Chapter 131 The Geriatric Patient
Surgical morbidity and mortality have been shown to be greater in the elderly patient.1 Although this subset of patients is very heterogeneous, the general decline in physiologic reserve and presence of coexistent disease are likely primarily responsible for this finding.2,3 The spine surgeon should be able to recognize specific surgical risk factors and develop an appropriate treatment plan that accommodates the specific needs of elderly patients.
Organ Systems
Cardiovascular System
It has been reported that at autopsy 50% of patients older than 70 years of age have significant cardiovascular disease. The cardiac risk index, a commonly used assessment tool, incorporates myocardial infarction in the past 6 months, uncompensated congestive heart failure, aortic stenosis, nonsinus rhythm greater than five premature ventricular contractions per minute, diabetes mellitus, and age older than 70 years as major risk factors for postoperative cardiac complications of noncardiac surgery4 (Box 131-1).
The basic cardiovascular workup in patients older than 65 years of age should include a thorough history and physical examination and a baseline electrocardiogram. Myocardial infarction, unaccompanied by recognized symptoms, occurs in as much as 10% of elderly patients.5 Reports of syncope or dyspnea are the most suggestive symptoms of this event. Peripheral vascular disease is often present with coronary artery disease and may complicate the diagnosis of neurogenic claudication. Absent peripheral pulses or a history of transient ischemic attacks or stroke should lead to a more comprehensive cardiac workup.
In patients with unstable angina, elective spinal surgery is clearly contraindicated. Patients with well-controlled stable angina, however, have only a slightly increased risk for perioperative cardiac complications, and may therefore be considered for surgery.6 Moderate to severe congestive heart failure is associated with a significant perioperative risk.7–9 Jugular venous distention and peripheral edema are suggestive signs, whereas a history of dyspnea on exertion and orthopnea are symptoms of a more severe form of congestive heart failure.
Respiratory System
Elderly patients are at particular risk for perioperative pulmonary complications for several reasons. Decline in pulmonary function and reserve, underlying chronic obstructive disease and bronchitis, lack of mobility or bed rest associated with spinal surgery, and airway obstruction all can lead to significant morbidity or mortality for these patients.10,11 In a series of 100 patients older than 70 years of age, approximately 40% of those without a history of lung disease had abnormal pulmonary function.12 Pulmonary function tests (spirometry) should be obtained for patients older than 65 years of age or with a history of obstructive lung disease if a ventral approach is being considered.13
A forced expiratory volume in 1 second of less than 50% of the predicted value does not suggest an increased risk of postoperative mechanical ventilation, but combined with dyspnea at rest and arterial hypoxemia, it is an established risk factor.14 Room air arterial blood gas should be tested in elderly patients with lung disease, as well as those with a history of shortness of breath, poor exercise tolerance, orthopnea, or excessive smoking. Elevated partial pressure of carbon dioxide (Pco2) reflects a loss of pulmonary reserve. A preoperative Pco2 of greater than 45 mm Hg is associated with an increased incidence of postoperative pulmonary complications,15 and patients with a Pco2 of greater than 50 mm Hg often require a period of postoperative mechanical ventilation.16
Renal System
Decline of renal function in the elderly is more consistent than that of other organ systems.17 In geriatric patients, serum creatinine levels may be artificially low because of decreased production, caused by a shrinking muscle mass. For this reason, creatinine clearance is the preferred test for patients suspected of having significant renal disease. The effect of chronic nonsteroidal anti-inflammatory drug (NSAID) use on the kidney may also contribute to the decline in renal function with advancing age. These drugs can decrease renal blood flow, adding to an already diminished glomerular filtration rate.18 This has clinical significance in the perioperative patient because water homeostasis may be difficult to achieve in elderly patients, leaving them prone to hyponatremia and volume overload. The use of isotonic fluids, restriction of free water, and careful administration of diuretics may be helpful.
Other Sources of Morbidity
Advanced age itself is a risk factor for deep venous thrombosis.1 Given the risks associated with bleeding after spine surgery, many surgeons are hesitant to anticoagulate, even with deep venous thrombosis demonstrated by venous Doppler ultrasonography. Such patients can be considered for vena cava filter placement or delayed (5 to 7 days after surgery) anticoagulation. All patients should receive aggressive physical therapy with early ambulation and range-of-motion exercises. Pneumatic compression devices should be used on all patients during their period of bed rest.
Malnutrition is associated with increased morbidity and mortality in elderly surgical patients.19 Dietary supplements should be added to the hospital diet of patients with reduced postoperative caloric intake to achieve a protein intake of 1 to 2 g/kg/day.
Advanced age is also a risk factor for wound infection. A sixfold increase in clean wound infections has been reported in patients older than 66 years compared with patients younger than 14 years of age.20 The use of routine perioperative antibiotics, minimizing operative times, appropriate postoperative wound care, and attention to nutritional status all may decrease this risk.
Spinal Disorders in the Elderly Patient
Osteoporosis
Osteoporosis is a state of decreased density of mineralized bone. The biochemical makeup and structure of osteoporotic bone are normal, but the volume density of bone is below normal. Bone mass reaches its maximum in the third decade of life and then begins to decrease.21 At its peak, the maximum surface area of bone crystals in an adult is estimated to be 100 acres.
Loss of bone mineral content predominantly occurs from trabecular bone because of its increased baseline metabolic activity and greater surface area compared with cortical bone. Hence, structures formed of trabecular bone are more susceptible to osteoporosis.22 In vertebral bodies, trabecular bone accounts for 90% of axial load-bearing resistance. As a result of primary osteoporosis, elderly people may sustain vertebral compression fractures with minimal trauma. Current recommendations for the medical management of osteoporosis are summarized in Box 131-2.
Bone densitometry has been shown to predict risk of osteoporosis.23 Currently, two methods are used to evaluate bone density. Dual-energy radiography measures area density (g/cm2) of the spine. This test is simple and accurate and carries a low radiation dose. It is also well tolerated, with a procedure time of 10 to 15 minutes. Quantitative CT scanning is a measurement of true density (g/cm3) through a cross-sectional view of the vertebral body. The precision of this test is excellent, but it can be compromised by patient positioning and movement. The small increase in accuracy provided by this test over dual-energy radiography may not justify the expense, discomfort, and added radiation dose.24 A bone mineral density by dual-energy radiography of 1 g/cm2 carries a fracture risk over time of 32%, whereas a density of less than 0.8 g/cm2 carries a risk of 50%.25,26
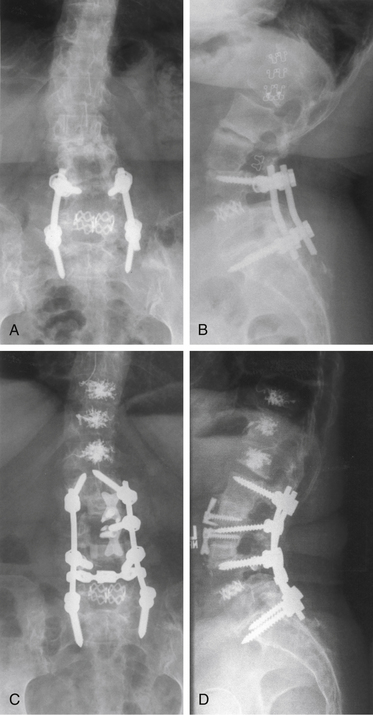
The effect of osteoporosis on vertebrae adjacent to areas of spinal fusion must also be considered. In elderly or osteoporotic patients in whom long fusion constructs are unavoidable, the long-term stability of adjacent vertebral segments is a significant concern. Particularly for areas of high mechanical stress, such as fusions stopping at the thoracolumbar junction, consideration should be given to prophylactic enhancement of the strength of vertebrae adjacent to long fusion constructs through procedures such as vertebroplasty27 (Fig. 131-1).
Osteoporotic Compression Fractures
The most common type of spinal fracture in the elderly patient is the vertebral compression fracture. These fractures occur not only with higher-energy mechanisms but often with bending, lifting, or even during normal activity. Management should be directed primarily toward pain control. It should also be recognized that such low-energy fractures often are the first indication of underlying osteoporosis, and patients should be started on appropriate medical therapy (see Box 131-2).
Elderly patients with osteoporotic compression fractures who are requiring bed rest or significant narcotic analgesia, or for whom disabling pain has persisted over 4 to 6 weeks, may be candidates for percutaneous stabilization procedures, such as vertebroplasty or balloon-assisted vertebroplasty (kyphoplasty).28 However, results of two randomized, controlled trials of vertebroplasty suggest limited benefit to such procedures.29,30 This has led some insurers and academic organizations such as the American Academy of Orthopaedic Surgeons to recommend limits on the use of these procedures. At this time, evidence-based medicine guidelines for vertebroplasty must include the results of these studies, which represent the highest level of medical evidence available on this condition.
Degenerative Lumbar Spondylolisthesis
Degenerative spinal stenosis results from neurologic impingement by the disc, facet joints, and spinal ligaments. Kirkaldy-Willis et al.24 proposed that biochemical and biomechanical changes associated with age cause increased mobility at a spinal segment, leading to osteophyte formation and joint hypertrophy that reduce spinal canal diameter and local stiffness. The increased joint laxity resulting from facet degeneration leads in some cases to spondylolisthesis between adjacent vertebrae.
Two prospective, randomized, controlled trials support treatment of patients with degenerative lumbar spondylolisthesis with laminectomy and dorsal fusion.31,32 Several studies have demonstrated increased fusion rates with pedicle screw instrumentation, and further studies have shown better clinical outcomes in patients who achieve solid arthrodesis.33–35
Despite those results, use of instrumentation has not been convincingly shown to improve clinical outcomes after fusion for patients with degenerative spondylolisthesis.32,36,37 Avoiding instrumentation when performing fusion in elderly, osteoporotic patients with degenerative spondylolisthesis may thus be a reasonable option, particularly when facets are oriented relatively in the coronal plane and segmental instability is not present.
Degenerative Scoliosis
Degenerative scoliosis, unlike idiopathic scoliosis, is an acquired disorder of adult patients. Patients often present with symptoms similar to those of degenerative lumbar stenosis, although for some patients the deformity itself becomes an issue. Nonoperative treatment modalities include physical therapy, muscle relaxants, and NSAIDs. Surgical options include neurologic decompression through laminotomy or laminectomy. Spinal fusion may or may not be appropriate, depending on the patient’s presentation, health status, and expectations from surgery.38–41 There are conflicting reports regarding the need for spinal stabilization after decompression for degenerative scoliosis.38–4042 Patients without lateral listhesis between adjacent vertebrae may be appropriately treated with laminectomy without fusion.
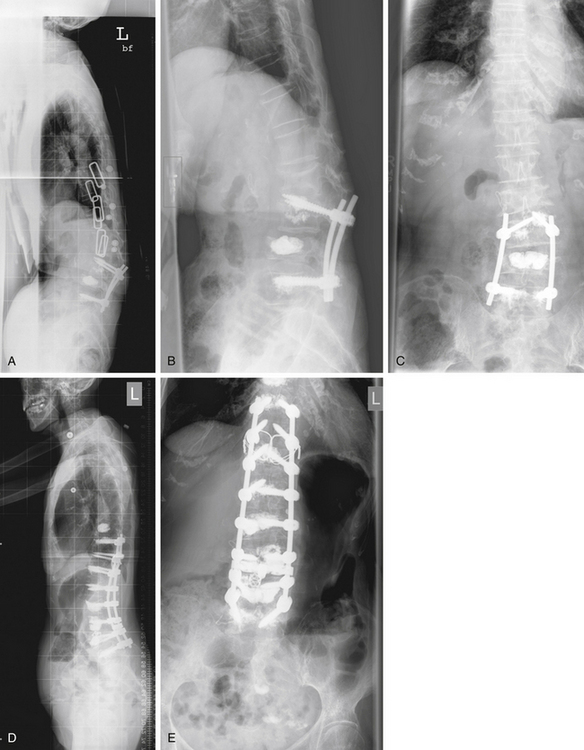
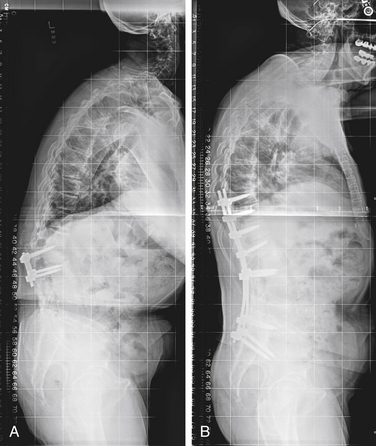
Patients of advanced age with significant scoliotic curves may not be appropriate candidates for the large reconstructive fusion procedures required to treat their spinal deformity. Judiciously selected nerve root blocks with isolated unilateral foraminotomies may be used to good effect in such patients with limited risk of deformity progression (Fig. 131-2). Elderly patients for whom stabilization is required will benefit from efforts to limit the extent of surgery, including use of dorsal (posterior) or transforaminal lumbar interbody fusions in favor of ventral approaches (Fig. 131-3).
Cervical Degenerative Disease
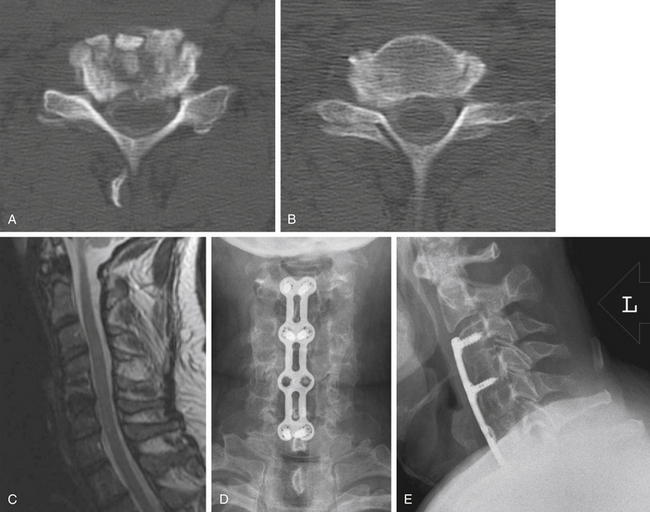
Ventral decompressive surgery by multilevel corpectomy may prove difficult in this patient population. Although ventral decompression may be appropriate on a neurologic basis because of kyphotic alignment of the cervical vertebrae,42 reduced mechanical strength of vertebral bodies increases the risk of graft subsidence or dislodgement if an isolated ventral procedure is performed. In addition, the substantial surgery required to accomplish combined ventral-dorsal cervical reconstruction may not be well tolerated by elderly patients.
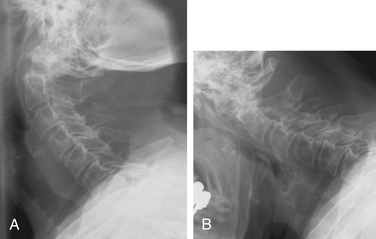
Patients with central stenosis and neutral or lordotic alignment may be treated via an isolated dorsal procedure, such as laminoplasty.42 If ventral decompression is required, standard discectomy/corpectomy procedures with ventral plating may be performed for short segments (Fig. 131-4). Inclusion of dorsal instrumentation should be considered for patients requiring decompression over more than three disc spaces, and for those with significant kyphosis. These treatment approaches generally provide satisfactory clinical outcomes while reducing significant complications.
Spinal Trauma and Spinal Cord Injury
Numerous characteristics of spinal injury are unique in the elderly patient, including injury mechanisms, fracture types, incidence of neurologic deficits, and outcomes. The primary mechanism of injury in young patients is motor vehicle collisions, whereas the leading cause of spine fracture in patients older than 65 years of age is falls.43,44 Significant neurologic deficits are also significantly more common in younger patients than in the elderly, possibly reflecting this difference in injury mechanisms.43,45
Outcomes from traumatic spinal injuries also differ significantly between elderly and nonelderly adult patients. Elderly patients have a significantly lower survival rate than nonelderly adults, both with and without neurologic injury. Neurologic injury is especially devastating in the elderly because the 60-day mortality rate for patients older than 65 years of age with traumatic paralysis approaches 30%.43
Understanding these issues may factor significantly in clinical decision making. Families of elderly patients with significant neurologic injuries should understand the high risk of poor outcomes in this age group. Given the significant risk of early mortality, as well as the likely disability resulting from profound neurologic deficits, patients and families may in some cases prefer withdrawal of support over aggressive interventional treatment.
Finally, injuries appropriately treated with surgical intervention in younger patients may be treatable with minimal intervention in the elderly population. For example, risks associated with nonunion after dens fracture appear to be limited in elderly patients, and it is not clear that surgical stabilization of established nonunions is warranted.28,46 Treatment decisions for these injuries are best decided on a case-by-case basis and depend on patient preferences, health, and mental status, and the nature of the injury (Fig. 131-5).
Fischgrund J.S., Mackay M., Herkowitz H.N., et al. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976). 1997;22:2807-2812.
Hart R.A., Prendergast M. Spine surgery for lumbar degenerative disease in the elderly and osteoporotic patient. Instr Course Lect. 2007;56:257-272.
Irwin Z.N., Arthur M.A., Mullins R.J., et al. Variations in injury patterns, treatment, and outcome for spinal fracture and paralysis in adult versus geriatric patients. Spine (Phila Pa 1976). 2004;29:796-802.
Kornblum M.B., Fischgrund J.S., Herkowitz H.N., et al. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine (Phila Pa 1976). 2004;29:726-733.
Weinstein J.N., Lurie J.D., Tosteson T.D., et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg [Am]. 2009;91:1295-1304.
1. Yoshida M., Otani K., Shibasaki K., et al. Expansive laminoplasty with reattachment of spinous process and extensor musculature for cervical myelopathy. Spine (Phila Pa 1976). 1992;17:491-497.
2. Harbrecht P.J., Garrison R.N., Fry D.E. Surgery in elderly patients. South Med J. 1981;74:594-598.
3. Nunn J.F., Milledge J.S., Chen D., et al. Respiratory criteria of fitness for surgery and anaesthesia. Anaesthesia. 1988;43:543-551.
4. Goldman L. Cardiac risks and complications of noncardiac surgery. Ann Intern Med. 1983;98:504-513.
5. Mangano D.T. Perioperative cardiac morbidity. Anesthesiology. 1990;72:153-184.
6. Wasnich R.D., Ross P.D., Heilbrun L.K., et al. Prediction of postmenopausal fracture risk with use of bone mineral measurements. Am J Obstet Gynecol. 1985;153:745-751.
7. Deron S.J., Kotler M.N. Noncardiac surgery in the cardiac patient. Am Heart J. 1988;116:831-838.
8. Goldman L., Caldera D.L., Nussbaum S.R., et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845-850.
9. McGlinchey-Berroth R., Morrow L., Ahlquist M., et al. Late-life spinal cord injury and aging with a long-term injury: characteristics of two emerging populations. J Spinal Cord Med. 1995;18:183-193.
10. Knudson R.J., Clark D.F., Kennedy T.C., et al. Effect of aging alone on mechanical properties of the normal adult human lung. J Appl Physiol. 1977;43:1054-1062.
11. Levitzky M.G. Effects of aging on the respiratory system. Physiologist. 1984;27:102-107.
12. von Knorring J. Postoperative myocardial infarction: a prospective study in a risk group of surgical patients. Surgery. 1981;90:55-60.
13. Tornebrandt K., Fletcher R. Pre-operative chest x-rays in elderly patients. Anaesthesia. 1982;37:901.
14. Riggs B.L., Wahner H.W., Melton L.J.III, et al. Rates of bone loss in the appendicular and axial skeletons of women: evidence of substantial vertebral bone loss before menopause. J Clin Invest. 1986;77:1487-1491.
15. Thomsen K., Christiensen F.B., Eiskjasr S.P., et al. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spine fusion: a prospective, randomized clinical study. Spine (Phila Pa 1976). 1997;22:2813-2822.
16. Milzman D.P., Boulanger B.R., Rodriguez A., et al. Preexisting disease in trauma patients: a predictor of fate independent of age and injury severity score. J Trauma. 1992;32:236-243. discussion 243–244
17. San Martino A., D’Andria F.M. San Martino C: The surgical treatment of nerve root compression caused by scoliosis of the lumbar spine. Spine (Phila Pa 1976). 1983;8:261-265.
18. Garella S., Matarese R.A. Renal effects of prostaglandins and clinical adverse effects of nonsteroidal anti-inflammatory agents. Medicine (Baltimore). 1984;63:165-181.
19. Bastow M.D., Rawlings J., Allison S.P. Undernutrition, hypothermia, and injury in elderly women with fractured femur: an injury response to altered metabolism? Lancet. 1983;1:143-146.
20. Cruse P.J., Foord R. The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27-40.
21. Rowe J.W., Andres R., Tobin J.D., et al. The effect of age on creatinine clearance in men: a cross-sectional and longitudinal study. J Gerontol. 1976;31:155-163.
22. Lonstein J. Adult scoliosis. In Bradford D., Lonstein J., Ogilvie T., et al, editors: Moe’s textbook of scoliosis and other spinal disorders, ed 2, Philadelphia: WB Saunders, 1987.
23. Milledge J.S., Nunn J.F. Criteria of fitness for anaesthesia in patients with chronic obstructive lung disease. BMJ. 1975;3:670-673.
24. Kirkaldy-Willis W.H., Paine K.W., Cauchoix J., et al. Lumbar spinal steno sis. Clin Orthop Relat Res. 1974;99:30-50.
25. Stein M., Koota J.M., Simon M., et al. Pulmonary evaluation of surgical patients. JAMA. 1962;181:765-770.
26. Watters J.M., McClaran J.C. The elderly surgical patient. Wilmore D.W., editor. American College of Surgeons: care of the surgical patient, vol I. New York: Scientific American, 1991.
27. Hart R.A., Prendergast M. Spine surgery for lumbar degenerative disease in the elderly and osteoporotic patient. Instr Course Lect. 2007;56:257-272.
28. Irwin Z.N., Arthur M.A., Mullins R.J., et al. Variations in injury patterns, treatment, and outcome for spinal fracture and paralysis in adult versus geriatric patients. Spine (Phila Pa 1976). 2004;29:796-802.
29. Kallmes D.F., Comstock B.A., Heagerty P.J., et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-579.
30. Buchbinder R., Osborne R.H., Ebeling P.R., et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-568.
31. Weinstein J.N., Lurie J.D., Tosteson T.D., et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg [Am]. 2009;91:1295-1304.
32. Fischgrund J.S., Mackay M., Herkowitz H.N., et al. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976). 1997;22:2807-2812.
33. Kornblum M.B., Fischgrund J.S., Herkowitz H.N., et al. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine (Phila Pa 1976). 2004;29:726-733.
34. Djurasovic M., Glassman S.D., Dimar J.R.2nd, et al. Does fusion status correlate with patient outcomes in lumbar spinal fusion? Spine (Phila Pa 1976). 2011;36:404-409.
35. Zdeblick T.A. A prospective, randomized study of lumbar fusion: preliminary results. Spine (Phila Pa 1976). 1993;18:983-991.
36. Christensen F.B., Hansen E.S., Laursen M., et al. Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral spinal fusion: randomized clinical study with 5-year followup. Spine (Phila Pa 1976). 2002;27:1269-1277.
37. Tisi G.M. Preoperative evaluation of pulmonary function: validity, indications, and benefits. Am Rev Respir Dis. 1979;119:293-310.
38. Benner B., Ehni G. Degenerative lumbar scoliosis. Spine (Phila Pa 1976). 1979;4:548-552.
39. MacDonald J.B. Presentation of acute myocardial infarction in the elderly: a review. Age Ageing. 1984;13:196-200.
40. Smith O.C. Advanced age as a contraindication to operation. Med Rec (New York). 1907;72:642-644.
41. Smith R.W.Jr., Rizek J. Epidemiologic studies of osteoporosis in women of Puerto Rico and southeastern Michigan with special reference to age, race, national origin and to other related or associated findings. Clin Orthop Relat Res. 1966;45:31-48.
42. Zdeblick T.A., Bohlman H.H. Cervical kyphosis and myelopathy. J Bone Joint Surg [Am]. 1989;71:170-182.
43. Kaplan F.S. Prevention and management of osteoporosis. Clin Symp. 1995;47:2-32.
44. Melton L.J.III, Riggs B.L. Impaired bone strength and fracture patterns at different skeletal sites. In: Unthoff H.K., Stahl E., editors. Current concepts of bone fragility. Berlin: Springer-Verlag, 1986.
45. Bracken M.B., Freeman D.H.Jr., Hellenbrand K. Incidence of acute traumatic hospitalized spinal cord injury in the United States, 1970-1977. Am J Epidemiol. 1981;113:615-622.
46. Hanigan W.C., Powell F.C., Elwood P.W., et al. Odontoid fractures in elderly patients. J Neurosurg. 1993;78:32-35.