CHAPTER 85 The Elbow in Metabolic Disease
INTRODUCTION
With the possible exception of tumoral calcinosis, no metabolic diseases have a special predilection for or a characteristic presentation at or about the elbow joint.1,6,19 Therefore, information is rather limited on the effects of metabolic bone disease of the elbow joint. In fact, at the Mayo Clinic, the radiographic bone survey routinely taken to assess the extent of involvement of these diseases does not include the elbow region. A MEDLINE review of all the conditions discussed herein from 1996 to 2007 revealed only one citation of any of these conditions related to the elbow.12 No attempt will be made here to mention all the conditions that might incidentally involve the elbow. However, several conditions are regularly manifested at this joint: gout, pseudogout, and inborn errors of metabolism that cause congenital anomalies (see Chapters 13 and 75). Paget’s disease may, of course, involve any part of the body, including the elbow (see Chapter 82). Synovial chondromatosis is mentioned here and in the section on arthroscopic management of loose bodies (see Chapter 38).
RICKETS
In the immature skeleton, vitamin D deficiency typically causes widening of the physis and cupping of the metaphysis, which are well represented at the wrist. Interestingly, although it has not been emphasized in the literature, rather dramatic widening of the radiohumeral joint is typical of this disease (Fig. 85-1). The deficiency will obviously be better demonstrated in the faster growing bones, and the physes of the distal humerus and proximal forearm are relatively slow growing.6 Thus, the manifestations of rickets in the region of the elbow are usually not dramatic.
OSTEOMALACIA
Classically, vitamin D deficiency of the mature skeleton resulting in the production of uncalcified osteoid may be due to one of several mechanisms—nutritional intake deficiencies, absorption abnormalities, and utilization abnormalities.15,16 Dialysis is one of the most common causes for this condition today. Radiographically, marked loss of bone density is usually observed along with coarsening of the trabecular pattern. There are no characteristic features at the elbow (Fig. 85-2). The lack of structural integrity causes bowing deformities of the weight-bearing extremities, but this is uncommon in the upper limbs.
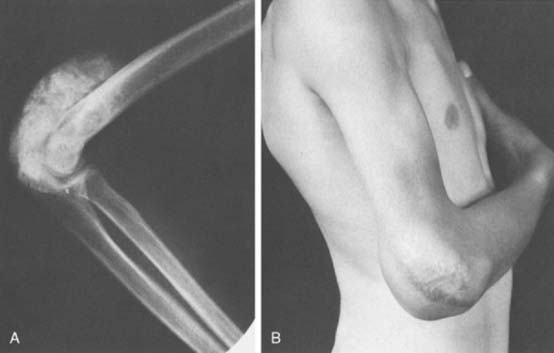
TUMORAL CALCINOSIS
Extensive para-articular calcification, so-called tumoral calcinosis, does have a certain predilection for the elbow region, although it is more common at the hips and shoulders.7 The differential diagnosis includes hyperparathyroidism, hypervitaminosis D, calcinosis universalis, and calcinosis circumscripta.4 Tumoral calcinosis characteristically occurs in young persons who have normal serum calcium concentrations, but a predilection has been noted in black persons and a familial tendency has also been reported.7,12 First described by Inclan and colleagues in 1943,9 the association with hyperphosphatemia has suggested a metabolic cause for this disease.2,13 Chemical assessment reveals hyperphosphatemia but normal levels of serum calcium, parathyroid hormone, and alkaline phosphatase. The exact cause of the condition is obscure, but calcium salts are deposited in the posterior or anterior extra-articular regions of the elbow. The calcium salt is usually calcium phosphate or carbonate. A well-circumscribed capsule may be present around the firm to soft, discrete masses. Sinus drainage may be seen as well.12 In one report, a similar radiographic appearance was demonstrated that was attributed to the deposition of hydroxyapatite crystals.8 The intra-articular nature of this deposition serves to distinguish it from true tumoral calcinoses (Fig. 85-3). Surgical treatment can be successful, particularly if the tumor masses are relatively small. Large areas of involvement, however, often cause difficulty with wound healing, and scarring in the skin and subcutaneous tissue (see Fig. 85-3). Recurrences are common even if excision appears to have been complete.
HYPERPARATHYROIDISM
Primary hyperparathyroidism may be due to an adenoma, hyperplasia, carcinoma, or an aberrant tumor that secretes the parathyroid hormone22 or to type II multiple endocrine neoplasia. Secondary hyperparathyroidism is the result of a chronic hypocalcemic state that stimulates the production of parathyroid hormone. The classic radiographic appearance of hyperparathyroidism is subperiosteal resorption, especially along the radial margin of the middle phalanges of the hand. More advanced but less common changes involve resorption of large amounts of bone, a phenomenon that results in the radiographic appearance of the so-called brown tumor. Hyperparathyroidism rarely demonstrates any features in the region of the elbow, but occasionally periosteal resorption or a brown tumor may be observed.
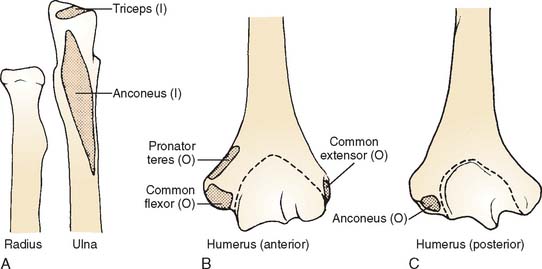
A careful radiographic analysis of the manifestations of renal osteodystrophy at the elbow was published by Kricun and Resnick.11 Subtendinous bone resorption tends to occur at the origin and insertion of the tendinous attachments about the elbow (Figs. 85-4 and 85-5). Possibly the most dramatic change is resorption of the subcutaneous border around the olecranon. Resorption at the ulnar site of the origin of the anconeus is such a prominent feature in this disease that it is believed to be pathognomonic for hyperparathyroidism.11 Additional radiographic characteristics include the subchondral cystic erosions often noted at the ulnohumeral articulation, which are thought to be one of the characteristic manifestations of the disease.3
ACROMEGALY
The skeletal manifestations of acromegaly have been well described.5 The elbow is affected in fewer than 10% of patients, 74% of whom have skeletal manifestations of the disease. Approximately 75% of patients have some skeletal manifestation, about 10% of which involve the elbow. The manifestation is a hypertrophic osteophytic reaction, especially of the coronoid process and olecranon.24 Thus, the appearance and treatment are similar to those for primary degenerative arthritis (see Chapter 67).
WILSON’S DISEASE (HEPATOLENTICULAR DEGENERATION)
Caused by an inborn error of copper metabolism, Wilson’s disease is best known for renal, hepatic, and neurologic symptoms; however, its effect on the bones and joints is well known.18,21,22 Osteoporosis occurs in about 75% of patients,18 and osteomalacia is also common.21 Joint involvement includes degenerative changes, sclerosis, fragmentation, and periarticular calcification (Fig. 85-6).
HYPERLIPOPROTEINEMIA TYPE II (FAMILIAL ESSENTIAL HYPERCHOLESTEROLEMIA)
Periosteal xanthomatosis and tendon xanthomas result from increased serum cholesterol levels, which promote accumulation of cholesterol crystals. Typically, the olecranon bursa and the triceps tendon are susceptible to this disorder.23 If the process is symptomatic in the olecranon bursa, excision may be indicated. Care should be taken, however, before excising these deposits in the triceps tendon, because this can weaken the extensor mechanism. The usual approach is to treat the underlying disease, as with diet and clofibrate (Atromid-S).
OSTEOPOROSIS
In the broadest sense, osteoporosis may be defined as a decrease of bone substance so extreme as to be pathologic and to result in spontaneous fractures.10 Although these usually occur in the spine, distal radius, and hip, proximal humeral20 and pelvic fractures17 associated with minimal trauma have been linked to osteoporosis. The effects at the elbow are most often manifested as type III radial head fractures or comminuted olecranon fractures in older persons and are associated with relatively little trauma. Unlike the spine and hip, the elbow region exhibits no characteristic radiographic features of osteoporosis.
STEROID-INDUCED AVASCULAR NECROSIS
Although recognized complications are known to involve the hip, shoulder, knee, and ankle, steroid-induced avascular necrosis is uncommon.14 The diagnosis is easily made by magnetic resonance imaging (Fig. 85-7). This has been the subject of only a few case reports, and we, personally, have seen less than 10 such cases. Although this experience is hardly definitive, we have had some success with arthroscopic dissected drilling/decompression of the involved portion of the joint.
1 Aegerter E., Kirkpatrick J.A. Orthopedic Diseases, 4th ed. Philadelphia: W. B. Saunders Co., 1975.
2 Baldursson H., Evans E.B., Dodge W.F., Jackson W.T. Tumoral calcinosis with hyperphosphatemia. J. Bone Joint Surg. 1969;51A:913.
3 Bywaters E.G.L., Dixon A.S.J., Scott J.T. Joint lesions in hyperparathyroidism. Ann. Rheum. Dis. 1963;22:171.
4 Destouet J.M., Gilula L.A. Painful nodules of the right forearm and elbow. Orthop. Rev. 1985;14:99.
5 Dettenbeck L.C., Tressler H.A., O’Duffy J.D., Randall R.V. Peripheral joint manifestations of acromegaly. Clin. Orthop. Relat. Res. 1973;91:119-127.
6 Greenfield G.B. Radiology of Bone Diseases, 2nd ed. Philadelphia: J. B. Lippincott Co., 1975.
7 Hensley D.C., Lin J.J. Massive intra-synovial deposition of calcium pyrophosphate in the elbow. J. Bone Joint Surg. 1984;66A:133.
8 Hartofilakidis-Garofalidis G., Theodossiou A., Matsoukas J., Rigopoulos C., Papathanassiou B. Tumoral lipo-calcinosis. Ann. Intern. Med. 1970;41:387.
9 Inclan A., Leon P., Gomez C.M. Tumoral calcinosis. J. A. M. A. 1943;121:490.
10 Jowsey J. Metabolic Diseases of Bone. Philadelphia: W. B. Saunders Co., 1977.
11 Kricun M.E., Resnick D. Elbow abnormalities in renal osteodystrophy. A. J. R. 1983;140:577.
12 Kumaran M.S., Bhadada S., Bhansali A., Shiriram M., Kumar B. Young boy with multiple periarticular swellings and discharging sinuses: Tumoral calcinosis. Indian J. Pediatr. 2004;71:e74.
13 Lafferty F.W., Reynolds E.S., Pearson O.H. Tumoral calcinosis: a metabolic disease of obscure etiology. Am. J. Med. 1965;38:105.
14 Madsen P.V., Andersen G. Multifocal osteonecrosis related to steroid treatment in a patient with ulcerative colitis. Gut. 1994;35:132.
15 Mankin H.J. Rickets, osteomalacia, and renal osteodystrophy, Part I (review article). J. Bone Joint Surg. 1974;56A:101.
16 Mankin H.J. Rickets, osteomalacia, and renal osteodystrophy, Part II (review article). J. Bone Joint Surg. 1974;56A:352.
17 Melton L.J., Sampson J.M., Morrey B.F., Ilstrup D.M. Epidemiologic features of pelvic fractures. Clin. Orthop. 1981;155:43.
18 Mindelzun R., Elkin M., Scheinberg I.H., Sternlieb I. Skeletal changes in Wilson’s disease. A radiological study. Radiology. 1970;94:127.
19 Pugh D.G. Radiographic Diagnosis of Diseases of the Bone. New York: Thomas Nelson, 1951.
20 Rose S.H., Melton L.J., Morrey B.F., Ilstrup D.M., Riggs B.L. Epidemiologic features of humeral fractures. Clin. Orthop. Relat. Res. 1982;168:24.
21 Rosenoer V.M., Mitchell R.C. Skeletal changes in Wilson’s disease (hepatolenticular degeneration). Br. J. Radiol. 1959;32:805.
22 Salassa R.M., Jowsey J., Arnaud C.D. Hypophosphatemic osteomalacia associated with “non-endocrine tumors.”. N. Engl. J. Med.. 1970;283:65.
23 Smith F.M. Surgery of the Elbow, 2nd ed. Philadelphia: W. B. Saunders, 1972.
24 Tsai E., Freiberg A.A., Louis D.S. Elbow arthrosis as an initial presentation of acromegaly. Orthopedics. 1998;21:901-902.