouting/pursing elicited by pressing a tongue blade on the patient’s lips.
 Rooting is the shift of the mouth toward a tactile stimulus. It can be elicited by gently stroking the lateral upper lip—or, in newborns, by touching the junction of the lips. This causes head-turning and mouth-opening, as if “rooting” toward the stroke (mom’s breast or the bottle).
Rooting is the shift of the mouth toward a tactile stimulus. It can be elicited by gently stroking the lateral upper lip—or, in newborns, by touching the junction of the lips. This causes head-turning and mouth-opening, as if “rooting” toward the stroke (mom’s breast or the bottle).
 Sucking is pouting or sucking following gentle touching of the patient’s lip. Normal in infants until weaning, it is absent in adults—except in diffuse frontal lobe injury.
Sucking is pouting or sucking following gentle touching of the patient’s lip. Normal in infants until weaning, it is absent in adults—except in diffuse frontal lobe injury.
10 What are the most important levels of consciousness? How do they deteriorate?
There are four levels of consciousness. In increasing degree of deterioration they are:
 Alertness: An awake person with normal level of consciousness (alert patient)
Alertness: An awake person with normal level of consciousness (alert patient)
 Lethargy: A sleepy patient who needs continuous stimulation to remain awake
Lethargy: A sleepy patient who needs continuous stimulation to remain awake
 Stupor: An unarousable patient who can still moan, withdraw, or roll around during exam
Stupor: An unarousable patient who can still moan, withdraw, or roll around during exam
 Coma: A patient who offers no purposeful response to stimulations of any kind
Coma: A patient who offers no purposeful response to stimulations of any kind
12 What is memory? How do you assess it?
Memory is the ability to register and recall prior sensory input. For testing purposes:
(1)Language
22 What is cerebellar speech?
Another disorder of articulation of sound, rather than ideation or perception (ataxic speech).
23 Beside cerebellar speech, what are the two most important types of dysarthria?
 Spastic dysarthria. This is due to damage of upper motor neurons (connecting the cortex to the spine), resulting in excessive and uncontrolled tone.
Spastic dysarthria. This is due to damage of upper motor neurons (connecting the cortex to the spine), resulting in excessive and uncontrolled tone.
 Flaccid dysarthria. This is due instead to damage of lower motor neurons, compromising all aspects of speech production. Lesions of individual cranial nerve(s) (brain stem stroke or peripheral facial nerve paralysis) also can cause dysarthria. For instance, Bell’s palsy may cause difficulty in saying “mo-mo-mo” (see Table 19-1).
Flaccid dysarthria. This is due instead to damage of lower motor neurons, compromising all aspects of speech production. Lesions of individual cranial nerve(s) (brain stem stroke or peripheral facial nerve paralysis) also can cause dysarthria. For instance, Bell’s palsy may cause difficulty in saying “mo-mo-mo” (see Table 19-1).
Table 19-1 Dysarthria and Possible Cranial Nerve Involvement
| Syndrome | Sounds | Possible Cranial Nerve Involved |
|---|---|---|
| Labial | “mo-mo-mo” | CN VII (facial nerve) |
| Lingual | “la-la-la-la” | CN XII (hypoglossal nerve) |
| Pharyngeal | “ka-ka-ka” | CN IX and X (glossopharyngeal nerve and vagus nerve) |
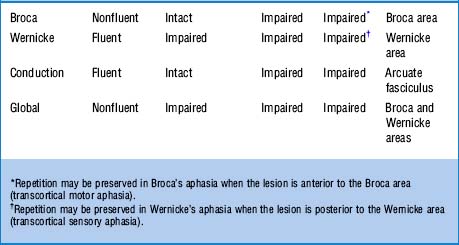
25 What are the most important defects in aphasia?
 Inability to understand language (receptive, sensory, posterior aphasia; also called fluent or Wernicke’s aphasia)
Inability to understand language (receptive, sensory, posterior aphasia; also called fluent or Wernicke’s aphasia)
 Inability to transfer signals from Wernicke to Broca (conductive aphasia)
Inability to transfer signals from Wernicke to Broca (conductive aphasia)
 Inability to properly execute speech (expressive, motor anterior aphasia; also called nonfluent or Broca’s aphasia)
Inability to properly execute speech (expressive, motor anterior aphasia; also called nonfluent or Broca’s aphasia)
Combined Broca’s and Wernicke’s aphasias constitute global aphasia.
26 What are the clinical differences between fluent and nonfluent aphasia?
 In fluent aphasia (Wernicke’s), talking is easy, but words are often jumbled and meaningless. There is difficulty in naming objects, repeating sentences, or comprehending. Speech is full of emptiness and gibberish “jargon,” even though patients seem unaware of it. In fact, they may even appear confused and almost psychotic. Reading impairment parallels the speech deficit. The responsible lesion is in the temporal or parietal lobe.
In fluent aphasia (Wernicke’s), talking is easy, but words are often jumbled and meaningless. There is difficulty in naming objects, repeating sentences, or comprehending. Speech is full of emptiness and gibberish “jargon,” even though patients seem unaware of it. In fact, they may even appear confused and almost psychotic. Reading impairment parallels the speech deficit. The responsible lesion is in the temporal or parietal lobe.
 In nonfluent aphasia (Broca’s), there is obvious struggling for words and great difficulty with speaking. Language is slow, made up of monosyllabic sentences, and full of latency. In fact, it resembles the labored use of English by tongue-tied foreigners. Although nonfluent aphasics have a hard time naming objects and repeating sentences, their comprehension of spoken and written material is often quite good. Yet, they may be dyslexic (i.e., making semantic errors and having difficulty in reading highly imaginable words). A writing deficit usually parallels the phonologic deficit. The responsible lesion is in the frontal lobe.
In nonfluent aphasia (Broca’s), there is obvious struggling for words and great difficulty with speaking. Language is slow, made up of monosyllabic sentences, and full of latency. In fact, it resembles the labored use of English by tongue-tied foreigners. Although nonfluent aphasics have a hard time naming objects and repeating sentences, their comprehension of spoken and written material is often quite good. Yet, they may be dyslexic (i.e., making semantic errors and having difficulty in reading highly imaginable words). A writing deficit usually parallels the phonologic deficit. The responsible lesion is in the frontal lobe.
31 What is cortical dementia? What is subcortical dementia?
 Cortical dementia is cortical damage resulting in aphasia, dyspraxia, agnosia.
Cortical dementia is cortical damage resulting in aphasia, dyspraxia, agnosia.
 Subcortical dementia is damage of the basal ganglia, thalamus, rostral brain stem nuclei, and frontal lobe projections. It results in bradyphrenia, a unique slowness of thought processes (such as cognition, motivation, and attention) that is absent in cortical dementia.
Subcortical dementia is damage of the basal ganglia, thalamus, rostral brain stem nuclei, and frontal lobe projections. It results in bradyphrenia, a unique slowness of thought processes (such as cognition, motivation, and attention) that is absent in cortical dementia.
B. Cranial Nerves Examination
35 How do you test CN I (olfactory nerve)?
By asking patients to close their eyes, occlude one nostril, and then smell through the open naris a distinctive scent—like cinnamon, cloves, or peppermint. Transient anosmia is common, usually resulting from simple colds or intercurrent sinus infection. Chronic anosmia (especially if congenital) is instead quite important (see Chapter 6, question 33). Note that anosmia can also be seen in frontal/temporal lobectomies or Parkinson’s disease.
36 How do you test CN II (optic nerve)?
 Visual acuity:Ask the patient to read an eye chart from a distance of 20 feet. Glasses or contacts are allowed, since the test measures the best corrected vision. A normal person reads at 20 feet letters that others also can read at 20 feet (20/20 vision). A person who reads at 20 feet letters that others can read at 40 is said to have an acuity of 20/40 (see Chapter 4, questions 1–15).
Visual acuity:Ask the patient to read an eye chart from a distance of 20 feet. Glasses or contacts are allowed, since the test measures the best corrected vision. A normal person reads at 20 feet letters that others also can read at 20 feet (20/20 vision). A person who reads at 20 feet letters that others can read at 40 is said to have an acuity of 20/40 (see Chapter 4, questions 1–15).
 Visual fields: Their assessment can localize damage anywhere from the retina to the occipital lobes, resulting in loss of vision of only a discrete area (or field). The best way to detect visual cuts is by confrontation: place yourself head-to-head and eye-to-eye with the patient, while both of you occlude the opposite eye (because while looking into each other’s eyes, both you and the patient have the same peripheral vision). To determine whether the patient can see what you see, move objects into his/her peripheral vision, starting from above, then below, then left and right. Patients should be able to see the objects at the same time you do. If they cannot, they probably have a visual cut corresponding to a particular region of peripheral vision (see Chapter 4, questions 20–35).
Visual fields: Their assessment can localize damage anywhere from the retina to the occipital lobes, resulting in loss of vision of only a discrete area (or field). The best way to detect visual cuts is by confrontation: place yourself head-to-head and eye-to-eye with the patient, while both of you occlude the opposite eye (because while looking into each other’s eyes, both you and the patient have the same peripheral vision). To determine whether the patient can see what you see, move objects into his/her peripheral vision, starting from above, then below, then left and right. Patients should be able to see the objects at the same time you do. If they cannot, they probably have a visual cut corresponding to a particular region of peripheral vision (see Chapter 4, questions 20–35).
37 How do you test CN III, IV, and VI?
Together, since oculomotor (III), trochlear (IV), and abducens (VI) work in concert to produce the various eye movements. To test them, ask patients to hold the head stationary while following your finger as it moves through the main directions of gaze: left-up, left-middle, left-down, and right-up, right-middle, and right-down. Normal eyes move symmetrically and smoothly. Any restriction or double vision (from inability of the eyes to move together) suggests damage to III, IV, or VI (see Chapter 4, questions 84–90).
38 What abnormal eye movements result from damage to CN III, IV, or VI?
 The oculomotor supplies medial, superior, and inferior rectus; inferior oblique; and levator palpebrae (which raises the eyelid). It also contains parasympathetic fibers that constrict the pupil. Hence, its lesions result in a partially abducted eye that is difficult to adduct, raise, or lower. In fact, it is frequently turned out (exotropia). There also is a drooping eyelid (ptosis) and a pupil that may be larger (mydriatic) and difficult to constrict. In more subtle cases, there may only be diplopia or blurred vision. A CN III palsy that spares the pupils (i.e., ptosis, and external rotation of the globe, but symmetric and equally reactive pupils) suggests diabetes, but also vasculitides and multiple sclerosis.
The oculomotor supplies medial, superior, and inferior rectus; inferior oblique; and levator palpebrae (which raises the eyelid). It also contains parasympathetic fibers that constrict the pupil. Hence, its lesions result in a partially abducted eye that is difficult to adduct, raise, or lower. In fact, it is frequently turned out (exotropia). There also is a drooping eyelid (ptosis) and a pupil that may be larger (mydriatic) and difficult to constrict. In more subtle cases, there may only be diplopia or blurred vision. A CN III palsy that spares the pupils (i.e., ptosis, and external rotation of the globe, but symmetric and equally reactive pupils) suggests diabetes, but also vasculitides and multiple sclerosis.
 The trochlear supplies the superior oblique muscle by extending over a trochlea, or pulley. Since this nerve allows us to view the tip of our nose, its lesion will result in an eye that cannot be depressed when adducted. Hence, whenever patients pull their eyes inward (toward the nose), they will be unable to move them downward. This is often subtle. An isolated right superior oblique paralysis results in (1) exotropia to the right (R); (2) double vision that worsens when looking to the left (L); and (3) head tilt to the right (R). The mnemonic is R, L, R (the marching rule—conversely, the rule for left superior oblique paralysis is L, R, L). This rule and the lack of ptosis and/or mydriasis differentiate the exotropia of CN IV palsy from that of CN III.
The trochlear supplies the superior oblique muscle by extending over a trochlea, or pulley. Since this nerve allows us to view the tip of our nose, its lesion will result in an eye that cannot be depressed when adducted. Hence, whenever patients pull their eyes inward (toward the nose), they will be unable to move them downward. This is often subtle. An isolated right superior oblique paralysis results in (1) exotropia to the right (R); (2) double vision that worsens when looking to the left (L); and (3) head tilt to the right (R). The mnemonic is R, L, R (the marching rule—conversely, the rule for left superior oblique paralysis is L, R, L). This rule and the lack of ptosis and/or mydriasis differentiate the exotropia of CN IV palsy from that of CN III.
 id=”u0300″/>The abducens supplies the lateral rectus. Hence, its damage prevents eye abduction to the side of the lesion. This results in double vision on horizontal gaze only (horizontal homonymous diplopia). It is often injured in patients with increased intracranial pressure.
id=”u0300″/>The abducens supplies the lateral rectus. Hence, its damage prevents eye abduction to the side of the lesion. This results in double vision on horizontal gaze only (horizontal homonymous diplopia). It is often injured in patients with increased intracranial pressure.
39 How do you test CN V (trigeminal nerve)?
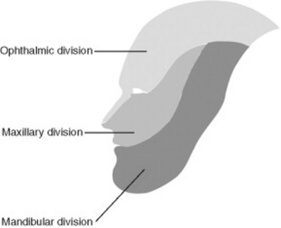
It depends on whether you are testing a motor or sensory component. The divisions of the trigeminal nerve are shown in Figure 19-1.
 The sensory component is predominant, providing pain, tactile, and thermic sensations to the face. Note that sensation to the tragus, most of the external ear, and angle of the jaw is not trigeminal and thus is preserved in diseases of the V (it is supplied instead by cervical sensory roots).
The sensory component is predominant, providing pain, tactile, and thermic sensations to the face. Note that sensation to the tragus, most of the external ear, and angle of the jaw is not trigeminal and thus is preserved in diseases of the V (it is supplied instead by cervical sensory roots).
 The motor component is smaller and primarily involved in chewing. It travels along the mandibular branch of the V and controls the masseters and lateral pterygoids. If damaged, it causes deviation of the jaw to the paralyzed side when attempting to open the mouth.
The motor component is smaller and primarily involved in chewing. It travels along the mandibular branch of the V and controls the masseters and lateral pterygoids. If damaged, it causes deviation of the jaw to the paralyzed side when attempting to open the mouth.
40 Where are the sensory and motor nuclei of the trigeminal nerve?
They are both in the pons. Yet the sensory also extends into the cervical cord.
41 How do you test the sensory function of CN V?
By pinprick or light touch over the areas of distribution of the trigeminal branches: upper (supplied by V1, or ophthalmic; forehead), mid (V2, or maxillary; cheek), and lower (V3, or mandibular; jaw). Sensory function of the ophthalmic branch is also tested by the corneal reflex (see question 58).
42 How do you test the motor function of CN V?
By feeling the masseters during teeth clinching. Contraction must be strong and symmetric.
45 What is the significance of a sensory deficit of the trigeminal nerve?
It depends on whether it involves both the face and body, or only the face:
 Isolated facial anesthesia suggests disease of the temporal bone or metastatic spread to the ipsilateral mandible and skull base. This presents with numbness to the chin and lower lip (“numb/chin syndrome”).
Isolated facial anesthesia suggests disease of the temporal bone or metastatic spread to the ipsilateral mandible and skull base. This presents with numbness to the chin and lower lip (“numb/chin syndrome”).
 Combined facial and body anesthesia suggests hemispheric and thalamic involvement, typically cerebrovascular. This presents with numbness to the same side of face and body (and contralateral to the ischemic area), plus hemiparesis and aphasia. Conversely, patients with facial numbness to one side and body numbness to the opposite have a brain stem lesion.
Combined facial and body anesthesia suggests hemispheric and thalamic involvement, typically cerebrovascular. This presents with numbness to the same side of face and body (and contralateral to the ischemic area), plus hemiparesis and aphasia. Conversely, patients with facial numbness to one side and body numbness to the opposite have a brain stem lesion.
47 What is the jaw-jerk reflex?
A reflex that tests the integrity of sensory (afferent) and motor (efferent) components of the V. To test for it, place your index finger (or tongue depressor) over the patients’ chin, while asking them to keep their mouth slightly open. Then, gently tap the index finger with your reflex hammer. Abnormal responses include jaw deviation or brisk closure. Exaggerated masseteric contraction, often with clonus, suggests upper motor neuron pathology (i.e., above the trigeminal nucleus in the mid-pons). This occurs in 70% of pseudobulbar palsy patients (see below, question 65).
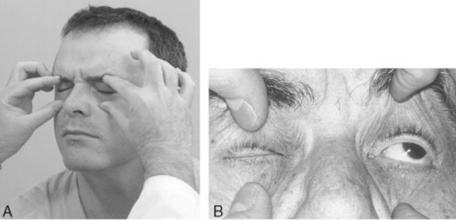
48 How do you test CN VII (facial nerve)?
Through the muscles of facial expression. Damage to CN VII causes inability to wrinkle the forehead, tightly close the eye (Fig. 19-2), or smile. It also causes facial asymmetry (i.e., ipsilateral widening of the palpebral fissure and sagging of the nasolabial fold).
60 How do you test CN VIII (acoustic/vestibular nerve)?
It depends on the function you want to test, vestibular or auditory:
 Vestibular function should be assessed by the Romberg, positional vertigo, and caloric irrigation tests only in cases of vertigo and dizziness.
Vestibular function should be assessed by the Romberg, positional vertigo, and caloric irrigation tests only in cases of vertigo and dizziness.
 Auditory function may instead be compromised in very subtle ways. Hence, the need for routine testing. This can be simply done by asking patients if they can hear whispered words, the soft noise of a ticking watch, or fingers rubbing against each other near the ear. Conductive and sensorineural hearing loss can be separated by Rinne and Weber tests (see Chapter 5, questions 59–65).
Auditory function may instead be compromised in very subtle ways. Hence, the need for routine testing. This can be simply done by asking patients if they can hear whispered words, the soft noise of a ticking watch, or fingers rubbing against each other near the ear. Conductive and sensorineural hearing loss can be separated by Rinne and Weber tests (see Chapter 5, questions 59–65).
64 What is the anatomy of CN IX (glossopharyngeal) and CN X (vagus)? How do you test them?
Axons from several brain stem nuclei mingle together to emerge from the neuraxis through two separate nerves, named by early neuroanatomists as glossopharyngeal (IX) and vagal (X) (the vagus was so termed since, as a vagabond, it wanders long distances in the body). In reality, the origin of the two nerves is essentially identical. Function also is similar: motor control of the palate and pharynx (plus, for the IX, sensory supply to the pharynx and posterior third of the tongue). Hence, their clinical testing is not entirely separable. Since the brain stem nuclei of these two nerves receive bilateral innervation from the cortex, their dysfunction results from one of three possibilities: (1) bilateral damage to the cortex or pyramidal tracts (pseudobulbar palsy), (2) brain stem disease (lateral medullary syndrome), or (3) peripheral nerve lesions (jugular foramen syndrome). You can test IX and X by asking patients to say “ahhh” or “ehhh” (see Chapter 6, questions 53 and 54) while observing whether the velum of the palate rises symmetrically. Alternatively, you can use the gag and palatal reflexes. The latter is elicited by touching the patient’s palate with a cotton swab, which causes elevation of the soft palate and ipsilateral deviation of the uvula. The gag is instead triggered by touching the posterior wall of the pharynx (or alternatively, the tonsillar area or base of the tongue). It causes tongue retraction and elevation/constriction of the pharyngeal musculature. In unilateral CN IX and X paralysis, these reflexes result in deviation of the uvula toward the normal side. Lesions of the IX also will result in loss of taste in the posterior third of the tongue, and loss of pain and touch sensations in the same area plus the soft palate and pharyngeal walls. Conversely, unilateral paralysis of CN X’s recurrent laryngeal nerve will cause hoarseness. Bilateral paralysis will cause stridor (requiring tracheostomy).
69 How do you test CN XI?
By first looking for asymmetry in the SCMs and trapezii. Then, by asking patients to shrug their shoulders against resistance (which tests the trapezius; Fig 19-3) or by having them first turn the head to one side and then attempt to turn it back against your resistance (which tests the SCM; Fig. 19-4). To test the right SCM, instruct the patient to turn the head toward the left, hold it there, and to not let you push it back. Then place your hand on the patient’s left cheek, and try to force the head toward the midline. When the right SCM is weak, pushing against your resistance will be impaired. Repeat the same for the opposite side. Note that atrophy of these muscles reflects a “lower” lesion (peripheral nerve or brain stem/cervical spine). Weakness, on the other hand, also may reflect cerebral hemispheric disease. The latter weakens the contralateral trapezius and the ipsilateral SCM (hence, the patient will be unable to turn the head toward the hemiparetic side). Disease of the accessory nucleus per se (like syringomyelia) weakens instead (and atrophies) both ipsilateral muscles. Hence, the patient will be unable to shrug ipsilaterally or turn the head toward the same side. This also occurs for peripheral nerve lesions.
C. Motor System Examination
72 What is the motor system made of?
 The pyramidal component (i.e., the corticospinal level of the motor system). This consists of (1) the upper (cortical) motor neurons (residing in the posterior regions of the frontal lobes [i.e., the motor cortex]) and (2) the pyramidal tracts (i.e., descending corticospinal pathways).
The pyramidal component (i.e., the corticospinal level of the motor system). This consists of (1) the upper (cortical) motor neurons (residing in the posterior regions of the frontal lobes [i.e., the motor cortex]) and (2) the pyramidal tracts (i.e., descending corticospinal pathways).
 The extrapyramidal component. This has instead its nuclei of origin in the basal ganglia and their complex connections, creating an elaborate neural organization that works closely with other levels of the motor system to achieve muscular control.
The extrapyramidal component. This has instead its nuclei of origin in the basal ganglia and their complex connections, creating an elaborate neural organization that works closely with other levels of the motor system to achieve muscular control.
(1) Atrophy, Hypertrophy, and Fasciculations
77 What is muscle atrophy?
From the Greek a (lack of) and trophe (nourishment), this is the muscular wasting caused by damage to lower motor neurons or their axons. Since these lesions typically interrupt the flow of trophic factors to the muscle, they result in degeneration and wasting of dependent myofibers (and fasciculations too—see question 79). Atrophy also may result from congenital muscular diseases or simple disuse, because of either trauma or arthritis. Yet the most common cause is indeed damage to the supplying neuron/nerve. Examples of atrophic muscles include the flat thenar eminence of carpal tunnel syndrome, the prominent metacarpals of polyneuropathy (with loss of interossei), and the atrophic calf of sciatica. To test for it, assess the muscle’s three S’s: size, symmetry, and shape. Atrophy, hypertrophy, and abnormal bulging/depressions are all important findings in identifying various muscular diseases or abnormalities—especially if asymmetric. Shape may be diagnostic, too, especially when altered by tendinous rupture.
(2) Muscle Strength and Tone
81 How is muscle strength graded?
 0/5 represents no muscle contraction and no joint movement.
0/5 represents no muscle contraction and no joint movement.
 1/5 is visible contraction of a muscle without sufficient strength to move a joint.
1/5 is visible contraction of a muscle without sufficient strength to move a joint.
 2/5 is strength sufficient to move a joint but not to overcome the resistance of gravity.
2/5 is strength sufficient to move a joint but not to overcome the resistance of gravity.
 3/5 is strength sufficient to move against gravity but not to withstand active resistance.
3/5 is strength sufficient to move against gravity but not to withstand active resistance.
 4/5 is strength sufficient to move against gravity and to overcome some resistance by the examiner.
4/5 is strength sufficient to move against gravity and to overcome some resistance by the examiner.
This system is well accepted and clinically useful but does have flaws.
86 In addition to lower motor neuron disease, are there any other causes of hypotonia?
Definitely spinal shock, but also some cerebellar diseases (see below, questions 91, 159, and 166).
87 What are the extreme forms of hypertonia?
 Spasticity: The hypertonia of pyramidal tract disease. Resistance is initially low, but gradually increases as the muscle is being progressively stretched by repeat limb extension and flexion. When it reaches considerable tension, there is a protective relaxation and a sudden “clasp-knife” loss of tone, usually toward completion of joint flexion or extension.
Spasticity: The hypertonia of pyramidal tract disease. Resistance is initially low, but gradually increases as the muscle is being progressively stretched by repeat limb extension and flexion. When it reaches considerable tension, there is a protective relaxation and a sudden “clasp-knife” loss of tone, usually toward completion of joint flexion or extension.
 Rigidity: The hypertonia of extrapyramidal disease (Parkinson’s). It occurs throughout the full range of motion of the joint, with neither weakness nor clasp-knife phenomenon. It is constant (independent of the speed of the examiner’s movement) and equal in both extensors and flexors. It may result in a cogwheel (stepwise) or lead-pipe (uniform) resistance to passive movement.
Rigidity: The hypertonia of extrapyramidal disease (Parkinson’s). It occurs throughout the full range of motion of the joint, with neither weakness nor clasp-knife phenomenon. It is constant (independent of the speed of the examiner’s movement) and equal in both extensors and flexors. It may result in a cogwheel (stepwise) or lead-pipe (uniform) resistance to passive movement.
 Paratonia: An increased tone that occurs not at rest, but at the time the limb tested contacts another object. It is a sign of bilateral frontal lobe disease, often associated with dementia.
Paratonia: An increased tone that occurs not at rest, but at the time the limb tested contacts another object. It is a sign of bilateral frontal lobe disease, often associated with dementia.
88 Name the four commonly used examples of hypertonia
 Clasp-knife: Direct proportional increase in resistance, followed by a sudden and giveaway release in tone. It is common in upper motor neuron disease and a feature of spasticity.
Clasp-knife: Direct proportional increase in resistance, followed by a sudden and giveaway release in tone. It is common in upper motor neuron disease and a feature of spasticity.
 id=”u0580″/>Lead-pipe: A steady resistance throughout range of motion. It is a feature of rigidity.
id=”u0580″/>Lead-pipe: A steady resistance throughout range of motion. It is a feature of rigidity.
 Cogwheel: A ratchet-like resistance during active range of motion. The affected limb gives in intermittently to the pulling by the examiner, as if it were a lever over a ratchet. It is common in extrapyramidal disease, such as Parkinson’s, and is a feature of rigidity.
Cogwheel: A ratchet-like resistance during active range of motion. The affected limb gives in intermittently to the pulling by the examiner, as if it were a lever over a ratchet. It is common in extrapyramidal disease, such as Parkinson’s, and is a feature of rigidity.
 Gegenhalten (German for “against-stop”): A resistance that increases in proportion to how quickly the limb is actively moved, diminishing when movement slows. It is common in frontal lobe diseases, such as Alzheimer’s and head trauma, and is a feature of paratonia.
Gegenhalten (German for “against-stop”): A resistance that increases in proportion to how quickly the limb is actively moved, diminishing when movement slows. It is common in frontal lobe diseases, such as Alzheimer’s and head trauma, and is a feature of paratonia.
92 What is asterixis?
An inability to maintain muscle tone. It is commonly elicited by having patients close their eyes and then stretch out their arms, with fingers spread and dorsiflexed wrists—as if they were “stopping traffic.” This results in rhythmic flexion at the wrist due to sudden loss of tone, causing the hand to flap (flapping tremor). It reflects various metabolic encephalopathies (see Chapters 20, questions 50–52).
(3) Muscle Percussion
93 What is the response of a muscle to the stroke of a reflex hammer?
The normal is myoedema. The abnormal is percussion myotonia.
(4) Reflexes
98 How do you elicit the corneal/conjunctival reflex?
By gently touching the cornea or conjunctiva with a sterile wisp of cotton. A normal response consists of bilateral winking (see questions 58 and 59).
100 How do you elicit the cremasteric reflex?
By drawing a line along the medial thigh. A normal reflex will elevate the ipsilateral testis.
103 Is there any evidence that one hammer is better than the others?
No. Taylor, Queen Square, or Troemner are very much the same. Preference depends on taste.
105 How are reflexes graded?
 0/4 is absence of any reflex (areflexia)—despite reinforcement.
0/4 is absence of any reflex (areflexia)—despite reinforcement.
 1/4 is a reduced or weak reflex—usually requiring reinforcement.
1/4 is a reduced or weak reflex—usually requiring reinforcement.
 3/4 is a brisk reflex (hyperreflexia).
3/4 is a brisk reflex (hyperreflexia).
 4/4 is extremely brisk hyperreflexia, usually accompanied by clonus (from the Greek klonos, tumult). This is a self-sustained and rhythmic muscle movement, marked by a rapid sequence of contractions and relaxations, which occurs (and persists) after the clinician has briskly stretched a hyperreflexic muscle and maintained tension on it. Typical of feet, clonus also can be elicited in the quadriceps, jaw, and other muscles.
4/4 is extremely brisk hyperreflexia, usually accompanied by clonus (from the Greek klonos, tumult). This is a self-sustained and rhythmic muscle movement, marked by a rapid sequence of contractions and relaxations, which occurs (and persists) after the clinician has briskly stretched a hyperreflexic muscle and maintained tension on it. Typical of feet, clonus also can be elicited in the quadriceps, jaw, and other muscles.
106 What is the Jendrassik maneuver?
A reinforcement technique that can help elicit deep tendon reflexes in apprehensive and tense patients, who, either voluntarily or unconsciously, may be bracing their muscles (Fig. 19-5). During the patellar reflex, have the patient hook together the flexed fingers of the two hands and then pull them apart at the moment the reflex is being elicited. Other re-enforcement maneuvers include having the patient look up at the ceiling, count numbers, read, or cough—all aimed at redirecting the patient’s attention, thus relaxing the tested muscles.
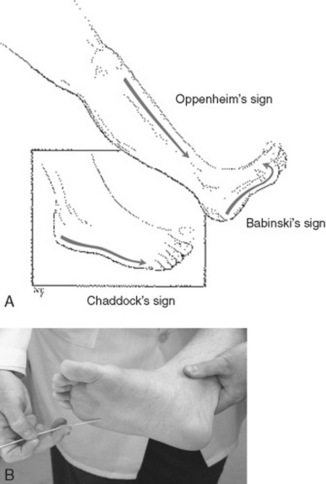
113 What is the plantar reflex?
A cutaneous reflex (i.e., one triggered by skin stimulation) (Fig. 19-6). In normal subjects, a noxious stimulation of the sole leads to a plantar flexion of the toes, including the big toe. Conversely, in organic neurologic disease, there will be an extensor response (i.e., an upward movement of the great toe). Babinski used this finding to exclude hysterical weakness, which typically lacks “Babinski,” as this reflex soon came to be known. Note that when stroking the lateral aspect of the sole of the foot, the big toe may display one of the responses shown in Table 19-3 below.
114 What is the Babinski sign?
It is the original Babinski’s: dorsiflexion (or extension) of the big toe in response to stroking of the lateral aspect of the sole (see Fig. 19-6). In other words, the big toe goes up. Except for infants (where it is normal), this indicates a lesion of upper motor neurons or their pyramidal tracts. It also can occur in metabolic involvement of these tracts, such as meningitis, seizure, overdose, and hepatic/renal encephalopathy. Dorsiflexion of the big toe also may be associated with fanning out of the other toes (as in Babinski’s description), yet this is not a requirement for the response to be abnormal. An extensor plantar response (or Babinski) is an excellent bedside test: sensitive, specific, and able to pinpoint the lesion.
116 Name the different techniques to elicit the extensor plantar response
 Babinski: Stimulate the lateral plantar surface of the foot with a blunt point, going from the heel forward, medially crossing the metatarsal pad to the big toe.
Babinski: Stimulate the lateral plantar surface of the foot with a blunt point, going from the heel forward, medially crossing the metatarsal pad to the big toe.
 Chaddock: Stimulate the lateral aspect of the foot from the heel forward to the small toe.
Chaddock: Stimulate the lateral aspect of the foot from the heel forward to the small toe.
 Oppenheim: Apply pressure with your thumb and index finger to the anterior surface of the tibia downward toward the ankle.
Oppenheim: Apply pressure with your thumb and index finger to the anterior surface of the tibia downward toward the ankle.
 Gordon: Apply deep pressure to the calf muscles.
Gordon: Apply deep pressure to the calf muscles.
 Strumpell: Apply strong pressure on the anterior tibia.
Strumpell: Apply strong pressure on the anterior tibia.
 Moniz: Forceful plantar flexion of the ankle
Moniz: Forceful plantar flexion of the ankle
 Gonda-Allen: Downward snapping the distal phalanx of the second or fourth toe (Hoffman-like)
Gonda-Allen: Downward snapping the distal phalanx of the second or fourth toe (Hoffman-like)
The first four are the most used, with decreasing effectiveness from Babinski to Gordon.
120 What are the most important abnormal involuntary movements?
 Tremors: Rhythmic muscular oscillations around a joint, to-and-fro or up-and-down
Tremors: Rhythmic muscular oscillations around a joint, to-and-fro or up-and-down
 Fibrillations: Not visible to the naked eye except possibly those in the tongue
Fibrillations: Not visible to the naked eye except possibly those in the tongue
 Chorea: One of many writhing and twisting motions, which also include athetosis and hemiballismus
Chorea: One of many writhing and twisting motions, which also include athetosis and hemiballismus
 Myoclonus: A sudden and brief (<0.25 second) muscle jerk, shock-like, with twitching of a joint; often asymmetric; isolated or in association with hypoxic encephalopathy/epilepsy
Myoclonus: A sudden and brief (<0.25 second) muscle jerk, shock-like, with twitching of a joint; often asymmetric; isolated or in association with hypoxic encephalopathy/epilepsy
 Dystonia: A persistent, fixed contraction of a muscle—such as torticollis or wry neck
Dystonia: A persistent, fixed contraction of a muscle—such as torticollis or wry neck
 Seizures: May result in automatisms of the face or limbs, repeated eye blinks, or tonic-clonic activity
Seizures: May result in automatisms of the face or limbs, repeated eye blinks, or tonic-clonic activity
121 Name the three types of tremors and how to elicit them
 Resting tremor: Best observed when patients are distracted (i.e., counting numbers with eyes closed) and their hands are lying on the lap. Resting tremor of 4–6 Hz is typical of Parkinson’s. Amplitude and frequency of the tremor increase during stress and improve with voluntary movements. The rest tremor of the hand is often described as “pill-rolling.”
Resting tremor: Best observed when patients are distracted (i.e., counting numbers with eyes closed) and their hands are lying on the lap. Resting tremor of 4–6 Hz is typical of Parkinson’s. Amplitude and frequency of the tremor increase during stress and improve with voluntary movements. The rest tremor of the hand is often described as “pill-rolling.”
 Postural tremor: Postural tremor of 6–11 Hz is best elicited by having the arms or legs maintain a particular posture against gravity (i.e., benign essential tremor of aging). There also may be titubation of head or jaw and tremulous speech, like in the late Katherine Hepburn.
Postural tremor: Postural tremor of 6–11 Hz is best elicited by having the arms or legs maintain a particular posture against gravity (i.e., benign essential tremor of aging). There also may be titubation of head or jaw and tremulous speech, like in the late Katherine Hepburn.
 Action tremor: Best elicited by having the patient perform common tasks, like drinking from a cup or writing. Most prominent in goal-directed movements (e.g., finger-to-nose testing) and usually associated with cerebellar lesions.
Action tremor: Best elicited by having the patient perform common tasks, like drinking from a cup or writing. Most prominent in goal-directed movements (e.g., finger-to-nose testing) and usually associated with cerebellar lesions.
124 What is hemiballismus?
It is a violent flinging movement of half of the body due to lesions of the subthalamic nucleus.
D. Sensory System Examination
136 Which dermatomeric rules should be kept in mind during the exam?
 Contiguous dermatomes overlap. Yet each has a unique “signature zone” (i.e., an area with no overlap that can be used to identify the spinal site of lesion).
Contiguous dermatomes overlap. Yet each has a unique “signature zone” (i.e., an area with no overlap that can be used to identify the spinal site of lesion).
 Tactile dermatomes are larger than pain dermatomes. Hence, pain testing is more sensitive than touch testing.
Tactile dermatomes are larger than pain dermatomes. Hence, pain testing is more sensitive than touch testing.
 Sensory level in spinal cord lesions can be several segments below the actual lesion. This is caused by the vascular supply (which may be injured at one level, but cause ischemia at another and more distant section) or the anatomic organization of nociceptive pathways (which carry lower body sensations more laterally than others, thus making themselves more exposed to injury). This does not occur with motor fibers. Hence, whenever there is discrepancy between motor and sensory level, always trust the motor level.
Sensory level in spinal cord lesions can be several segments below the actual lesion. This is caused by the vascular supply (which may be injured at one level, but cause ischemia at another and more distant section) or the anatomic organization of nociceptive pathways (which carry lower body sensations more laterally than others, thus making themselves more exposed to injury). This does not occur with motor fibers. Hence, whenever there is discrepancy between motor and sensory level, always trust the motor level.
137 Which sensations should be tested during the neurologic exam?
 A comprehensive exam should test (1) pain (pinprick), (2) touch, (3) vibration, and (4) position.
A comprehensive exam should test (1) pain (pinprick), (2) touch, (3) vibration, and (4) position.
 A screening exam should test only touch (on all extremities).
A screening exam should test only touch (on all extremities).
 If examining patients presenting with sensory complaints to one extremity, test both touch and pain, even though pain testing is usually more sensitive than touch testing. If concerned about spinal cord disease (i.e., extensive sensory deficits, involving, for example, trunk or large parts of an extremity), test instead all sensations. This may reveal sensory dissociation (i.e., loss of one perception, but not of others).
If examining patients presenting with sensory complaints to one extremity, test both touch and pain, even though pain testing is usually more sensitive than touch testing. If concerned about spinal cord disease (i.e., extensive sensory deficits, involving, for example, trunk or large parts of an extremity), test instead all sensations. This may reveal sensory dissociation (i.e., loss of one perception, but not of others).
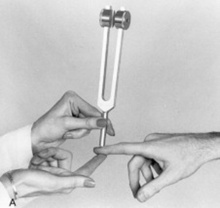
143 How do you assess vibration?
By using a 128-Hz tuning fork (Fig. 19-7). To do so:
1. First set it in motion by striking it against your palm from a distance of 20 cm.
2. Apply its handle to a bony prominence of the patient’s hand or foot.
3. Ask the patient whether he or she can feel the vibration.
144 Which vibration frequencies are well perceived by humans?
Those between 200–300 Hz. Frequencies <100 Hz are instead poorly felt.
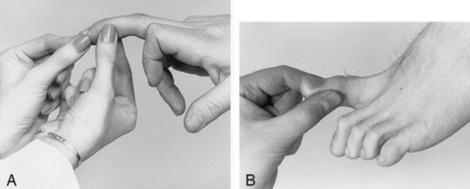
147 How do you test for position sensation?
First of all, ask patients to shut their eyes. Then, use your thumb and forefinger to grasp the lateral aspect of their great toe (or index finger) (Fig. 19-8). Move it up or down, while inquiring about direction of movement. Patients with intact proprioception should detect joint movements of as little as 1–2 degrees, even though 10% of the time they might be wrong in describing direction, since motion is more easily perceived than direction.
155 What is bilateral simultaneous tactile stimulation?
The ability to recognize that two sides of your body are being simultaneously touched.
E. Cerebellum
159 Which clinical findings suggest damage to the cerebellum and its tracts?
 Abnormal posture or gait (truncal ataxia): Due to median cerebellar lesions
Abnormal posture or gait (truncal ataxia): Due to median cerebellar lesions
 Intention tremor: A tremor that worsens at end-of-movement, while approaching the target
Intention tremor: A tremor that worsens at end-of-movement, while approaching the target
 Dyssynergia (incoordination): Lack in smoothness of execution of various motor activities
Dyssynergia (incoordination): Lack in smoothness of execution of various motor activities
 Dysmetria: Inability to control range of movement, resulting in overshooting or undershooting of a target
Dysmetria: Inability to control range of movement, resulting in overshooting or undershooting of a target
 Dysrhythmia: Inability to tap and keep a rhythm; for example, while tapping the table with a hand or the floor with a foot
Dysrhythmia: Inability to tap and keep a rhythm; for example, while tapping the table with a hand or the floor with a foot
 Dysdiadochokinesia: Difficulty in performing rapidly alternating movements
Dysdiadochokinesia: Difficulty in performing rapidly alternating movements
 Dysarthria: A breakdown of melody and prosody of speech, with poor modulation
Dysarthria: A breakdown of melody and prosody of speech, with poor modulation
162 How do you test for ataxia?
 Diadochokinesia: From the Greek diadocha (in succession) and kinesis (movements). This is the ability to rapidly perform alternating movements. To test for it, instruct the patient to pat the knee with the dorsum and palm of one hand, pronating and supinating back and forth. Since this is difficult to perform in cerebellar disease, the test is quite sensitive for ataxia. Observe speed, rhythm, accuracy, and smoothness of movements. Anything that is slow, irregular, clumsy, and inaccurate is abnormal, and suggestive of either dysdiadochokinesia (from the Greek dys, impaired) or adiadochokinesia (“a,” lack of; complete inability to perform these movements). Another way to test for diadochokinesia consists of having the patient touch the tip of each finger with the tip of the thumb, in rapid sequence, back and forth. Speed, coordination, force, and direction of movement are all affected.
Diadochokinesia: From the Greek diadocha (in succession) and kinesis (movements). This is the ability to rapidly perform alternating movements. To test for it, instruct the patient to pat the knee with the dorsum and palm of one hand, pronating and supinating back and forth. Since this is difficult to perform in cerebellar disease, the test is quite sensitive for ataxia. Observe speed, rhythm, accuracy, and smoothness of movements. Anything that is slow, irregular, clumsy, and inaccurate is abnormal, and suggestive of either dysdiadochokinesia (from the Greek dys, impaired) or adiadochokinesia (“a,” lack of; complete inability to perform these movements). Another way to test for diadochokinesia consists of having the patient touch the tip of each finger with the tip of the thumb, in rapid sequence, back and forth. Speed, coordination, force, and direction of movement are all affected.
 Finger-to-finger: Hold a finger in front of the patient and ask him or her to use the index finger to touch first your finger and then the tip of his/her nose—back and forth several times. Inability to hit the mark in a coordinated fashion indicates cerebellar disease/dysfunction (dysmetria). Intention tremor and dyssynergia may occur, too. Test each hand separately, and keep arms fully extended during testing, since this may precipitate tremors and incoordination.
Finger-to-finger: Hold a finger in front of the patient and ask him or her to use the index finger to touch first your finger and then the tip of his/her nose—back and forth several times. Inability to hit the mark in a coordinated fashion indicates cerebellar disease/dysfunction (dysmetria). Intention tremor and dyssynergia may occur, too. Test each hand separately, and keep arms fully extended during testing, since this may precipitate tremors and incoordination.
 Heel-to-shin-to-knee: Ask a supine patient to place one heel on the opposite knee, and then slide it smoothly down the shin, over the dorsum of the foot, and back up to the knee. Look for wobbling or unsteadiness. Overshooting (hypermetria) or undershooting (hypometria) represents abnormal responses (i.e., dysmetria).
Heel-to-shin-to-knee: Ask a supine patient to place one heel on the opposite knee, and then slide it smoothly down the shin, over the dorsum of the foot, and back up to the knee. Look for wobbling or unsteadiness. Overshooting (hypermetria) or undershooting (hypometria) represents abnormal responses (i.e., dysmetria).
164 How do patients with cerebellar deficits walk? How do they stand?
They walk with an ataxic gait: legs spread wide apart, as in a staggering and “drunk” fashion. Especially difficult is tandem walking (i.e., with one foot directly in front of the other [heel-to-toe]), as if on an imaginary tight rope (hence, its use for alcohol intoxication testing). Patients with cerebellar deficits have problems with stance, too, which is unbalanced, incoordinated, and with tendency to sway or fall to one side—especially when unassisted by vision (Romberg, see also Chapter 1, questions 90–94).
165 How common is ataxic gait in cerebellar disease?
Very common. In fact, the most common of all cerebellar manifestations.
170 How is the speech of cerebellar disease?
Dysarthric. In other words: slow, irregular, slurred, and with sudden changes in tempo, volume, and pitch (scanning or staccato speech), and yet still capable of conveying meaningful and intelligible words. This is due to discoordination of the muscles of phonation. In contrast to aphasics, patients with cerebellar deficits have no problems understanding or making themselves understood (see also questions 19–27).
F. Gait
172 What is the control of walking? How is gait assessed?
Walking is a highly complex action that requires integration of motor, cerebellar, vestibular, sensory, visual, and other systems. Hence, almost any abnormality in the nervous system will affect a patient’s gait. To evaluate it, ask the patient to first walk normally, then on heels and toes, and finally to perform tandem walking. This simple test will allow you to detect many neurologic deficits, including weakness, incoordination, and dizziness (see also Chapter 1, question 71).
G. Application of the Neurologic Examination
185 What are the symptoms of muscle disease?
 Can you arise from a chair, get out of a car seat, get off the toilet, or go up stairs without using your hands? This question checks for proximal leg weakness.
Can you arise from a chair, get out of a car seat, get off the toilet, or go up stairs without using your hands? This question checks for proximal leg weakness.
 Can you lift or carry objects, such as briefcases, schoolbooks, children, grocery bags, or garbage bags? This question checks for proximal arm weakness.
Can you lift or carry objects, such as briefcases, schoolbooks, children, grocery bags, or garbage bags? This question checks for proximal arm weakness.
 Is your weakness symmetric? Since most generalized processes are slightly asymmetric, there may be some minor differences. Yet, weakness confined to either one limb or one side of the body is very unlikely in pure myopathy.
Is your weakness symmetric? Since most generalized processes are slightly asymmetric, there may be some minor differences. Yet, weakness confined to either one limb or one side of the body is very unlikely in pure myopathy.
 Is there any associated numbness or sensory loss? Pain, cramping, and uncomfortable sensations may occur in some myopathic patients, but sensory loss should be absent.
Is there any associated numbness or sensory loss? Pain, cramping, and uncomfortable sensations may occur in some myopathic patients, but sensory loss should be absent.
187 What are the symptoms of neuromuscular junction (NMJ) disease?
 Symptoms similar to those of myopathy: proximal and symmetric weakness with intact sensory. Yet, NMJ disease has a unique hallmark: fatigability (i.e., the worsening of weakness with use, and its recovery after rest). Since resting improves strength, fatigability does not present as a steady progressive decline during the day, but as variability (or fluctuation) in strength, as the muscle first fatigues, then recovers, and then fatigues again.
Symptoms similar to those of myopathy: proximal and symmetric weakness with intact sensory. Yet, NMJ disease has a unique hallmark: fatigability (i.e., the worsening of weakness with use, and its recovery after rest). Since resting improves strength, fatigability does not present as a steady progressive decline during the day, but as variability (or fluctuation) in strength, as the muscle first fatigues, then recovers, and then fatigues again.
 NMJ symptoms also are very proximal. Hence, they affect the facial muscles, resulting in drooping of the eyelids (ptosis), double vision (diplopia), difficulty with chewing and swallowing, slurred speech, and facial weakness.
NMJ symptoms also are very proximal. Hence, they affect the facial muscles, resulting in drooping of the eyelids (ptosis), double vision (diplopia), difficulty with chewing and swallowing, slurred speech, and facial weakness.
189 What are the symptoms of peripheral neuropathy?
1. Do you wear out the toes of shoes, or catch the toes and trip? This checks distal weakness in the legs. Symptoms are typical of patients with a foot drop.
2. Do you have trouble with grip? Do you frequently drop things? This checks distal strength in the hands.
3. Is the process asymmetric? Some neuropathies are distal, symmetric, stocking-and-glove in distribution, but most are asymmetric.
4. Have you noticed shrinking or wasting of your muscles (atrophy)? How about quivering and twitching muscles (fasciculations)?
193 What is the presentation of spinal cord disease (SCD)?
 Is there a sensory level? Some patients describe it as a belt, a band, or “tight swimming trunks” around waist or chest.
Is there a sensory level? Some patients describe it as a belt, a band, or “tight swimming trunks” around waist or chest.
 Do you drag the toe or trip because of distal leg weakness? Lesions of the upper motor neuron or pyramidal tract cause weakness that is usually greatest distally. Hence, they may mimic a peripheral neuropathy.
Do you drag the toe or trip because of distal leg weakness? Lesions of the upper motor neuron or pyramidal tract cause weakness that is usually greatest distally. Hence, they may mimic a peripheral neuropathy.
 Are your legs stiff? Pyramidal tract weakness causes spasticity. Hence, patients report their legs as being “stiff” and their knees as unable to bend properly during walking.
Are your legs stiff? Pyramidal tract weakness causes spasticity. Hence, patients report their legs as being “stiff” and their knees as unable to bend properly during walking.
 Is there either retention or incontinence of bowel and bladder? Note that the bladder is usually much more sensitive to spinal cord injury than the bowel.
Is there either retention or incontinence of bowel and bladder? Note that the bladder is usually much more sensitive to spinal cord injury than the bowel.
195 What are the symptoms of brain stem disease?
196 After eliciting brain stem symptoms, which findings can you expect on exam?
A combination of cranial nerve and long-tract abnormalities.
 For cranial nerves, there may be ptosis, extraocular movements abnormalities, diplopia, nystagmus, decreased corneal reflexes, facial weakness or numbness, decreased hearing, dysarthria, paralysis of the palate, decreased gag reflex, or tongue deviation.
For cranial nerves, there may be ptosis, extraocular movements abnormalities, diplopia, nystagmus, decreased corneal reflexes, facial weakness or numbness, decreased hearing, dysarthria, paralysis of the palate, decreased gag reflex, or tongue deviation.
 For long-tract abnormalities, there may be hemiparesis (with a pyramidal pattern of distal weakness), hyperreflexia, hypertonia, and positive Babinski. Hemisensory loss may include decreased sensation to all modalities.
For long-tract abnormalities, there may be hemiparesis (with a pyramidal pattern of distal weakness), hyperreflexia, hypertonia, and positive Babinski. Hemisensory loss may include decreased sensation to all modalities.
197 What are the symptoms of cerebellar disease?
 Is there a staggering, drunken walk? Alcohol impairs the cerebellum, especially the rostral vermis, which is responsible for the characteristic wide-based gait of intoxication.
Is there a staggering, drunken walk? Alcohol impairs the cerebellum, especially the rostral vermis, which is responsible for the characteristic wide-based gait of intoxication.
 Is there difficulty putting a key in a lock, lighting a cigarette, or carrying out other target-directed movements? Cerebellar tremor is typically worsened by voluntary and intentional movements, especially when the hand approaches the target. Hence, fine/coordinated motions (like extending a key and inserting it into the narrow slot of a lock) are impossible.
Is there difficulty putting a key in a lock, lighting a cigarette, or carrying out other target-directed movements? Cerebellar tremor is typically worsened by voluntary and intentional movements, especially when the hand approaches the target. Hence, fine/coordinated motions (like extending a key and inserting it into the narrow slot of a lock) are impossible.
199 What are the symptoms of cerebral hemispheric disease (CHD)?
 Does the patient have aphasia or altered mental status?
Does the patient have aphasia or altered mental status?
 Do weakness and numbness affect the face, arm, and leg on the same side of the body?
Do weakness and numbness affect the face, arm, and leg on the same side of the body?
 Is there a visual field defect? Visual fibers run subcortically (in the optic tract, lateral geniculate, and optic radiations) and terminate in the occipital cortex.
Is there a visual field defect? Visual fibers run subcortically (in the optic tract, lateral geniculate, and optic radiations) and terminate in the occipital cortex.
 Is there a movement disorder, such as chorea, dystonia, or hemiballismus?
Is there a movement disorder, such as chorea, dystonia, or hemiballismus?
 Any history of seizures? This indicates the paroxysmal discharge of neurons, usually cortical.
Any history of seizures? This indicates the paroxysmal discharge of neurons, usually cortical.
200 After eliciting CHD symptoms, which findings can you expect on exam?
Aphasia or other mental status changes, plus hemiparesis, hemianesthesia, or visual field cuts.
H. Special Problems—Meningeal Signs
208 How clinically useful are these signs in the detection of meningitis?
It depends on the underlying process:
 In acute bacterial meningitis, the most common sign is nuchal rigidity (84% sensitive), followed by Kernig’s or Brudzinski’s (61% sensitive). Other findings (such as change in mental status, focal neurologic findings, and fever) are more frequent in the elderly. Note that no meningeal sign is specific for meningitis. In fact, neck stiffness can be seen in one third of elderly hospitalized patients without meningitis, and Kernig’s is often positive in sciatica.
In acute bacterial meningitis, the most common sign is nuchal rigidity (84% sensitive), followed by Kernig’s or Brudzinski’s (61% sensitive). Other findings (such as change in mental status, focal neurologic findings, and fever) are more frequent in the elderly. Note that no meningeal sign is specific for meningitis. In fact, neck stiffness can be seen in one third of elderly hospitalized patients without meningitis, and Kernig’s is often positive in sciatica.
 In subarachnoid hemorrhage, the most common finding also is nuchal rigidity (sensitivity 21–86%), accompanied by the sudden onset of severe headache (present in 80% of the cases) in an otherwise nonfocal neurologic exam. In fact, nonfocality and nuchal rigidity argue strongly for subarachnoid hemorrhage in patients with an acute neurologic presentation. Stroke or intracranial hemorrhage is much less likely.
In subarachnoid hemorrhage, the most common finding also is nuchal rigidity (sensitivity 21–86%), accompanied by the sudden onset of severe headache (present in 80% of the cases) in an otherwise nonfocal neurologic exam. In fact, nonfocality and nuchal rigidity argue strongly for subarachnoid hemorrhage in patients with an acute neurologic presentation. Stroke or intracranial hemorrhage is much less likely.
1 Greenberg DA. Clinical Neurology. New York: McGraw-Hill, 2002.
2 Haerer AF. DeJong’s The Neurologic Examination, 5th ed. Philadelphia: JB Lippincott, Mosby, 1992.
3 Jankovic J, Marsden CD, et al. Parkinson’s Disease & Movement Disorders. Philadelphia: Lippincott, 2002.
4 McGee S. Evidence-Based Physical Diagnosis. Philadelphia: WB Saunders, 2001.
5 Medical Research Council. Aids to the Examination of the Peripheral Nervous System. London: Her Majesty’s Stationery Office, 1986.
6 Olson, WH. Handbook of Symptom-Oriented Neurology. Mosby: St. Louis, Mosby; 1994.
7 Patten J. Neurological Differential Diagnosis, 2nd ed. London: Springer, 1996.
8 Strub RL, Black FW, et al. The Mental Status Examination in Neurology. Philadelphia: FA Davis, 1977.