17 The integumentary system
Desquamation: The process by which dead cells are shed at a fairly constant rate.
Dermis: Corium, or the second layer of the skin.
Epidermis: Multilayered outer covering of the skin.
Frostbite: Trauma caused by the crystallization of tissue fluids in the skin or subcutaneous tissue.
Integumentary system anatomy
The skin, or integument, provides a boundary between the internal and external environments of the body. With aging, the skin becomes thinnerwith less elasticity and diminished collagen. There is less inflammatory response and integumentary immunity protection with aging. Skin generally accounts for about 15% of the total body weight. The skin is divided into two major layers: the epidermis and the dermis, which includes the hypodermis (Fig. 17-1). Depending on location, skin varies in number of layers and thickness. The soles of the feet and palms of the hands have the thickest skin (approximately 1.5 mm) and have five layers. Eyelids have the thinnest skin (approximately 0.10 mm) and have four layers.
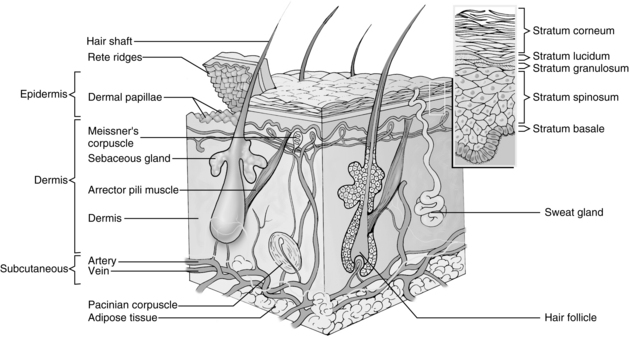
FIG. 17-1 Layers of epidermis.
(From Monahan FD, et al: Medical-surgical nursing health and illness perspectives, ed 8, St. Louis, 2007, Mosby.)
Hypodermis
The hypodermis functions as a shock absorber and heat insulator. Located under the dermis, it comprises fat, smooth muscle, and adipocytes. These cells store and accumulate necessary fats. The hypodermis acts as a site of energy production, and insulation. This area of the body stores fat in characteristic locations: hips on women, abdomen in men.2
Integumentary functions
Thermoregulation
Skin, subcutaneous tissue, and fat in the subcutaneous tissue provide heat insulation for the body. Heat is lost from the body to the surroundings by radiation, conduction, convection, and evaporation (Fig. 17-2). Radiation of heat from the body accounts for approximately 60% of the total heat loss. In this mechanism, heat is lost in the form of infrared heat waves. Conduction of heat to objects represents approximately 3% of the total heat loss, whereas conduction of heat to the air represents approximately 15% of the total heat loss. When water is carried away from the skin by air currents, convection of heat occurs. Evaporation constitutes approximately 22% of the heat loss. Even without sweating, water still evaporates from the skin and the lungs; this is called insensible loss and totals approximately 600 mL/day.
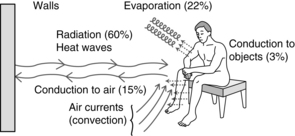
FIG. 17-2 Major mechanisms of heat loss from body.
(From Hall JE: Guyton and Hall textbook of medical physiology, ed 12, St. Louis, 2011, Saunders.)
The skin regulates body temperature by conserving heat in a cold environment. Sweating can lower the body temperature in hot environments. The sweat glands are innervated by the sympathetic and parasympathetic nervous systems. When the anterior hypothalamus, in the preoptic area of the brain, is stimulated by excess heat, impulses are sent from this area by way of the autonomic pathways to the spinal cord. From the spinal cord through the sympathetic outflow tracts, the impulses go to the skin all over the body. The sweat glands are innervated by sympathetic nerve fibers. However, in these specific fibers, the neurotransmitter is acetylcholine. Consequently, these fibers are actually sympathetic cholinergic nerve fibers and are stimulated by epinephrine or norepinephrine. Norepinephrine is a catecholamine that is a hormone and neurotransmitter that assists with the fight-or-flight response. It is responsible for cutaneous vasoconstriction and has been associated with the pain of fibromyalgia.3
Protection
The skin protects the body from injurious physical, chemical, electric, thermal, or biologic stimuli. Of particular importance to the perianesthesia nurse is the presence of bacteria on the skin that can cause infection when a patient’s skin barrier is broken. Normal florae of the skin include Staphylococcus, Streptococcus, and Corynebacterium organisms. Diphtheroids are also widely distributed on the skin, especially in moist areas. The normal pH of the skin is 4 to 6.5, resulting from production of lactic acid and residues of amino acids. This slightly acid environment serves a protective mechanism by inhibiting bacterial growth. Diabetic, cardiac, and renal patients tend to have more alkaline skin surfaces, thus being at higher risk for skin infections.4
Importance of aseptic technique
Because all skin has disease-causing organisms on its surface, skin can never be sterile. Precautions should be taken to reduce the number of pathogenic organisms that may be introduced into a wound. Good hand washing technique is the most important activity in the prevention of disease transmission. Hands should be washed using traditional hand washing techniques, or using one of the new sanitizing gels before caring for any patient. When hands are visibly soiled, traditional washing should occur.5
Standard precautions in the postanesthesia care unit
The Centers for Disease Control and Prevention developed a guideline for preventing transmission of infectious agents in health care settings.6 This document is discussed in Chapter 5 with more complete information on the standard precautions in the PACU.
Sterile technique for intravenous therapy
Establishment of an intravenous infusion should be accomplished via sterile technique. The site chosen for venipuncture and cannula (needle) placement should be prepared using aseptic technique according to institutional policies and guidelines. There are many good quality pre-packaged IV prep kits. In general though, all IV preparation includes thorough cleaning of the site with alcohol or Betadine-based preparation solutions, the use of sterile angiocatheters, supplies, and an occlusive dressing over the cannulated site. After the intravenous administration route is established, the cannula should be securely anchored to prevent irritating back-and-forth motion and to avoid potential transport of cutaneous bacteria into the puncture wound.
Burn injuries
A burn, no matter how small, represents a total body assault. The postoperative care of the patient with burn injury can be most challenging to the perianesthesia nurse. These patients usually have a complex array of physiologic complications, from deranged fluid and electrolyte balance to respiratory complications. These patients are also routinely suffering from psychologic problems related to pain, disfigurement, anxiety, and potential permanent lifestyle changes. With their first line of defense against external assaults disrupted, temperature regulation of the burn patient is compromised. It is difficult to maintain normothermia in these patients; the perioperative nurse must take care to prevent burn patients from experiencing hypothermia or hyperthermia. Infection is the most common complication of a burn injury. Meticulous, aseptic skin care is of primary importance. Nursing care of the patient with a burn injury is complex; the reader should refer to Chapter 55 for a discussion of specific pathophysiologic processes, assessment, and nursing interventions for the patient with a burn injury in the PACU.
The terms partial thickness, deep, and full thickness are commonly used in the classification of burn injuries. The terms first degree, second degree, third degree, and sometimes fourth degree are based on the degree of destruction, depth, and surface appearance of the burn wound (Fig. 17-3). Ambroise Paré, a French surgeon from the 1500s, developed the burn classification system that is still in use today.
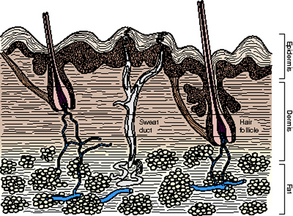
FIG. 17-3 Cross section of skin depicting levels contained in split-thickness and full-thickness skin grafts.
(From Townsend T, et al: The biological basis of modern surgical practice, ed 18, Philadelphia, 2008, Saunders.)
A partial-thickness burn heals without grafting. Grafting is required when part of the skin has been damaged or destroyed, but enough epithelial cells remain in the skin to provide new epidermis. The partial-thickness burn can also be referred to as a first-degree or second-degree burn. Partial-thickness burns can be divided into three categories: (1) superficial burns, in which partial skin loss is seen but no dermal death and therefore no slough; (2) intermediate partial-thickness burn, typically characterized by healing from the level of the hair follicles; and (3) deep partial-thickness burn, which typically heals from the level of the sweat ducts. A deep dermal burn is a partial-thickness burn that can heal without grafting. However, if the burn is complicated by infection or mechanical trauma, it is likely to be converted into a full-thickness burn. Full-thickness, or third-degree, burns cause destruction of all the skin. No viable epithelial elements are present, and destruction of the subcutaneous tissue, muscles, and bones may be seen. The wound must be grafted because the skin will not regenerate.7
The effects of burns ranges from redness and a burning sensation to edema, blisters, excruciating pain, debilitating and devastating scarring, shock, and death. Burn patients often require frequent, numerous surgeries to remove dead tissue (debridement), release scarring, and apply split thickness skin grafts or one of the many other applications now available: artificial skin, cultured skin autografts, or collagen-based allograft membranes.8 As a result, the perianesthesia nurse may see these patients repeatedly in the preoperative and PACU areas.
Summary
It is important for the perianesthesia nurse to have an understanding of the anatomy and physiology of the integumentary system in order to appropriately care for patients who are at risk because of disturbances in this system. The importance of following aseptic technique and universal precautions cannot be understated. With all the possible infectious agents and opportunistic organisms seen in the surgical arena, the perianesthesia nurse needs an understanding of the basics of the integumentary system as presented here. For a more comprehensive description of PACU infection control, see Chapter 5 for aseptic technique; and for care of the patient with burn injury, see Chapter 55.
1. Drake R, et al. Gray’s anatomy for students. Philadelphia: Churchill Livingstone; 2005.
2. Marks JG, Miller J. Lookingbill and Marks principles of dermatology, ed 4. St. Louis: Saunders; 2006.
3. Blumenfeld H, Taylor LA. The role of serotonin norepinephrine reuptake inhibitors in the treatment of fibromyalgia: a guide for the physician assistant. The Internet Journal of Academic Physician Assistants. 2009;4(2). available at http://www.ispub.com/journal/the_internet_journal_of_academic_physician_assistants/volume_4_number_2_7/article_printable/the_role_of_serotonin_norepinephrine_reuptake_inhibitors_in_the_treatment_of_fibromyalgia_a_guide_for_the_physician_assistant.html Accessed January 14, 2012
4. Graham-Brown R, Bourke J. Mosby’s color atlas and text of dermatology, ed 2. St. Louis: Mosby; 2007.
5. Center for Disease Control and Prevention: Handwashing clean hands save lives. available at: http://www.cdc.gov/handwashing, January 14, 2012. Accessed
6. Siegel JD, et al. and the Healthcare Infection Control Practices Advisory Committee: 2007 Guideline for isolation precautionspreventing transmission of infectious agents in healthcare settings. available at: http://www.cdc.gov/hicpac/2007IP/2007isolationPrecautions.html, January 14, 2012. Accessed
7. Nagelhout J, Plaus K. Handbook of nurse anesthesia, ed 4. St. Louis: Saunders; 2010.
8. ECRI Institute: Skin substitutes for treatment of burns. Plymouth Meeting, PA: ECRI Institute; 2009.
Aitkenhead A, et al. Textbook of anesthesia, ed 5. Philadelphia: Churchill Livingstone; 2007.
Atlee J. Complications in anesthesia, ed 2. Philadelphia: Saunders; 2007.
Barash P, et al. Clinical anesthesia, ed 6. Philadelphia: Lippincott Williams & Wilkins; 2009.
Fisher L. Benumof’s anesthesia and uncommon diseases, ed 5. Philadelphia: Saunders; 2007.
Hall J. Guyton and Hall textbook of medical physiology, ed 12. Philadelphia: Saunders; 2011.
Monahan FD, et al. Medical-surgical nursing health and illness perspectives, ed 8. St. Louis: Mosby; 2007.
Walls R, et al. Rosen’s emergency medicine: concepts and clinical practice. St. Louis: Mosby; 2009.





