The limbic system: influence over motor control and learning
DARCY A. UMPHRED, PT, PhD, FAPTA, MARCIA HALL THOMPSON, PT, DPT, DSc and THERESE MARIE WEST, PhD, MT-BC, FAMI
After reading this chapter the student or therapist will be able to:
1. Understand the complexity of the limbic network and the influence of the limbic network on behavioral and functional responses.
2. Describe the behavioral responses directly influenced by the limbic network.
3. Describe the structures of the limbic network.
4. Describe the interaction between the limbic network and body systems responsible for behavioral responses.
5. Differentiate between limbic-driven motor control responses and frontal, cerebellar, and basal ganglia motor regulation.
6. Differentiate between declarative and procedural learning.
7. Identify signs of both positive and negative limbic network influence on a client’s observable behavior and functional responses.
8. Describe appropriate treatment interventions or program modifications for both the limbic high and limbic low client.
9. Understand the influence of the therapist over the limbic network and behavioral and functional responses, and effectively integrate limbic network treatment techniques into current treatment models.
Since the publication of the fifth edition of this book, the limbic network has emerged as a key component of central nervous system (CNS) function, becoming one of the most researched areas of the CNS when analyzing behavior, learning, emotions, and their influence on activities and participation. In the past, review of the literature on the limbic network was limited to investigating potential interactions of other systems with nuclei within the limbic network. This is no longer the case, as neuroscience research has helped to identify the critical nature of behaviors controlled or influenced by the limbic network. Based on research at a cellular level,1–3 a consciousness level,4–7 a bodily systems level,8–10 and a quantum level11–13 it is now clear that the motor system is just one of the many systems affected by the complex limbic network.14–21
Obviously, the human organism is a complex totality made up of many interlocking parts. The medical system has traditionally divided the body into systems and has forgotten that each specific system is co-dependent on many other systems for function. Today the medical profession is rediscovering the importance of how the systems interact with and influence one another.22,23 It is very important that movement specialists do not fall into the same trap as medicine in the past and look at movement from only a biomechanical, muscular, neurological, cardiopulmonary, or integumentary system perspective. They must consider the interaction among systems and their subsystems within an individual. For example, the motor system is a system in and of itself. But cognitive impairment and limbic network involvement can lead to tremendous errors in motor responses even when the motor system is intact. In our clients with CNS dysfunction, impairments exist in the motor and limbic network and in cognition, thus creating the potential for a complex set of behavioral responses to internal or external environmental influences.
The concept of patient/client-centered therapy has evolved to become an important aspect of health care delivery.24–34 The desire to improve or regain function can be self-motivated, but very often it is instilled through the clinician to the patient that his or her best interests and unique goals are the focus of the health care team. This belief is based on trust, hope, and attainable steps toward desired and realistic goals. Patients know that their desires, interests, and needs as unique and valued members of society are considered. They first believe and then recognize that they are persons with specific problems and desired outcomes. Although they may have specific medical diagnoses, be placed on clinical pathways, administered drugs, and sent off to the next facility in a couple of days, patients need to feel that they, as individuals, have not lost all individuality and that someone cares. That need is a feeling of security and safety that bonds a patient to a therapist along the journey of learning.35–37
Before understanding and becoming compassionate regarding the needs of other people, such as patients with signs and symptoms of neurological problems, therapists need to understand their own limbic network and how it affects others who might interact with them.38–43 Because both occupational and physical therapy professions have evolved to using enablement models and systems interactions to explain movement responses of their respective client populations, separating limbic from true motor or cognitive impairments will help guide the clinician toward intervention strategies that will lead to the quickest and most effective outcomes.
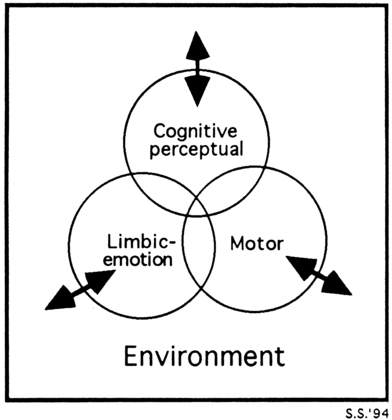
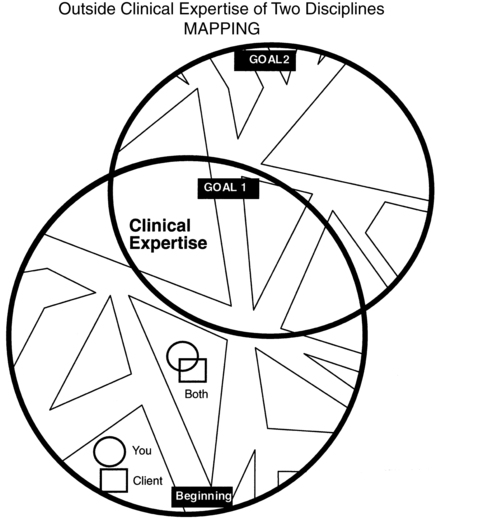
The complexity of the limbic anatomy, physiology, and neurochemistry baffles the minds of basic science doctoral students. The changes in understanding of cellular metabolism, membrane potentials, and the new mysteries of cell communication and memory perplex the world of science and neuroscience.44–47 How this microcosm relates to the macroworld and how the external environments influence not only consciousness but all levels of CNS function are slowly unraveling but still remain mysteries. Yet a therapist deals with the limbic network of clients on a moment-to-moment functional level throughout the day. Figure 5-1 illustrates the interlocking co-dependency of all major CNS components with the environment. At no time does any system stand in isolation. Thus from a clinical perspective the therapist should always maintain focus on the whole environment and all major interactive components within it, while directing attention to any specific component. How the feedback (internal and external) to the patient’s CNS changes the neurochemistry and membrane potential, triggers memory, creates new pathways, or elicits other potential responses is not the responsibility of the clinician or therapist. The responsibility of the clinician is accurate documentation of changes and consistency of those changes toward desired patient outcomes. The professions that focus on movement science are interacting more closely with the neurosciences and other biological sciences and many related professions to unravel many of these mysteries and create better assessment and intervention procedures for future patients.
The primary purpose of this chapter is to discuss the influence of the limbic network on motor learning, motor performance, neuroplasticity, and functional independence in life activities. If a person is fearful or apprehensive, motor performance and the ability to learn either a motor skill or intellectual information will be very different48–55 from that of an individual who feels safe, is given respect, and becomes part of the decision-making process and thus functions inherently with control.52,56–61
An individual will naturally have feelings of loss and reservations or fears about the unknown future after injury to any part of the body, but especially the CNS (see Chapter 6). Yet that individual needs to be willing to experience the unknown to learn and adapt. The willingness, drive, and adaptability of that individual will affect the optimal plasticity of the CNS.62 The limbic network is a key player that drives and motivates that individual. The lack of awareness of that variable or its effect on patient performance will ultimately lead to questions and doubts about the effectiveness and efficacy of both assessment and intervention results. Similarly, if this system is overwhelmed either internally or externally, it will dramatically affect neuroplasticity and motor learning as well as cognitive, syntactical learning (see Chapter 4). At the conclusion of this chapter it is hoped that therapists will comprehend why there is a need to learn to modulate or neutralize the limbic network so that patients can functionally control movement and experience cognitive learning. Then therapists need to reintroduce emotions into the activity and allow the patient to once again experience movement and cognitive success during various levels of emotional demands and environments. This change in the emotional environment will create novelty of the task. This novelty is a critical motivator for learning and will drive neuroplasticity.63–65
The functional relationship of the limbic network to clinical performance
The limbic network’s role in motor control, memory, and learning
It is not easy to find a generally accepted definition of the “limbic network or complex,” its boundaries, and the components that should be included. Mesulam66 likens this to a fifth-century bce philosopher’s quotation, “the nature of God is like a circle of which the center is everywhere and the circumference is nowhere.” Brodal67 suggests that functional separation of brain regions becomes less clear as we discover the interrelatedness through continuing research. He sees the limbic network reaching out and encompassing the entire brain and all its functional components and sees no purpose in defining such subdivision. Although the anatomical descriptions of the limbic network may vary from author to author, the functional significance of this system is widely acknowledged in defining human behavior and behavioral neurology.68
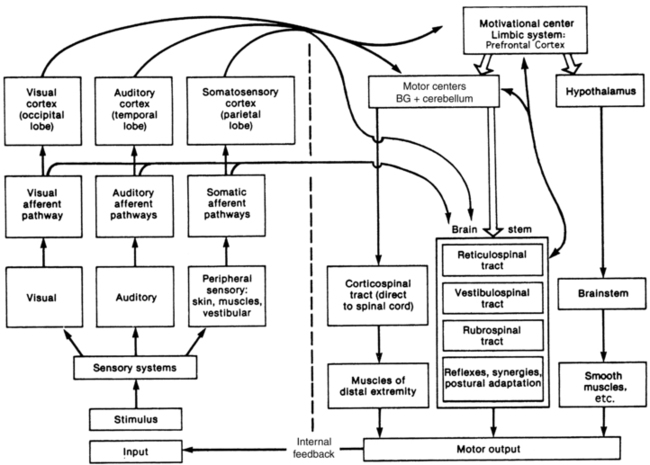
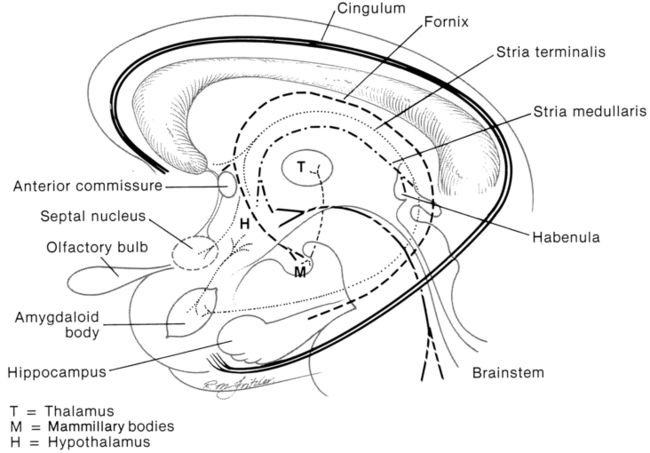
Brooks69 divides the brain into the limbic brain and the nonlimbic sensorimotor brain. He also defines the two limbic and nonlimbic systems functionally, not anatomically, because their anatomical separation according to function is almost impossible and task specific (Figure 5-2). The sensorimotor portion is involved in perception of nonlimbic somatosensory sensations and motor performance. Brooks defines the limbic brain component as primitive and essential for survival, sensing the “need” to act. The limbic brain is also responsible for memory and the ability to select what to learn from each experience, either positive or negative. Thus the overall purpose of the limbic network is to initiate need-directed motor activity for survival, based on experience. The limbic network therefore initiates and can send neurons up to the frontal lobe or down to the brainstem and thus regulates motor output.
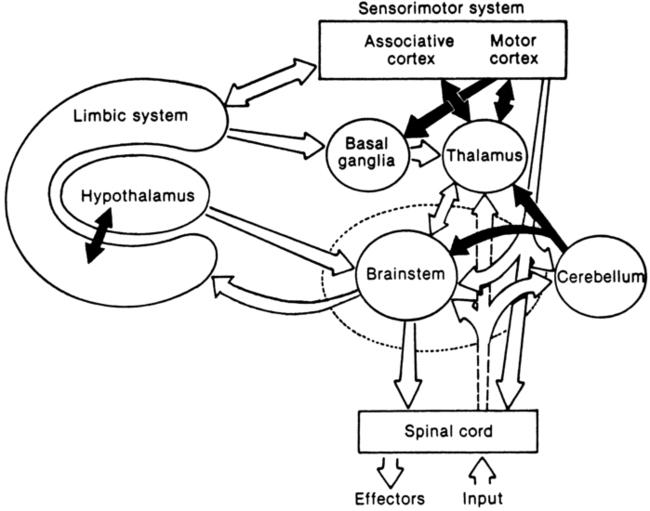
 Divisions and interconnections between the limbic and nonlimbic cortices (sensory and motor areas).
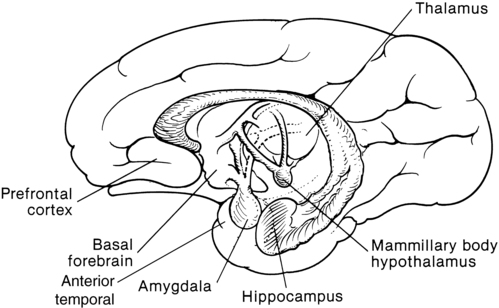
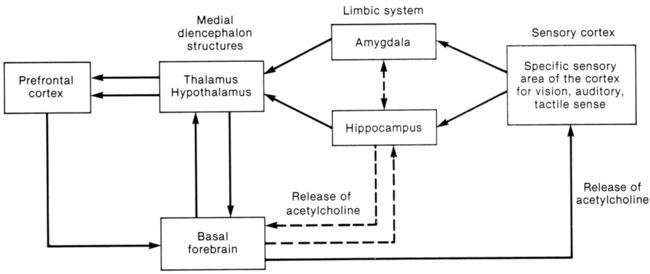
Divisions and interconnections between the limbic and nonlimbic cortices (sensory and motor areas).Kandel and colleagues56 state that functional behavior requires three major systems: the sensory, the motor, and the motivational or limbic systems. When a seemingly simple action, such as swinging a golf club, is analyzed, the sensory system is recruited for visual, tactile, and proprioceptive input to guide the motor systems for precise, coordinated muscle recruitment and postural control. The motivational (limbic) system does the following: (1) provides intentional drive for the movement initiation, (2) integrates the total motor input, and (3) modifies motor expression accordingly, influencing both the autonomic and the somatic sensorimotor systems. It thereby plays a role in controlling the skeletal muscles through input to the frontal lobe and brain stem and the smooth muscles and glands through the hypothalamus, which lies at the “heart” of the limbic network (Figure 5-3).
Noback and co-workers70 state that the limbic network is involved with many of the expressions that make us human; namely, emotions, behaviors, and feeling states. That humanness also has individuality. Our unique memory storage, our variable responses to different environmental contexts, and our control or lack thereof over our emotional sensitivity to environmental stimuli all play roles in molding each one of us. Because of this uniqueness, each therapist and each client need to be accepted for their own individuality.
Broca71 first conceptualized the anatomical regions of the limbic lobe as forming a ring around the brain stem. Today, neuroanatomists do not differentiate an anatomical lobe as limbic, but rather refer to a complex system that encompasses cortical, diencephalon, and brain stem structures.56 This description is less precise and encompasses but is not limited to the orbitofrontal and prefrontal cortex, hippocampus, parahippocampal gyrus, cingulate gyrus, dentate gyrus, amygdaloid body, septal area, hypothalamus, and some nuclei of the thalamus.56,72–76 Anatomists stress the importance of looking at the interrelated structures and segments or loops within the complex limbic region.77,78
These multiple nuclei and interlinking circuits play crucial roles in behavioral and emotional changes77,79,80 and declarative memory.79–96 The loss of any link can affect the outcome activity of the whole circuit. Thus damage to any area of the brain can potentially cause malfunctions in any or all other areas, and the entire circuit may need reorganization to restore function.
Researchers do not ascribe a specific single function to CNS formations but see each as part of a system participating to various degrees in the multitude of behavioral responses (see Chapters 3 and 4 for additional information). Therefore the loss of any part of higher centers or the limbic network may not be clearly definable functionally, and the return of function is not always easy to predict.
Recovery of function after injury may involve mechanisms that allow reorganizing of the structure and function of cortical, subcortical, and spinal circuits. In very young infants, areas within opposite hemispheres may “take over” function, whereas in more mature brains reorganization of existing systems seems to be the current accepted hypothesis within the expanding knowledge of neuroplasticity.97–100 For complex behavior, such as in motor functioning requiring many steps, the limbic network, cortex, hypothalamus, basal ganglia, and brain stem work as an integrated unit, with any damaged area causing the whole system to initially malfunction. Without change or encouragement of appropriate external and internal environmental changes that will create neuroplasticity, the initial malfunction can become permanent.101 The timing for optimal neuroplasticity has not yet been established. The medical use of drugs to alter cellular activity and plasticity after CNS damage has become a huge pharmaceutical research area (see Chapter 36). Early as well as later drug therapy may encourage neuroplasticity.102–108 The same questions must be asked about early instead of later rehabilitation intervention, as well as the limbic influence over the motor system. A loss of function or a change in behavior cannot necessarily be localized as to the underlying cause. A lesion in one area may cause secondary dysfunction of a different area that is not actually damaged.
The limbic network’s influence on behavior: its relevance to the therapeutic environment
Levels of behavioral hierarchies: where does the limbic network belong?
Strub and Black109 view behavior as occurring on distinct interrelated levels that represent behavioral hierarchies. Starting at level 1, a state of alertness to the internal and external environment must be maintained for motor or mental activity to occur. The brain stem reticular activating system brings about this state of general arousal by relaying in an ascending pathway to the thalamus, the limbic network, and the cerebral cortex. To proceed from a state of general arousal to one of “selective attention” requires the communication of information to and from the cortex, the thalamus, and the limbic network and its modulation over the brain stem and spinal pattern generators.56,110
On level 3 only cerebral cortical areas are activated. This level deals with abstract conceptualization of verbal or quantitative entities. It is at this level that the somatosensory and frontal motor cortices work together to perceptually and procedurally develop motor programs. The prefrontal areas of the frontal lobe can influence the development of these motor programs, thus again illustrating the limbic influence over the motor system.111,112
Level 4 behavior is concerned with the expression of social aspects of behavior, personality, and lifestyle. Again, the limbic network and its relationship to the frontal lobe are vital. The shift to the World Health Organization International Classification of Functioning, Disability and Health (WHO-ICF) model, which reflects patient-centered therapy, has actualized the critical importance of this level of human behavior.24,28,31,113,114
As Western medicine is unraveling the mysteries behind the neurochemistry of the limbic network58,115–117 and alternative medicine is establishing effectiveness and efficacy for various interventions and philosophies (see Chapter 39), a fifth level of limbic function may become the link between the hard science of today and the unexplained mysteries. Those medical mysteries would be defined as unexplained yet identified events that have either been forgotten or been hidden from the world by those scientists—mysteries such as why some people heal from terminal illnesses spontaneously, various others heal in ways not accepted by traditional medicine,60,118 and still others just die without any known disease or pathological condition.119–122 One critical component everyone identifies as part of that unexplained healing is a belief by the client that he or she will heal. That belief has a strong emotional component,120 and that may be the fifth level of limbic function. How conscious intent drives hypothalamic autoimmune function is being unraveled scientifically, and clinicians often observe these changes in their patients. Through observation it becomes apparent that clients who believe they will get better often do, and those who believe they will not generally do not. Whether belief comes from a religious, spiritual, or hard science paradigm, that belief drives behavior, and that drive has a large limbic component.
The limbic network moves us
Moore123 eloquently describes the limbic network as the area of the brain that moves us. The word MOVE can be used as a mnemonic for the functions of the limbic network.
Limbic network function.
Memory: attention and retrieval, declarative learning
Motivation: desire to learn, try, or benefit from the external environment
Olfaction (especially in infants)
Only sensory system that does not have to go through the thalamus as a second-order synapse in the sensory pathway before it gets to the cerebral cortex
Visceral (drives: thirst, hunger, and temperature regulation; endocrine functions)
As seen in this outline, the M (memory, motivation) depicts the drive component of the limbic network. Before learning, an individual must be motivated to learn, to try to succeed at the task, to solve the problem, or to benefit from the environment. Without motivation the brain will not orient itself to the problem and learn. Motivation drives both our cortical structures to develop higher cognitive associations and the motor system to develop procedures or motor programs that will enable us to perform movement with the least energy expenditure and the most efficient patterns available. Once motivated, the individual must be able to pay attention and process the sequential and simultaneous nature of the component parts to be learned, as well as the whole. Thus there is an interlocking dependence among somatosensory mapping of the functional skills124 (cognitive), attention (limbic) necessary for any type of learning, and the sequential, multiple, and simultaneous programming of functional movement (motor). The limbic amygdala and hippocampal structures and their intricate circuitries play a key role in the declarative aspect of memory.125–128 Once this syntactical, intellectual memory is learned and taken out of short-term memory by passing through limbic nuclei, the information is stored in cortical areas and can be retrieved at a later time without limbic involvement.129
The O refers to olfaction, or the incoming sense of smell, which exerts a strong influence on alertness and drive. This is clearly illustrated by the billions of dollars spent annually on perfumes, deodorants, mouthwashes, and soap as well as scents used in stores to increase customers’ desires to purchase. This input tract can be used effectively by therapists who have clients with CNS lesions such as internal capsule and thalamic involvement. The olfactory system synapses within the olfactory bulb and then with the limbic structures and then may go directly to the cerebral cortex without synapsing in the thalamus. Although collaterals do project to the thalamus, unlike all other sensory information, olfaction does not need to use the thalamus as a necessary relay center to access the cortical structures, although many collaterals also project there.56,130 Other senses may not be reaching the cortical levels, and the client may have a sensory-deprived environment. Olfactory sensations, which enter the limbic network, may be used to calm or arouse the client. The specific olfactory input may determine whether the person remains calm or emotionally aroused.131,132 Pleasant odors would be preferable to most people. With the limbic network’s influence on tone production through brain stem modulation, this is one reason aromatherapy causes relaxation and is used by many massage therapists.
A comatose, seemingly nonresponsive client may respond to or be highly sensitive to odor.133 The therapist needs to be acutely aware of the responses of these patients because these responses may be autonomic instead of somatomotor and may be reflected in a higher heart rate or an increase in blood pressure. Using noxious stimuli to try to “wake up” a patient in a vegetative state has the possibility of causing negative arousal, fear, withdrawal, or anxiety and an increase in base tone within the motor generators.132 Using this type of input places the patient at level 2 in a “protective state of survival.” Using a pleasant and personal desirable smell will more likely place a client at level 2 “safety.” The former can lead to strong emotions such as anger, whereas the latter often leads to bonding and motivation to learn. Research has shown that retrieval processing and retrieval of memory have a distinctive emotionality when they are linked to odor-evoked memories.134–136
The V represents visceral or autonomic drives. As noted earlier, the hypothalamus is nestled within the limbic network. Thus, regulation of sympathetic and parasympathetic reactions, both of the internal organ systems and the periphery, reflects continuing limbic activity. Obviously, drives such as thirst, hunger, temperature regulation, and sexuality are controlled by this system. Clients demonstrating total lack of inhibitory control over eating or drinking or manifesting very unstable body temperature regulation may be exhibiting signs of hypothalamic-pituitary involvement or direct pathways from hypothalamus to midbrain structures.56 Today, this interaction of the hypothalamus with motor neurons that change or support movement has clearly been established.137
If the sensory input to the client is excessive whether through internal or external feedback, the limbic network may go into an alert, protective mode and will not function at the optimal level, and learning will diminish. The client may withdraw physically or mentally, lose focus or attention, decrease motivation, and become frustrated or even angry. The overload on the reticular system may be the reason for the shutdown of the limbic network and not the limbic network itself. Both are part of the same neuroloop circuitry. All these behaviors may be expressed within the hypothalamic-autonomic system as motor output, no matter where in the loop the dysfunction occurs. Having a functional understanding of the neuroanatomy and their relationships with each other helps therapists unravel some of the mysteries patients present after CNS insult.138,139 The evaluation of this system seems even more critical when a client’s motor control system is locked, with no volitional movement present. Therapists often try to increase motor activity through sensory input; however, they must cautiously avoid indiscriminately bombarding the sensory systems. The limbic network may demonstrate overload while at the same time the spinal motor generators reflect inadequate activation. How a therapist might assess this overload would be to closely monitor the ANS’s responses such as blood pressure, heart rate, internal temperature, and sweating versus observing or measuring muscle tone. Although the somatosensory system and the ANS are different, they are intricately connected. The concept of massively bombarding one system while ignoring the other does not make sense in any learning paradigm, especially from a systems model in which consensus creates the observed behavior. To illustrate this concept, think of an orchestra leader conducting a symphony. It would make no sense for the conductor to ask the string section to play louder if half the brass section got sick. Instead, the conductor would need to quiet the string section and all other sections to allow the brass component to be heard.
E relates to emotions, the feelings, attitudes, and beliefs that are unique to that individual. These beliefs include psychosocial attitudes and prejudices, ethnic upbringing, cultural experiences, religious convictions, and concepts of spirituality.120 All these aspects of emotions link especially to the amygdaloid complex of the limbic network and orbitofrontal activity within the frontal lobe.140–142 This is a primary emotional center, and it regulates not only our self-concept but our attitudes and opinions toward our external environment and the people within it.
To appreciate the sensory system’s influential interaction with the limbic network directly, the reader need only look at the literature on music and how it interacts with emotions.143,144 Most people can give examples of instances where music has elicited immediate and compelling emotional responses of various types. Pleasant and unpleasant musical stimuli have been found to increase or decrease limbic activity and influence both cognitive and motor responses. Although the neurological mechanisms are not yet well understood, the limbic network seems to be implicated in both “positive” and “negative” emotions in response to musical stimuli.145–148 The clinical implications are huge. Excessive noise, loudspeaker announcements, piped in music, and all the therapists’ voices can affect the CNS of a client. These responses can be highly emotional, cause changes in visceral behavior, and affect striated motor expression. Level of musical consonance or dissonance is just one element of the auditory stimulus that is subjectively experienced by the listener as pleasant or unpleasant. The implications not only that listening to music affects limbic emotional states but that the influence may direct the hypothalamus in regulation of blood flow within the CNS have also been shown.148 With music or sound being just one input system, the therapist must realize that sensory influence from smell, taste, touch, proprioception, and vestibular and organ system dysfunction can lead to potential limbic involvement in all aspects of CNS function and directly affect the emotional stability of the patient.
A second self-concept deals with my attitude about my worth or value to society and the world and my role within it.149 Again, this attitude can change with mood, but more often it seems to change with experience. This aspect of client-therapist interaction can be critical to the success of a therapeutic environment. The two following examples illustrate this point, with the focus of bringing perceived roles into the therapeutic setting:
Your client is Mrs. S., a 72-year-old woman with a left cerebrovascular accident (CVA). She comes from a low socioeconomic background and was a housekeeper for 40 years for a wealthy family of high social standing. When addressing you (the therapist), she always says “yes, ma’am” or “no, ma’am” and does just what is asked, no more and no less. It may be very hard to empower this client to assume responsibility for self-direction in the therapeutic setting. Her perceived role in life may not be to take responsibility or authority within a setting that may, from her perception, have high social status, such as a medical facility. She also may feel that she does not have the right or the power to assume such responsibilities. Success in the therapeutic setting may be based more on changing her attitudes than on her potential to relearn motor control. That is, the concept of empowerment may play a crucial role in regaining independent functional skill and control over her environment.24,28,31,150–153
Your client is a 24-year-old lumberjack who sustained a closed-head injury during a fall at work. It is now 1 month since his accident, and he is alert, verbal, and angry and has moderate to severe motor control problems. During your initial treatment you note that he responds very well to handling. He seems to flow with your movement, and with your assistance is able to practice a much higher level of motor control within a narrow biomechanical window; although at times he needs your assistance, you release that control whenever possible to empower him to control his body. At the end of therapy he sits back in his chair with much better residual motor function. Then he turns to you (the female therapist) and instead of saying, “That was great,” he says, “You witch, I hate you.” The inconsistency between how his body responded to your handling and his attitude toward you as a person may seem baffling until you realize that he has always perceived himself as a dominant male. Similarly, he perceives women as weak, to be protected, and in need of control. If his attitude toward you cannot be changed to see you in a generic professional role, he will most likely not benefit as much from your clinical skills and guidance as a teacher. Before the accident the patient may have suppressed that verbal response but not tone and body language. After a traumatic brain injury affecting the orbitofrontal system, the inhibition of the behavioral response itself may be lost, further embarrassing the patient emotionally.
Preconceived attitudes, social behaviors, and opinions have been learned by filtering the input through the limbic network. If new attitudes and behaviors need to be learned after a neurological insult, the status of the amygdaloid pathways seems crucial. Damage to these limbic structures may prevent learning154; thus, socially maladaptive behavior may persist, making the individual less likely to adapt to the social environment. It is often harder to change learned social behaviors than any other type of learning.155–158 Because our feelings, attitudes, values, and beliefs drive our behaviors through both attention and motor responses, the emotional aspect of the limbic network has great impact on our learning and motor control. If a patient is not motivated and places little value on a motor output, then complacency results and little learning will occur.159–161 On the other hand, if a therapist places an extremely high value on a motor output as a pure expression of motor control without interlocking that control with the patient’s limbic influence, the behavioral response may lead to inconsistency, lack of compliance, and thus lack of motor learning and carryover.159 Similarly, it can cause extreme stress, which even the general public knows causes disease.162
Motivation and reward.
Moore123 considers motivation and memory as part of the MOVE system. Esch and Stefano163 link motivation with reward and help, illustrating how the limbic network learns through repetition and reward. They state that the concept of motivation includes drive and satiation, goal-directed behavior, and incentive. They recognize that these behaviors maintain homeostasis and ensure the survival of the individual and the species. Although the frontal lobe region appears to play an important role in self-control and execution activities, these functions seem to require a close interlocking neuronetwork between cognitive representation within the frontal regions and motivational control provided by limbic and subcortical structures.140,164 An important aspect of motivated behavior is linked to patient- and family-centered therapy.* “The most powerful force in rehabilitation is motivation.”167 These words are strong and reflect the importance of the limbic network in rehabilitation.
Motivated behavior is geared toward reinforcement and reward, which are based on both internal and external feedback systems. Repeated experience of reinforcement and reward leads to learning, changed expectancy, changed behavior, and maintained performance.168 Emotional learning, which certainly involves the limbic network, is very hard to unlearn once the behavior has been reinforced over and over.169,170 For that reason, motor behavior that is strongly linked to a negative emotional response might be a very difficult behavior to unlearn. For example, a patient who is willing to stand up and practice transfers just to get the therapist off his back is eliciting a movement sequence that is based on frustration or anger. When that same patient gets home and his spouse asks him to perform the same motor behavior, he may not be able to be successful. The spouse may say, “The therapist said you could.” The patient may respond, “I never did like him!” Thus repetition of motor performance with either the feeling of emotional neutrality or the feeling of success (positive reinforcement) is a critical element in the therapeutic setting. Consistently making the motor task more difficult just when the client feels ready to succeed will tend to decrease positive reinforcement or reward, lessen the client’s motivation to try, and decrease the probability of true independence once the patient leaves the clinical setting. When pressure is placed on therapists to produce changes quickly, repetition and thus long-term learning are often jeopardized, which may have a dramatic effect on the quality of the client’s life and the long-term treatment effects once he or she leaves the medical facility. Motor control theory (see Chapter 4) coincides with limbic research regarding reinforcement. Inherent feedback within a variety of environmental contexts allowing for error with correction leads to greater retention.171 Repetition or the opportunity to practice a task (motor or cognitive) in which the individual desires to succeed will lead to long-term learning.172 Without practice or motivation the chance of successful motor learning is minimal to nonexistent.
Positive emotional states may create a limbic environment in which the therapist can link reward and pleasure associations to new motor sequences. Although it is well known that appropriate selections of music can stimulate states of highly pleasant positive affects and physical relaxation, the neurological mechanisms for these effects are not well understood. In an early study by Goldstein173a subjects reported pleasant physical sensations of tingling or “thrills” in response to music listening. After subjects were injected with naloxone, which blocks opiate receptors, thrill scores and tingling sensations were attenuated in some subjects. Although responses to music are highly individualized and this study has not been replicated, it suggests that endorphins may be released under certain music listening conditions that elicit pleasant physical sensations. In a positron emission tomography (PET) study of cerebral blood flow (CBF) changes measured during highly pleasurable “shivers or chills” in response to subject-selected music, Blood and colleagues147 found that as the intensity of the chills increased, CBF increases occurred in the left ventral striatum, dorsomedial midbrain, bilateral insula, right orbitofrontal cortex, thalamus, anterior cingulate cortex, supplementary motor area, and bilateral cerebellum. As the intensity of chills increased, significant CBF decreases were also observed in the right amygdala, left hippocampus and amygdala, and ventral medial prefrontal cortex. The increases found in brain structures associated with reward or pleasant emotions and decreases in areas associated with negative emotional states suggest that music (1) must be carefully selected according to individual preferences and responses, in order to reliably elicit such highly pleasurable experiences as “shivers down the spine” and (2) might be used therapeutically to positively affect limbic activity.
Other studies provide additional support for the notion that music may activate limbic and paralimbic areas associated with reward or pleasurable emotions. Brown and colleagues145 conducted a PET study of 10 nonmusicians who listened passively to unfamiliar music, which they later reported had elicited strongly pleasant feelings. Unlike previous studies of music, emotion, and limbic activity, this research design called for subjects to listen passively without engaging in any task such as evaluating affective components during the music. The authors noted that the music stimuli used was musically complex and strongly liked by the subjects. When the CBF during the music was compared with silent rest conditions in the same subjects, activations were seen, as expected, in areas presumed to represent perceptual and cognitive responses to music (primary auditory cortex, auditory association cortex, superior temporal sulcus bilaterally, temporal gyrus of the right hemisphere, in the right superior temporal pole, and adjacent insula). In addition, responses were found in limbic and paralimbic areas, which included the left subcallosal cingulate, the anterior cingulate, left retrosplenial cortex and right hippocampus, and the left nucleus accumbens and cerebellum. The researchers compared these results with those from the earlier studies by members of the same team147,148 and suggest that areas such as the subcallosal cingulate are related to the direct experience of occurrent emotions rather than discriminate processing for emotion and that different areas are specifically activated during the pleasant physical responses known as “chills.” They go on to propose that the superior temporal pole and adjacent insula may serve as a point of bifurcation in neural circuitry for processing music. They also suggest that neurons from that region project to limbic and paralimbic areas involved in emotional processing and to premotor areas possibly involved in discrimination and structural processing of music. Although research has increased our appreciation of the complexity of brain activation by music, much more study is needed to validate a model of limbic network activity in human emotional responses to musical stimuli. Clinically, music can be used to improve mood and increase patient motivation to participate in rehabilitation treatment. Case studies174,175 suggest that music can be used to decrease crying by infants and toddlers during physical therapy treatment. West has participated in both developmental and rehabilitation settings as a music therapist in co-treatment with physical and occupational therapists. The music therapist first does a thorough assessment of the individual’s preferences and responses to music, then provides music selected or composed specifically to provide motivating energy, pleasant associations, and positive affective states to accompany the motor activity. This individualized, live-music approach allows the music therapist to modify the musical elements as needed in the moment, working in a real-time limbic partnership with both the client and the physical or occupational therapist. Music or pleasure sounds can be used to help neutralize or balance the limbic influence on motor expression. Obtaining a limbic-neutral impact is critical before evaluating functional movement in order to accurately determine true motor system involvement.
Many types of emotions create motivation, such as pleasure, reward processes, emotions associated with addiction, appreciation of financial benefits, amusement, sadness, humor, happiness, and depression.163,173b,176–179 Some emotions tend to drive learning, whereas others may discourage learning, whether that learning be cognitive or motor.
Integration of the limbic network as part of a whole functioning brain
Motivation, alertness, and concentration are critical in motor learning because they determine how well we pay attention to the learning and execution of any motor task. These processes of learning and doing are inevitably intertwined: “We learn as we do, and we do only as well as we have learned.”180
Both motivation (“feeling the need to act”) and concentration (“ability to focus on the task”) are interlinked with the limbic network. The amygdaloid complex with its multitude of afferent and efferent interlinkages is specially adapted for recognizing the significance of a stimulus, and it assigns the emotional aspect of feeling the need to act. These neuroanatomical loops have tremendous connections with the reticular system. Hence, some authors call it the reticulolimbic network.56,157 The interaction of the limbic network and the motor generators of the brain stem and ultimate direct and indirect modulation over the spinal system lead to need-directed and therefore goal-directed motor activity. It also filters out significant from insignificant information by selective processing and storing the significant for memory, learning, and recall. These interconnected neuroloop circuitries reinforce the concept that areas have both specialization and generalization and thus work closely together with other areas of the brain.169,181
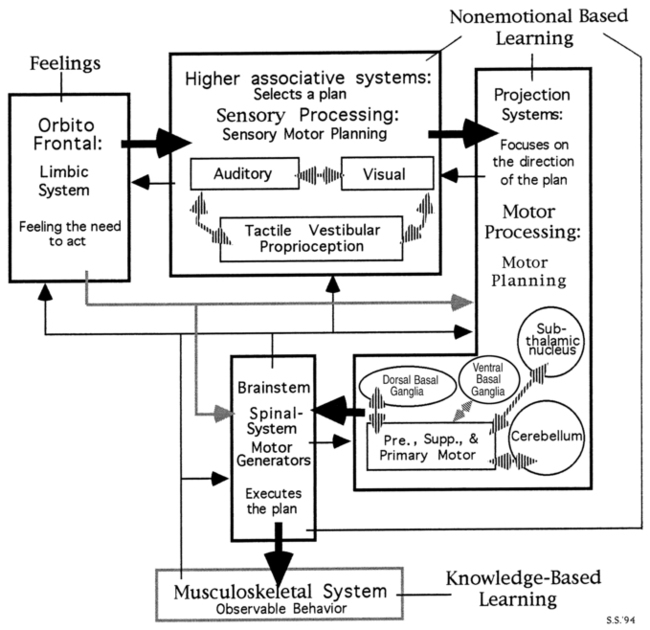
Goal-directed or need-directed motor actions are the result of the nervous system structures acting as an interactive system. Within this system (Figure 5-4), all components share responsibilities. The limbic network and its cortical and subcortical components represent the most important level. In response to stimuli from the internal or external environment, the limbic network initiates motor activity out of the emotional aspect of feeling the need to act. This message is relayed to the sensory areas of the cerebral cortex, which could entail any one or all association areas for visual, auditory, olfactory, gustatory, tactile, or proprioceptive input. These areas are located in the prefrontal, occipital, parietal, and temporal lobes, where they analyze and integrate sensory input into an overall strategy of action or a general plan that meets the requirements of the task. Therefore these cortices recognize, select, and prepare to act as a response to relevant sensory cues when a state of arousal is provided by reticular input. The limbic cortex (uncus, parahippocampal gyrus /isthmus, cingulate gyrus, and septal nucleus) has even greater influence over the sensorimotor cortices through the cingulate gyrus, both directly and indirectly through association areas.182–184 The thalamus, cerebellum, and basal ganglia contribute to the production of the specific motor plans. These messages of the general plan are relayed to the projection system. The limbic structures through the cingulate gyrus also have direct connections with the primary motor cortex. These circuits certainly have the potential to assist in driving fine motor activities through corticobulbar and corticospinal tract interactions. The thalamus, cerebellum, basal ganglia, and motor cortices (premotor, supplementary motor, and primary motor) contribute to the production of the specific motor plans.56 Messages regarding the sensory component of the general plan are relayed to the projection system, where they are transformed into refined motor programs. These plans are then projected throughout the motor system to modulate motor generators throughout the brain stem and spinal system.56 Limbic connections with (1) the cerebellum, basal ganglia, and frontal lobe56,185–189 and (2) the motor generator within the brain stem enable further control of limbic instructions over motor control or expression. If the limbic and the cognitive systems decide not to act, goal-driven motor behavior will cease. An individual’s belief (emotional and spiritual) can inhibit even the most basic survival skills, as has been clearly shown in history when individuals with particular religious beliefs were pitted against vicious predators and those people chose not to defend themselves.
Within the projection system and motor planning complexes, the specifics are programmed and the tactics are given a strategy. In general, “what” is turned into “how” and “when.” The necessary parameters for coordinated movement are programmed within the motor complex as to intensity, sequencing, and timing to carry out the motor task. These programs, which incorporate upper motor neurons and interneurons, are then sent to the brain stem and spinal motor generators, which in turn, through lower motor neurons, send orders regarding the specific motor tasks to the musculoskeletal system. (See Chapters 3, 4, and 8 for more specific in-depth discussion.) The actions performed by each subsystem within the entire limbic–motor control complex constantly loop back and communicate to all subsystems to allow for adjustments of intensity and duration and to determine whether the plan remains the best choice of responses to an ever-changing three-dimensional world.138,186,187
The limbic network has one more opportunity to modify and control the central pattern generators and control the body and limbs through direct connections to the spinal neuronetwork.110,190–193 That is, the limbic network can alter existing motor plans by modulating those generators up and down or altering specific nuclear clusters and varying the patterns themselves. Therapists as well as the general public see this in sports activities when emotions are high, no matter the emotion itself. Individuals who have excellent motor control over a specific sport may find high-level performance difficult as the stress of competition increases. Having control over emotional variance as well as motor variance with a functional activity is an accurate example of empowerment. Thus, for a therapist to get a true picture of a patient’s motor system’s function, the limbic network should be flowing in a neutral or balanced state without strong emotions of any kind. Generally, that balance seems to reflect itself in a state of safety, trust, and compliance. Once the motor control has been achieved then the therapist must reintroduce various emotional environments during the motor activity to be able to state that the patient is independent.
In summary, the limbic complex generates need-directed motor activity and communicates that intent throughout the motor system.110,191,194,l95 This step is vital to normal motor function and thus client care. Clients need the opportunity to analyze correctly both their internal environment (their present and feed-forward motor plans and their emotional state) and the external world around them requiring action on a task. The integration of all this information should produce the most appropriate strategy available to the patient for the current activity. These instructions must be correct, and the system capable of carrying out the motor activity, for effortless, coordinated movement expression to be observed. If the motor system is deficient, lack of adaptability will be observed in the client. If the limbic complex is faulty, the same motor deficits might present themselves. The therapist must differentiate what is truly a motor system problem versus a limbic influence over the motor system problem.
Schmidt196 stresses the significance of “knowledge of results feedback” as being the information from the environment that provides the individual with insights into task requirements. This insight helps the motor system correctly select strategies that will successfully initiate and support the appropriate movement for accomplishing the task. This knowledge of results feedback is required for effective motor learning and for forming the correct motor programs for storage.197,198
Brooks69 distinguishes insightful learning, which is programmed and leads to skills when the performer has gained insight into the requirements, from discontinuous movements, which need to be replaced by continuous ones. This process is hastened when clients understand and can demonstrate their understanding of what “they were expected to do.” Improvement of motor skills is possible by using programmed movement in goal-directed behavior. The reader must be cautioned to make sure that the client’s attention is on the goal of the task and not on the components of the movement itself. The motor plan needs programming and practice without constant cognitive overriding. The limbic/frontal system helps drive the motor toward the identified task or abstract representation of a match between the motor planning sequence and the desired outcome. The importance of the goal being self-driven by the patient cannot be overemphasized.*
Without knowledge of results, feedback, and insight into the requirements for goal-directed activity, the learning is performing by “rote,” which merely uses repetition without analysis, and meaningful learning or building of effective motor memory in the form of motor holograms will be minimal. Children with cognitive and limbic deficits can learn basic motor skills through repetition of practice, but the insights and ability to transfer that motor learning into other contexts will not be high (see Chapters 12, 13, and 14).
Schmidt196 suggests that to elicit the highest level of function within the motor system and to enable insightful learning, therapy programs should be developed around goal-directed activities, which means a strong emotional context. These activities direct the client to analyze the environmental requirements (both internal and external) by placing the client in a situation that forces development of “appropriate strategies.” Goal-directed activities should be functional and thus involve motivation, meaningfulness, and selective attention. Functional and somatosensory retraining uses these concepts as part of the intervention (see Chapters 4 and 9). Specific techniques such as proprioceptive neuromuscular facilitation, neurodevelopmental therapy, the Rood method, and the Feldenkrais method can be incorporated into goal-directed activities in the therapy programs, as can any treatment approach, as long as it identifies those aspects of motor control and learning that lead to retention and future performance and allows the patient to self-correct.196 With insights into the learned skills, clients will be better able to adjust these to meet the specific requirements of different environments and needs, using knowledge of response feedback to guide them. The message then is to design exercise activities or programs that are meaningful and need directed, to motivate clients into insightful goal-directed learning. Thus, understanding the specific goals of the client, patient-centered learning, is critical and will be obtained only by interaction with that client as a person with needs, desires, and anticipated outcomes.201,202 A therapist cannot assume that “someone wants to do something.” The goal of running a bank may seem very different from that of birdwatching in the mountains, yet both may require ambulatory skills. If a client does not wish to return to work, then a friendly smile and the statement, “Hi, I’m your therapist and I’m going to get you up and walking so you can get back to work,” may lead to resistance and decreased motivation. In contrast, a therapist who knows the goal of the client may help him or her become highly motivated to ambulate; that client may be present in the clinic every day to meet the goal of birdwatching in the mountains although never wishing to walk back into the office again.
Limbic influence on emotional output: the F2ARV and GAS continua
F2arv (fear and frustration, anger, rage, and violence or withdrawal) continuum.
One sequence of behaviors used to describe the emotional circuitry of the limbic network through the amygdala is the F2ARV continuum157,203,204 (Figure 5-5). This continuum begins with fear or frustration. This fear can lead to avoidance behavior.205 If the event inducing the fear or frustration continues to heighten, avoidance behaviors can continue to develop.205 In a simple example, we recall or have seen these behaviors in our teens and as young adults, when the challenges faced in high school can lead to avoidance of activities. Alternately, extreme fear and frustration can also lead to anger. Anger is a neurochemical response that is perceived and defined cognitively (at the cortical level) as anger. If the neurochemical response continues to build or is prolonged, the anger displayed by the person may advance to rage (internal chaos) and finally into violence (strong motor response). A common societal example is in the case of domestic discord and violence. Women who attain the level of rage may become withdrawn and thus become victimized by a partner who is also in rage or inflicting physical or emotional violence.206 Another current example is posttraumatic stress disorder (PTSD), in which the prolonged stress of deployment and unique challenges of warfare lead to limited adaptive reserves in warriors and returning veterans. Suicide and domestic violence have become a more common occurrence between deployments, necessitating a dramatic shift in mental health policy in the last 5 years.207–210
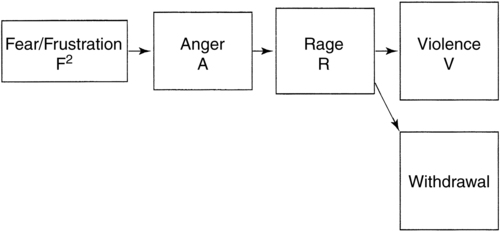
 Fear and frustration, anger, rage, and violence or withdrawal: F2ARV continuum.
Fear and frustration, anger, rage, and violence or withdrawal: F2ARV continuum.How quickly and completely any individual will progress from fear to violence is dependent on several factors. First, the genetic neurochemical predisposition (initial wiring) will influence behavioral responses.204 Second, “soft-wired” or conditioned responses resulting from experiences and reinforced patterns will influence output. For example, it is commonly known that abusive parents were usually abused children203,211; they learned that anger quickly leads to violence and that the behavior of violence was somehow acceptable. Last, the quality and intensity of the stimulus initiating the continuum will influence the level of response.
The neurochemistry within an individual’s CNS, whether inherently active or altered through drugs or injury, will have great influence on the plasticity of the existing wiring.40,212 Repetitive or prolonged exposure to negative environmental stimuli may also lead to a chronically imbalanced neurochemical state that results in a lowered threshold or tolerance to a given stimulus. Chemistry or wiring can become imbalanced from damage, environmental stress, learning, or other potentially altering situations, changing an individual’s control over this continuum.56,106–108,213,214 When neurochemical imbalance exists, these behaviors will persist, and balance may be restored only through natural neurochemical activity (e.g., sleep, exercise, diet, spirituality) or medication support (chemical replacement).
Therapists need to be acutely aware of this continuum in clients who have diffuse axonal shearing within the limbic complex. Diffuse axonal shearing is most commonly seen and reported in research on individuals with head trauma215,216 (see Chapter 24). Resulting lesions within the limbic structures may cause an individual to progress down this continuum at a rapid speed. This point cannot be overemphasized. Patients with an accelerated F2ARV continuum may physically strike out at a clinician or caregiver out of simple frustration during care. Knowing the social history of the client and the causation of the injury often can help the therapist gain insight into how an individual patient might progress down this continuum. Not all head-injured patients had prior difficulty with the F2ARV continuum; however, it is important to note that many individuals received their head injuries in violent confrontational situations or in wartime conflict. Some individuals, primarily females, when confronted with stress, anger, and potential violence from another, will withdraw and become depressed. This behavior, similar to violence, will change the structure of the limbic network.55
Gas (general adaptation syndrome).
The autonomic responses to stress also follow a specific sequence of behavioral changes and are referred to as the general adaptation syndrome.217–223 The sequential stages of GAS are a direct result of limbic imbalance and can play a dramatic role in determining client progress.
This stress or overstimulation syndrome is characterized by common symptoms as described earlier.140,224–231 If the acute symptoms are not eliminated, they will become chronic and the behavior patterns much more resistant to change.
GAS is often seen in the elderly, with various precipitating health crises,221 and also in neonatal high-risk infants (see Chapter 11), victims of head trauma, and other clients with neurological conditions. The initial alarm can be precipitated by moderate to maximal internal instability with less intensive external stress, or by minimal internal instability with severe external sensory bombardment. For instance, in the elderly, stresses such as change of environment, loss of loved ones, failing health, and fears of financial problems can each cause the client’s system to react as if overloaded.223 As another example, individuals with head trauma (Chapter 24), vestibular dysfunction (Chapter 22B), inflammatory CNS problems (Chapter 26), and brain tumors (Chapter 25) often possess hypersensitivity to external input such as visual environments, noise, touch, or light. In these individuals, typical clinical environments and therapeutic activities may create a sensory overload and trigger a GAS response.
Stress, no matter what the specific precipitating incident (confusion, fear, anxiety, grief, or pain), has the potential to trigger the first steps in the sequence of this syndrome.224–229,232 The clinician’s sensitivity to the client’s emotional system will be the therapeutic technique that best controls and reverses the acute condition.
Similarly, patients with dizziness and instability, particularly within visually stimulating environments, can develop feelings of panic, which can evolve into full attacks and agoraphobic responses.233 These individuals avoid participating in activities that put them within visually overstimulating environments in an effort to control the dizziness and prevent the associated autonomic reactions. Similar types of reactions have been documented, such as space-motion discomfort (SMD),234 postural phobic vertigo,233 visual vertigo,235 and dizziness of “psychogenic” origin. Often these individuals are referred first to psychology or psychiatry. However, there is an underlying physiologic explanation for these symptoms. In a majority of individuals with SMD, there is a documented increase in vestibular sensitivity (increased vestibulo-ocular reflex [VOR] gain) and an impairment in velocity storage (shorter VOR time constant).236 In addition, the dorsal raphe nucleus (DRN of the midbrain and rostral pons) is the largest serotonin-containing nucleus in the brain and directly modulates the firing activity of the superior and medial vestibular nuclei. It is this interaction between serotonin and vestibular function that helps to explain the link between vestibular and anxiety disorders. It can also help explain how patients with sleep disorders or other serotonin-depleting disorders develop vestibular-like symptoms and anxiety.237,238
The F2ARV and GAS continua are often interrelated in individuals who have direct or indirect limbic network involvement. The therapist needs to be aware that a patient may overrespond to stress, frustration, or fear of failure in both cognitive and motor activities. The initial response may be an escalation of the F2ARV continuum with what then seems like a rapid withdrawal or a heightened state of anger (GAS). There are many ways to help the patient balance these autonomic reactions and continue to learn within the therapeutic setting. The Bonny Method of Guided Imagery and Music is a music-centered psychotherapy method that has been used extensively with individuals recovering from various types of trauma.239–242 In reviewing specific Bonny Method treatment approaches used with trauma patients, Körlin242 describes a cyclical process whereby an important initial treatment period emphasizes the mobilization of inner resources, alleviating vulnerability and increasing the patient’s self-confidence. This phase uses carefully selected music that elicits positive limbic states and “bodily manifestations with qualities of warmth, energy, strength, movement, nourishing, and healing, all belonging to the implicit realm of positive vitality affects and mental models” (p. 398). The individual is then better equipped to face a period of confrontation with painful or traumatic material or the challenges faced within a therapeutic rehabilitation environment. Successful confrontation of difficult realities is then followed by a new phase of resource mobilization and consolidation of healthier behaviors that begin to replace dysfunctional defenses such as avoidance, behavioral extremes, or substance abuse.
Developing limbic network assessment tools (or repurposing existing tools) for their ability to screen or identify the presence of direct or indirect limbic involvement is of critical value. In addition, the ability to discriminate the type of limbic involvement (decreased responsiveness and withdrawal from increased responsiveness or overresponsiveness) is important to treatment planning. Treatment techniques will be discussed later in the chapter. However, the specific techniques appropriate for treating these syndromes are tools all therapists possess. These tools range from simple variations in approach (e.g., lighting, sound, smell) to more formal therapeutic techniques, such as the Feldenkrais approach, or The Bonny Method of Guided Imagery and Music.239 How each clinician uses those tools is a critical link to success or failure in clinical interaction.
Specific limbic influences on motor system output.
Throughout the existence of humankind, emotions have been identified in all cultures. A child knows when a parent is angry without a word being spoken. A stranger can recognize a person who is sad or depressed. People walk to the other side of the road to avoid being close to someone who seems enraged. Emotions are easily recognizable as they are expressed through motor output of the face and body. Emotions similarly have an impact on functional motor control. The effect and intensity of emotions and limbic influence on motor control are an important part of the therapy evaluation. Table 5-1 helps differentiate the level of limbic activity with observed behavioral states cross-referenced with various medical conditions.
TABLE 5-1 
INTERACTIONS AMONG LIMBIC STATE, MEDICAL CONDITIONS, AND BEHAVIORS*
| LIMBIC STATE | OFTEN ASSOCIATED WITH | OBSERVED BEHAVIORS |
| Neutral | Health and wellness | Relaxed state |
| Low | Depression, stroke | Decreased eye contact, crying |
| Lack of motivation | ||
| High | Anxiety and panic disorders Vestibular disorders Mild or traumatic head injury Blast injury, PTSD |
Anxiety, anger, fear, increased respiratory rate, higher blood pressure, high muscle tension or tone, hyperactivity |
| Overload (F2ARV, GAS) | Traumatic head injuryBlast injury, PTSD, frail individual (either young or old), physiologically unstable individual | Violence, extreme withdrawal, loss of inhibition, reversal of expected behavior |
*Many individuals with neurological dysfunction fall into these categories.
Fear.
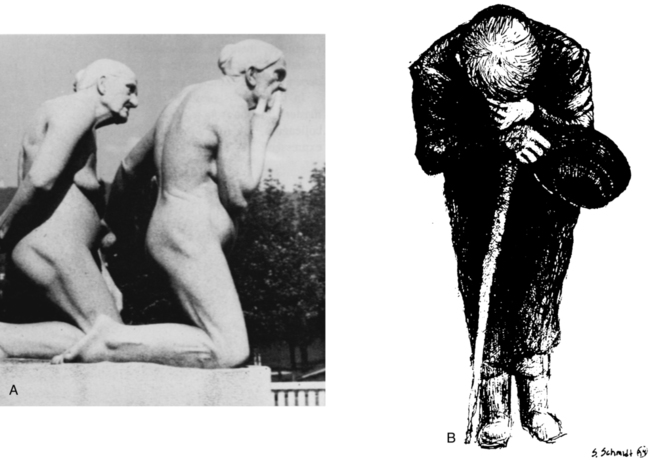
Fear is often associated with pain, be it somatic or emotional. To the individual in pain, pain is just pain. Figure 5-6, A illustrates two people who are on a rollercoaster which could create automatic responses of fear. The boy looks scared and obviously exhibits fear. The woman could be expressing joy or fear given her motor responses. Her eyes seem fixed, which might lead to the assumption that she is truly in fear. She may not have control over her facial responses and could be exhibiting an extreme reaction to fear. If that were the case, this would be a limbic motor reaction, which could be semiautomatic. This extension pattern, if limbic, could trigger hyperextension of the neck, causing opening of the mouth. In Figure 5-6, B, the rollercoaster has stopped, and she still has the same expression. In fact, it took over a minute before she was able to relax her face and regain the feeling that she had some control over her emotional reaction. Her next reaction to occur was crying and observable frustration in her inability to control her initial response. The amygdala nuclei plays a critical role in regulation of facial responses to fear, pain, and other incoming stimuli.243 This is often observed in healthy normal individuals such as seen in Figure 5-6 and similarly can be seen in patients who are extremely fearful, no matter the cause.
Fear of falling is a common problem with the elderly, especially the elderly who have various neurological diagnoses.244,245 Therapists working with individuals who have a fear of falling need to first acknowledge that the fear is normal and then make sure that when the individual moves, he or she does not fall. Trust will be discussed later in the chapter, but fear often precedes the development of trust. Fear is an emotional response and thus is initiated and controlled by the limbic network.
Fear of pain is another emotional response housed within the limbic network that drives many individuals’ motor responses. Whether individuals have fear of movement after a musculoskeletal injury,243 fear of going to the dentist after a dental procedure,246 fear of pain intensity after a chronic pain problem,247 or fear of falling,248 fear will drive motor responses, and that fear will often lead to a lower quality of life.244 For that reason alone, therapists need to differentiate the limbic system’s and the motor system’s summated responses when observing the movement patterns of the individual in therapy.
Anger.
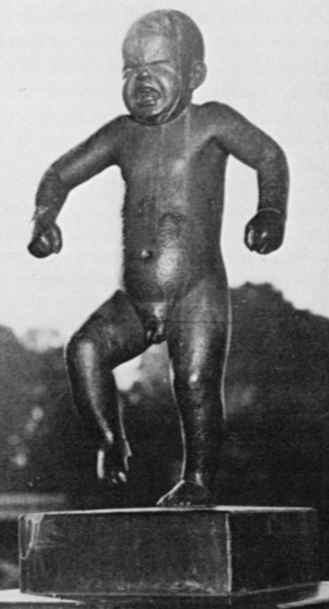
Anger itself creates muscle tone through the amygdala’s influence over the basal ganglia and the sensory and motor cortices and their influence over the motor control system. This is clearly exhibited in a child throwing a temper tantrum (Figure 5-7) or an adult putting his fist through a wall. How far a client or a friend will progress through the F2ARV continuum (discussed in the previous section) depends on a large number of variables. When a client loses control, the therapist must first determine whether the intervention forced the client beyond her or his ability to control. If so, changes within the therapeutic environment need to be made to allow the client opportunities to develop control and modulation over that continuum.
Grief, depression, or pain.
Emotions such as grief or depression can be expressed by the motor system.56,249 The behavioral responses are usually withdrawal, decreased postural extension, and often a feeling of tiredness and exhaustion (Figure 5-8). Sensory overload, especially in the elderly, can create low muscle tone and excessive flexion. Again, because of the strong emotional factor, these motor responses are considered to be the result of the limbic network’s influence over motor control.110 Learned helplessness is another problem that therapists need to avoid.250 When patients are encouraged to become dependent, their chances of benefiting from services and regaining motor function are drastically reduced.251,252
Pain is a complex phenomenon, and the more it is understood, the more complex it becomes253–257 (see Chapter 32). The concept of pain and pain management is discussed in detail in both Chapters 18 and 32. Hippocampal volume has been identified as a variable in pain ratings in the elderly.258 Whether the pain is peripherally induced or centrally induced because of trauma or emotional overload, often the same motor responses will exist. A withdrawn flexor pattern from pain makes postural activities exhausting because of the work it takes to override the existing central pattern generators. Thus, daily living activities, which constantly require postural extension against gravity, may be perceived as overwhelming and just not worth the effort. The therapist needs to learn to differentiate between peripheral physical pain and central or emotional pain and between mixed peripheral and central induced pain. To the patient, “pain is pain!”259–266
Client-therapist bonding.
Bonding projects relaxation, whereas lack of bonding reflects isolation. Because of the potency of the limbic network’s connections into the motor system, a therapist’s sensitivity to the client’s emotional state would obviously be a key factor in understanding the motor responses observed during therapy. This requires that a therapist first understand her or his own feelings, emotional responses, and communication styles that are being used within any given clinical or social environment.267–274
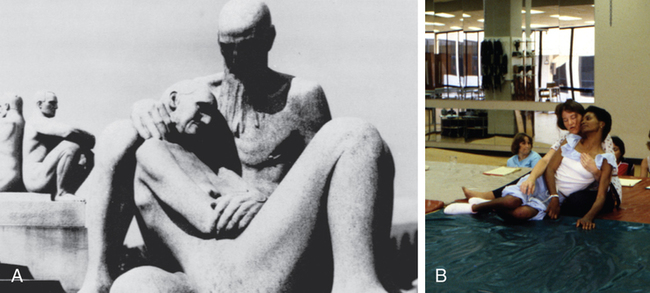
In Figure 5-9 an entire spectrum of motor responses can be observed in four statues. A client who feels safe can relax and participate in learning without strong emotional reactions. The woman being held in Figure 5-9, A is safe and relaxed. The man and woman are interacting through touch with the warmth and compassion that are often observed in the client-therapist interaction of an experienced or master clinician. In Figure 5-9, B, the client and clinician seem to flow together during the treatment as if they shared one motor system. When looking at the therapist and client or looking at the man and woman in the statue, it becomes obvious that the two figures seem to flow together. In the statue, those two figures make one piece of art.
With clinical emphasis on clients generating and self-correcting motor programming, it would perhaps seem reasonable for a therapist to conclude that he or she need not, or should not, touch the patient. This conclusion may be accurate when considering the motor system in isolation and assuming that patients can self-correct errors in motor programs. When correction by the therapist is through words rather than touch, external feedback through the auditory system has replaced internal feedback from the somatosensory system. The voice, as well as touch, can be soothing and instill confidence.275 Yet language in and of itself will not replace the trust and safety felt both physically and emotionally through the deep pressure of touch as illustrated in Figure 5-9. Bonding and trust occur much more often through touch than through conversation.276 Recall, also, that verbal instructions require intact auditory processing and translation from declarative to procedural information, a cognitive ability that the client may not possess.
Referring again to Figure 5-9, A, the two men in the statue on the left demonstrate a lack of bonding. In fact, if the artist could have brought them closer together, they might just have rejected or repelled each other with greater intensity. If one of the men were the therapist and one the patient, little interaction would be occurring, and thus an assumption that learning is occurring is probably false. The therapist could do nothing to the other person (and vice versa) without that person perceiving the act as invasive, negative, or even disrespectful, with little consideration of the person’s individual values. The therapist’s responsibility is to open the patient’s receptiveness to learning, not to close it.277,278
These pictures clearly illustrate two types of therapist-client interactions. If an artist can clearly depict the tonal characteristics of emotion, certainly the therapist should be able to recognize those behaviors in the client.279 If a client is frustrated or angry and simultaneously has rigidity, spasticity, or general high tone, then a therapist might spend the entire session trying to decrease the motor response. If the client could be helped to deal with the anger or frustration during the therapy session and neutralize the emotion and achieve a limbic neutral state, then the specific problems could be treated effectively. Differentiating the limbic network component from the motor control system when establishing treatment protocols has not typically been within the spectrum of a therapist’s skills. It is a skill that must be developed and practiced, as it is clear that the influence of an overactive or overloaded (limbic high) or underactive (limbic low) limbic network state may drastically alter the consistent responses of the motor systems and thus dampen the procedural learning and limit the success of the therapeutic setting. Carryover of procedural learning (Chapter 4) into adaptive motor responses needs to be practiced with consistency.56
Many factors in an interactive setting, such as therapy, cannot be identified, but certain limbic or emotional factors may play a role in that gifted clinician’s skill. Although therapists are trained to be skilled observers of patient behavior, the development of “master clinician” capabilities also requires self-awareness on the part of the helping professional. “Behavioral activity can often tell us about the inner state of another or ourselves” (p. 19).280 The willingness to be aware of one’s own internal state increases the therapist’s ability to perceive subtleties in the patient’s responses.
Trust.
Trust is a critical component of a successful therapy session.281 The therapist gains the client’s trust by his or her actions. The therapist may also build trust through sincere acknowledgment that the patient has life-limiting functional problems and that those problems are limiting normal participation. Trust is further developed when the therapist’s words can be supported by data. When the therapist can illustrate the presence of functional limitations and generate a treatment plan with the patient using objective data, a bond and trust between the patient and the therapist are created.282 In today’s environment the use of reliable, valid, objective tests and measures allows for this form of communication, which has not existed to the same extent in the past. Honesty and truth lead to trust.119,283–287
Because these symptoms can be overt or covert, the therapist needs to be aware of both the physical and emotional responses of the patient. The use of analog or perceived exertion scales can be a valuable way to make the covert more overt to the therapist. Symptoms are valuable to the therapist as well as the patient to create environments for change, but the intensity of those stimuli need close monitoring because they can dramatically affect motor responses and ultimately overwhelm the CNS and prevent learning. Compliance to participate is limbic, and the limbic system has tremendous control over intentional movement, no matter the context of the environment.119
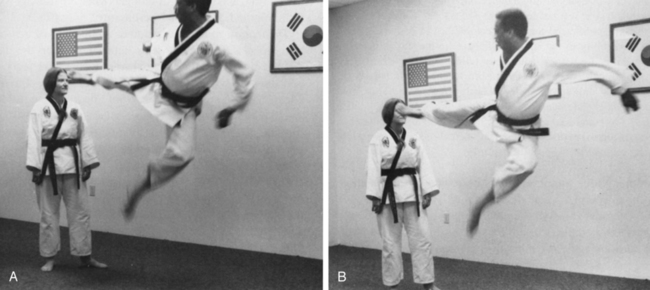
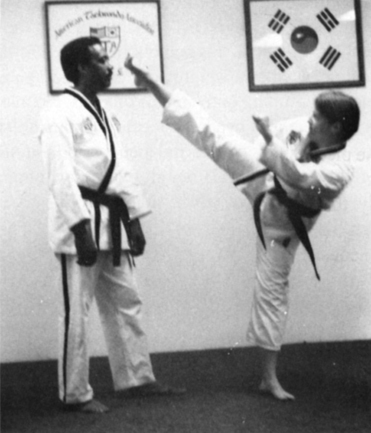
Once a client gives his or her trust, a clinician can freely move with the client and little resistance caused by fear, reservations, or need to protect the self will be felt or observed. When the patient is limbic neutral (the limbic network is emotionally neutralized), the tightness or limitations in movement that are present on examination can be considered true impairments within those systems or subsystems. Examination and interventions at this time will more consistently reflect true motor performance. Once limbic neutral has been achieved and examination is complete, it is recommended, for example, that if the pain is a result of peripheral tightness or joint immobility, the therapist does not elicit pain during that session. Deal with those issues in the next session after gaining the trust of the client. Trust by the therapist or the client does not mean lack of awareness of potential danger. Trust means acceptance that although the danger is present, the potential for harm, pain, or disaster is very slight and the expected gain is worth the risk (in this case, delay in intervention). In Figure 5-10, the student’s trust that the instructor will not hurt her can be seen by her lack of protective responses and by her calm, relaxed body posture. The student is aware of the potential of the kick but trusts her life to the skills, control, and personal integrity of the teacher. Those same qualities are easily observed in patient-therapist interactions when watching a gifted clinician treat clients. The motor activities in a therapeutic setting may be less complex than in Figure 5-10, but in no way are they less stressful, less potentially harmful, or less frightening from the client’s point of view.
In addition, therapists must first trust themselves enough to know that they can effect changes in their clients.7,288 Understanding one’s own motor system, how it responds, and how to use one’s hands, arms, or entire body to move someone else is based partly on procedural skills, partly on declarative learning, and partly on self-confidence or self-trust. Trusting that one, as a therapist, has the skill to influence the motor response within the patient has a limbic component. If a therapist has self-doubts about therapeutic skills, that doubt will change performance, which will alter input to the client. This altered input can potentially alter the client’s output and vary the desired responses if the client’s motor system cannot run independently.
Responsibility.
Very close to the concept of trust is the idea of responsibility. Accepting responsibility for our own behavior seems obvious and is accepted as part of a professional role.289 Accepting and allowing the client the right to accept responsibility for her or his own motor environment are also key elements in creating a successful clinical environment and an independent person.*
Figure 5-11 illustrates the concept through the following example: The instructor asked the student to perform a motor act, in this case, to perform a kick to the teacher’s head. The kick was to be very strong or forceful and completed. The student was instructed not to hold back or stop the kick in any way, even though the kick was to come within a few inches of the teacher’s head. This placed tremendous responsibility on the student. One inch too far might dangerously hurt the instructor, yet one inch too short was not acceptable. The teacher knew the student had the skill, power, and control to perform the task and then passed the responsibility to the student. The student was hesitant to assume the responsibility, for the consequence of failure could have been very traumatic. However, the student trusted that the teacher would not ask for the behavior unless success was fairly guaranteed. That trust reduced anxiety and thus neutralized the neurochemical limbic effect on the motor system of the student, giving her optimal motor control over the act.292 Once the task was completed successfully, the student gained confidence and could repeat the task with less fear or emotional influence while gaining refinement over the motor skill.
Current literature has shown that people are more motivated by novelty and change than by success at mastery or accomplishment of a goal.90,292,293 The limbic complex and its interwoven network throughout the nervous system play a key role in this behavioral drive.294 The task itself can be simple, such as a weight shift, or as complex as getting dressed or climbing onto and off of a bus. No matter what the activity, the client needs to accept responsibility for her or his own behavior before independence in motor functioning can be achieved. Although the motor function itself is not limbic, many variables that lead to success, self-motivation, and feelings of independence are directly related to limbic and prefrontal lobe circuitry. The variance and self-correction within the movement expression also create novelty and motivation to continue to practice.90,292–295
Flexibility and openness.
Another component of a successful clinical environment deals with learning and flexibility on the part of the therapist. A master clinician sees and feels what is happening within the motor control output system of the client. Letting go of preestablished belief of what will happen is difficult.296,297 It is important for a clinician to be open to what is present as the motor expression. This openness is critical to actually identifying what is being expressed by the nervous system of the patient. Master clinicians do not get stuck on what they have been taught but use that as a foundation or springboard for additional learning. Learning is constantly correlated to memories and new experiences.
To the therapist, each client is like a new map, sparsely drawn or sketchy at the beginning, but one that is constantly revised as the terrain (client) changes. The initial medical diagnosis may link to many paths provided within the map, but the comorbidities can result in great variance among patients.298 That initial map might be a critical care pathway for the client, given her or his neurological insult. That pathway is a map, but only a sketchy one, and may not even be a map that a particular patient falls within in spite of his or her medical diagnosis. It is the therapist’s responsibility to evaluate the patient and determine whether that pathway or map will work or is working and when changes in that map need to be altered. That is, the therapist must let go of an outdated map or treatment technique and create a new one as the environment and motor control system of the client change. This transference or letting go of old maps or ideas is true for both the client and therapist. If a position, pattern, or technique is not working, then the clinician needs to change the map or directions of treatment and let the client teach the therapist what will work. The ability to change and select new or alternative treatment techniques is based on the attitude of the therapist toward selecting alternative approaches. Willingness to be flexible and open to learning is based on confidence in oneself, a truly emotional strategy or limbic behavior. Master clinicians have learned that the answers to the patient’s puzzle are within the patient, not the textbooks.
Figure 5-12 depicts two maps with a beginning point and a terminal outcome or goal in each. The parameters of the first map illustrate the boundaries of that therapist’s experience and education. The clinician, through training, can identify what would seem to be the most direct and efficient way or path toward the mutually identified goal of the therapist and client. When the client becomes a participant within the environment or map, what would seem like a direct path toward a goal might not be the easiest or most direct path for the client. If empowerment of the client leads to independence, then allowing and encouraging the client to direct therapy may provide greater variability, force the client to problem solve, and lead to greater learning. The therapist needs to recognize when the client is not going in the direction of the goal. For example, the client is trying to perform a stand-pivot transfer and instead is falling. If it is important to practice transfers, then practicing falling is inappropriate and the environment (either internal or external) needs modification. Falling can be learned and practiced at another time. Once both strategies are learned, the therapist must empower the patient to take ownership of the map. In the examples of transferring, if the therapist asks the client to practice transfers and if the client starts to fall, a change in required motor behavior must be made and the opportunity given to the client to self-correct. In that way the client is gaining independent control over a variety of environmental contexts and outcomes. Within the same figure (Figure 5-12) is a second map. That second map might represent another professional’s interaction and goal with the same client. It is during these overlapping interactions that both professionals can empower the patient to practice, and that practice will help lead to those functional goals established by both practitioners. In some situations a clinician from one profession may guide a client toward obtaining the functional skill necessary for a member of the second profession to begin guiding the client toward the expected outcomes of the second profession. These interlocking dependencies of the client and the professions are illustrated in Figure 5-12. If the client begins therapy striving for the first goal and ends at the functional outcome of the second goal, then additional functional outcomes have been achieved and both professions interacted for the ultimate prognosis for the patient. That interaction requires respect and openness of both professionals toward each other as well as toward the client. Those attitudes and ultimate behaviors are limbic driven.
Matching maps should be a collaborative effort instead of coincidence. These collaborative efforts include interactions with all professions within the rehabilitation setting. Occupational and physical therapists are very familiar with collaboration, and both often approach interventions as a team effort. There are many additional therapists and individuals within that same setting who could also collaborate. Recreational therapists, psychologists, nurses, family members, and music therapists are but a few. Within a profession such as music therapy, the existence of two maps may overlap within a multidimensional environment. When a physical or occupational therapist needs to challenge a patient, the music therapist may be able to calm the system at the same time (overlapping maps). Research on affective responses to consonance and dissonance in music supports the creation of a map within a rehabilitation environment that could overlap with either physical, occupational, or speech therapy. Words such as relaxed or calm correlated positively with higher levels of consonance in the music, whereas adjectives associated with negative emotions (unpleasant, tense, irritable, annoying, dissonant, angry) were found to correlate positively with higher levels of dissonance.133 Creating a whole environment where potential frustrations within motor learning could be balanced with higher levels of consonance in the music would potentially balance the limbic network emotional response within the overlapping maps and bring balance or stability to the limbic network’s influence on motor learning and control. A later study by Peretz and colleagues148 related the same variables to a happy-sad rating task. Given the research evidence for activity within the limbic network as it relates to music,144,299 motor learning,300 and cognitive enhancement,301 a natural multiple map system would be easy to incorporate within a therapeutic setting. The clinician needs to appreciate the uniqueness of each map while holding onto the concept of the interaction of the two maps.
Vulnerability.
To be open totally to processing the individual differences of the client, the clinician must be relaxed and nonthreatened, and feel no need to protect himself or herself from the external environment. This environment needs to project beyond the therapist-client relations and envelope all disciplines interacting with the client.302 In order for these interactions to occur, the clinician’s emotional state requires some vulnerability, allowing him or her to be open to new and as-yet-unanalyzed or unprocessed input. This vulnerability implies the role not of an expert who knows the answers beforehand but of an expert investigator. Being open must incorporate being sensitive not only to the variability of motor responses but also to the variability of emotional responses on the part of the client.303,304 This vulnerability leads to compassion, understanding, and acceptance of the client as a unique human being. It can also be exhausting. Therapists need to learn ways to allow openness without taking on the emotional responsibility of each patient.
Limbic lesions and their influence on the therapeutic environment
Many lesions or neurochemical imbalances within the limbic network drastically affect the success or failure of physical, occupational, and other therapy programs. This chapter does not discuss in detail specific problems and their treatment, but instead it is hoped that identification of limbic involvement may help the reader develop a better understanding of specific neurological conditions and carry that knowledge into Section II, where the specific clinical problems are discussed.
Substance abuse (see chapter 24).
The anterior temporal lobe (especially the hippocampus and amygdala) has a lower threshold for epileptic seizures than do other cortical structures.56 This type of epilepsy is produced by use of systemic drugs such as cocaine and alcohol. The seizure is often accompanied by sensory auras and alterations in behavior, with specific focus on mood shifts and cognitive dysfunction.305 Obviously, the precise association between behavior and emotions or temporolimbic and frontolimbic activity is not understood, yet the associations and thus their impact on a therapeutic setting cannot be ignored.217,306
Whether street bought, medically administered, or ingested for private or social reasons (such as in alcohol consumption), drugs and alcohol can have dramatic effects on the CNS and often are associated with limbic behavior.307 Korsakoff syndrome, caused by chronic alcoholism and its related nutritional deficiency, is identified by the structural involvement of the diencephalon with specific focus on the mammillary bodies, and the dorsal medial and anterior nucleus of the thalamus56 usually shows involvement (see the anatomy section and Figure 5-13). This syndrome is not a dementia but rather a discrete, localized pathological state with specific clinical signs. The most dramatic sign observed in a client with Korsakoff syndrome is severe memory deficits.252,308–310 These deficits involve declarative memory and learning losses, but the most predominant problem is short-term memory loss.311 As the disease progresses, clients generally become totally unaware of their memory loss and are unconcerned. Initially, confabulation may be observed,312 but in time most clients with a chronic condition become apathetic and somewhat withdrawn and are in a profound amnesic state. They are trapped in time, unable to learn from new experiences because they cannot retain memories for more than a few minutes and are unable to maintain their independence252,308–310,313; many may become social isolates and homeless.
The use of alcohol affects not only adults but also children and adolescents. Still another population of children affected by alcohol abuse has surfaced as a specific clinical problem. These children are infants who have the effects of fetal alcohol syndrome. A variety of researchers have investigated the effects of alcohol and other toxic drugs on neuromotor and cognitive development.314–319
Alzheimer disease (see chapter 27).
In Alzheimer disease, the hippocampus and nucleus basalis are the most severely involved structures, followed by neurofibrillar degeneration of the anterotemporal, parietal, and frontal lobes.252,320–323
Initially the symptoms fall into several categories: emotional, social, and cognitive. Usually the symptoms have a gradual onset. Depression and anxiety often are seen during the early phases because of the neuronal degeneration within the prefrontal lobes and limbic network.322,324–326 During the second stage, the emotional, social, and intellectual changes become more marked. Clients have difficulty with demands, business affairs, and personal management. Their memory and cognitive processing continue to deteriorate, whereas their awareness of the problem is often still insightful, causing additional anxiety and depression. During this phase clients may be unable to recognize familiar objects and become scared because they are losing control of the environment both internally and externally. Thus the client may become combative out of a defensive (fight-or-flight) autonomic response. For that reason, therapists need to make sure the client feels safe during therapy to optimize the learning and compliance. The third phase manifests itself with moderate to severe aphasic, apraxic, and agnosic problems. Object agnosia, the failure to recognize objects, is a typical sign of advancing Alzheimer disease. Distractibility and inattentiveness are also common signs of this third stage. The final stage of Alzheimer disease is marked by an individual who is uncommunicative, with little meaningful social interaction, who often takes on the features of the Klüver-Bucy syndrome (see Chapter 13). Thus they exhibit emotional outbursts, inappropriate sexual behaviors, severe memory loss, constant mouth movements, and often a flexor-type postural pattern. In this latter phase, the client is virtually decorticate and clinically indistinguishable from persons with other dementias. The prognosis of Alzheimer disease was only a few years ago totally bleak, but today there are hopes that in the future, pharmacological interventions may slow and even reverse the damage inflicted by this disease.327–330
In spite of future treatments, the continual degeneration of the limbic network is a key distinguishing factor in Alzheimer disease.109,331–333 Many clients in the past have been misdiagnosed as having other problems such as intracranial tumors, normal pressure hydrocephalus, multiinfarct dementia, or alcoholic or chronic drug intoxication.334–337 Similarly, many clients with tumors, multifaceted dementias, alcoholism, or heart attacks resulting in hippocampal damage may be diagnosed with Alzheimer disease. When the disease is correctly evaluated and diagnosed, however, it becomes obvious that the limbic-cortical area involved from phase 1 through the last phase is interacting with other areas of the brain and constantly affecting the behavioral patterns of the patient.338–341 Owing to the neurochemical sensitivity and production within the limbic network, drugs are often used to prevent or slow the progression of Alzheimer disease (see Chapter 36).342–346 Similarly, a genetic predisposition has been found in some patients with Alzheimer disease56,347–349; thus, gene therapy may prove to have great therapeutic value.350 Because music is able to activate many different brain areas, it is particularly valuable in the treatment of persons at all stages of Alzheimer disease351 and can effectively be used during physical or occupational therapy. Long after declarative memory is lost, individuals can sing entire songs (procedural memory), dance with a loved one they no longer recognize (procedural memory), or be soothed and calmed by hearing someone who cares about them singing familiar favorite songs or lullabies (limbic response). This is why the power of music is so great, especially as observed in individuals with Alzheimer disease who have lost declarative memory. In earlier phases of the disease, individuals who have lost words can recall words such as song lyrics through the linking with melody. When melody is lost, individuals still retain rhythmic responses. At the palliative stage of Alzheimer disease care, agitated patients are observed to calm to simple music such as familiar lullabies. Thus Alzheimer disease patients are able to continue to respond to music through the progression of the disease, and the response to rhythm may represent overlearned motor responses that are tied to positive limbic states. For example, nonambulatory individuals, when presented with familiar and preferred music, may stand and move with the rhythm of the sound. Their bodies may remember how to dance with the spouse whose name they no longer know.352 A physical or occupational therapist can instruct a caregiver to use music as part of everyday activities. The therapeutic effects of music to engage and maintain attention, activate long-term memory, and modulate emotion states are well suited to the needs of both the person with Alzheimer disease and his or her caregivers.352
Head injury (see chapter 24).
Traumatic injury.
One potentially severe limbic problem that can be present after traumatic closed head injury is diffuse axonal injury.215,216,353–356 The long associative bundles or fibers that transverse the cortex on a curved route can be sheared by an impact or a blow to the head. One of these long associative bundles is the cingulate fasciculus, which coordinates the amygdala and hippocampal projections to and from the prefrontal cortex. Many basic perceptual strategies, such as body schema, hearing, vision, and smell, are linked into the emotional and learning centers of the limbic network through the cingulate fasciculus.357 Thus, declarative learning through sensory and cognitive processing can become impossible. If the pathways to and from the hippocampus and amygdala are sheared bilaterally, total and permanent global anterograde amnesia will be present.109,358,359 If destruction of both tracts on one side occurs, but the contralateral side is left intact, the individual can compensate, but learning will be slower or the rate of processing delayed.157 If only one tract on one side is damaged, such as the tract to and from the hippocampus, the amygdaloid system on the same side will compensate but be slower than without the lesion.157 Thus the specific degree of involvement will vary and depend on the extent of shearing. Those with total shearing on both sides will usually be in a deep coma and will not survive the injury.360 Those with less severe insult will show signs ranging from total amnesia to minor delays in declarative learning.361 The emotional problems of traumatic head injury can often be associated with other limbic problems such as posttraumatic stress syndrome. This problem is especially apparent when treating soldiers injured on the battlefield who have returned home.362
Integrating various professions becomes a critical aspect of an injured soldier’s rehabilitation. When the interaction of the limbic network and higher control is considered, additional variables can be taken into consideration within the therapeutic environment. In treating more than 200 patients who had trauma, Körlin242 found that certain kinds of musical elements often triggered intrusive and traumatic reexperiences of the event. (For a theoretical discussion of this phenomenon, see Goldberg.363) The phenomenon of auditory triggering has implications for the rehabilitation setting, where patients may be recovering from traumas related to accident, injury, or difficult medical procedures. Both environmental noise and “background” music may present auditory triggers that elicit limbic network and ANS activity. Thus the potential for eliciting the F2ARV continuum during a physical or occupational therapy treatment session is always present, and the therapists need to be acutely aware of background noise.
Cerebral contusions (bruises) have long been a primary sign of traumatic head injury.364 Regardless of area of impact, the contusions are generally found in the frontal and temporal regions. There are long-term neuropsychological ramifications after mild traumatic brain injury even when there is no loss of consciousness.365 The regions most frequently involved are orbitofrontal, frontopolar, anterotemporal, and lateral temporal surfaces.
The limbic network’s connection to these areas would suggest the potential for direct and indirect limbic involvement. The greater the contusion, the greater the likelihood that the limbic structures might simultaneously be involved. Impulsiveness, lack of inhibition, and hyperactivity are a few of the clinical signs associated with orbitofrontal or limbic involvement.366 The dorsomedial frontal region, involved in the hippocampal-fornix circuit (once referred to as the Papez circuit),367 when damaged seems to induce a pseudodepressed state, including slowness, lack of initiation, and perseveration.
Nontraumatic head injuries: anoxic or hypoxic brain injury.
Lack of oxygen to the brain, regardless of the cause, seems not only to have a dramatic effect throughout the cortex but also selectively damages the hippocampal regions.368 The loss of hippocampal declarative memory systems bilaterally would certainly provide one reason for the slowness in processing so commonly observed in head injury.369 A hypothesis could also be made regarding the limbic network’s interrelation with other cortical and brain stem structures. In cases of hypoxia, many structures interconnecting in the limbic network are potentially affected, so information sent to the limbic network may be distorted. These distortions could cause tremendous imbalances within the limbic processing system, with not only attention and learning problems but also the hypothalamic irregularity often seen in head trauma. Individuals who demonstrate obstructive sleep apnea, another cause of hypoxia, have been shown to have an imbalance in the hippocampal area.370 This imbalance may lead to severe cognitive dysfunction.371 This preexisting hypoxic environment certainly can have a long-term effect on any patient who has CNS damage at any age.
Summary of limbic problems with head-injured clients.
The behavioral sequelae after any head injury reflect many signs of limbic involvement. In studies of both the pediatric and adult populations,353–355,357,365,372,373 behaviors of impulsiveness, restlessness, overactivity, destructiveness, aggression, increased tantrums, and socially uninhibited behaviors (lack of social skills) are frequently reported. These behaviors all reflect a strong emotional or limbic component. Given Moore’s concept of a limbic network that MOVEs us and the F2ARV continuum regarding emotional control over noxious or negative input, it is no wonder so many clients have difficulty with personal and emotional control over their reactions to the therapeutic world. If the imbalance were within the client, then the external environment would be one possible way to help center the client emotionally.374,375 This centering requires that the therapist be sensitive to the emotional level of the client. As the client begins to regain control, an increase in external environmental demands would challenge the limbic network. If the demand is excessive, the client’s emotional reaction as expressed by motor behavior should alert the therapist to downgrade the activity level.
Head injuries affect many areas of the CNS. A client with spasticity, rigidity, or ataxia may exhibit an increase in those motor responses when the limbic network becomes stressed. Learning to differentiate a motor control problem from a limbic problem that influences the motor control systems requires that the therapist be willing to address the cause of the problems and their respective treatments.376 Each client is different, no matter the commonalities of the site or extent of the lesions, because of prior learning, conditioning of the limbic network, and their respective perception of quality of life.377 The response of two clients to the same clinical learning environment may have great variance and should not surprise the clinician. Thus the therapist needs to give undivided attention to the client at all times and be willing to make moment-to-moment adjustments within the external environment to help the client maintain focus on the desired learning.
Vestibular disorders.
It is generally accepted that vestibular dysfunction results in erroneous input to the CNS. This erroneous sensory information creates a mismatch between the external (afferent) cues and the internal conceptual model for movement contained by the cerebellum. This mismatch creates an imbalance in vestibular and cerebellar signals to the CNS, flooding the central limbic structures and resulting in symptoms such as vertigo, motion sickness, nausea, or decreased postural control. Detection of this mismatch results in an attempt by the cerebellum to compensate for the imbalance, which becomes a core tenet of recovery.378 Alternately, this neural stimulation may create an internal stressor, and trigger an adverse limbic response, such as a GAS response.
Newer evidence from animal research has demonstrated that vestibular lesions result in dramatic changes in the morphology and function of the hippocampus. Of note is that bilateral vestibular lesions have been associated with hippocampal atrophy. The hippocampus makes unique contributions to memory, both spatial and nonspatial. Thus vestibular lesions impair learning and memory, particularly those tasks that require spatial processing. In addition to the more well known deficits in spatial and gravitational orientation for balance control, vestibular lesions can also result in impaired cognition, learning, and memory through damage to this connection. Decreased concentration, thought processes, and memory are among the most common complaints in patients with vestibular disorders. In the past these complaints were often attributed to competitive resources, suggesting that cognitive resources were being devoted to the basic tasks of staying balanced during function. It is now clear that there is a true physiologic explanation for these secondary symptoms, which are quite limiting to activity and participation in normal daily activities, particularly working. It has also been suggested that treatment activities that stimulate the function of the vestibular system also stimulate activity within the hippocampus and can improve memory, which has important implications for treatment.379–387
Thus vestibular dysfunction can influence the therapeutic environment both in the assessment and the treatment of this system. However, the vestibular system is not a primary consideration of most physicians and therapists during evaluation. On the basis of benchmarking data from within specialized balance centers, the average patient with a vestibular disorder (dizziness or imbalance) travels within the medical system an average of 52 months before finding a solution. During this time, he or she has seen on average four physicians. There is also at least one visit to the emergency department in crisis and one visit to a psychiatrist. Typically there has been no rehabilitation referral or intervention during this time.388
The patient with a chronic vestibular disorder can have myriad symptoms, including vegetative, autonomic, motoric, cognitive, psychological, and behavioral symptoms that are often misdiagnosed during this search for an outcome as other, more serious medical diagnoses. As an example, of those patients diagnosed with dizziness or imbalance of a psychologic origin, evidence has determined that more than 70% of these patients have underlying vestibular dysfunction on key vestibular function tests (electronystagmography and calorics, rotary chair, computerized dynamic posturography, auditory brain stem response, and acoustic reflexes).233,235,389–391 Conversely, of those patients with chronic dizziness and imbalance, only 16% were found to have dizziness of a true psychogenic origin.392 Acknowledgment of a patient’s symptoms, use of data, and explanation (in understandable detail) that there is a physiologic explanation for his or her complaints builds the client-therapist relationship and begins to neutralize the client’s abnormal limbic state (anxiety versus depression). It can lower the GAS or autonomic cascade, maximizing the treatment time before the onset of limiting symptoms (i.e., raise the symptom threshold).
Even patients with motion sickness have documentable physiologic and functional changes. Some of the best current evidence is in our military personnel with symptoms of motion sickness. On examination, these soldiers have physiological changes identifiable by results of rotary chair (60% with abnormally long time constants) and computerized dynamic posturography (70% with abnormal sensory organization test [SOT] condition 5 and 6).393
Patients who have sustained a mild head injury, postconcussive syndrome, blast exposure or injury (positive or negative pressure event), or whiplash often have concomitant involvement of the vestibular apparatus or nuclei. This often goes undetected within the initial medical workup and management plan excepting in specialty vestibular practices.393–397 When the disorder is undetected and left unchecked, the patients do not respond to standard treatment interventions. They also complain of atypical symptoms or responses to these typical treatments. When the patient does not respond in predictable ways to standard treatment, the label “aphysiological” is applied, particularly in situations where disability or secondary gain is a factor. Fortunately there are well established performance criteria that can effectively differentiate true balance or vestibular impairment from embellishment for secondary gain.398 (Refer to Chapters 22A and 22B.)
In treatment, recovery is based on long-term compensation mediated by the cerebellum, and symptoms must be reproduced for recovery to occur. However, stimulation of the vestibular system must be controlled, with every effort made to maintain a limbic (emotional) neutral state. Some patients have true vestibular dysfunction that affects only motor responses, whereas other patients have true limbic psychiatric problems that do not manifest themselves with vestibular symptoms. These two behaviors are located at the polar ends of the curve between limbic motor and vestibular motor dysfunction. Before prescribing appropriate intervention strategies, the clinician must be clear regarding the degree of limbic overlay on the vestibular dysfunction, and the question “What are the best vestibular and limbic interactive environments that will challenge and drive neuroplastic change?” must be answered. Although researchers233,390 have identified tools that differentiate the two extremes, today researchers are trying to clarify the midrange of patients who clearly have symptoms on the basis of the interaction of both systems.398,399 Development of tools that can further discriminate whether the behaviors are first driven by vestibular and followed by limbic responses, or vice versa, is a key to treatment planning.
Parkinson disease.
The motor impairments seen in individuals with Parkinson disease are widely accepted, understood, and treated by physical and occupational therapists (see Chapter 20). What is not commonly synthesized by physical and occupational therapists, no matter the working environment (hospital, outpatient, rehabilitation, home health), is that individuals diagnosed with Parkinson disease often have limbic involvement.
Masked expression is accepted as a motor sign of this disease and is linked directly to the rigidity expressed within the motor system. Yet, a masked expression is also associated with fear as an emotion (see Figure 5-6). Similarly, the ability to extinguish this fear response or masked expression is also based on the infralimbic prefrontal lobe and the number of dopamine receptors.400 These areas may not be directly damaged by Parkinson disease, but the amount of available dopamine is dramatically reduced. Given this interaction, patients with Parkinson disease may have difficulty facially expressing what they are feeling. Thus, when a therapist sees a patient with a fixed facial expression, that therapist cannot draw a conclusion from that facial expression.
Similarly, depression is commonly associated with any individual with a degenerative disease.401,402 Obviously, depression from a neuroanatomical perspective is housed with the limbic system. Depression from a motor response perspective causes lower postural tone with increased flexion in the neck (see Figure 5-8, B). This pattern within the trunk is also often described as the postural patterns of an individual with Parkinson disease. The question arises, “Is the tone generated from the motor system alone, from the limbic influence on the motor system alone, or from a combination of the two?”
Individuals working in a psychological setting (inpatient and outpatient) may focus on the psychoemotional problems without addressing the functional motor involvement. It is not infrequent that an individual with this disease may simultaneously exhibit signs of psychosis and other potential psychiatric problems.403–407 It is critical for therapists, despite the physical setting, to develop and understand the entire spectrum of the problems associated with this disease.
Cerebrovascular accidents (see chapter 23).
The most common insult in CVA results in occlusions within tributaries of the middle cerebral artery.56 When this occlusion is in the right hemisphere, studies have shown that clients are often confused and exhibit metabolic imbalance.408 The primary problem of this confused state is inattention. After brain scans, it has been shown that focal lesions existed within both the reticulocortical and limbic cortical tracts, suggesting direct limbic involvement in many middle cerebral artery problems.66
With the use of magnetic resonance imaging (MRI), specific lesion deficits after CVA can help physicians and therapists identify specific motor and limbic behavioral problems that would limit quality of life of the patients.409–411 Many clients who have had a CVA do not have direct limbic involvement, yet the stresses placed on the client,412,413 whether external or internal, are often reflected in the limbic network’s influence over cognition and the motor control systems.414 Everyday existence as well as performance of motor tasks required during therapy are usually valued highly in the client’s life. This value or stress placed on the limbic network overflows into the motor system and never allows it to relax, as observed by noting the increase of tonus in the unaffected leg. The client is usually unaware of this buildup of tonus but can release it once attention is drawn to it. If attention is never directed toward these tension buildups, a therapist trying to decrease tonus in the affected arm or leg will always be interacting with the associated patterns from the less-involved extremities.
Tumor (see chapter 25).
Tumors specifically arising within limbic structures415,416 can cause dramatic changes in the client’s emotional behavior and level of alertness, especially with hypothalamic tumors.417 The behaviors reported include aggressiveness, hyperphagia, paranoia, sloppiness, manic symptoms, and eventual confusion.56 Tumors within the hypothalamus cause not only behavioral abnormalities but also autonomic endocrine imbalances, including body temperature changes, menstrual abnormalities, and diabetes insipidus.109
When the tumor is located within the frontal and temporal lobes, associated with limbic structures, psychiatric problems may manifest, ranging from depression to anorexia to psychosis.109,418 Obsessive-compulsive disorder resulting from limbic tumor has been used as a tumor marker for relapse.419 Amnesia has been reported in patients with dorsomedial thalamus, fornix, midbrain, and reticulolimbic pathway lesions. This again reinforces the importance of the limbic network’s role in storage.109,420,421
The neurochemistry within the limbic network is very complex and will be discussed within the next large section, but even without a keen understanding of the specific chemistry, therapists need to recognize behavior and mood changes within the client. These changes often signal neurochemical problems affecting the individual’s motor system. If medical intervention includes medicine, pharmacists should be able to explain how those behaviors are being regulated by pharmacological intervention. Literature is now reporting that what were once thought idiopathic seizures are now believed to be neurochemical imbalances with the limbic structure and may someday be controlled with medications that directly affect the immune system.422
Ventricular swelling after spinal defects in utero, central nervous system trauma, and inflammation (see chapters 15, 24, and 26).
Although the effects of ventricular swelling after trauma, inflammation, and in utero cerebrospinal malformations are not discussed in great detail in the literature with respect to limbic involvement, the proximity of the lateral and third ventricle to limbic structures cannot be ignored. It is common knowledge that most people exposed to hot, humid weather begin to swell; become more irritable, less tolerant, and moody; and may complain of headaches. Some people become aggressive, others lethargic. All these behaviors are linked to some extent with limbic function. Thus, ventricular swelling causing hydrocephalus, whether caused by trauma, inflammation, or obstruction, would potentially affect the limbic structures. Reported behavioral changes such as seizures, memory and learning problems, personality alterations, alertness, dementia, and amnesia can be tied to direct or indirect limbic activity.56
Summary of clinical problems affected by limbic involvement.
It is easy to identify limbic problems when the behaviors deviate drastically from normal responses. It is much more difficult to determine subtle behavior shifts in clients. The therapist should be sensitive to these minor mood shifts because they may represent early signs of future problems. Similarly, noting that a particular client is always irritable and has difficulty learning on hot days should help direct the therapist toward establishing a treatment session that regulates humidity and temperature to optimize the learning environment. The limbic network is not just a neurochemical bundle of nuclei and axons found within the brain. It is a pulsating center that links perception of the world and the way an individual responds to that perception. Quality of life is a value, and that value has a strong limbic component. If functional outcomes leading to maintaining or improving the quality of life of our clients is the goal of both physical and occupational therapy,291,423,424 then the limbic network is no less important during examination, evaluation, prognosis, and intervention than the motor system itself.
The neuroscience of the limbic network
Basic anatomy and physiology
A brief overview of the anatomy and physiology of the limbic network is presented in the following sections. The reader is referred to a variety of textbooks and websites for a more in-depth understanding of this system56,119 and how higher thought might be much more complex than previously identified.44,68,425–427
Basic structure and function
The limbic network can best be visualized as consisting of cortical and subcortical structures with the hypothalamus located at the central position (Figures 5-13 and 5-14). The hypothalamus is surrounded by the circular alignment of the subcortical limbic structures vitally linked with one another and the hypothalamus. These structures are the amygdaloid complex, the hippocampal formation, the nucleus accumbens, the anterior nuclei of the thalamus, and the septal nuclei (see Figure 5-13). These structures are again surrounded by a ring of cortical structures collectively called the “limbic lobe,” which includes the orbitofrontal cortex, the cingulate gyrus, the parahippocampal gyrus, and the uncus. Other neuroanatomists also include the olfactory system and the basal forebrain area (see Figure 5-14). Vitally linked and often included in the limbic network as the “mesolimbic” part is the excitatory component of the reticular activating system and other brain stem nuclei of the midbrain. Some consider components of the midbrain a very important region for emotional expression.86 Derryberry and Tucker86 found that attack behavior aroused by hypothalamic stimulation is blocked when the midbrain is damaged and that midbrain stimulation can be made to elicit “attack behavior” even when the hypothalamus has been surgically disconnected from other brain regions. Recent research has clearly identified the neurochemical precursors to this aggressive behavior.53,56,428–430 This “septo-hypothalamic-mesencephalic” continuum, connected by the medial forebrain bundle, seems to be vital to the integration and expression of emotional behavior.431 The linking of other brain structures to emotions came initially from the work of Papez,367 who first identified the hippocampal-fornix circuit. He saw this as a way of combining the “subjective” cortical experiences with the emotional hypothalamic contribution. Earlier, Broca71 labeled the cingulate gyrus and hippocampus “circle” as “the great limbic lobe.” Today, the concept of the limbic network and its interaction with sensory inputs and motor expression has become extremely complex.432 Mood can change motor output, and motor activity can change mood.421,433
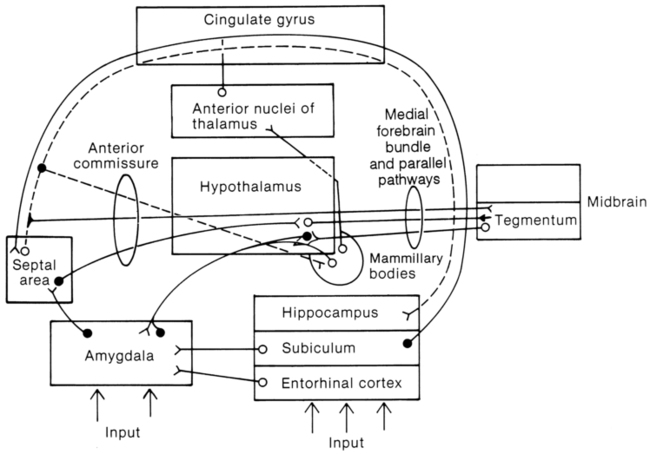
 Limbic network circuitry with parallel and reverberating connections and with medial forebrain bundle.
Limbic network circuitry with parallel and reverberating connections and with medial forebrain bundle.Klüver and Bucy434 linked the anterior half of the temporal lobes and the amygdaloid complex to the limbic network. They showed changes in behavior, with specific loss of the amygdaloid complex and anterior hippocampus input, resulting in (1) restless overresponsiveness, (2) hyperorality of examining objects by placing them in the mouth, (3) psychic blindness of seeing and not recognizing objects and the possible harm they may entail, (4) sexual hyperactivity, and (5) emotional changes characterized by loss of aggressiveness. These changes have been named the Klüver-Bucy syndrome (see Chapter 13).435 Myriad connections link the amygdala to the olfactory pathways, the frontal lobe and cingulate gyrus, the thalamus, the hypothalamus, the septum, and the midbrain structures of the substantia nigra, locus coeruleus, periaqueductal gray matter and the reticular formation. The amygdala receives feedback from many of these structures it projects to by reciprocal pathways.
At the heart of the limbic network is the hypothalamus. The hypothalamus, in close reciprocal interaction with most centers of the cerebral cortex and the amygdala, hippocampus, pituitary gland, brain stem, and spinal cord, is a primary regulator of autonomic and endocrine functions and controls and balances homeostatic mechanisms. Autonomic and somatomotor responses controlled by the hypothalamus are closely aligned with the expression of emotions.429,436–438
In the temporal lobe, anteromedially is the amygdaloid complex of nuclei, with the hippocampal formation situated posterior to it. Located medial to the amygdala is the basal forebrain nuclei, which receive afferent neurons from the reticular formation, the hypothalamus, and the limbic cortex. From this basal forebrain, efferents project to all areas of the cerebral cortex, the hippocampus, and the amygdaloid body, providing an important connection between the neocortex and the limbic network. These nuclei represent the center of the cholinergic system, which supplies acetylcholine to limbic and cortical structures involved in memory formation. Depletion of acetylcholine in clients with Alzheimer disease relates to their memory loss.192,320,321,439
Interlinking the components of the system
The limbic network has many reciprocating interlinking circuits among its component structures, which provide for much functional interaction and also allow for continuing adjustments with continuous feedback (Figure 5-15).56,429 The largest pathway is the fornix.440
Another limbic pathway is the stria terminalis, which originates in the amygdaloid complex and follows a course close to the fornix to end in the hypothalamus and septal regions. The amygdala and the septal region are also connected by a short direct pathway called the diagonal band of Broca. A third pathway, the uncinate fasciculus, runs between the amygdala and the orbitofrontal cortex.56,441,442
The medial forebrain bundle and other parallel circuits (see Figure 5-14) are vital connections of the limbic network.443 These pathways course through the lateral hypothalamus to terminate in the cingulate gyrus in its ascending limb and in the reticular formation of the midbrain in its descending part; these pathways have strong interconnections and control over the periaqueductal gray area.192 These links enable the limbic network itself and the non–limbic-associated structures to act as one neural task system. No portion of the brain, whether limbic or nonlimbic, has only one function.56 Each area acts as an input-output station. At no time is it totally the center of a particular effect, and each site depends on the cooperation and interaction with other regions. For therapists the concept of neuroplasticity within the motor system is incorporated into our theories of motor learning, but we still have difficulty integrating sensory, emotional, and motor components as interactive elements in motor performance. Yet research is identifying that these neurocircuitries are present and interactive.444
The parvicellular reticular formation (PCRF, or lateral medullary reticular formation), together with the nucleus tractus solitarius, receives both vestibular and nonvestibular input from the cortex, cerebellum, and limbic network and is considered functionally as the vomiting center. It also receives input from the area postrema (floor of the fourth ventricle), which contains the chemoreceptor region for the production of vomiting in response to noxious chemicals. Commissural fibers from the vestibular nuclei complexes run through the PCRF and connect the vestibular nucleus to the reticular formation through axon collaterals. The PCRF also projects fibers to the parabrachial nuclei that contain the respiratory centers and to the hypoglossal nucleus.378 Visceral autonomic input from multiple sources, including the vestibular nuclei, converges in the parabrachial nucleus. The locus ceruleus and autonomic brain stem nuclei also receive vestibular nuclear input.234,445–448 Thus, cardiovascular activity and respiration (brain stem–mediated autonomic activity), as well as vomiting, are highly influenced by the status of the vestibular system. If we could understand how cold to the neck or forehead, pressure to the wrist, or taste or olfactory input of ginger interacts with known autonomic reactions and nausea in response to chronic vestibular or interneuronal connections problems, the synthesis of many aspects of health care delivery would no longer be a mystery. Obviously, these older treatment techniques are effective and have been for thousands of years, but to today’s researchers the “why” drives the desire to better understand the neuromechanisms underlying the observable responses. There are three different types of drugs that neuroanatomically suppress or modulate vestibular input and thus have a dramatic effect on dizziness and nausea.449
Research involving functional MRI (fMRI) supports the concept that there is increased activity within the inferior frontal cortex when nausea is induced by either vestibular stimulation or ingestion of an emetic.450 This research verifies that there is a strong interconnection among vestibular input, limbic nuclei, and autonomic responses.451
There are also connections between the parabrachial nucleus and higher brain centers, including the amygdala, which is known to be critical in the development of conditioned avoidance, such as found in agoraphobia, as an example. Thus, vestibular input results in a sensory stimulus that may induce a state of general autonomic discomfort as a trigger of avoidance that precedes the onset of a panic attack.378,445,451,452
Vestibular firing rates are modulated and regulated from the DRN of the midbrain and rostral pons. The DRN is the largest producer of serotonin in the brain and explains the significant linkage between vestibular dysfunction and anxiety, and sleep deprivation and anxiety.237
Vestibular lesions in animals result in dramatic changes in the morphology and function of the hippocampus. Of note is that bilateral vestibular lesions have been associated with hippocampal atrophy. The hippocampus is responsible for spatial and gravitational orientation, cognition, learning, and memory (spatial and nonspatial).379–387
During the past decade anatomical pathways have been identified that are descending motor tracts that terminate in the caudal brain stem and spinal cord.453–455 These pathways help modulate the activity level of somatic and autonomic motor neurons. Some of these tracts receive direct and indirect afferent information from the periphery and are part of the interneuronal projection system to motor neurons. They are found in the caudal brain stem, in the spinal cord, and between the two and play a role in the generation of fixed action patterns such as biting and swallowing, which have a strong emotion context linked to the motor program.456,457 Some of the pathways are linked with the ventromedial and lateral systems, identified for many years as part of the proximal and axial and distal motor control system, modulated by a variety of structures.192,457 They connect the limbic network to the brain stem and spinal neuronal pools. These tracts do not seem to synapse on what would be considered true motor nuclei of the brain stem (e.g., red nucleus, vestibular nuclei, lateral reticular nuclei, interstitial nuclei of Cajal, or inferior olive). However, these pathways do connect with raphe nuclei, periaqueductal gray matter, and locus coeruleus. The medial components of these tracts originate within the medial portion of the hypothalamus, and the lateral portion originates in the limbic network (lateral hypothalamus, amygdala, and bed nucleus of the stria terminalis). The prefrontal area may be the master controller over this regulatory system.458–461 The functional motor implication of these tracts is determined by whether the fibers project as part of a medial or lateral descending system. The medial system, through the locus coeruleus, periaqueductal gray matter, and raphe spinal pathways, plays a role in the general level of activity of both somatosensory and motor neurons. Thus the emotional brain or limbic network has an effect on both somatosensory input and motor output. These fibers can alter the level of excitation to the first synapse of somatosensory information, thus altering the processing or importance of that information as it enters the nervous system. Similarly, it can alter the level of motor generators involved in motor expression, which may account for the extension with anger and flexion with depression. The lateral system seems to be involved in more specific motor output related to emotional behavior and may explain some of the loss of fine motor skill when one is placed in an emotional situation such as competition. To differentiate whether the tonal conditions of a client are a result of limbic imbalance or problems within the traditionally accepted motor system, the clinician would need to observe the emotional state and how it changes within the client. If the abnormal state consistently alters with mood shifts, then limbic involvement causing motor control disturbances would be identified. Human social behavior requires motor expression, yet that behavior is driven through the limbic circuitry.444,462–464 Neuroimaging has helped to reduce uncertainty concerning the anatomical pathways, and neurochemistry has widened the possibilities of variations across synaptic connections.465–467
Neurobiology of learning and memory
Functional applications for an intact system
“Ultimately, to be sure, memory is a series of molecular events. What we chart is the territory within which those events take place.”123 Although expressed more than four decades ago, these words are still accurate. They were expressed by a master clinician and researcher, a clinician who watched behavior, emphasized neuroscience, stressed accurate documentation, and always was respectful and aware of patient interaction and how that affected motor behavior.
The brain stores sensory and motor experiences as memory. In processing incoming information, most sensory pathways from receptors to cortical areas send vital information to the components of the limbic network. For example, extensions can be found from the visual pathways into the inferior temporal lobe (limbic network).56,468,469 Visual information is “processed sequentially” at each synapse along its entire pathway, in response to size, shape, color, and texture of objects. In the inferior temporal cortex, the total image of the item viewed is projected. In this way the sensory inputs are converted to become “perceptual experiences.” This also applies to other sensory stimuli, such as tactile, proprioceptive, and vestibular. The process of translating the integrated perceptions into memory occurs bilaterally in the limbic network structures of the amygdala and the hippocampus.56,470–481
Before the limbic network’s impact on learning and memory can be delved into, a clear understanding of what is meant by these functions is needed. Current theories support a “dual memory system” that uses different pathways in the nervous system. Terms such as verbal and nonverbal, habit versus recognition, intrinsic and extrinsic, and procedural and declarative have been given to these two memory systems. These systems do not operate autonomously, and many therapeutic activities seem to combine these memory systems to achieve functional behavior.56 In reality, the complexity of memory is not a two-category system. Verbal and nonverbal memory both interact with declarative function.482 Even within spatial memory, additional areas of integration and parallel circuitry have been identified.483,484
For this discussion, two specific categories of learning—procedural and declarative—will be used, although in today’s neuroscience environment, the terms implicit and explicit memory are used as frequently. Both categories of learning have been correlated to limbic function.485–487 Declarative (explicit) memory entails the capability to recall and verbally report experiences. This recall requires deliberate conscious effect, whereas the procedural counterpart is the recall of “rules, skills, and procedures (implicit),”56 which can be recalled unconsciously.
Procedural learning is vital to the development of motor control. A child first receives sensory input from the various modalities through the thalamus, terminating at the appropriate sensory cortex. That information is processed, a functional somatosensory map is formulated,124,488 and the information is programmed and relayed to the motor cortex. From there, it is sent to both the basal ganglia and the cerebellum to establish plans for postural adaptations, refinement of motor programs, and coordination of direction, extent, timing, force, and tone necessary throughout the entire sequence of the motor act. Storage and thus retrieval of memory of these semiautomatic motor plans are thought to occur throughout the motor control system.56 The complexity of this process has had an impact on the study of motor control and variables that might affect that control.489
The frontal lobe, basal ganglia, and cerebellum are critical nuclei for changing and modulating existing programs.56 Many interlocking neuronetworks establish pathways allowing for the conceptualization of research on motor theory concepts of reciprocity, distributed function, consensus, and so on (see Chapter 4). Procedural learning and memory do not necessitate limbic network involvement as long as an emotional value is not placed on the task. This memory deals with skills, habits, and stereotyped behaviors. This motor system is involved in developing procedural plans used in moving us from place to place or holding us in a position when we need to stop.56
Unlike procedural learning and memory, declarative (explicit) learning and memory require the wiring of the limbic network. Recent literature has clearly identified that the basal ganglia and cerebellum both play roles in cognitive function, especially as it relates to category learning tasks.490 This type of learning is closely associated with limbic function, further identifying the complexity of what was considered two entirely separate systems. Declarative thought deals with factual, material, semantic, and categorical aspects of higher cognitive and affective processing. A strong emotional and judgmental component is linked with declarative thought. Thus as soon as a motor behavior has value placed on the act, it becomes declarative as well as procedural, and the limbic network may become a key element in the success or failure of that movement.491,492 Most functional tasks or activities practiced in a clinical setting have value attached to them. That value can be clearly seen by observing the emotional intent placed on the activity by the client.493
The hippocampus may be more concerned with sensory and motor signals relating to the external environment, whereas the amygdala is concerned more with those of the internal environment. They both contribute in relation to the significance of external or internal environmental influences.475,494–499 The hippocampus is rich in stem cells and may be a primary nuclear mass that directs the bodily systems to heal after injury. This is especially true when the external environment is enriched and nurtures the emotional environment for that healing.500,595
The amygdaloid circuits seem to deal with strongly emotional and judgmental thoughts, whereas the hippocampal circuits are less emotional and more factual. The amygdala may be more involved in emotional arousal and attention, as well as motor regulation, whereas the hippocampus may deal with less emotionally charged learning. These limbic circuits seem crucial in the initial processing of material that leads to learning and memory. Once the thought has been laid down within the cortical structures, retrieval of that specific intermediate and long-term memory does not seem to require the limbic network, although new associations will need to be run through the system.56,471,473,475
A third component in the memory pathway involves the medial diencephalon, a structure that contains the thalamic nucleus. When this region is destroyed by neurotrauma such as strokes, neoplasms, infections, or chronic alcoholism, global amnesias result, owing to the destruction of the amygdala and hippocampus. The amygdala and hippocampus send fibers to specific target nuclei in the thalamus, and the destruction of these tracts also causes the same amnesic effect. It appears that the limbic network and the diencephalon cooperate in the memory circuits. The medial diencephalon seems to be another relay station along the pathway that leads from the specific sensory cortical region to the limbic structures in the temporal lobe to the medial diencephalic structures and ends in the ventromedial part of the prefrontal cortex (Figure 5-16).56,501,502
As shown in Figure 5-16, memories may be stored in the sensory cortex area, where the original sensory input was interpreted into “sensory impressions.” Today, concepts regarding memory storage suggest that declarative memory is stored in categories similar to a filing system. Those categories or files seem to be stored in several cortical areas bilaterally depending on the context.503,504 This system allows for easy retrieval from multiple areas. Memory has stages and is continually changing. It was once thought that the hippocampus only dealt with long-term memory, but it is now accepted that it also supports multi-item working memory.505 To go from short-term to long-term memory, the brain must physically change its chemical structure (a plastic phenomenon). Memory first begins with a representation of information that has been transformed through processing of perceptual systems. The transferring of this new memory into a long-lasting chemical bond requires the neuronetwork of the limbic complex. Owing to the multiple tracts or parallel circuits in and out of the limbic network and throughout neocortical systems, clients, even with extensive lesions, can often learn and store new information.56,506 This may also explain why damage to the limbic network structures does not destroy existing memory nor make it unavailable because it is actually stored in many places throughout the neocortex. The circular memory circuit illustrated in Figure 5-16 shows only one system. The reader must remember that many parallel circuits function simultaneously. The circular memory circuit shown reverts to the original sensory area after activation of the limbic structures to cause the necessary neuronal changes that would inscribe the event into retrievable stored memory.507 This information can be recognized and retrieved by activation of storage sites anywhere along the pathway.56,508
The last station or system to be added to the circuit is the “basal forebrain cholinergic system,” which delivers the neurochemical acetylcholine to the cortical centers and to the limbic network, with which it is richly linked. The loss of this neurotransmitter is linked to memory malfunctioning in Alzheimer disease. Currently, many chemicals are being studied for their influence on brain structures and specially limbic structures.509,510 Similarly, loss of this cholinergic system plays a key role in dementia problems in Parkinsonism.511 Performance of visual recognition memory can be augmented or impaired by administration of drugs that enhance or block the action of acetylcholine.512–514
It has also been shown that the amygdala and hippocampus are interchangeably involved in recognition memory.515 The hippocampus is vital for memory of location of objects in space, whereas the amygdala is necessary for the association of memories derived through the various senses with a specific recognition recall. For example, a whiff of ether might bring to mind a painful surgical experience or the sight of some food may cause a recall of its pleasant smell. Removal of the amygdala brings out the behavior shown in Klüver-Bucy syndrome. For clients with this neurological problem, familiar objects do not bring forth the correct associations of memories experienced by sight, smell, taste, and touch and relate them to objects presented.516 Association of previously presented stimuli and their responses appear to be lost. Animals without amygdaloid input had different response patterns that ignored previous fears and aversions. Thus the amygdala adds the “emotional weight” to sensory experience. Loss of the amygdala takes away many positive associations and potential rewards, thereby altering the shaping of perceptions that lead to memory storage.
When stimuli are endowed with emotional value or significance, attention is drawn to those possessing emotional significance, selecting these for attention and learning. This would give the amygdala a “gatekeeping” function of selective filtering. The amygdala may enable emotions to influence what is perceived and learned by reciprocal connection with the cortex. Emotionally charged events will leave a more significant impression and subsequent recall. The amygdala alters perception of afferent sensory input and thereby affects subsequent actions.126,517,518
In the human, memory functioning has been associated with the phenomenon of long-term potentiation observed in hippocampal pathways.56 This potentiation of synaptic transmission, lasting for hours, days, and weeks, occurs after brief trains of high-frequency stimulation of hippocampal excitatory pathways. Whether this phenomenon is caused by alteration at the presynaptic or postsynaptic terminals has not been established, and the complexity continues to evolve.250 The question remains whether there is an increased amount of neurotransmitter released presynaptically (glutamate) or whether the expected amount is producing a heightened postsynaptic response. Or, are both sites involved56? Even a third hypothesis regarding nonsynaptic neurotransmission or exocytoses with receptor sites on the surface of neurons beyond postsynaptic sites may help guide our understanding of memory and memory storage in the future.56,192 Recent literature has linked a neurotropic factor usually considered for long-term potentiation within the hippocampus as a factor in amygdala-dependent learning, thus reiterating the interaction between these two nuclei and their role in memory and learning.126
Learning and memory evoke alterations in behavior that reflect neuroanatomical and neurophysiological changes.56,115 These alterations include the phenomenon of long-term potentiation as an example of such changes. The hippocampus demonstrates the importance of input of long-term potentiation in associative learning. In this type of learning, two or more stimuli are combined. Tetanizing of more than one pathway needs to occur simultaneously. When only one pathway is tetanized, the effect is decreased synaptic transmission. Long-term potentiation, requiring the cooperative action of numbers of coactive fibers, is engendered and formed by the “associative” interaction of afferent inputs. Thus, long-term potentiation serves as one model for understanding the neural mechanism for associative learning. Interacting with this neural mechanism are hormones,which, combined with stress, can change the specific circuitry active during the experience.519 As our understanding of the complexity of the limbic network evolves, limbic responses to input stimuli need to be differentiated from limbic memory and initiation of a response without the stimuli. Recent research has shown that the amygdala is not only involved in learning related to emotional experiences but is also responsible for changing motor expression or conditioned response generated as part of an autonomic fear expression.444,520
Learning and memory problems after limbic involvement
For initial declarative learning and memory, the combination of hippocampus and amygdala of the limbic network is required.56 For memory formation to occur, there must be a storing of the “neural representation” of the stimuli in the association and the processing areas of the cortex. This storage occurs when sensory stimuli activate a “cortico-limbo-thalamo-cortical” circuit.56 Although there is not one single all-purpose memory storage system, this circuit serves as the “imprinting mechanism,” reinforcing the pathway that activated it. On subsequent stimulation, a stimulus recognition or recall would be elicited. In associative recall, stored representations of any interconnected imprints could be evoked simultaneously.56
A vital processing area for all sensory modalities is located in the region of the anterior temporal lobe. This area is directly linked with the amygdala and indirectly with the hippocampus. The hippocampus and amygdala are also linked both structurally and functionally to each other and to specific thalamic nuclei. Clients with temporal epileptic seizures and whose temporal lobes have been surgically removed develop global anterograde amnesia—that is, amnesia develops for all senses, and no new memories can be formed. Experimental removal of only the hippocampus does not bring about these changes, although processing is slowed down. When both the hippocampus and the amygdala are removed bilaterally, the amnesia is both retrograde and global. It is postulated that the amygdala is the area of the brain that adds a “positive association,” the reward part to stimuli received and passed through processing. In this way, stimulus and reward are associated by the amygdala, and an emotional value is placed on them.521,522
It appears that limbic involvement in the declarative memory creates a chemical bond that allows cortical storage of “stimulus representation” necessary for subsequent recognition and recall of the information.56,471,473,474,494
When declarative and procedural learning from a clinical reference is analyzed, a separation of functional mediation can be observed. Clients with brain lesions localized in the limbic network components of the amygdala and hippocampus have the ability to acquire and function with “rule-based” games and skills but have lost the capacity to recall how, when, or where they gained this knowledge or to give a description of the games and skills learned. Relating this to clinical performance, clients may develop the skill in a functional activity but not the problem-solving strategies necessary to associate danger or other potentially harmful aspects of a situation that may develop once out of the purely clinical setting.212,428,523–525 Similarly, if a client needs to learn a procedural task such as walking, transfers, eating, and so on, it may be extremely important to direct the attention off the task while the task is being practiced procedurally. As knowledge about the complexity of memory evolves, the clear dichotomy between explicit and implicit learning or declarative and procedural learning is being questioned by current research.526 This study clearly demonstrates that anterograde amnesia affects learning that is dependent on combining a novel association with the development of memory compared with its accessibility to consciousness. As the specificity and generalizability of memory come under scrutiny, a question arises regarding the differentiation of semantic memory from music perception, music production, and music memory.527 If emotional and associational aspects of music memory are different from declarative memory and if both are different from procedural memory, then perhaps music may be used to activate existing robust and rich neural networks linking different kinds of memory and learning, and/or elicit neuroplasticity potentials, to address therapeutic goals.528
Neurochemistry
Discussion of the limbic network’s intricate regulation of many neurochemical substances is not within the scope of this chapter. Yet therapists need to appreciate how potent this system can be with respect to neurochemical reactions. The amount of research reflecting new understanding of the role of neurochemistry in brain function is inundating the pharmacological research literature on a monthly basis.479,529–536
The hypothalamus, the physiological center of the limbic network (see Figures 5-2 and 5-14), is involved in neurochemical production and is geared for passage of information along specific neurochemical pathways.
Squire and colleagues537 consider it the major motor output pathway of the limbic network, which also communicates with every part of this system. Certain nuclei of the hypothalamus produce and release neuroactive peptides that have a long-acting effectiveness as neuromodulators. As such, they control the levels of neuronal excitation and effective functioning at the synapses. By their long-lasting effects, they regulate motivational levels, mood states, and learning. These peptide-producing neurons extend from the hypothalamic nuclei to the ANS components and to the nuclei of the limbic network, where they modulate neuroendocrine and autonomic activities. The importance of these neuropeptides is being recognized as research begins to unravel the mysteries of the limbic network’s role in the regulation of affective and motivated behaviors.56,140,192,538–540 Lesions in the medial hypothalamus affect hormone production and thus alter regulation of many hormonal control systems.56 For example, clients with medial hypothalamic lesions may have huge weight gain because of the increase of insulin in the blood, which increases feeding and converts nutrients into fat. Similarly, this weight gain may be caused by hyperphagic responses resulting from the loss of satiety. General hyperactivity and signs of hostility after minimal provocation can also be observed. These problems are often encountered in patients with head trauma.
Lesions in the lateral hypothalamus lead to damage of dopamine-carrying fibers that begin in the substantia nigra and filter through the hypothalamus to the striatum. Lesions, either along this tract or within the lateral hypothalamus, lead to aphagia and hypoarousal. Decreased sensory awareness contributing to sensory neglect is also present in lateral hypothalamic lesions. The decreased awareness may be caused by a decrease of orientation to the stimuli versus awareness of the stimuli once they are brought to conscious attention. These lesions cause the client to exhibit marked passivity with decreased functioning. Bilateral infarcts within the mammillothalamic tract create an acute Korsakoff syndrome.541
As noted earlier, depression is clearly identified as a limbic function. A functional deficiency in monoamines, especially serotonin, is hypothesized to be a primary cause of depression.542,543 The serotonin systems originate in the rostral and caudal raphe nuclei in the midbrain. Ascending serotonergic tracts start in the midbrain and ascend to the limbic forebrain and hypothalamus; they are concerned with mood and behavior regulation. Damage with direct or indirect limbic involvement results in the client exhibiting depression. Descending pathways to the substantia gelatinosa are involved in pain mechanisms and have also been linked through a complex sequence of biochemical steps to the increased sensitization of the presynaptic terminals of the cutaneous sensory neurons, leading to a hyperactive withdrawal reflex or hypersensitivity to cutaneous input.56 This would account for the behavior patterns seen in clients with head trauma, when the therapist sees a flexed posture with a withdrawn or depressed affect yet with an extremely sensitive tactile system.
It is hypothesized that the underlying pathophysiological mechanism of one form of schizophrenia involves an excessive transmission of dopamine within the mesolimbic tract system.56 The dopaminergic cell bodies are located in the ventral tegmental area and the substantia nigra. Some of these neurons project to the limbic network. These projections go to the nucleus accumbens, the stria terminalis nuclei, parts of the amygdala, and the frontal entorhinal and anterior cingulate cortex. It is the projection to the nucleus accumbens that seems critical because of its influence over the hippocampus, frontal lobe, and hypothalamus. This nucleus may act as a filtering system with respect to affect and certain types of memory, and the dopaminergic projections may modulate the flow of neural activity.56 The masked facies caused by the impaired motor activity seen in clients with Parkinson disease and the paranoid-schizophrenic behaviors observed in some clients with CNS damage may directly reflect these mesolimbic dopaminergic systems.
The specific roles of the noradrenergic pathway are numerous and affect almost all parts of the CNS. The center for the noradrenergic pathways is located within the caudal midbrain and upper pons. Its nucleus is referred to as the locus coeruleus. This nucleus sends at least five tracts rostrally to the diencephalon and telencephalon.56 Of specific interest for this discussion are the projections to the hippocampus and amygdala. The axons of these neurons modulate an excitatory effect on the regions where they terminate.56 Thus the activation of this system will heighten the excitation of the two nuclei within the limbic network intricately involved in declarative learning and memory. Hyperactivation may cause overload or the lack of focus of attention.544 Decreased activity may prevent the desired responses. Attention to task may depend on continuing noradrenergic stimulation. These tracts from the midbrain rostrally play a key role in alertness. The correlation of alertness and attention to performance of motor tasks as well as to learning can be demonstrated.56 Again, these research findings reiterate previous statements regarding a therapist’s role in balancing the neurochemistry within the client’s limbic network. From a clinical perspective, a therapist will observe a relaxed, motivated, alert participant in the learning environment and will observe better carryover because the chemical interactions will only enhance the learning.
More than 200 neurotransmitters have been identified within the nervous system.56 How each transmitter and the interaction of multiple transmitters on one synapse affect any portion of the CNS is still unclear. Certainly, some relationships have been identified. Novelty-seeking behavior of the limbic network seems to be dopamine dependent,545 whereas melatonin receptors seem to coordinate circadian body rhythm.546 Adrenal corticosteroids modulate hippocampal long-term potentiation.547 The complexity of this system still challenges many researchers.