The extended fast protocol
Overview
Ultrasound has become a permanent part of the evaluation of trauma patients ever since its first use in the emergency department more than 30 years ago.1 First used in Europe in the 1970s, abdominal ultrasound ultimately replaced diagnostic peritoneal lavage during the 1980s.2 Currently, bedside ultrasound is the initial imaging modality of choice for trauma care and is integrated into the Advanced Trauma Life Support protocol developed by the American College of Surgeons.3
“FAST,” an acronym for the focused assessment with sonography in trauma, was first described by Rozycki and Shackford4 in 1996. The basic four-view examination consisting of perihepatic, perisplenic, pelvic, and pericardial views has become the foundation of FAST. The ability to be performed rapidly and safely during resuscitative measures makes it an ideal initial imaging modality in trauma patients. Ultrasound is reliably sensitive in diagnosing free fluid and free air in peritoneum, allowing the rapid recognition of hemoperitoneum and perforated viscera in hypotensive patients and traumatic injuries.5–8 Previous work demonstrated that ultrasound has a higher sensitivity (49%-99%) than standard chest radiography (27%-75%) in the identification of hemothorax or pneumothorax.9–12 The extended FAST (e-FAST) protocol, which includes the assessment of the lung and pleura bilaterally and the subcostal cardiac view, has been developed as point-of-care ultrasound for assessing and treating thoracic pathology in the intensive care environment. Its use has increased considerably over the last decade.13
Ultrasound has been recognized as a powerful diagnostic tool in many clinical settings beyond trauma and has proliferated through a variety of medical specialties. Although pioneered in emergency medicine, e-FAST has now become an important part of critical care evaluation of medical and surgical patients.14,15
Limitations of e-fast
As an operator-dependent test, the learning curve, which is correlated with the results, has been studied. The literature describes variable outcomes related to different operators (radiologists vs. emergency medicine doctors). In addition, e-FAST is limited by technical factors that affect image acquisition, which include, but are not limited to, obesity and deep tissue structures, subcutaneous emphysema, bandages, or barriers to adequate transducer contact. Also, although sensitive for the detection of free fluid or air, ultrasound is not as adept in isolating the associated parenchymal injuries.5,16–19 Once free air or fluid is identified, additional imaging modalities, such as computed tomography (CT), are usually required to further isolate a parenchymal injury.
Application of e-fast in the intensive care unit
Learning to perform the e-FAST examination involves learning how to visualize the heart, diaphragms, liver, spleen, and bladder.20 Interpretation of the e-FAST examination involves learning where free fluid commonly collects adjacent to these structures.
At this time, there is still lack of agreement on recommendations for e-FAST training. It appears that most investigators find that sensitivity and specificity begin to plateau after 25 to 50 examinations.18,21 Current guidelines recommend performing 200 e-FAST examinations.22
Thorax
Key findings
Of note, it has been demonstrated that 30% to 50% of pneumothoraces are missed by chest radiography.23 This diagnostic inaccuracy is partially due to the fact that hemothoraces settle out posteriorly and pneumothoraces anteriorly. In the trauma setting, the e-FAST examination has a sensitivity of 81% to 100% and specificity of 100% for the diagnosis of free fluid in the thoracic cavity.24 About 200 mL of free fluid in the thoracic cavity need to be accumulated to be detected by a plain chest radiography.25 However, ultrasound is much more sensitive and is able to detect as little as 20 mL of free fluid in the same settings.26 The time required for ultrasound versus radiography, in one study, was 1 minute versus 14 minutes, highlighting the potential for rapid diagnosis and intervention.27 Although no similar studies are done for ICU patients, our clinical experiences fully support the time savings associated with bedside ultrasound.
Anterior pneumothorax can often be undetected on a supine portable chest radiograph due to underlying normal lung tissue. However, it can easily be detected with ultrasound as air rises to the highest point within the chest cavity. Therefore, in a supine patient, free intrathoracic air will likely be detected in an anterior examination unless pleural loculations are present. Furthermore, presence of a lung point will be diagnostic of pneumothorax.28
Detection of fluid in the thoracic cavity should promote acute interventions, such as rapid bedside thoracentesis, to determine the gross presence of blood and can facilitate chest tube placement in efforts to resuscitate an unstable patient (Figure 45-1).
Abdomen
Key findings
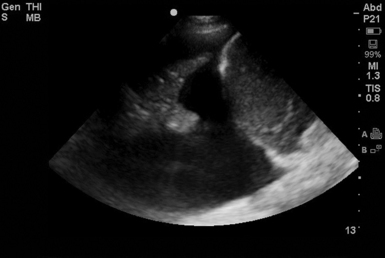
The initial investigations with e-FAST examination focused primarily on the use of bedside ultrasound in the detection of free peritoneal fluid. Sites of evaluation consist of the hepatorenal and splenorenal spaces, paracolic gutters bilaterally, and posterior to the bladder. Although ultrasound is inferior to abdominal CT in the detection of parenchymal injury, it is greater than 95% sensitive and specific for the presence of hemoperitoeum.29,30 It is generally accepted that 250 mL of fluid in the peritoneal cavity is the minimum volume that can be sonographically detected. Of note, large amounts of free peritoneal fluid can be sonographically detectable even by inexperienced operators, whereas small amounts of peritoneal fluid may be missed, especially when located in areas in between structures (e.g., the Morison pouch; Figures 45 E-1 and 45 E-2). To optimize sensitivity to detect the smallest amount of free fluid possible, it is important to obtain images of good quality at multiple intraperitoneal sites.15,31
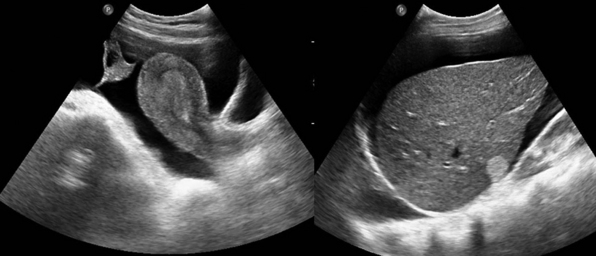
Figure 45 E-1 Large amounts of free peritoneal fluid can be detected even by novice operators. (Courtesy Dr. D. Karakitsos.)
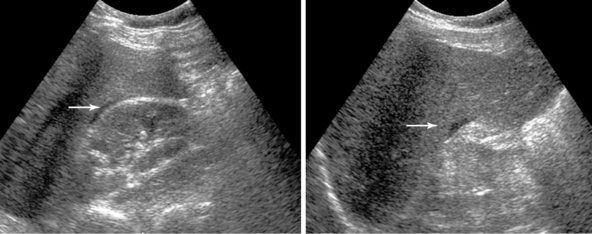
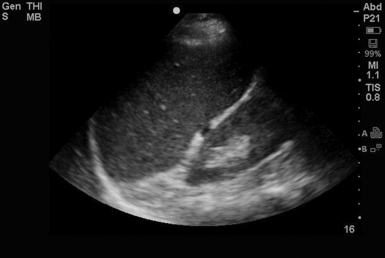
Figure 45 E-2 Small amounts of peritoneal fluid (arrows) may be missed especially when located in areas in between structures, such as the Morison pouch, in this example. (Courtesy Dr. D. Karakitsos.)
In a multicenter prospective trial, Rozycki et al5,7 found that the hepatorenal interface was the most common location for free fluid collection and was associated with significant parenchymal injuries. Although a single hepatorenal view has been advocated by some, a multiple-view e-FAST examination is still recommended because the sensitivity for identification of free fluid is increased and the additional time required is minimal.32–35
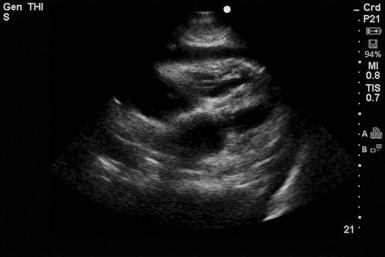
Intraabdominal parenchymal injury is harder to detect when the organ capsule remains intact. The most common sonographic finding associated with splenic rupture is a diffuse pattern of mixed echogenicity within the spleen (Figure 45 E-3). This can be difficult to identify because the stomach overlies the acoustic window of the spleen and can give a hyperechoic signal that appears to be within the spleen.29 The liver has a greater volume than the spleen; thus small intraparenchymal lesions may be missed with the rapid e-FAST technique (Figures 45 E-4 and 45 E-5). Retroperitoneal injuries are also difficult or impossible to detect with ultrasound. e-FAST can yield negative findings or fail to help detect signs of retroperitoneal injury, even in the presence of significant injury, because ultrasound can mainly assess the peritoneal space (see Chapter 41).36,37
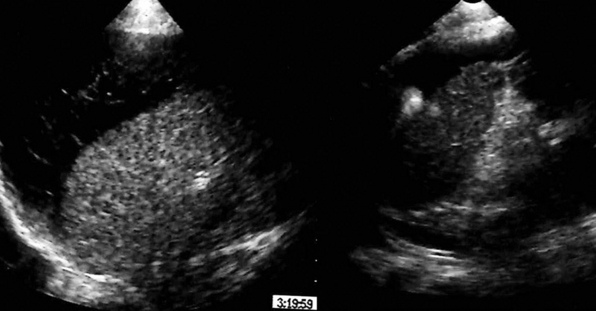
Figure 45 E-3 Visualization of a diffusely heterogeneous splenic parenchyma of mixed echogenicity and perisplenic fluid, whereas the capsule appears not to be intact (splenic rupture). (Courtesy Dr. J. Poularas.)

Figure 45 E-4 Visualization of a diffusely heterogeneous hepatic parenchyma of mixed echogenicity and perihepatic fluid, whereas the Glisson capsule appears not to be intact (hepatic rupture; zoom image). (Courtesy Dr. D. Karakitsos.)
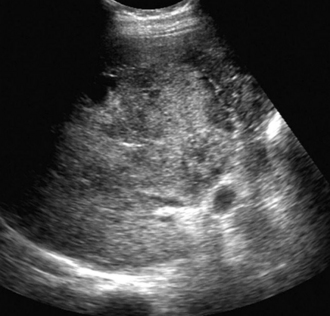
Figure 45 E-5 Visualization of a diffusely heterogeneous hepatic parenchyma of mixed echogenicity and partially intact Glisson capsule (hepatic rupture). (Courtesy Dr. J. Poularas.)
Detection of free fluid in the peritoneal cavity, in a hemodynamically unstable patient, usually necessitates immediate laparotomy. Ultrasound cannot reliably distinguish acute bleeding from simple ascitic fluid or urine because all appear hypoechoic (Figure 45-2). However, ultrasound-guided paracentesis can quickly make this differentiation (Figure 45 E-6). In case conservative management is followed, repeated ultrasound examinations can evaluate possible alterations in the amount of fluid. As blood coagulates, a “hematocrit sign” may be observed as the more echogenic particles of blood precipitate to dependent areas (Figure 45-3).38
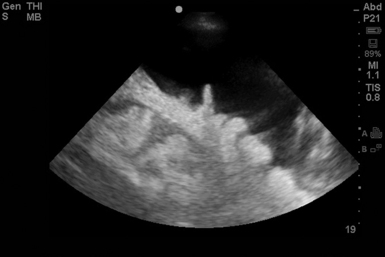
Figure 45-2 Free fluid in the abdominal cavity. Bowel loops can be identified. The fluid can be described as nonechogenic simple fluid.
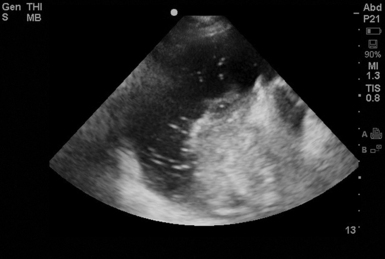
Figure 45-3 The hematocrit sign. As blood coagulates, a “hematocrit sign” may be seen as the more echogenic particles of blood precipitate to dependent areas.
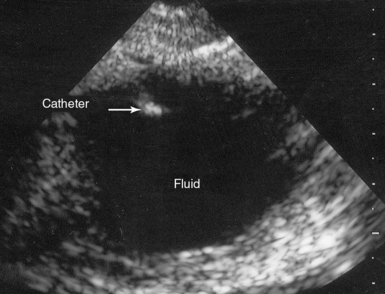
Figure 45 E-6 Transverse view of an ultrasound-guided paracentesis of free peritoneal fluid. (Courtesy Dr. J. Poularas.)
A free-flowing effusion seeks a dependent position in the abdomen by gravitational effect. Free fluid is usually seen in the hepatorenal recess or along the lower edge of the liver and around the lower tip of the liver.39 Placing a patient in the Trendelenburg position improves the sensitivity for detecting free fluid.34 Trendelenburg positioning can be also applied when the pelvic view is indeterminate or difficult to visualize. Overall, the e-FAST examination is 90% sensitive for detecting any amount of intraperitoneal free fluid (Figure 45-4).36
Swirling echoes, strands, fronds, or septations may be visible in exudative collections. Effusions with these findings are described as being heterogeneously echogenic. Echogenic effusions with septations often indicate infectious peritonitis or empyema.40,41 Ultrasound may be superior to a CT scan in revealing septations.
Bowel injuries in the acute settings are notoriously difficult to diagnose, even with CT. Ultrasound is inaccurate for detecting bowel injuries, and the most common associated finding is free fluid.42 Abdominal ultrasound is useful in detection of free peritoneal air during emergent assessment. Similar to lung sliding, “gut sliding” of the intact visceral and parietal peritoneal layers has been described. The absence of gut sliding with an associated horizontal air pattern arising from the peritoneal line (similar to A-lines) can be highly indicative of free intraabdominal air.43 The scanner should look for a splanchnogram sign indicating that the major abdominal organs (such as liver and spleen) are visible. The absence of the splanchnogram sign coupled with the absence of sliding gut predicted pneumoperitoneum with 100% sensitivity (Figure 45-5).43
Cardiac
Key findings
As part of the e-FAST, a subcostal (subxiphoid) cardiac view is obtained. Work done by Plummer44 demonstrated the value of bedside ultrasound in the evaluation of cardiac injuries. In this study, the ultrasound group had a significantly faster rate of diagnosis and disposition and higher survival rates (100% vs. 57%).44 Although e-FAST visualization of the heart consists mainly of a subcostal view, ideally, imaging in multiple views (using several windows) provides the most accurate detection of pericardial effusion.
Cardiac function can be quickly estimated, and pericardial fluid can be identified (Figure 45-6). Signs of pericardial tamponade are described in detail in previous chapters. However, in a hemodynamically unstable patient, significant fluid should be drained via ultrasound guidance. From the subxiphoid view, the IVC can be visualized adjacent to the right atrium, where it can be analyzed (diameter and collapse). IVC analysis can be used as a measure of volume responsiveness (detailed in previous chapters).31,32
Pearls and highlights
• e-FAST is a rapid tool for detection of cardiac, intrathoracic, and intraabdominal pathology.
• Detection of free fluid or air on e-FAST should prompt immediate further investigation or intervention.
• Ultrasound can be used to follow patients managed conservatively or to guide diagnostic procedures.
References
1. Bartrum, RJ. Introduction. In: Winsberg F, Cooperberg PL, eds. Real-time ultrasonography. New York: Churchill Livingstone; 1982:1–5.
2. JA, Pilbrow, WJ, Ultrasound in abdominal trauma: an alternative to peritoneal lavage. Arch Emerg Me. 1988; 5:26–33.
3. MR, The Advanced Trauma Life Support course: a history of its development and review of related literature. Postgrad Med . 2005; 81:87–91.
4. Rozycki, GS, Shackford, SR. Ultrasound, what every trauma surgeon should know. J Trauma. 1996; 40:1–4.
5. Rozycki, GS, Ballard, RB, Feliciano, DV, et al, Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540. patients. Ann Sur. 1998; 228:557–567.
6. Wherrett, LJ, Boulanger, BR, McLellan, BA, et al, Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Traum. 1996; 41:815–820.
7. Rozycki, GS, Feliciano, DV, Ochsner, MG, et al, The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Traum. 1999; 46:543–552.
8. Plummer, D, Brunette, D, Asinger, R, Ruiz, E. Emergency department echocardiography improves outcome in penetrating cardiac injury. Ann Emerg Med. 1992; 21:709–712.
9. Dulchavsky, SA, Schwarz, KL, Kirkpatrick, AW, et al. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J Trauma. 2001; 50:201–205.
10. Kirkpatrick, AW, Sirois, M, Laupland, KB, et al, Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Traum. 2004; 57:288–295.
11. Ma, OJ, Mateer, JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997; 29:312–316.
12. Sisley, AC, Rozycki, GS, Ballard, RB, Namias, N, et al. Rapid detection of traumatic effusion using surgeon-performed ultrasonography. J Trauma. 1998; 44:291–297.
13. Moscati, R, Reardon, R, Clinical application of the FAST examJehle D, Heller M, eds.. Ultrasonography in trauma: the FAST: the FAST. American College of Emergency Physicians: Dallas, 2003; 39–60.
14. Ma, OJ, Kefer, MP, Mateer, JR, Thoma, B. Evaluation of hemoperitoneum using a single- vs multiple-view ultrasonographic examination. Acad Emerg Med. 1995; 2:581–586.
15. Von Kuenssberg Jehle, D, Stiller, G, Wagner, D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003; 21:476–478.
16. Plummer, D. Principles of emergency ultrasound and echocardiography. Ann Emerg Med. 1989; 18:1291–1297.
17. Jehle, D, Davis, E, Evans, T, et al. Emergency department sonography by emergency physicians. Am J Emerg Med. 1989; 7:605–611.
18. Ma, OJ, Mateer, JR, Ogata, M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995; 38:879–885.
19. Rozycki, GS, Ochsner, MG, Schmidt, JA, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995; 39:492–500.
20. Gracias, VH, Frankel, HL, Gupta, R, et al, Defining the learning curve for the Focused Abdominal Sonogram for Trauma (FAST) examination: implications for credentialing. Am Sur. 2001; 67:364–368.
21. Thomas, B, Falcone, RE, Vasquez, D, et al, Ultrasound evaluation of blunt abdominal trauma: program implementation, initial experience, and learning curve. J Traum. 1997; 42:384–388. [discussion 388-390].
22. Scalea, TM, Rodriguez, A, Chiu, WC, et al, Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Traum. 1999; 46:466–472.
23. Ding, W, Shen, Y, Yang, J, et al, Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Ches. 2011; 140:859–866.
24. Sartori, S, Tombesi, P, Trevisani, L, et al. Accuracy of thoracic sonography in detection of pneumothorax after sonographically guided comparison with chest radioigraphy. AJR Am J Roentgenol. 2007; 188:37–41.
25. Juhl, J. Diseases of the pleura, mediastinum, and diaphragm. In: Juhl J, Crummy A, eds. Essentials of radiologic imaging. Philadelphia: JB Lippincott; 1993:1026.
26. Rothlin, MA, Naf, R, Amgwerd, M, et al. Ultrasound in blunt abdominal and thoracic trauma. J Trauma. 1993; 34:488–495.
27. Sisley, AC, Rozycki, GS, Ballard, RB, et al. Rapid detection of traumatic effusion using surgeon-performed ultrasonography. J Trauma. 1998; 44:291–297.
28. Lichtenstein, DA, Menu, Y, A bedside ultrasound sign ruling out pneumothorax in the critically ill: lung sliding. Ches. 1995; 108:1345–1348.
29. Richards, JR, McGahan, JP, Jones, CD, et al. Ultrasound detection of blunt splenic injury. Injury. 2001; 32:95–103.
30. Zhou, J, Huang, J, Wu, H, et al. Screening ultrasonography of 2,204 patients with blunt abdominal trauma in the Wenchuan earthquake. J Trauma Acute Care Surg. 2012; 73:890–894.
31. Tiling, T, Bouillon, B, Schmid, A. Ultrasound in blunt abdomino-thoracic trauma. In: Border J, Allgoewer M, Hansen S, eds. Blunt multiple trauma: comprehensive pathophysiology and care. New York: Marcel Dekker; 1990:415–433.
32. Goldberg, BB, Goodman, GA, Clearfield, HR. Evaluation of ascites by ultrasound. Radiology. 1970; 96:15–22.
33. Paajanen, H, Lahti, P, Nordback, I. Sensitivity of transabdominal ultrasonography in detection of intraperitoneal fluid in humans. Eur Radiol. 1999; 9:1423–1425.
34. Abrams, BJ, Sukumvanich, P, Seibel, R, et al, Ultrasound for the detection of intraperitonealfluid: the role of Trendelenburg positioning. Am J Emerg Me. 1999; 17:117–120.
35. Huang, MS, Liu, M, Wu, JK, et al, Ultrasonography for the evaluation of hemoperitoneum during resuscitation: a simple scoring system. J Traum. 1994; 36:173–177.
36. Friese, RS, Malekzadeh, S, Shafi, S, et al. Abdominal ultrasound is an unreliable modality for the detection of hemoperitoneum in patients with pelvic fracture. J Trauma. 2007; 63:97–102.
37. Jurkovich, GJ, Bulger, EM. Duodenum and pancreas. In: Moore EE, Feliciano DV, Mattox KL, eds. Trauma. 5th ed. New York: McGraw-Hill; 2004:709–733.
38. Mayo, PH, Doelken, P. Pleural ultrasonography. Clin Chest Med. 2006; 27:215–227.
39. Rozycki, GS, Ochsner, MG, Feliciano, DV, et al, Early detection of hemoperitoneum by ultrasound examination of the right upper quadrant: a multicenter study. J Traum. 1998; 45:878–883.
40. Yang, PC, Luh, KT, Chang, DB, et al, Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. AJR Am J Roentgeno. 1992; 159:29–33.
41. Chian, CF, Su, WL, Soh, LH, et al. Echogenic swirling pattern as a predictor of malignant pleural effusions in patients with malignancies. Chest. 2004; 126:129–134.
42. Brown, MA, Casola, G, Sirlin, CB, et al, Blunt abdominal trauma: screening us in 2,693 patients. Radiolog. 2001; 218:352–358.
43. Lichtenstein, DA. General ultrasound in the critically ill. Berlin: Springer; 2007.
44. Plummer, D, Brunette, D, Asinger, R, et al. Emergency department echocardiography improves outcomes in penetrating cardiac injury. Ann Emerg Med. 1992; 21:709–712.