Chapter 16 The Epidemiology of Peripheral Artery Disease
Peripheral artery disease (PAD) is generally defined as partial or complete obstruction of one or more peripheral arteries due to atherosclerosis. Although the term PAD is sometimes inclusive of all peripheral arteries, in this chapter PAD refers to atherosclerotic occlusive disease of the lower extremities. Peripheral artery disease is associated with many of the same risk factors as atherosclerotic cardiovascular and cerebrovascular diseases, and is very common among the elderly. Peripheral artery disease that exhibits typical symptomatology, usually in the form of leg pain brought about by walking, has been conservatively estimated to reduce quality of life in at least 2 million Americans, and in some cases leads to a need for surgical revascularization or amputation.1 Six million more Americans have measurable asymptomatic disease or disease with atypical symptoms.2 Both symptomatic and asymptomatic PAD have been shown to be associated with a sharply elevated risk of mortality due to coronary and cerebrovascular disease.3
Symptoms and Measures of Peripheral Artery Disease in Epidemiology
Early studies of PAD focused primarily on claudication as the chief symptomatic manifestation of PAD. A number of patient questionnaires have been developed to uniformly identify claudication and distinguish it from other types of leg pain. The first of these was the Rose questionnaire, also referred to as the World Health Organization questionnaire.4 The San Diego Claudication Questionnaire (SDCQ) is a modification of the Rose questionnaire that additionally captures information on the laterality of symptoms.5 Recently we completed an evidence-based shortened revision of the SDCQ that is shown in Table 16-1.
Table 16-1 San Diego Claudication Questionnaire (Brief Version)
| Circle Answer | |
| 1. Do you get pain or discomfort in either leg on walking? (If no, stop.) | Right leg Yes No Left leg Yes No |
| 2. Does this pain ever begin when you are standing still or sitting? | Right leg Yes No Left leg Yes No |
| 3. Does this pain include your calf/calves? | Right leg Yes No Left leg Yes No |
| 4. Do you get it when you walk at an ordinary pace on the level? | Right leg Yes No Left leg Yes No |
| 5. What do you do if you get it when you are walking? | Right leg Stop or slow down Continue on Left leg Stop or slow down Continue on |
| 6. What happens to it if you stand still? | Right leg Lessened or relieved Unchanged Left leg Lessened or relieved Unchanged |
Determine pain category separately for each leg as follows:
1. No pain: 1 = no
2. Pain at rest: 1 = yes and 2 = yes
3. Non-calf: 1 = yes and 2 = no and 3 = no
4. Classic: 1 = yes and 2 = no and 3 = yes and 4 = yes and 5 = stop or slow down and 6 = lessened or relieved
5. Atypical calf: 1 = yes and 2 = no and 3 = yes and not classic
Ankle-Brachial Index
Although intermittent claudication is an important manifestation of PAD, it is not pathognomonic. Atherosclerosis may have been developing for many years before claudication begins, and the extent to which it occurs is influenced by factors other than disease per se, such as the patient’s level of activity.6 Furthermore, the definitional distinctions used to separate claudication from other leg pain make claudication more specific to arterial disease but less sensitive to other types of pain that may in some cases be related to arterial disease. Spinal stenosis can cause leg pain similar to claudication during exercise.
For these reasons, another method of diagnosing PAD was needed. Low blood pressure at the ankle was proposed as a test for PAD as early as 19507 and led to development of a simple measure called the ankle-brachial index (ABI). The ABI is the ratio of the systolic blood pressure at the ankle to that in the arm. An abnormally low ABI is indicative of atherosclerosis of the lower extremities. The ABI has been shown to have good receiver operating curve characteristics as a test for PAD. Although there is no definitive cut point above which disease is always absent and below which disease is always present, an ABI of 0.9 or less is commonly used in both clinical practice and epidemiological research to diagnose PAD. The ABI is also sometimes referred to as the ankle-brachial pressure index (ABPI)8 and the ankle-arm index (AAI).9
As a test for ABI-based PAD, claudication has been shown to have very high specificity but very low sensitivity. For example, in the Rotterdam Study, 99.4% of subjects with ABI 0.9 or greater did not have claudication, but only 6.3% of subjects with ABI of less than 0.9 had claudication.10 In a study of elderly women in the United States, the percentages were 93.3% and 18.3%, respectively.6 Peripheral artery disease based on ABI criteria is much more common than claudication in the general population, and large numbers of patients without claudication can be shown to have either atypical or no symptoms in the presence of PAD based on ABI.
To validate the ABI and the huge burden of previously unrecognized asymptomatic disease it implied, early studies compared the ABI-based diagnosis with angiography, which was considered the gold standard for visualizing atherosclerosis in the legs. Two such studies often cited reported the sensitivity and specificity of the ABI in the 97% to 100% range.11,12 However, because angiography presents some risk to patients, it was not ethical to perform angiography on patients not suspected to have PAD, so these studies involved comparisons of patients with angiographically confirmed PAD with young healthy patients assumed not to have PAD. The sensitivities and specificities calculated are therefore based on the ability of the ABI to discriminate between extremes of disease and wellness. If measured among patients seen in routine clinical practice or the population in general, the specificity of the ABI remains in the 97% + range, but the sensitivity is somewhat less—closer to 80%13—in part due to some PAD patients with stiff peripheral arteries and false-negative ABIs.14
The ABI has been demonstrated to have strong associations with cardiovascular disease risk factors and disease outcomes. In the Cardiovascular Health Study (CHS) cohort, a dose-response relationship was demonstrated between ABI and cardiovascular disease risk factors, as well as both clinical and subclinical cardiovascular disease.15 In a study in Edinburgh, asymptomatic patients with an ABI of less than 0.9 were shown to have a higher risk of developing claudication and higher mortality.16 In a clinical study, patients with an ABI of less than 0.9 who did not have exertional leg pain were shown to have poorer lower-extremity functioning even after adjustment for traditional risk factors and comorbidities.17 The ABI correlates with ability to exercise as measured on an accelerometer,18 and an ABI of less than 0.6 is related to development of walking impairment.19 Thus, even aside from its association with claudication, the ABI is related to the types of functional outcomes, risk factors, and associated diseases that one would expect of a measure of PAD. The ABI has also been shown to have high intra- and inter-rater reliability.20
In practice, the ABI is measured using a blood pressure cuff, a standard sphygmomanometer, and a Doppler instrument to detect pulses. Pressure measurements are made with the patient at rest in a supine position for 5 minutes prior to measurement. Ankle pressure is measured in both legs at the dorsalis pedis and posterior tibial arteries. The higher pressure measurement in each ankle has traditionally been used as the numerator of the ABI for that ankle. Using the lower or average pressure can substantially change estimates of PAD prevalence; one study reported 47% prevalence based on the higher pressure versus 59% based on the lower.20 Results of two recent studies support the use of the average of dorsalis pedis and posterior tibial pressures as the ankle pressure for each leg, based on superior reproducibility in repeated tests and closer statistical association with leg function.20,21 However, the relative predictive value of the higher versus the average (or perhaps the lower) of the two ankle pressures for clinical events has not yet been evaluated. Practice also differs as to the brachial pressure used as the denominator of the ABI; the same brachial pressure is usually used for both left and right ABIs in the same patient, but that pressure may be the right arm, the average of both arms, or the highest of both arms. A recent study supports use of the average of the left and right arms, based on superior reproducibility,21 but another study shows a strong correlation between PAD and subclavian stenosis, suggesting the highest arm pressure should be used in the ABI calculation.22 Another issue is that the first arm pressure measured is typically higher because of the “white coat” effect, and a repeat of the first arm pressure after the other pressures are complete will often give a more accurate reading. Based on the numerators and denominators described, separate ABIs are calculated for the left and right legs of each subject. In epidemiological analyses, the unit of analysis is either the leg, with appropriate statistical adjustments for intrasubject correlation, or the subject, with disease status classified based on the “worst” limb (i.e., the limb with the lowest ABI).
The ABI has several limitations as a measure of PAD. Occlusive disease distal to the ankle is not detected by the ABI; other measures, such as pressure ratios using pressures measured in the toe, are required for detecting such distal disease. The ABI is also sensitive to the height of the patient, with taller patients having slightly higher ABIs; it is unlikely these differences are related to real differences in PAD.23,24 Similarly, it has been noted in several studies that the ABI of the left leg tends to be slightly lower on average than the ABI of the right leg.23,24 Recent data also document that ABIs in normal subjects, on average, are slightly lower in women and African Americans.25
Arterial calcification (medial calcinosis) can make the arteries of the ankle incompressible and lead to artificially high ABI values. This is particularly common in patients with diabetes.26,27 Ankle-brachial index values above 1.5 are often excluded in epidemiological analyses and should be viewed with suspicion clinically.6,15,28–30 In two large population-based studies in the United States, the proportion of patients with such elevated values was around 0.5%.15,30 Some investigators use the more conservative cut point of 1.3. New evidence suggests 1.4 may be a good compromise.31,32
Incidence and Prevalence of Peripheral Artery Disease
Although uncommon among younger people, the prevalence of PAD rises sharply with age to include a substantial proportion of the elderly population. Figure 16-1 shows some ABI-based estimates of PAD prevalence by age from six large studies.10,15,33–36 In four of the studies, the standard ABI of less than 0.9 criterion was used; in the Limburg Study, PAD was diagnosed based on two ABI measurements of less than 0.95,35 whereas in the Rancho Bernardo Study, a combination of a conservative ABI cut point of 0.8 and other noninvasive tests was used.33 Although estimates vary, prevalence appears to be well under 5% before age 50, around 10% by age 65 and in excess of 25% in patients 80 years of age or older. All studies show this stronger-than-linear relationship of prevalence to age, although there is some variability in the age at which prevalence begins to increase most dramatically.
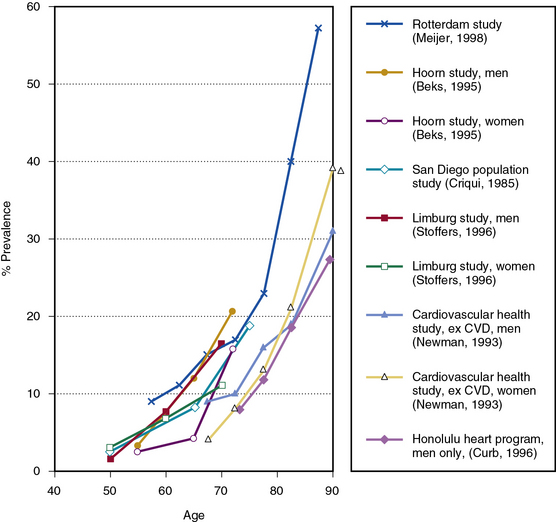
Figure 16-1 Peripheral artery disease (PAD) prevalence.
Estimates based on ankle-brachial index (ABI) from six large studies.
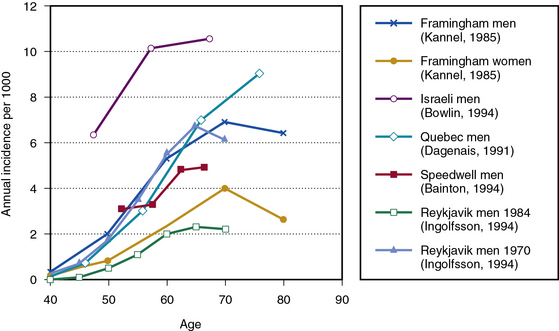
Estimates of PAD incidence are reported somewhat less frequently in the literature, with more data based on claudication incidence than on ABI. With respect to claudication, data from the Framingham Study show claudication in men rising from less than 0.4 per 1000 per year in men aged 35 to 45 years to more than 6 per 1000 per year in men aged 65 years and older.37 Incidence among women ranged from 40% to 60% lower by age, although estimates in men and women were similar by age 65 to 74. In a group of Israeli men, incidence of claudication ranged from 6.3 per 1000 per year at ages 40 to 49 to 10.5 per 1000 at age 60 and greater.1 In a study of 4570 men from Quebec, claudication incidence rose from 0.7 per 1000 per year at ages 35 to 44, to 3 per 1000 per year at ages 45 to 54, 7 per 1000 per year at ages 55 to 63, and 9 per 1000 at age 65 and greater.38 In the Speedwell Study that followed English men aged 45 to 63 years for 10 years, claudication incidence per 1000 per year ranged from 3.1 in the youngest to 4.9 in the oldest age group, based on age at baseline examination.39 A higher incidence of 15.5 per 1000 per year was reported among men and women aged 55 to 74 in the Edinburgh Artery Study; however, this study did not apply strict Rose criteria for probable claudication.40
In the Reykjavik Study, Ingolfsson et al. used Poisson regression techniques to conclude that intermittent claudication rates among Icelandic men dropped significantly between 1968 and 1986. Among 50-year-old men, their estimate of the rate of claudication dropped from 1.7 per 1000 per year in 1970 to 0.6 per 1000 per year in 1984, whereas in 70-year olds, the rate of claudication dropped from 6.0 to 2.0.41 The authors attributed this to decreased smoking and cholesterol levels. The design and duration of this study were uniquely suited to estimating long-term trends in disease incidence; comparable studies for other populations are unavailable. The potential for trends of this magnitude should be considered in reviewing results of other studies. Figure 16-2 shows incidence rates by age for various studies identifying PAD based on claudication.1,37–39,41
There are very few ABI-based studies of PAD incidence, given the time and resources required to periodically retest study subjects for incident disease. In the Limburg PAOD Study, incidence rates for PAD were based on two ABI measurements of less than 0.95. Among men, annual incidence was 1.7 per 1000 at ages 40 to 54; 1.5 per 1000 at ages 55 to 64; and 17.8 per 1000 at ages 65 and greater. Annual incidence in women was higher: 5.9, 9.1, and 22.9 per 1000, respectively, for the same age groups.42
Claudication incidence and prevalence have usually been found to be higher in men than women. For example, in the Framingham Study, annual claudication incidence for all ages combined was 7.1 per 1000 in men versus 3.6 per 1000 in women, for a male-to-female ratio of 1.97.37 In the Framingham Offspring Study, claudication prevalence was 1.9% in men versus 0.8% in women (ratio = 2.38), whereas in the Rotterdam Study it was 2.2% in men versus 1.2% in women (ratio = 1.83).10,30 However, the Edinburgh Artery Study and the Limburg PAOD Study found much lower male-to-female ratios of claudication prevalence of 1.11 and 1.2, respectively.23,35
The case for an excess of disease among males is even weaker for PAD diagnosed based on ABI. This is true even in those studies finding a clear male excess with respect to claudication. For example, in the Framingham Offspring Study mentioned earlier, PAD based on ABI was found in 3.9% of men and 3.3% of women, for a ratio of 1.18.30 In the Rotterdam Study, ABI-based PAD was actually lower in men than in women, with prevalences of 16.9% and 20.5% for a ratio of 0.8210. The Limburg PAOD Study, which reported a low male-to-female ratio for claudication, reported a similarly low ratio of 1.1 for ABI-based PAD.35 A population-based study from Southern Italy found prevalences of PAD based on ABI of less than 0.9 to be very similar in men and women, with male to female ratios by age of .89 to .99.43 In the CHS, ABI of less than 0.9 was somewhat more prevalent in men than women (13.8% vs. 11.4%; ratio = 1.21), but the association of disease with sex was not significant after adjustment for age and cardiovascular disease status.15 In the Atherosclerosis Risk in Communities (ARIC) Study, PAD prevalence based on ABI was actually lower in men than women among both African Americans (3.3% vs. 4.0%) and whites (2.3% vs. 3.3%).44
The greater male excess observed for symptomatic versus ABI-diagnosed disease may be related to severity of disease. A prevalence study in Southern California found that the excess of disease among males increased with severity of PAD.33 A report from the Multi-Ethnic Study of Atherosclerosis (MESA) showed PAD prevalence (ABI of less than 0.90) was the same in men and women (3.7%), but borderline values of ABI (0.90-0.99) were much higher in women (10.6% vs. 4.3%).45
Peripheral Artery Disease Risk Factors
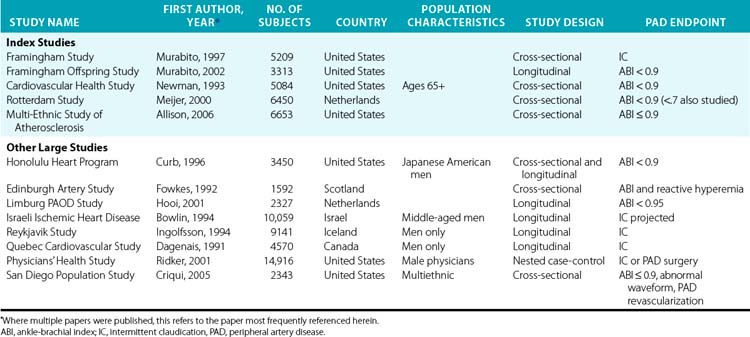
The following discussion of risk factors focuses on the results from five large epidemiological studies referred to as index studies (Table 16-2). These studies each had over 3000 subjects drawn from the general population and included both men and women. The studies are similar enough in their selection and manner of measuring risk factors and in their statistical analyses to allow reasonable comparisons for most of the common risk factors. Although the discussion draws on data from many other studies (see Table 16-2 for a partial list), data are presented from these five studies across all the conventional cardiovascular disease risk factors to provide some consistency and comparability for the reader, and as a check against potential biases that might be introduced by selecting all the studies to present for each risk factor in a more ad hoc fashion.
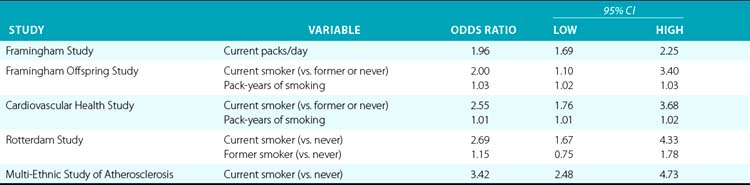
Smoking
Smoking is one of the strongest risk factors for PAD in virtually all studies. Studies vary as to their measurement of smoking, often combining a categorical assessment of smoking status (current, past, or never) with some measure of current or historical volume of smoking; these multiple approaches to measurement make comparisons difficult. However, even with some type of additional adjustment for volume of smoking, current smoking versus nonsmoking has been shown to at least double the odds of PAD in most studies, with some estimates as high as a four times greater risk among smokers than others. Among the index studies, current smoking (vs. never or former/never) resulted in 2.0 to 3.4 times higher odds of PAD in the three studies using such categorization; however, in two of these studies, the models also included pack-years of smoking as a significant variable. The Rotterdam study included only current packs/day, showing a doubling of the odds of PAD for each pack a day smoked (Table 16-3). All the large population-based studies reviewed found a significant independent association between PAD and smoking.
Cessation of smoking among patients with claudication has been shown to improve various functional and physiological measures related to PAD, as well as reducing mortality.46–48 However, because symptomatic PAD patients have long been advised to quit smoking, it is possible that observational comparisons of patients who quit smoking with those who do not are confounded by other differences in compliance with medical advice between the two groups. Randomized trials of this question would raise ethical issues, but substantial bias is unlikely, given the large effect size for cigarette smoking.
Aside from the large increase in risk associated with it, smoking is the traditional risk factor for which the best case can be made for a more important role in PAD than in other atherosclerotic diseases. In a comparison of risk factors conducted in the same large cohort, Fowkes et al. found smoking to be associated with a significantly higher relative risk for PAD compared to other cardiovascular diseases. Smoking was the only traditional cardiovascular disease risk factor for which the odds ratio differed significantly between PAD and other cardiovascular diseases.49
Diabetes
Diabetes is strongly associated with an elevated risk of PAD, although the evidence for an independent role in multivariable analysis is not entirely consistent. Four of the five index studies found diabetes, dichotomized based on different criteria, to be associated with PAD after multivariable adjustment, with odds ratios ranging from 1.89 to 4.05.9,15,50,51 The Framingham Offspring Study found such an association on an age- and sex-adjusted basis, but not in multivariable models.30
Among other large population-based studies, multivariable logistic regression models have often shown a relationship to diabetes as a categorical variable,1,34,36,42,52 or various blood sugar measures as linear variables.39 Other null findings for diabetes or blood sugar measures were seen in the Edinburgh Artery Study49 and the Reykjavik Study.41
More severe and/or long-standing diabetes appears to be more strongly related to PAD. In the Hoorn Study, it was shown that known diabetes was associated with PAD in multivariable analysis, whereas newly diagnosed diabetes was only of borderline significance, and impaired glucose tolerance was not associated with PAD.34 In that study, after excluding known diabetics, none of the common glycemic indices that were tested were significantly associated with PAD based on ABI, although significant associations were observed when the PAD criteria were broadened to include patients with additional criteria. Studies conducted in patients with diabetes have shown that duration of diabetes and use of insulin are associated with PAD.53–55
Outcomes of PAD in diabetic patients have been shown to be worse. In one study, diabetic patients with PAD were five times more likely to have an amputation than other PAD patients; they also had more than three times the odds of mortality.56 There is also some evidence to support a somewhat different anatomical distribution of disease, with more disease in arteries distal to the knee in diabetic than nondiabetic persons.56,57
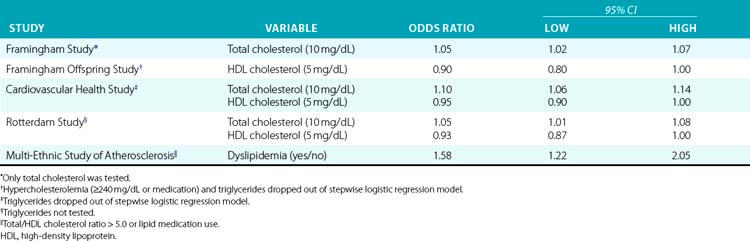
Lipids
As is the case in cardiovascular disease epidemiology, the challenge of defining the roles of various lipid fractions in PAD lies in identifying the strongest independent risk factors from among multiple correlated measures. In recent studies, recognition that the ratio of total cholesterol to high-density lipoprotein (HDL) cholesterol is the best lipid measure of risk,58 along with increasing use of medication, has led to analyses that employ both these variables in the same model52 or combine the ratio with medication use in a single variable (e.g., “dyslipidemia”).51 Results from the index studies appear in Table 16-4.
Total cholesterol was the first lipid measure examined as a potential risk factor for PAD and has been the most widely studied. Total cholesterol was examined as a potential risk factor in four of the index studies, and was significantly associated with PAD in multivariable analysis in three. In the remaining study, total cholesterol was significant in univariate analysis but dropped out of multivariable models that considered other lipid measures.30 Similarly, in other studies total cholesterol has usually been found to be associated with PAD,1,36,41,49 with occasional null findings in multivariable analyses where other lipid measures are considered.39,59 One of the few null findings for total cholesterol as the sole lipid measure was an analysis of the Quebec Cardiovascular Study cohort.38
High-density lipoprotein cholesterol (HDL-C) has been shown to be protective against PAD in most studies where it was evaluated, usually in models that also considered total cholesterol. High-density lipoprotein cholesterol was included among potential risk factors in three of the five index studies and in the TC/HDL-C ratio in a fourth, and was significantly associated with PAD in multivariable analysis in all four. In two studies, both HDL-C and total cholesterol were significant in multivariable analysis, whereas in one study HDL-C but not total cholesterol was significant. Other studies have also shown a protective effect of HDL-C.36,59
Bowlin et al. found that non-HDL cholesterol (total cholesterol minus HDL cholesterol) was significantly associated with incident claudication in a large cohort of Israeli men. Neither total cholesterol nor HDL cholesterol were significantly associated with disease in models that included non-HDL cholesterol.1 In a comparison of incident cases of claudication with healthy controls in the Physician’s Health Study, Ridker et al. found that the ratio of total to HDL cholesterol was the lipid measure most strongly associated with disease, with patients in the highest quartile having 3.9 times the claudication risk of patients in the lowest quartile. Screening for other lipid fractions was judged to have little clinical usefulness beyond measurement of this ratio.60
Evidence for high triglycerides as an independent risk factor for PAD is fragmentary. Early case-control studies showed a very consistent relationship between triglycerides and PAD, suggesting a uniquely strong relationship with PAD, but large population-based cohort studies employing multivariable modeling later called this into question.49,61 Among the index studies, only two included triglycerides among the potential risk factors evaluated. In both cases, triglycerides were significant in univariate analysis but dropped out of multivariable models based on stepwise logistic regression.15,30 Similarly, in the Edinburgh Artery Study cohort and in a large study of geriatric patients in the United States, triglycerides were not significantly associated with PAD after adjustment for other lipid meaures.49,59 However, other studies have shown triglycerides to be significantly and independently associated with PAD in multivariable analysis.39,53,62 There is also some evidence suggesting that elevated triglycerides may have a special role in disease progression or more severe PAD.49,63
In summary, although total cholesterol, HDL-C, and triglycerides all appear to be associated with PAD on a univariate basis, in multivariable analysis triglycerides frequently drop out as an independent risk factor. Although it has been the most extensively studied, it is not clear that total cholesterol is the strongest independent risk factor for PAD; in one comparison of PAD patients with healthy controls, it was found that mean total cholesterol did not differ significantly, whereas triglycerides, very low-density lipoprotein (VLDL) cholesterol, low-density lipoprotein (LDL) cholesterol, HDL cholesterol, and the total-to-HDL cholesterol ratio all did.64
Hypertension and Blood Pressure
The association of hypertension with PAD has been demonstrated in most studies in which blood pressure was studied. All five of the index studies reported a significant association between hypertension as a categorical variable and PAD. The lowest reported odds ratio was 1.32 as reported in the Rotterdam Study; this is somewhat understated relative to the others, since it was based on a model that included both a categorical hypertension variable and an adjustment for systolic blood pressure level that was also significant.9 Other than this, odds ratios for hypertension ranged from 1.50 to 2.20. Most other large population-based studies have also found a significant independent association of hypertension or systolic blood pressures with PAD.38,39,42,49,52
Where both systolic and diastolic pressures were considered, systolic pressure was usually found to be associated with PAD, whereas diastolic pressure was not significantly associated9,15,65 or had a nonlinear relationship with PAD.36 Two large studies found no relationship of blood pressure with PAD. In the Israeli Ischemic Heart Disease Project cohort, neither systolic nor diastolic blood pressure was associated with claudication,1 whereas in the Reykjavik Study, systolic and diastolic blood pressures were significantly associated with claudication in cross-sectional but not longitudinal models.41 It is interesting to note that both of these studies appear to have used blood pressure as a linear term in their models. Most other recent large studies have used a categorization of subjects into normotensive and hypertensive groups based on systolic and diastolic pressures as well as hypertension medication use.
Both of the null findings also come from studies in which claudication was the outcome of interest. It has been speculated that elevated central perfusion pressure as indicated by (axial) blood pressure will sometimes delay onset of claudication by increasing blood pressure in the lower extremities, which—if true—would obscure the relationship of hypertension with underlying disease processes.66 However, randomized trials of blood pressure lowering in PAD patients generally do not report worsened claudication.
Although the relative risks associated with hypertension are modest in some studies, its high prevalence, particularly among older patients, make it a significant contributor to the total burden of PAD in the population. For example, in one large study from the Netherlands, the odds ratio for hypertension was 1.32, but its attributable risk (a measure of the proportion of PAD due to hypertension in the population) was 17.0%, second only to current smoking in this group.9 In the Framingham Study, 30% of the risk of claudication in the population was attributable to blood pressure in excess of 160/100.50
Obesity
To date, the preponderance of evidence fails to support a consistent independent positive association between obesity and PAD. In one of the few large studies with a positive finding, Bowlin et al. estimated an odds ratio of 1.24 (95% confidence interval [CI], 1.05-1.46) for incident claudication related to a 5.0 kg/m2 difference in body mass index (BMI) in a study of 10,059 Israeli men.1
Three of the index studies and a number of other large population-based studies have failed to find a significant association between obesity and PAD or claudication after multivariable adjustment.9,30,41,42,51,59 There have also been many studies, including the other two index studies, in which higher relative weight or BMI was actually shown to be protective against PAD. In the Framingham Study, claudication was significantly inversely related to relative weight in men in multivariable analysis, and appeared to have a “U-shaped” nonlinear relationship with relative weight in women.37 In an analysis from the Edinburgh Artery Study, BMI was significantly associated with less disease in preliminary multivariable analysis, although BMI was excluded from the paper’s final multivariable model because it “suggested a counterintuitive effect.”49 The CHS found higher BMI to be significantly protective against PAD after multivariable adjustment in a large sample of Medicare beneficiaries.15 Body mass index was significantly protective against PAD (defined based on a combination of ABI, Doppler flow curves, and history of surgery) in the Hoorn Study.34 Similarly, the odds of PAD among subjects in the highest quintile of BMI compared with the lowest quintile were found to be significantly reduced in a cross-sectional analysis of elderly Japanese American men.36 Subjects with higher BMI were again shown to be at significantly lower risk of PAD in a study of Taiwanese subjects with diabetes.67 Finally, the multiethnic San Diego Population Study (SDPS) reported a significant inverse association for BMI and PAD.52
Obesity has been implicated in the etiology of other risk factors for PAD, such as hypertension, type II diabetes, and dyslipidemia. In epidemiology, adjusting for factors that are on the causal pathway between a risk factor and disease is known to attenuate the observed strength of that risk factor. Therefore, estimates of risks related to obesity in multivariable models are estimates of the risk of obesity that artificially ignore most of the mechanisms by which obesity might reasonably cause PAD. In a few cases, unadjusted models or models adjusted only for age and sex show a significant association with PAD, even though obesity was nonsignificant or protective after multivariable adjustment.30,49,59 However, in other studies, obesity was found to be either protective or nonsignificant even in unadjusted models or models adjusted only for age and sex.9,15,36,37,39 Thus, the failure to find more cases of positive association between PAD and obesity is not simply an artifact of adjusting for factors on the causal pathway in multivariable modeling, but seems to suggest a real lack of consistent evidence that such a relationship exists at all.
As in coronary heart disease (CHD) epidemiology, there is some evidence to suggest that central adiposity, rather than obesity per se, may be more closely related to an increased risk of PAD. Vogt et al. found that after adjustment for BMI, higher waist/hip ratio was associated with significantly higher risk of PAD.6 In a group of patients with diabetes, it was shown that waist/hip ratio, but not BMI or body fat percentage, was associated with PAD.53
Alcohol Consumption
Evidence for a protective effect of light to moderate alcohol consumption, as seen in CHD, is less consistent for PAD. Two of the five index studies considered alcohol intake; neither showed alcohol to be significantly associated with PAD in either age- and sex-adjusted or multivariable models.9,30 However, in a later analysis of data from one of these studies, a significant protective effect was found in women but not men.68 Conversely, a protective effect of alcohol was seen in men but not women in the Edinburgh Artery Study, but this association disappeared after adjustment for social class.69 In Native Americans, a protective effect of alcohol was seen in multivariable analysis,70 but in elderly Japanese American men, alcohol intake was found to increase rather than decrease the risk of incident PAD.36 Data from the Physician’s Health Study suggest that a protective effect related to moderate alcohol consumption may exist.71 In that study, there was no univariate association between alcohol and claudication incidence, but adjustment for cigarette smoking “unmasked” a significant protective association, reflecting the positive correlation of alcohol consumption with smoking, a strong risk factor for PAD. Based on this, it seems possible that incomplete adjustment for smoking in other studies might allow residual confounding that could obscure any protective effect of alcohol, despite multivariable adjustment.
Race and Ethnicity
Data on the association of race with PAD are limited because many large studies of PAD have been conducted in non-Hispanic white groups. A 2003 review of ethnicity and PAD concluded that there were “no large population-based studies assessing the prevalence of PAD in non-Caucasians.”72
Several studies suggest a higher risk of PAD among blacks. The CHS, a study of 5084 Medicare beneficiaries in the United States, found that nonwhite (mostly black) race was associated with an odds ratio of 2.12 for PAD after adjustment for traditional risk factors.15 A study of 933 women aged 65 and older found a higher percentage of black subjects among the PAD (36.3%) versus non-PAD (24.8%) groups.17 In the ARIC Study, Zheng et al. found that PAD prevalence was higher in African Americans than whites in both men (3.3% vs. 2.3%) and women (4.0% vs. 3.3%).44 The MESA reported a multivariable odds ratio of 1.67 for blacks versus non-Hispanic whites.51 The SDPS reported an odds ratio of 2.34 for blacks versus non-Hispanic whites after adjustment for hypertension and diabetes,52 and additional analyses also showed no evidence of a greater sensitivity of blacks to traditional cardiovascular disease risk factors. Finally, a synthesis of three studies addressing this question reported odds ratios of 2.3 to 3.1 for blacks versus non-Hispanic whites adjusted for age and gender; odds ratios of 1.7 to 2.9 after adjustment for traditional risk factors; and odds ratios of 1.5 to 2.0 after further adjustment for novel risk factors including inflammatory risk factors.73 Thus, this association is in part explained by traditional risk factors and in part by novel risk factors, but there is an unexplained residual difference. Interestingly, hospital-based studies suggest that anatomical distribution of disease may differ in blacks, with a higher percentage of distal disease in black subjects, even after adjustment for diabetes and other cardiovascular risk factors.72
Data on other races and ethnic groups are limited. In a study in Honolulu, Hawaii, Asians were reported to have lower PAD prevalence than comparable non-Hispanic white subjects.36 Both the MESA and the SDPS data suggest somewhat lower rates of PAD in Asians and Hispanics than in non-Hispanic whites.51,52 A study of Native Americans suggested PAD prevalence comparable with that in non-Hispanic whites.70
Homocysteine
The association of homocysteine with PAD has been examined in a number of studies, with conflicting results. A 1995 meta-analysis of early case-control studies conducted in the late 1980s and early 1990s suggested an odds ratio of 6.8 for a 5 μmol/L difference in fasting total homocysteine (tHcy).74 To put this in perspective, the differences between the 25th and 75th percentiles of tHcy among controls in the Physician’s Health Study and a study of women in the Netherlands were between 3.5 and 4.0 μmol/L.60,75 The 5 μmol/L difference noted is therefore not unreasonable as the difference between low and high tHcy levels in the population. In that light, an odds ratio of 6.8 might make homocysteine the single most powerful risk factor for PAD. Interestingly, the odds ratio for PAD in the meta-analysis was strikingly higher than the odds ratios for coronary artery disease (CAD) and cerebrovascular disease, which were below 2 in the same study.
However, more recent studies have produced much lower and frequently nonsignificant estimates of the PAD risk associated with homocysteine. In a large European case-control study, Graham et al. estimated an odds ratio of 1.7 for subjects in the top quintile of homocysteine for their control group versus all other subjects—a result of only borderline statistical significance.76 One population-based study from the Netherlands found a 1.44 odds ratio for a 5 μmol/L difference in fasting tHcy, based on an extreme definition of PAD involving surgery or an ABI of less than 0.5.77 However, an analysis of a subset of the Rotterdam Study cohort found no significant relationship between tHcy and PAD, based either on the conventional 0.9 ABI cut-off or on a 0.7 ABI cut-off for severe disease.9 The MESA reported a significant association for homocysteine after multivariable adjustment for traditional risk factors, but the association just missed significance after adjustment for other novel risk factors.51 A nested case-control study using the Physician’s Health Study cohort failed to find any association between quartiles of fasting tHcy and claudication.60 A recent case-control study of young women in the Netherlands also failed to find any significant association between fasting homocysteine and symptomatic PAD.75 Among patients with PAD, disease progression based on ABI was not significantly different in patients with the highest and lowest 20% of homocysteine levels.78
At this point, although it is still possible that homocysteine may be an independent risk factor for PAD, it appears that the early results summarized in the 1995 meta-analysis may have overstated the importance of homocysteine. This may be related to the quality of the studies included in the meta-analysis, which included primarily small case-control studies.74
C-Reactive Protein and Fibrinogen
C-reactive protein (CRP) and fibrinogen are two inflammatory markers that have been shown to be associated with PAD in a number of studies. In an analysis from the Physician’s Health Study, each was found to be significantly associated with PAD in multivariable models, with odds ratios for the upper versus lower population quartiles of 2.2 for fibrinogen and 2.8 for CRP.60 However, adding both variables to risk prediction models did not improve the accuracy of prediction because they are significantly intercorrelated. Of the index studies, CRP was studied only in the MESA, and it was not significant in multivariable analysis.51 However, fibrinogen was included in four of the five studies and was significantly associated with PAD in multivariable analysis in three of them.9,30,51 Other studies have also reported significant and independent associations of PAD with CRP75 and fibrinogen.36,78
Other Risk Factors
A variety of other potential risk factors for PAD have been examined. In several studies, various measures of oral health have been shown to be independently associated with PAD, possibly based on common inflammatory pathways.79 A study in young women found that self-reported history of various types of infectious diseases, such as chicken pox, shingles, mumps, pneumonia, chronic bronchitis, or peptic ulcer, was independently and significantly related to PAD.75 Another study found that a history of arthritis was associated with PAD as diagnosed by ABI.6
Psychosocial factors were found to be associated with PAD in one large cohort in Scotland,80 whereas in a large study of Israeli men, anxiety, job-related stress, and manner of coping with job-related conflicts were all significantly related to incident claudication even after adjustment for traditional risk factors.1 Among patients with PAD, depressive symptoms were found to be associated with poorer lower-extremity functioning.81
Genetic factors appear to have a role in PAD, but data are limited. In a study of fraternal and identical twins, Carmelli et al. estimated that 48% of the variability in ABI could be explained by additive genetic effects.82 It has also been shown that familial hypercholesterolemia, a genetic disorder, is related to a higher prevalence of PAD.83
Other possible risk factors for which some supporting data exist include antiphospholipid antibodies,84,85 hypothyroidism,86 and sedentary lifestyle.87 Possible protective effects have been reported for hormone replacement therapy,88 but the Women’s Health Initiative randomized clinical trial of combined estrogen/progestin therapy showed no effect on the incidence of PAD.89
Interaction and Risk Factor Comparisons
Differences in the relative strength and significance of risk factors in men and women have been examined in several studies. Many of these studies have concluded that risk factors do not differ substantially in men and women. In the Rotterdam Study, separate models for men and women were compared and failed to reveal differences in risk factors for PAD.9 In the large Framingham and Framingham Offspring cohorts, testing for statistical interactions between sex and risk factors failed to provide any evidence of such interactions.30,50 One study of Medicare beneficiaries in the United States (age 65 and older) found similar risk factor associations with ABI in men and in women, the exceptions being total and LDL cholesterol levels, which were related to ABI in women but not in men.15
Meijer et al. looked at whether severe PAD, diagnosed based on ABI of less than 0.7, had different risk factors than ABI diagnosed based on the traditional cut-point of 0.9.9 In their analysis, the direction and magnitude of odds ratios were similar for most risk factors under the two criteria. Point estimates suggested that age and current smoking were greater risk factors for conventionally defined PAD, whereas diabetes was more important for severe PAD; however, the 95% CIs overlapped in all cases.
Many risk factors that have been studied for their relationship to PAD were originally identified as risk factors for ischemic heart disease. In the most formal comparison of the relative significance and strength of risk factors for PAD versus ischemic heart disease, the same risk factors were analyzed for their association with the two diseases in the Edinburgh Artery Study cohort.49 In that study, only the association with smoking was significantly different for PAD versus ischemic heart disease, with a higher association with PAD. Especially strong or consistent relationships to PAD that were suggested for triglycerides and homocysteine were generally not borne out in later studies, as described earlier. In general among risk factors, only smoking and possibly more severe diabetes seem to show stronger associations with PAD than with ischemic heart disease.
Progression of Peripheral Artery Disease
Little is known about the early natural history of PAD, particularly the progression from asymptomatic to early symptomatic disease. Average annual change in ABI has been estimated as 0.01 and 0.02 in various groups,90,91 but these figures may be somewhat misleading because an average change in ABI masks a variety of changes of different directions and magnitudes.
A more meaningful approach may be to look at the percentage of the population achieving some categorically defined measure of change. The CHS, a population-based study, found that over 6 years of follow-up, 9.5% of persons showed incident PAD, defined as an ABI drop of more than 0.15 to a level of 0.9 or lower.92 Nicoloff et al. found that in 5 years, 37% of patients experienced a significant (≥ 0.15) worsening of ABI, whereas 22% of patients experienced clinical progression of PAD based on a change in symptoms or a need for surgical intervention.93 Among 415 English smokers with PAD referred for a surgical opinion, about half experienced a significant (≥ 0.14) drop in ABI over the following 48 months.63 In a group of German PAD patients, PAD was reported to progress in 18.6% of patients during an average follow-up of 64 months, based on a variety of criteria including change in ABI.94 Bird et al. defined a ranked series of six categories of PAD defined based on ABI and other tests; in a study of patients referred to a vascular laboratory, 30.2% of limbs progressed to a more serious category of PAD over an average follow-up time of 4.6 years, but 22.8% of limbs regressed to a less severe category during the same period.90
In a study based on angiography, 9.1% of patients annually were found to have evidence of progression of PAD.95 In a study using development of rest pain or gangrene as the criteria for PAD progression, PAD progressed in 2.5% of patients annually.87 In the latter study, it was noted that PAD progressed at a rate approximately three times greater in the first year following diagnosis than in subsequent years.96 Because many studies of PAD progression have used subjects whose recruitment is linked to the referral for diagnostic testing, estimates of progression from such studies may be appropriate only for newly diagnosed populations, particularly if follow-up time is short.
Data on risk factors associated with progression of PAD are relatively sparse. In the CHS, significant independent predictors of decline were age, cigarette smoking, diabetes, and dyslipidemia.92 One report showed age, diabetes, classic claudication, previous intervention, and PAD in the contralateral leg to be independently predictive of PAD progression. 90 One study of English smokers with PAD identified hypertriglyceridemia as the most important independent risk factor for progression of PAD and onset of critical ischemia.63 Hemorheological factors have been shown to be associated with an increased risk of need for vascular intervention.97 Patients with premature PAD (onset of symptoms at or before age 45) appear to have more rapid progression of disease and generally poorer outcomes.98–102 Recent data suggest that while PAD progression in large arteries was related to smoking, the TC/HDL-C ratio, lipoprotein(a) (lp[a]), and high-sensitivity CRP assay (hs-CRP), only diabetes was associated with progression in smaller arteries.103
Co-Prevalence of Peripheral Artery Disease and Other Atherosclerotic Disease
Given the common risk factors for PAD and other cardiovascular and cerebrovascular diseases, it is not surprising that cross-sectionally, people with PAD are more likely to have these other disorders, and vice versa. Among 5084 Medicare beneficiaries in the CHS, prevalence of history of MI was 2.5 times as high in subjects with PAD (based on ABI < 0.9) than those without. For angina, congestive heart failure (CHF), stroke, and transient ischemic attack (TIA), the prevalences were 1.9, 3.3, 3.1, and 2.3 times as high, respectively.15 Conversely, prevalence of PAD was 2.1 times as high in patients with a history of MI than in those without. Corresponding ratios for angina, CHF, stroke, and TIA were 1.7, 2.6, 2.4, and 2.1, respectively.15 Other studies have found similar cross-sectional correlations.44,104,105 Subjects with PAD have also been shown to have an elevated prevalence of carotid artery stenosis,106,107 and a modest but significant correlation between severities of the two diseases has been demonstrated.108
Peripheral Artery Disease as a Predictor of Mortality and Morbidity
Attempts to elucidate this association epidemiologically began with studies of patients having symptomatic PAD in the form of intermittent claudication. Elevated mortality rates among subjects with claudication were reported in the 1970s and 1980s in the Framingham cohort, although this excess risk was markedly attenuated when subjects with baseline cerebrovascular and CHD were excluded.37,109,110 Similarly, a 1982 Finnish study failed to find an association between claudication and total or cardiovascular mortality in men after adjustment for cardiovascular risk factors and baseline cardiovascular disease.111 Other studies demonstrated increased mortality risk among claudicants but did not fully adjust for the conventional cardiovascular risk factors.38,95,112 However, in a large and methodologically rigorous study, data from the 18,403 men in the Whitehall cohort were used to show that after adjusting for cardiovascular risk factors, claudication was a significant predictor of cardiovascular disease mortality even after excluding subjects with baseline disease.113
Development of the ABI and other noninvasive measures of PAD permitted further investigation into the association between PAD and cardiovascular disease. In 1985, it was first demonstrated that a combination of noninvasive measures, including ABI, were prospectively related to all-cause mortality even after adjustment for cardiovascular risk factors and exclusion of subjects with baseline cardiovascular disease.114 Relative risks in this study were in the range of 4 to 5; a later reanalysis of the same cohort with additional mortality follow-up demonstrated elevated relative risks for cardiovascular disease and CHD in particular, with no significant increase in noncardiovascular death.3
In the 1990s, a number of other prospective studies confirmed that ABI was related to cardiovascular disease, based on either mortality or combined mortality and morbidity. This was found to be true in a variety of populations: vascular laboratory patients,28,115 elderly patients with hypertension,116 elderly women,117 an employment-based cohort from Belgium,118 the Edinburgh Artery Study cohort from Scotland,16 and the CHS cohort.29 Most of these studies controlled for various known cardiovascular disease risk factors and presence of cardiovascular disease at baseline. Relative risks reported ranged from roughly 2 to 5. Many of these studies also found PAD to be significantly associated with incident CHD in particular, although the very large CHS failed to find such associations for either total MI or angina.29
Data regarding the association of PAD with cerebrovascular disease are less conclusive. A 1991 study showed a strong association between multiple noninvasive measures of PAD and cerebrovascular disease morbidity and mortality, with risk ratios of 3.3 for men and 9.0 for women after multivariable adjustment.119 Data from the Edinburgh Artery Study also showed such an association based on ABI, although after multivariable adjustment, the association persisted for nonfatal but not fatal stroke.16 However, data from the CHS failed to show a relationship between low ABI and incident stroke.29 Another large study, the ARIC Study, showed a significant association between ABI as a continuous variable and ischemic stroke after multivariable adjustment, but failed to show such association when ABI was categorized based on a 0.8 cut-point.120
Population studies suggest a high ABI (> 1.4), is also associated with elevated risk of cardiovascular disease.32 Such high ABIs are caused by stiff, often calcified, ankle arteries that may mask underlying PAD.14 Recently, the MESA reported that both “low” (< 1.00) and “high” (> 1.40) ABI were associated with increased risk of incident cardiovascular disease events, even after adjustment for traditional and novel risk factors.121 Interestingly, high ABI showed a stronger association for stroke than low ABI. Also, this was the first report to show that the ABI predicted events independent of other measures of extant atherosclerosis—specifically, coronary artery calcium, carotid intima media thickness, and major electrocardiographic abnormalities. Recent evidence also indicates that independent of baseline ABI, a more rapid deterioration in ABI carries a worse prognosis.122
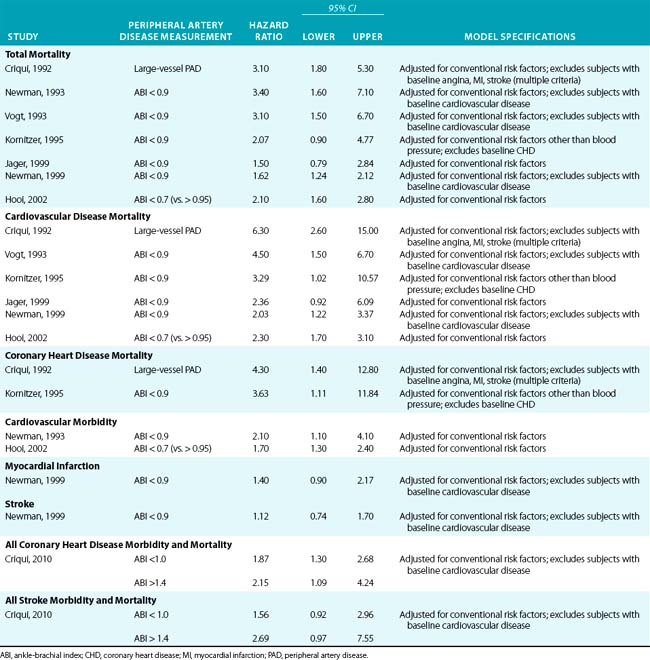
Table 16-5 provides a summary of studies of the association of PAD with various mortality and morbidity outcomes. The table is limited to studies using a noninvasive measure of PAD (usually ABI at various cut-points), and logistic or proportional hazards regression models with multivariable adjustment for conventional cardiovascular risk factors. Results are shown with multivariable adjustment and after exclusion of subjects with baseline cardiovascular disease, where such exclusion was attempted.
1 Bowlin S.J., Medalie J.H., Flocke S.A., et al. Epidemiology of intermittent claudication in middle-aged men. Am J Epidemiol. 1994;140:418.
2 Allison M.A., Ho E., Denenberg J.O., et al. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am J Prev Med. 2007;32:328.
3 Criqui M.H., Langer R.D., Fronek A., et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381.
4 Rose G.A. The diagnosis of ischaemic heart pain and intermittent claudication in field surveys. Bull World Health Organ. 1962;27:645.
5 Criqui M.H., Denenberg J.O., Bird C.E., et al. The correlation between symptoms and non-invasive test results in patients referred for peripheral arterial disease testing. Vasc Med. 1996;1:65.
6 Vogt M.T., Cauley J.A., Kuller L.H., et al. Prevalence and correlates of lower-extremity arterial disease in elderly women. Am J Epidemiol. 1993;137:559.
7 Winsor T. Influence of arterial disease on the systolic blood pressure gradients of the extremity. Am J Med Sci. 1950;220:117.
8 Hooi J.D., Stoffers H.E., Kester A.D., et al. Peripheral arterial occlusive disease: prognostic value of signs, symptoms, and the ankle-brachial pressure index. Med Decis Making. 2002;22:99.
9 Meijer W.T., Grobbee D.E., Hunink M.G., et al. Determinants of peripheral arterial disease in the elderly: the Rotterdam study. Arch Intern Med. 2000;160:2934.
10 Meijer W.T., Hoes A.W., Rutgers D., et al. Peripheral arterial disease in the elderly: the Rotterdam Study. Arterioscler Thromb Vasc Biol. 1998;18:185.
11 Yao S.T., Hobbs J.T., Irvine W.T. Ankle systolic pressure measurements in arterial disease affecting the lower extremities. Br J Surg. 1969;56:676.
12 Ouriel K., McDonnell A.E., Metz C.E., et al. Critical evaluation of stress testing in the diagnosis of peripheral vascular disease. Surgery. 1982;91:686.
13 Lijmer J.G., Hunink M.G., van den Dungen J.J., et al. ROC analysis of noninvasive tests for peripheral arterial disease. J Ultrasound Med Biol. 1996;22:391.
14 Aboyans V., Ho E., Denenberg J.O., et al. The association between elevated ankle systolic pressures and peripheral occlusive arterial disease in diabetic and non-diabetic subjects. J Vasc Surg. 2008;48:1197.
15 Newman A.B., Siscovick D.S., Manolio T.A., et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Heart Study (CHS) Collaborative Research Group. Circulation. 1993;88:837.
16 Leng G.C., Fowkes F.G., Lee A.J., et al. Use of ankle-brachial pressure index to predict cardiovascular events and death: a cohort study. BMJ. 1996;313:1440.
17 McDermott M.M., Fried L., Simonsick E., et al. Asymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: the Women’s Health and Aging Study. Circulation. 2000;101:1007.
18 McDermott M.M., Liu K., O’Brien E., et al. Measuring physical activity in peripheral arterial disease: a comparison of two physical activity questionnaires with an accelerometer. Angiology. 2000;51:91.
19 McDermott M.M., Ferrucci L., Simonsick E.M., et al. The ankle-brachial index and change in lower-extremity functioning over time: the Women’s Health and Aging Study. J Am Geriatr Soc. 2002;50:238.
20 McDermott M.M., Criqui M.H., Liu K., et al. Lower ankle-brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease. J Vasc Surg. 2000;32:116.
21 Aboyans V., Lacroix P., Lebourdon A., et al. The intra- and interobserver variability of ankle-arm blood pressure index according to its mode of calculation. J Clin Epidemiol. 2003;56:215.
22 Shadman R., Criqui M.H., Bundens W.P., et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44:618.
23 Fowkes F.G., Housley E., Cawood E.H., et al. Edinburgh Artery Study: Prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1991;20:384.
24 Hiatt W.R., Hoag S., Hamman R.F. Effect of diagnostic criteria on the prevalence of peripheral arterial disease: the San Luis Valley Diabetes Study. Circulation. 1995;91:1472.
25 Aboyans V., Criqui M.H., McClelland R.L., et al. Intrinsic contribution of gender and ethnicity to normal ankle-brachial index values: the Multi-Ethnic Study of Atherosclerosis (MESA). J Vasc Surg. 2007;45:319.
26 Kreines K., Johnson E., Albrink M., et al. The course of peripheral vascular disease in non-insulin-dependent diabetes. Diabetes Care. 1985;8:235.
27 Orchard T.J., Strandness D.E.Jr. Assessment of peripheral vascular disease in diabetes. Report and recommendations of an international workshop sponsored by the American Heart Association and the American Diabetes Association, 18-20 September 1992, New Orleans, Louisiana. Diabetes Care. 1993;16:1199.
28 McKenna M., Wolfson S., Kuller L. The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis. 1991;87:119.
29 Newman A.B., Shemanski L., Manolio T.A., et al. Ankle-arm index as a predictor of cardiovascular disease and mortality in the Cardiovascular Health Study. The Cardiovascular Health Study Group. Arterioscler Thromb Vasc Biol. 1999;19:538.
30 Murabito J.M., Evans J.C., Nieto K., et al. Prevalence and clinical correlates of peripheral arterial disease in the Framingham Offspring Study. Am Heart J. 2002;143:961.
31 Wang J.C., Criqui M.H., Denenberg J.O., et al. Exertional leg pain in patients with and without peripheral arterial disease. Circulation. 2005;112:3501.
32 Ankle Brachial Index Collaboration. Ankle brachial index combined with Framingham risk score to predict cardiovascular events and mortality. A meta-analysis. JAMA. 2008;300:197.
33 Criqui M.H., Fronek A., Barrett-Connor E., et al. The prevalence of peripheral arterial disease in a defined population. Circulation. 1985;71:510.
34 Beks P.J., Mackaay A.J., de Neeling J.N., et al. Peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: the Hoorn study. Diabetologia. 1995;38:86.
35 Stoffers H.E., Rinkens P.E., Kester A.D., et al. The prevalence of asymptomatic and unrecognized peripheral arterial occlusive disease. Int J Epidemiol. 1996;25:282.
36 Curb J.D., Masaki K., Rodriguez B.L., et al. Peripheral artery disease and cardiovascular risk factors in the elderly. The Honolulu Heart Program. Arterioscler Thromb Vasc Biol. 1996;16:1495.
37 Kannel W.B., McGee D.L. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985;33:13.
38 Dagenais G.R., Maurice S., Robitaille N.M., et al. Intermittent claudication in Quebec men from 1974-1986: the Quebec Cardiovascular Study. Clin Invest Med. 1991;14:93.
39 Bainton D., Sweetnam P., Baker I., et al. Peripheral vascular disease: consequence for survival and association with risk factors in the Speedwell prospective heart disease study. Br Heart J. 1994;72:128.
40 Leng G.C., Lee A.J., Fowkes F.G., et al. Incidence, natural history and cardiovascular events in symptomatic and asymptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1996;25:1172.
41 Ingolfsson I.O., Sigurdsson G., Sigvaldason H., et al. A marked decline in the prevalence and incidence of intermittent claudication in Icelandic men 1968-1986: a strong relationship to smoking and serum cholesterol—the Reykjavik Study. J Clin Epidemiol. 1994;47:1237.
42 Hooi J.D., Kester A.D., Stoffers H.E., et al. Incidence of and risk factors for asymptomatic peripheral arterial occlusive disease: a longitudinal study. Am J Epidemiol. 2001;153:666.
43 Gallotta G., Iazzetta N., Milan G., et al. Prevalence of peripheral arterial disease in an elderly rural population of southern Italy. Gerontology. 1997;43:289.
44 Zheng Z.J., Sharrett A.R., Chambless L.E., et al. Associations of ankle-brachial index with clinical coronary heart disease, stroke and preclinical carotid and popliteal atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis. 1997;131:115.
45 McDermott M.M., Liu K., Criqui M.H., et al. The ankle brachial index and subclinical cardiac and carotid disease: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2005;162:33.
46 Faulkner K.W., House A.K., Castleden W.M. The effect of cessation of smoking on the accumulative survival rates of patients with symptomatic peripheral vascular disease. Med J Aust. 1983;1:217.
47 Quick C.R., Cotton L.T. The measured effect of stopping smoking on intermittent claudication. Br J Surg. 1982;69(Suppl):S24.
48 Jonason T., Bergstrom R. Cessation of smoking in patients with intermittent claudication: effects on the risk of peripheral vascular complications, myocardial infarction and mortality. Acta Med Scand. 1987;221:253.
49 Fowkes F.G., Housley E., Riemersma R.A., et al. Smoking, lipids, glucose intolerance, and blood pressure as risk factors for peripheral atherosclerosis compared with ischemic heart disease in the Edinburgh Artery Study. Am J Epidemiol. 1992;135:331.
50 Murabito J.M., D’Agostino R.B., Silbershatz H., et al. Intermittent claudication: a risk profile from The Framingham Heart Study. Circulation. 1997;96:44.
51 Allison M.A., Criqui M.H., McClelland R.L., et al. the effect of novel cardiovascular risk factors on the ethnic-specific odds for peripheral arterial disease in the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Coll Cardiol. 2006;48:1190.
52 Criqui M.H., Vargas V., Denenberg J.O., et al. Ethnicity and peripheral arterial disease: the San Diego Population Study. Circulation. 2005;112:2703.
53 Katsilambros N.L., Tsapogas P.C., Arvanitis M.P., et al. Risk factors for lower extremity arterial disease in non-insulin-dependent diabetic persons. Diabet Med. 1996;13:243.
54 Tseng C.H. Prevalence and risk factors of peripheral arterial obstructive disease in Taiwanese type 2 diabetic patients. Angiology. 2003;54:331.
55 Kallio M., Forsblom C., Groop P.H., et al. Development of new peripheral arterial occlusive disease in patients with type 2 diabetes during a mean follow-up of 11 years. Diabetes Care. 2003;26:1241.
56 Jude E.B., Oyibo S.O., Chalmers N., et al. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24:1433.
57 Haltmayer M., Mueller T., Horvath W., et al. Impact of atherosclerotic risk factors on the anatomical distribution of peripheral arterial disease. Int Angiol. 2001;20:200.
58 Natarajan S., Glick H., Criqui M., et al. Cholesterol measures to identify and treat individuals at risk for coronary disease. Am J Prev Med. 2003;25:50.
59 Ness J., Aronow W.S., Ahn C. Risk factors for symptomatic peripheral arterial disease in older persons in an academic hospital-based geriatrics practice. J Am Geriatr Soc. 2000;48:312.
60 Ridker P.M., Stampfer M.J., Rifai N. Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA. 2001;285:2481.
61 Fowkes F.G. Epidemiology of atherosclerotic arterial disease in the lower limbs. Eur J Vasc Surg. 1988;2:2831.
62 Cheng S.W., Ting A.C., Wong J. Fasting total plasma homocysteine and atherosclerotic peripheral vascular disease. Ann Vasc Surg. 1997;11:217.
63 Smith I., Franks P.J., Greenhalgh R.M., et al. The influence of smoking cessation and hypertriglyceridaemia on the progression of peripheral arterial disease and the onset of critical ischaemia. Eur J Vasc Endovasc Surg. 1996;11:402.
64 Mowat B.F., Skinner E.R., Wilson H.M., et al. Alterations in plasma lipids, lipoproteins and high density lipoprotein subfractions in peripheral arterial disease. Atherosclerosis. 1997;131:161.
65 Criqui M.H., Denenberg J.O., Langer R.D., et al. Peripheral arterial disease and hypertension. In: Izzo J.L., Black H.R. Hypertension primer. Dallas: American Heart Association; 2003:250.
66 Dormandy J., Heeck L., Vig S. Predictors of early disease in the lower limbs. Semin Vasc Surg. 1999;12:109.
67 Tseng C.H. Prevalence and risk factors of peripheral arterial obstructive disease in Taiwanese type 2 diabetic patients. Angiology. 2003;54:331.
68 Vliegenthart R., Geleijnse J.M., Hofman A., et al. Alcohol consumption and risk of peripheral arterial disease: the Rotterdam Study. Am J Epidemiol. 2002;155:332.
69 Jepson R.G., Fowkes F.G., Donnan P.T., et al. Alcohol intake as a risk factor for peripheral arterial disease in the general population in the Edinburgh Artery Study. Eur J Epidemiol. 1995;11:9.
70 Fabsitz R.R., Sidawy A.N., Go O., et al. Prevalence of peripheral arterial disease and associated risk factors in American Indians: the Strong Heart Study. Am J Epidemiol. 1999;149:330.
71 Camargo C.A.Jr., Stampfer M.J., Glynn R.J., et al. Prospective study of moderate alcohol consumption and risk of peripheral arterial disease in U.S. male physicians. Circulation. 1997;95:577.
72 Hobbs S.D., Wilmink A.B., Bradbury A.W. Ethnicity and peripheral arterial disease. Eur J Vasc Endovasc Surg. 2003;25:505.
73 Ix J.H., Allison M.A., Denenberg J.O., et al. Novel cardiovascular risk factors do not completely explain the higher prevalence of peripheral arterial disease among African Americans. The San Diego Population Study. J Am Coll Cardiol. 2008;51:2347.
74 Boushey C.J., Beresford S.A., Omenn G.S., et al. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995;274:1049.
75 Bloemenkamp D.G., van den Bosch M.A., Mali W.P., et al. Novel risk factors for peripheral arterial disease in young women. Am J Med. 2002;113:462.
76 Graham I.M., Daly L.E., Refsum H.M., et al. Plasma homocysteine as a risk factor for vascular disease. The European Concerted Action Project. JAMA. 1997;277:1775.
77 Hoogeveen E.K., Kostense P.J., Beks P.J., et al. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus: a population-based study. Arterioscler Thromb Vasc Biol. 1998;18:133.
78 Taylor L.M.Jr., Moneta G.L., Sexton G.J., et al. Prospective blinded study of the relationship between plasma homocysteine and progression of symptomatic peripheral arterial disease. J Vasc Surg. 1999;29:8.
79 Hung H.C., Willett W., Merchant A., et al. Oral health and peripheral arterial disease. Circulation. 2003;107:1152.
80 Whiteman M.C., Deary I.J., Fowkes F.G. Personality and social predictors of atherosclerotic progression: Edinburgh Artery Study. Psychosom Med. 2000;62:703.
81 McDermott M.M., Greenland P., Guralnik J.M., et al. Depressive symptoms and lower extremity functioning in men and women with peripheral arterial disease. J Gen Intern Med. 2003;18:461.
82 Carmelli D., Fabsitz R.R., Swan G.E., et al. Contribution of genetic and environmental influences to ankle-brachial blood pressure index in the NHLBI Twin Study. National Heart, Lung, and Blood Institute. Am J Epidemiol. 2000;151:452.
83 Kroon A.A., Ajubi N., van Asten W.N., et al. The prevalence of peripheral vascular disease in familial hypercholesterolaemia. J Intern Med. 1995;238:451.
84 Taylor L.M.Jr., Chitwood R.W., Dalman R.L., et al. Antiphospholipid antibodies in vascular surgery patients: a cross-sectional study. Ann Surg. 1994;220:544.
85 Lam E.Y., Taylor L.M.Jr., Landry G.J., et al. Relationship between antiphospholipid antibodies and progression of lower extremity arterial occlusive disease after lower extremity bypass operations. J Vasc Surg. 2001;33:976.
86 Mya M.M., Aronow W.S. Increased prevalence of peripheral arterial disease in older men and women with subclinical hypothyroidism. J Gerontol A Biol Sci Med Sci. 2003;58:68.
87 Asgeirsdottir L.P., Agnarsson U., Jonsson G.S. Lower extremity blood flow in healthy men: effect of smoking, cholesterol, and physical activity—a Doppler study. Angiology. 2001;52:437.
88 Westendorp I.C., in’t Veld B.A., Grobbee D.E., et al. Hormone replacement therapy and peripheral arterial disease: the Rotterdam Study. Arch Intern Med. 2000;160:2498.
89 Hsia J., Criqui M.H., Rodabough R., et al. Estrogen plus progestin and the risk of peripheral arterial disease: the Women’s Health Initiative. Circulation. 2004;109:620.
90 Bird C.E., Criqui M.H., Fronek A., et al. Quantitative and qualitative progression of peripheral arterial disease by non-invasive testing. Vasc Med. 1999;4:15.
91 Fowkes F.G., Lowe G.D., Housley E., et al. Cross-linked fibrin degradation products, progression of peripheral arterial disease, and risk of coronary heart disease. Lancet. 1993;342:84.
92 Kennedy M., Solomon C., Manolio T.A., et al. Risk factors for declining ankle-brachial index in men and women 65 years or older: the Cardiovascular Health Study. Arch Intern Med. 2005;165:1896.
93 Nicoloff A.D., Taylor L.M.Jr., Sexton G.J., et al. Relationship between site of initial symptoms and subsequent progression of disease in a prospective study of atherosclerosis progression in patients receiving long-term treatment for symptomatic peripheral arterial disease. J Vasc Surg. 2002;35:38.
94 Taute B.M., Gläser C., Taute R., et al. Progression of atherosclerosis in patients with peripheral arterial disease as a function of angiotensin-converting enzyme gene insertion/deletion polymorphism. Angiology. 2002;53:375.
95 Walsh D.B., Gilbertson J.J., Zwolak R.M., et al. The natural history of superficial femoral artery stenoses. J Vasc Surg. 1991;14:299.
96 Jelnes R., Gaardsting O., Hougaard Jensen K., et al. Fate in intermittent claudication: outcome and risk factors. Br Med J (Clin Res Ed). 1986;293:1137.
97 Smith F.B., Lowe G.D., Lee A.J., et al. Smoking, hemorheologic factors, and progression of peripheral arterial disease in patients with claudication. J Vasc Surg. 1998;28:129.
98 McCready R.A., Vincent A.E., Schwartz R.W., et al. Atherosclerosis in the young: a virulent disease. Surgery. 1984;96:863.
99 Pairolero P.C., Joyce J.W., Skinner C.R., et al. Lower limb ischemia in young adults: prognostic implications. J Vasc Surg. 1984;1:459.
100 Hallett J.W.Jr., Greenwood L.H., Robison J.G. Lower extremity arterial disease in young adults: a systematic approach to early diagnosis. Ann Surg. 1985;202:647.
101 Valentine R.J., MacGillivray D.C., DeNobile J.W., et al. Intermittent claudication caused by atherosclerosis in patients aged forty years and younger. Surgery. 1990;107:560.
102 Levy P.J., Hornung C.A., Haynes J.L., et al. Lower extremity ischemia in adults younger than forty years of age: a community-wide survey of premature atherosclerotic arterial disease. J Vasc Surg. 1994;19:873.
103 Aboyans V., Criqui M.H., Denenberg J.O., et al. Risk factors for progression of peripheral arterial disease in large and small vessels. Circulation. 2006;113:2623.
104 Criqui M.H., Denenberg J.O., Langer R.D., et al. The epidemiology of peripheral arterial disease: importance of identifying the population at risk. Vasc Med. 1997;2:221.
105 Ness J., Aronow W.S. Prevalence of coexistence of coronary artery disease, ischemic stroke, and peripheral arterial disease in older persons, mean age 80 years, in an academic hospital-based geriatrics practice. J Am Geriatr Soc. 1999;47:1255.
106 Alexandrova N.A., Gibson W.C., Norris J.W., et al. Carotid artery stenosis in peripheral vascular disease. J Vasc Surg. 1996;23:645.
107 Pilcher J.M., Danaher J., Khaw K.T. The prevalence of asymptomatic carotid artery disease in patients with peripheral vascular disease. Clin Radiol. 2000;55:56.
108 Long T.H., Criqui M.H., Vasilevskis E.E., et al. The correlation between the severity of peripheral arterial disease and carotid occlusive disease. Vasc Med. 1999;4:135.
109 Kannel W.B., Skinner J.J.Jr., Schwartz M.J., et al. Intermittent claudication: incidence in the Framingham Study. Circulation. 1970;41:875.
110 Kannel W.B., Shurtleff D. The natural history of arteriosclerosis obliterans. Cardiovasc Clin. 1971;3:37.
111 Reunanen A., Takkunen H., Aromaa A. Prevalence of intermittent claudication and its effect on mortality. Acta Med Scand. 1982;211:249.
112 Kallero K.S. Mortality and morbidity in patients with intermittent claudication as defined by venous occlusion plethysmography: a ten-year follow-up study. J Chronic Dis. 1981;34:455.
113 Smith G.D., Shipley M.J., Rose G. Intermittent claudication, heart disease risk factors, and mortality: the Whitehall Study. Circulation. 1990;82:1925.
114 Criqui M.H., Coughlin S.S., Fronek A. Noninvasively diagnosed peripheral arterial disease as a predictor of mortality: results from a prospective study. Circulation. 1985;72:768.
115 McDermott M.M., Feinglass J., Slavensky R., et al. The ankle-brachial index as a predictor of survival in patients with peripheral vascular disease. J Gen Intern Med. 1994;9:445.
116 Newman A.B., Sutton-Tyrrell K., Vogt M.T., et al. Morbidity and mortality in hypertensive adults with a low ankle/arm blood pressure index. JAMA. 1993;270:487.
117 Vogt M.T., Cauley J.A., Newman A.B., et al. Decreased ankle/arm blood pressure index and mortality in elderly women. JAMA. 1993;270:465.
118 Kornitzer M., Dramaix M., Sobolski J., et al. Ankle/arm pressure index in asymptomatic middle-aged males: an independent predictor of ten-year coronary heart disease mortality. Angiology. 1995;46:211.
119 Criqui M.H., Langer R.D., Fronek A., et al. Coronary disease and stroke in patients with large-vessel peripheral arterial disease. Drugs. 1991;42(Suppl 5):16.
120 Tsai A.W., Folsom A.R., Rosamond W.D., et al. Ankle-brachial index and 7-year ischemic stroke incidence: the ARIC study. Stroke. 2001;32:1721.
121 Criqui M.H., McClelland R.L., McDermott M.M., et al. The ankle-brachial index and incident cardiovascular events in the MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2010;56:1506.
122 Criqui M.H., Ninomiya J.K., Wingard D.L., et al. Progression of peripheral arterial disease predicts cardiovascular disease morbidity and mortality. J Am Coll Cardiol. 2008;52:1736.