9 The elbow
Introduction
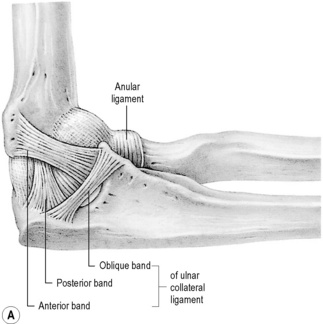
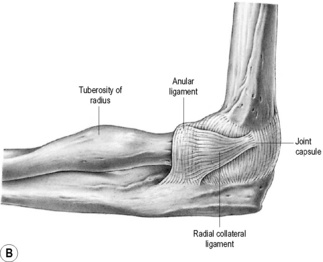
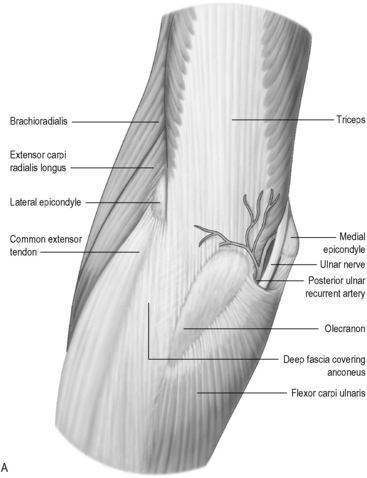
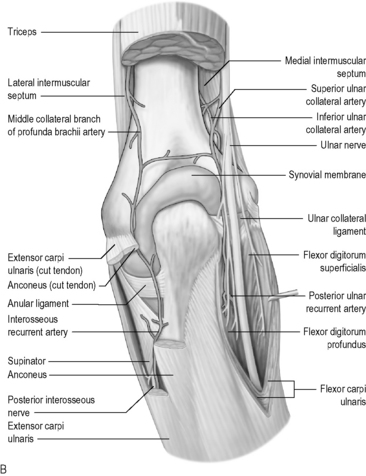
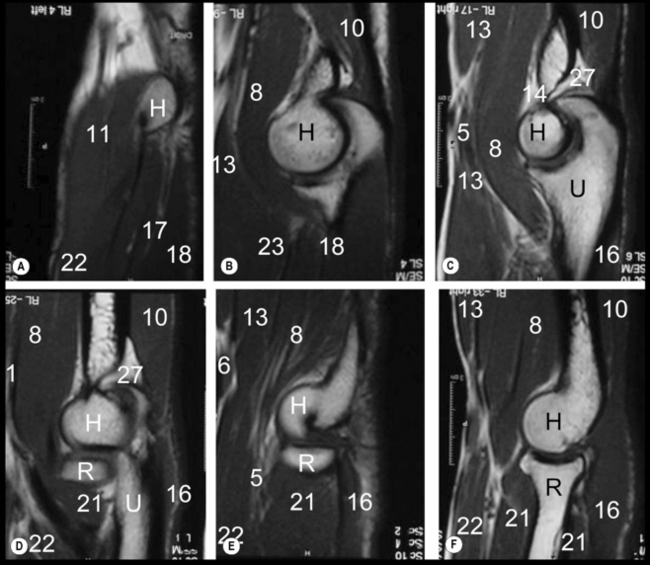
The elbow is a complex articulation in both structure and function1 and this demands from the clinician a detailed knowledge of the normal anatomical relationships, whether treating clinically or interpreting diagnostic imaging. It is worth reviewing these before proceeding further; this can be done by studying Figures 9.01 and 9.02.
However, diagnosis of elbow conditions does not begin with MR imaging. As with any other area of the body, an appropriate history and physical examination cannot be replaced by any diagnostic imaging modality. Not only do these establish a differential diagnosis that determines the necessity for and type of imaging required, but also it allows for clinical correlation of any pertinent findings.2
History and examination
Whenever the clinician is assessing a patient presenting with pain in or around the elbow, their evaluation should include the whole of the associated kinematic chain: hand, forearm, arm, shoulder and cervicothoracic spine. The contralateral elbow should also be considered for both comparison and evidence of compensation, which as well as indicating the level of disability can also determine the onset of adaptive injury.3
When taking the patient’s history, in addition to the customary questions, there are some key points that will help direct the physician to the most appropriate differential diagnoses. These are detailed in Box 9.01.
Box 9.01 Historical considerations for a patient presenting with elbow pain
Differential diagnosis
Mentally dividing the elbow into four regions is a valuable exercise, and assists both in constructing an initial differential diagnosis and in determining the imaging appearance. Each of the quadrants can be associated with specific pain-generators, pathologies and, to a certain extent, mechanisms of injury (Table 9.01); of course, disorders such as loose body formation or significant trauma may cause pain in any location.
Table 9.01 Structures and pathologies associated with different quadrants of the elbow
| Structures | Pathologies |
|---|---|
| Lateral quadrant | |
Correlating the localization of the pain to the timing of the complaint may help to further refine the diagnostic list. For example, pain at the anterior aspect of the elbow during the early cocking phase of a throw may be consistent with biceps tendonitis.4,5 Likewise, a tendinopathy involving the flexors and pronator teres will most likely manifest as anterior-medial pain during the late acceleration phase of a throw where forearm pronation and wrist flexion are maximal.6
These examples are specific to sports such as baseball, rounders or cricket, which involve throwing. The structures of the elbow are also specifically solicited during sports such as tennis,7–12 badminton,12–14 golf,12,15–18 squash/racquetball12,19,20 and basketball.21,22 Occupational injuries at the elbow are also frequent: ask any construction worker, musician or computer enthusiast!23–28 In addition, the forearm also becomes very active in compensation for shoulder or core deficiencies.15,29,30
Clinical indications for diagnostic imaging
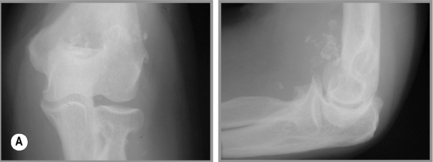
The initial imaging modality for the elbow remains plain film radiography: it is useful, widely available and inexpensive. Many projections are available and demonstrate the osseous anatomy well. The standard examination protocol involves an anteroposterior (AP) view with the forearm in supination and a lateral view, taken with the elbow in 90° of flexion and the forearm in neutral (i.e. without pronation or supination).31,32 A medial oblique view with the forearm in pronation is the most common supplementary view. Depending on the clinical question, projections specifically designed for the olecranon and the radial head are also commonly taken and can be very useful.31,32
Ultrasonographic evaluation of the elbow is becoming more and more popular. There is minimal bony interference in the elbow area, allowing for a good acoustic window. The tissues evaluated are also relatively superficial.33,34 Ultrasound examination can also be performed in real time and in a dynamic fashion with immediate patient feedback and localization of the region of complaint.35 The evaluation of the ulnar nerve in a patient with cubital tunnel syndrome, chronic epicondylitis or bursitis may be much more convenient and cost-effective with this modality than with MR imaging.36–42
Ultrasonography is also quite popular for the evaluation of the paediatric patient, since the use of MR imaging in young children can be quite problematic. In order to ensure compliance and decrease motion artifacts, it is often necessary to sedate children for the relatively lengthy MR image acquisition time. This process increases the invasiveness of the MR technique, and is why ultrasonography may be preferentially chosen as the imaging modality of choice in the paediatric population.43,44
Although radiographs and ultrasound may be used to determine the source of pain and functional deficit, MR imaging remains unsurpassable for many conditions because of the high soft tissue detail and bone marrow information it provides; however, this information may not always be necessary – many elbow conditions may be diagnosed clinically without any imaging and treated conservatively with great success. Approximately 90% of patients with an epicondylitis recover well without surgery.45 MR imaging or ultrasonography may only be appropriate for the remaining patients that do not respond to conservative care.46
Trauma
Trauma often necessitates MR imaging of the elbow in both the acute setting as well as the chronic situation such as the repetitive stresses experienced in sports activities, especially those involving a racquet.46,47 Chronic trauma may also arise from a complication of an acute incident where the patient continues to be affected by symptoms long after the precipitating event. Patients with persistent elbow symptoms related to sports may develop scar tissue, tendinous degeneration, partial or complete tears of the tendons, or articular changes, all of which can preclude a rapid or complete recovery.19,46
Those patients suffering from persistent elbow symptoms may be harbouring complications such as avascular necrosis or loose body formation resulting from an osteochondral injury. In such cases, MR imaging can determine the most appropriate clinical management of the patient, providing a wealth of information as to the size and position of the lesion and any associated fragment.48–51
In the acute trauma setting, there are also situations that may require planar imaging such as MR; in particular, dislocations and complex fractures. Patients sustaining posterior dislocations of the elbow are at risk of associated ligament and capsular tears, avulsion fractures and instability. In the case of fractures, MR imaging is not always needed for purposes of identification, but can be vital in determining the management and prognosis.52 When a simple radial head fracture is identified on plain film, the treatment plan is usually straightforward: initial immobilization and early rehabilitation to avoid capsular restriction, particularly into extension. No advanced imaging is normally performed; however, the management and prognosis of comminuted fractures is often based on the associated injuries as opposed to the fracture itself. In these instances, cross-sectional imaging becomes indicated.
MR imaging of the elbow may also provide important information regarding the neural elements that pass by the articulation during their course into the forearm and hand. The radial, median and ulnar nerves follow complicated pathways and are prone to entrapment in multiple locations by a wide variety of causes such as injury, mass compression or developmental variants.53–56 Surgery may also provoke scar tissue formation about the nerves, leading to adhesions, irritation, entrapment and, eventually, chronic denervation.57,58 In such syndromes, the use of MR imaging can be useful in determining the extent of any neuropathy and associated denervation and evaluating the potential for recovery. Clinical examination, electromyography and nerve conduction tests are also essential parts of the work-up, allowing for both the structure and function of the involved neural structures.
Techniques and protocols
Imaging of the elbow has benefited greatly from technological developments; in particular, high field strength magnets (1–3 T) and better surface coils have improved the speed and quality of the images.59 MR imaging of the elbow involves the patient lying in the supine position with the arm resting against the body. A surface coil, wrapped around the patient’s elbow, is used to improve the final image quality. With the patient in this position, motion artifacts are minimized.60
If there is clinical suspicion of a lesion to the distal biceps tendon or median nerve, the ‘FABS’ position (flexed elbow, abducted shoulder, supinated forearm) may be utilized to obtain a longitudinal view of the tendon and nerve. In this instance, the patient lies prone on the MR table with the involved arm overhead, the elbow flexed to 90° and the forearm supinated with the thumb pointing upwards. MR imaging can also be performed on a patient wearing a cast but, since the arm is sometimes fixated in an odd flexion position, it may cause difficulties in patient positioning. The cast also adds bulk, making the use of a standard elbow coil difficult.61
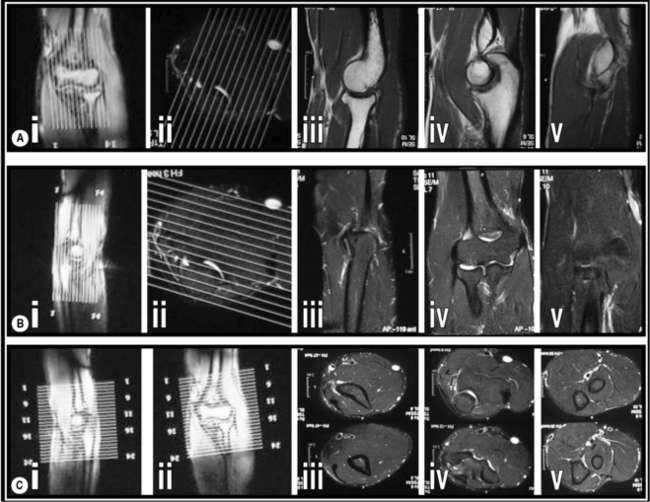
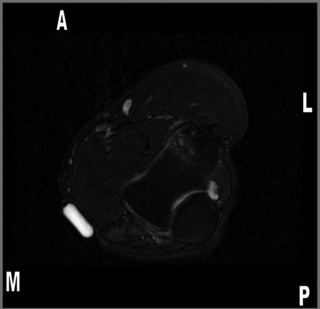
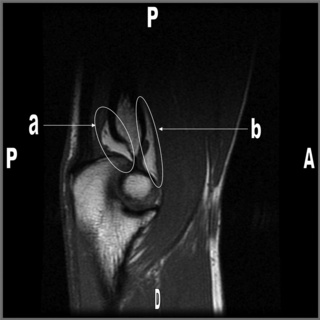
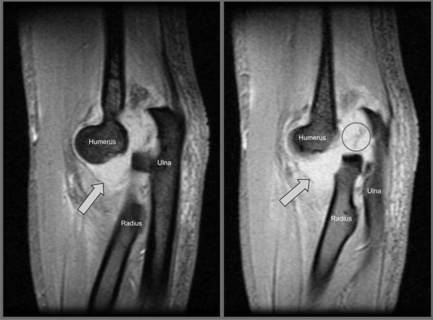
When possible, the three planes of interest are all included: axial, sagittal and coronal, maximizing the three-dimensional visualization of anatomical structures. The images are usually obtained with 4-mm slices and a 10% (0.4-mm) gap to prevent cross-talk (Figure 9.03). Since not all the aforementioned sequences are necessarily performed on a routine scan, it is always helpful to provide the radiographer and radiologist with the clinical findings and diagnostic suspicions, so that the appropriate parameters can be applied.62 Another useful trick that may be utilized when looking for a specific problem is to tape a capsule of vitamin E on the skin of the patient, adjacent to the area of complaint. This will serve as a marker to indicate the problematic region on the images and can be seen on the final image as a round, or oval, area of high signal focus lying on the patient’s skin (Figure 9.04).63
On occasion, intravenous contrast may be added, particularly if the clinical question involves the identification of a mass or the evaluation of an active, synovial-based disorder. MR arthrography is limited to assessing undersurface collateral tears or finding intra-articular loose fragments. The use of contrast carries risks and increases the invasiveness of the technique. The decision as to whether contrast is appropriate and, indeed, the most appropriate investigative protocol is based largely on the nature of the structure(s) under investigation (Table 9.02).64,65
Table 9.02 Optimum sequences for the visualization of different structures
| Bone and marrow | STIR in all three planes |
| Articular cartilage | STIR and gradient echo, Proton Density Fat Saturated coronal/sagittal planes |
| Ligaments | STIR in the coronal plane |
| Tendons | T1-weighted and STIR in all planes |
| Nerves | T1-weighted and STIR in the axial plane |
Normal imaging anatomy
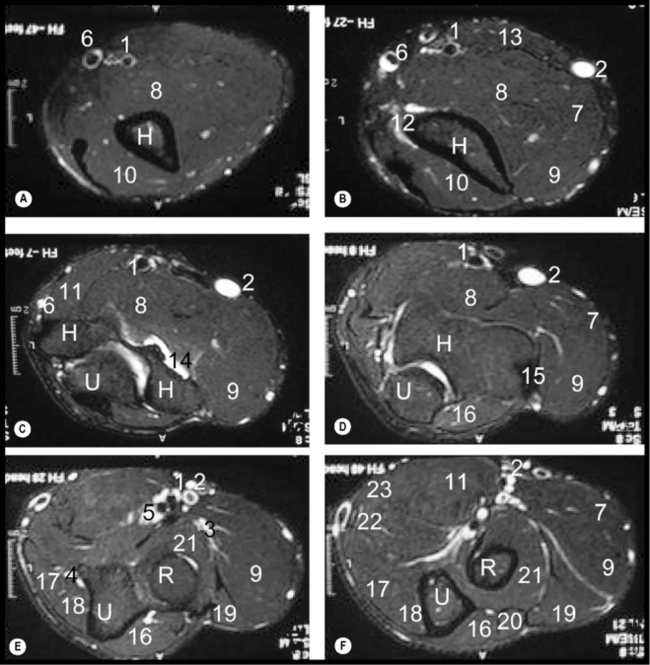
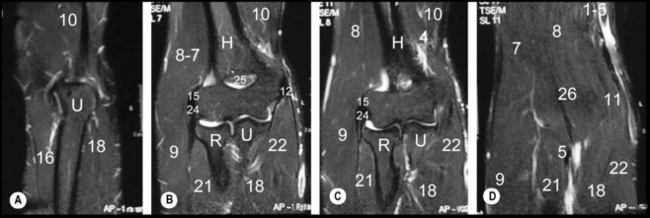
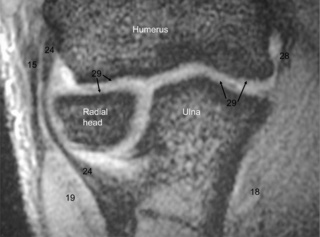
Osseous anatomy (Figures 9.05–9.07, Box 9.02)
The elbow is a compound, hinge-type synovial joint (ginglymus) composed of the distal humerus, proximal ulna and proximal radius (Figures 9.01, 9.02).66
On the distal humerus, there are two prominent processes, the medial and lateral epicondyles. The distal articular surface of the humerus is wide and flat. The lateral third, the capitellum, articulates with the head of the radius, which has a disc-shaped articular surface. The medial third, the trochlea, articulates with the trochlear notch of the ulna.67
This notch, which is large and C-shaped, is also sometimes termed the semilunar notch. The projection forming its upper border is called the olecranon process. It articulates with the posteriorly situated olecranon fossa of the humerus and may be palpated as the angular ‘point’ of the elbow. The projection that forms the inferior border of the trochlear notch, the coronoid process, enters the coronoid fossa of the humerus when the elbow is flexed. This fossa is separated from the cubital fossa anteriorly by only a thin layer of bone.68
The lateral side of the coronoid process has a small, shallow notch or groove, called the radial notch. This articulates with the head of the radius, forming a synovial pivot (trochoid) joint, which allows supination and pronation of the forearm.69 On the medial aspect of the coronoid process, approximately 2 cm posterior to the coronoid tip, is the sublime tubercle, the site of insertion for the ulnar collateral ligament.70
Nerves
Nerves are distinguishable on MR imaging owing to their surrounding layer of fatty myelin. The median, radial and ulnar nerves are usually obvious on axial images of the elbow (Figure 9.05E); however, they can be difficult to identify owing to their size, variable anatomical relationships and low signal intensity. They have complex courses, running through multiple compartments.
Ulnar nerve
Of the three, the ulnar nerve is the most vulnerable to injury, probably because of the superficial position that the nerve takes as it passes through the joint. The elbow is also the most common site for traumatic injury to the ulnar nerve, particularly where it passes through the cubital tunnel.53,69 The tunnel floor is made from the posterior and transverse portion of the ulnar collateral ligament (or medial collateral ligament of the elbow) as well as the articular capsule. The aponeurosis of the flexor carpi ulnaris muscle and the cubital tunnel retinaculum create the roof of the tunnel. This retinaculum, sometimes called the arcuate ligament, runs from the olecranon to the medial epicondyle and is not present in everyone.1 In some individuals, it is replaced by an accessory muscle, the anconeus epitrochlearis, which offers an additional site of potential entrapment and compression of the ulnar nerve.71,72
Median nerve
The median nerve may be better identified if the patient’s forearm is placed in pronation during imaging.73 If there is a clinical question regarding this nerve, it is thus wise to impart this information to the radiologist.
In the region of the elbow, the median nerve travels between the bicipital aponeurosis and the brachialis muscle, through the cubital fossa. The median nerve gives off its anterior interosseous branch just after passing between the two origins of the pronator teres muscle, as they arise from the medial epicondyle and coronoid process, offering a potential site of entrapment. If this pathology occurs before the separation of the nerve into its distal branches, it is termed pronator syndrome. If the entrapment occurs after the separation, it is referred to as anterior interosseous nerve syndrome.69,74,75
Radial nerve
The radial nerve can be found in the anterolateral portion of the elbow region, between the brachialis and brachioradialis muscles. It divides into two branches: the superficial sensory branch passes between the supinator and brachioradialis muscles, maintaining the title of the radial nerve, while the purely motor posterior interosseous nerve forms at the level of the capitellum and courses between the heads of the supinator muscle, in a fibrous tunnel named the arcade of Frohse.66,69,75
Muscles and bursae
Anterior
The group of muscles that contribute to the soft tissue structures anteriorly comprise the biceps brachii and brachialis. The two proximal heads of the biceps brachii unite to form a common tendon above the elbow that inserts on the radial tuberosity. The tendon anchors into the bicipital aponeurosis (or lacertus fibrosus). The brachialis muscle lies deep to the biceps brachii. It originates from the distal half of the anterior humerus and inserts onto the coronoid process.66,68 Both muscles are best seen on axial and sagittal images (Figures 9.05 and 9.07 respectively).
The bicipitoradial and interosseous bursae separate the extrasynovial, paratenon-wrapped distal tendon of the biceps from the anterior aspect of the radial tuberosity.68 The bursae are not normally visible on MR images, unless they have become inflamed and/or distended.
Posterior
The muscles contributing to the posterior elbow group are the anconeus and triceps muscles.76 The axial and sagittal sequences are the most useful to assess both these muscles (Figures 9.05 and 9.07 respectively). The anconeus is a small, triangular muscle that originates on the posterior aspect of the lateral epicondyle and inserts on the posterior superior surface of the ulna.76 Although it assists the (postero-) lateral ulnar collateral ligament (LUCL) in resisting varus stress, since it blends with the triceps distally, it is often considered as functionally part of this muscle.68 The triceps attaches to the posterior surface of the olecranon process and it is at this site that the tendon’s fibres become intertwined with fibrofatty slips that may be radiologically mistaken for a partial tear. This phenomenon will appear as an increased signal on both T1- and T2-weighted images. The olecranon bursa lies between the triceps tendon and the olecranon.69
Medial
The medial group of muscles consists of the pronator teres, the palmaris longus (when present) and the flexors of the hand (flexor digitorum superficialis and profundus; flexor carpi radialis, flexor carpi ulnaris and flexor pollicus longus).1 The pronator teres muscle is the most superficial of the group. It has two origins: from the medial condyle (the humeral head) and from the coronoid process of the ulna (the ulnar head). The pronator inserts onto the lateral surface of the mid-third of the radius. The remaining muscles unite in the common flexor tendon, which inserts into the medial epicondyle of the humerus.76 The ulnar (or medial) collateral ligament may also be identifiable along its course. It offers supports to the common flexor tendon in resisting valgus stresses. For best visualization, one should assess the axial and coronal images (Figures 9.05 and 9.06 respectively). Normal ligaments and tendons will be demonstrated as homogeneously low signal structures inserting onto the medial epicondyle.77
Lateral
The supinator and brachioradialis muscles, along with the extensor muscles of the hand, form the lateral group of elbow muscles.1 The supinator muscle is the deepest muscle, originating on the lateral epicondyle of the humerus and inserting onto the proximal third of the radius. It contributes to the floor of the cubital fossa whilst the brachioradialis serves as the lateral boundary of the cubital fossa.68 Originating at the supracondylar ridge of the humerus, the brachioradialis inserts onto the lateral surface of the distal radius.76 The extensor muscle group originates as the common extensor tendon from the lateral epicondyle. The tendon is common to extensor carpi radialis brevis and carpi ulnaris and to extensor digitorum and digiti minimi. The extensor carpi radialis longus is part of the lateral group but originates slightly more proximally on the lateral condyle of the humerus.69 The axial and coronal images are again the best to visualize the lateral compartment muscles (Figures 9.05 and 9.06 respectively).
Ligaments and capsule
The articular capsule of the elbow extends from the humerus, covering all the articular surfaces down to the radial neck and inferior aspect of the coronoid process of the ulna. It is weaker on its anterior and posterior aspects, the medial and lateral aspects being strengthened by the medial and lateral collateral ligament complexes.68 The anterior and posterior fat pads may be seen on lateral radiographs of the elbow joint as well as on MR imaging. Normally, with the elbow in a flexed position, the anterior fat pad is visible on radiographs as a relatively linear lucency in contact with the anterior aspect of the distal humerus. The posterior fat pad is not normally visible as it is hidden deep within the olecranon fossa. Articular oedema from effusion, haemarthrosis or synovitis will cause these fat pads to be displaced away from the humerus, resulting in radiographic visualization of the posterior fat pad and anterosuperior elevation of the anterior fat pad which adopts a curvilinear configuration.78 The fat pads are visible on MR imaging, particularly on T1-weighted or fat-sensitive sagittal sequences (Figure 9.08).
The ulnar collateral ligament (UCL) complex contributes to medial elbow stability (Figure 9.01A). It comprises three distinct bundles: the anterior, posterior and transverse portions.69 The anterior bundle extends from the medial epicondyle to the coronoid process and is best seen on coronal images (Figure 9.09).65,68 Its proximal aspect is flared and tapers distally; it is the principal restraint against valgus stress.79,80 The posterior fibres extend from the medial epicondyle to the olecranon. The transverse (or oblique) portion extends from the olecranon to the coronoid process and does not really contribute to stability of the joint. The posterior and transverse portions are not always present, but this is rarely an issue from a biomechanical or clinical standpoint.68 They are difficult to see on MR images; however, their presence is inferred as they form the floor of the cubital tunnel.81
The radial collateral ligament complex includes the lateral collateral ligament (LCL), the annular and accessory collateral ligaments and the LUCL (Figure 9.01B).68 It contributes to the lateral stability of the elbow and resists varus stress.82,83
The LCL extends from the anterior aspect of the lateral epicondyle and inserts into the annular ligament and supinator fascia. The posterior bundle, the LUCL, extends from the lateral epicondyle and inserts into the ulna (hence the name) at the crista supinatoris.68 The LUCL is the prime restraint against varus stress and its disruption will severely diminish the stability, leading to posterolateral rotatory instability of the elbow.83,84 This ligament is best seen on coronal images. The better-known annular ligament is the prime stabilizer for the proximal radioulnar joint69 and is best assessed on axial slices (Figure 9.05).65
Normal variants and diagnostic pitfalls
Osseous variants
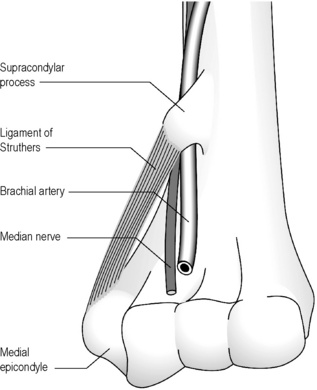
Most commonly asymptomatic, the supracondylar spur (or process) and its associated ligament are found in approximately 1% of the population. The spur, which is located on the anteromedial surface of the humerus, 5–6 cm above the epicondyle, can be rudimentary and tubercle-like or quite large.85 The ligament of Struthers connects the bony outgrowth to the medial epicondyle, forming the supracondylar foramen or arcade of Struthers. The median nerve and branches of the brachial artery run through the foramen (Figure 9.10). In some cases, the arcade can be the site of an anomalous origin of the pronator teres muscle.86–88 These close anatomical relationships can account for the symptoms that may be experienced by some patients and will be addressed along with the other causes of median nerve entrapment.
This variant is easy to visualize on plain film radiographs, especially if the arm is in a slightly oblique position. The spur will point towards the elbow joint, as opposed to its principal differential diagnosis, the osteochondroma, which points away from the joint. Although location and appearance are key to distinguishing the two, MR imaging demonstrates the cartilaginous cap in a developing osteochondroma.86
Two accessory ossicles are known to occur about the elbow joint: the os supratrochleare and the patella cubiti. The os supratrochleare is a developmental ossicle believed to originate from an accessory ossification centre of the olecranon. When present, it is located within the joint capsule in the olecranon fossa. It may restrict extension or can be asymptomatic. Because of its intra-articular position, it may benefit from synovial nutrition and increase in size. Its shape may be altered by the battering received from the adjacent olecranon. It is most common in the dominant arm of males.89,90
The patella cubiti is a rare sesamoid bone found in the tendon of the triceps, mimicking the patella in the quadriceps tendon. It may also be asymptomatic or cause restriction in the extension range of motion.91
Muscular variants
The biceps brachii provides a good example of this. Although the name of the muscle suggests the unvarying presence of two heads, the biceps can in fact possess anywhere between one and five heads. A third head is found in some 10%–20% of the population,92,93 so is not in any way a rarity. As long ago as 1875, the anatomist Macalister published a review of 48 different variations for the morphology of the biceps,94 and more have been reported since.95–99 Another example of relatively frequent variation is the brachioradialis muscle, which may be conjoined with the supinator. Alternatively, its tendon may be split into different slips and cause entrapment if the radial nerve passes between them.75
Paediatric considerations
Until recently, it was customary to obtain radiographs of the uninvolved arm; however, the increased exposure to ionizing radiation of developing tissue is no longer considered acceptable on a routine basis. On plain film, it is difficult on occasion to differentiate between a newly ossified centre and a fracture fragment. Fortunately, the ossification process follows a predictable order, for which the acronym CRITOE or CRITOL may be used in order to remember its sequence (Table 9.03).
Table 9.03 Ossification centres for the elbow in order of appearance: the CRITOE acronym
| Structure | Approximate age of appearance |
|---|---|
| C apitellum | 1 year |
| R adial head | 3 years |
| I nternal (medial) epicondyle | 5 years |
| T rochlea | 7 years |
| O lecranon process | 9 years |
| E xternal (lateral) epicondyle | 11 years |
The capitellum is the first such centre to become ossified and therefore radiologically visible; this happens towards the end of the first year of life. This is followed at approximately 2-yearly intervals by the radial head, medial (or, for acronymic purposes, internal) epicondyle, trochlea, olecranon process and, lastly, the lateral (external) epicondyle. These centres are usually completely fused by 16 years of age.100,101
Osseous conditions
Osteochondral injuries
These lesions, formerly referred to as osteochondritis dissecans, are classically seen in the femur and talus; nevertheless, the elbow may be also affected, especially at the capitellum.102–105 Rare reports of trochlea, radial head and olecranon process lesions have also been published.102,106,107 The condition is defined as a subchondral reaction in the bone that may lead to osteochondral fragment formation and articular deformity as the overlying cartilage collapses in to the area of osseous destruction.108
Adolescent males are most commonly affected, shortly before the point when the epiphyseal growth plate fuses.109,110 A history of athletic activity suggesting acute trauma or chronic overuse may be present; yet, in some cases, the history may be unremarkable.109,111 Athletes who participate in throwing events or gymnasts should be monitored closely when developing elbow pain as the constant valgus stress created by impaction accentuates the stress on the lateral aspect of the elbow.107,112 Patients may present with pain, tenderness and swelling, particularly in the lateral soft tissues surrounding the joint. Catching or locking sensations are suggestive of the presence of a loose fragment.109,113
It is important to clarify the terminology before moving on. There is much confusion between the terms ‘osteochondritis dissecans’, ‘Panner’s disease’ and ‘osteochondrosis of the capitellum’. Some authors utilize the terms interchangeably; some others establish them as different entities, although the evolution and pathophysiology of the processes are not well understood. Regardless of these semantic differences, most authors agree on this: the term ‘osteochondritis’ is undesirable owing to the inconsistency of inflammatory markers in this condition.109,113,114 When considered as separate entities, Panner’s disease is described as a condition affecting younger children (aged 5 to 11 years) which does not lead to loose body formation or residual deformity. For others, the conditions are linked and part of the continuum of osteochondrosis, wherein Panner’s disease would represent an early phase of the spectrum.115–118 Here, the terms ‘osteochondrosis’ (to identify the condition) and ‘osteochondral defect’ (to define the sequelae) will be used.
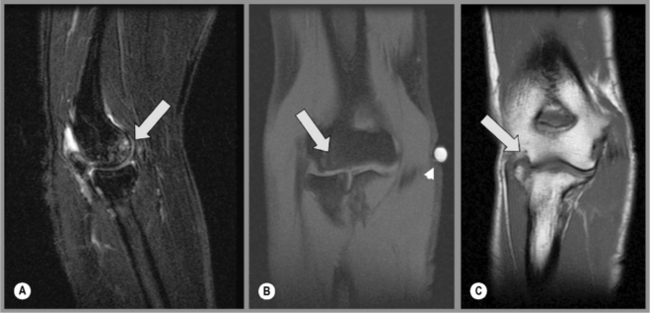
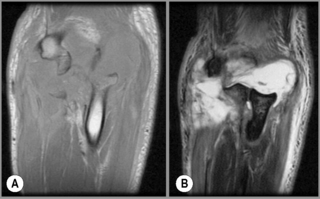
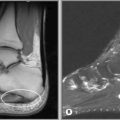
Although radiographs remain the initial evaluation method of choice for osteochondrosis, the use of MR imaging is increasing owing to its sensitivity and the aid that it provides in determining the prognosis and, thereby, patient management. MR imaging is definitely superior to plain film radiography in detecting early osteochondral defects (Figure 9.11).64,104,119,120
In the early stages, plain film radiology may appear normal or show only subtle density changes. Flattening of the articular surface and fragmentation of the subchondral bone may be observed as the condition progresses. Free fragments may be observed in the later stages, often lodged in the coronoid or olecranon fossae.109
MR imaging can demonstrate significant abnormalities, even when radiographs are normal. Signal changes can be observed on most sequences. Fat-suppressed T2-weighted images will demonstrate a focal increase in signal intensity in the subchondral region of the capitellum. On the T1-weighted sequences, focal areas of either low signal intensity surrounding a more intermediate signal area or of homogeneous low signal intensity correspond to the involved area (Figure 9.12). If fragments are present, these will be of the same intensity as the native bone, and are easier to locate if surrounded by joint effusion. MR imaging is also superior in assessing the size, location, displacement, stability and viability of any fragment, all of which are factors in treatment and prognosis determination.63,64
A high intensity zone surrounding the fragment on both T2-weighted and post-contrast T1-weighted images is a sign of instability of the fragment, suggesting that surgical intervention may be required. Imaging enhancement of the fragment with contrast is considered a positive sign suggesting adequate blood supply and viability. Timely detection may therefore determine the most appropriate management protocol, providing a better outcome for the patient.64,110,121
Early or stable lesions respond well to conservative treatment, mainly the discontinuation of the aggravating activity. The cessation or serious limitation of activity is imperative for a successful outcome. The prognosis for the condition also depends on the age of the patient and the severity of the original lesion. Unstable lesions, where an isolated fragment is present, usually necessitate surgical management. The principal long-term complication in osteochondrosis is degenerative joint disease.122
A normal variant may mimic the presentation of osteochondral defects in the elbow. Occasionally, the junction of smooth articular cartilage of the capitellum and the rough, non-articular cartilage on the posterior aspect of the lateral epicondyle may form a groove and simulate a bony defect. This appearance is referred to as the ‘pseudodefect of the capitellum’. The location on the posterior side is the key to recognition along with recognition of the continuity of the cartilage interface and lack of underlying osseous change.110,123
Bone injuries
MR imaging is not usually necessary to initially detect the majority of elbow fractures; however, MR imaging is superior to radiography in the evaluation of occult fractures, stress injuries and bone contusions, which may significantly affect both prognosis and management.78,123 Fat-suppressed T2-weighted images are considered the most sensitive but least specific images for their detection of these often subtle osseous conditions.64
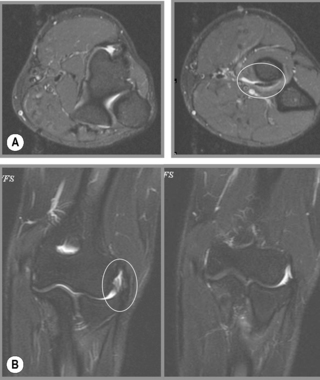
Fractures are demonstrated as a linear pattern of increased T2-weighted and decreased T1-weighted signal intensities. Signal changes associated with bone bruises are typically more diffuse, visible as a large region of increased signal intensity on fluid-sensitive sequences, affecting the subchondral bone and bony marrow about the site of the injury (Figure 9.12).64
MR imaging is also the best modality to evaluate the inevitable soft tissue injuries associated with fractures and determine their effect on both the clinical management and the prognosis of the trauma. For example, radial head fractures are often associated with disruption of the lateral and medial collateral ligaments. The damage to the soft tissues and the small fragments cannot be seen on plain film radiographs.124,125
Assessing damage to the growth plate and developing articular cartilage can also be performed using MR imaging. This makes the modality particularly useful for assessing traumatic injuries in the paediatric patient, notwithstanding the difficulties in imaging younger patients discussed above. The prognosis and management of growth-plate (Salter–Harris) injuries is greatly influenced by the location of the damage, making an accurate description of the injury a high priority. MR imaging offers an important advantage since the ossification centres of the distal humerus are not well seen on plain film radiographs. However, this benefit has to be clinically weighed against the risks of sedation in this population, often necessary to ensure image quality.64,110,123
Certain sites within the elbow are more prone to fractures than others; the most common location of fracture in adults is the radial head.78 The mechanism of injury always involves some form of axial overloading, such as falling on an outstretched hand (FOOSH).126 The ‘FOOSH’ mechanism may also be responsible for injuries throughout the upper extremity: fractures at the distal radius (Colles’ fracture), capitellum or the scaphoid as well as dislocations of the wrist, elbow or even glenohumeral joint. It is also a frequent cause of ligament ruptures, especially of the ulnar collateral ligament.78,127
When examining a patient with a suspected radial head fracture, it is therefore of the utmost importance to assess the rest of the upper extremity to explore the possibility of comorbid damage.3 With conventional radiographic evaluation of radial head fractures, it is imperative to look for the anterior fat pad ‘sail sign’ or the elevated capsular fat plane posteriorly, both of which indicate capsular oedema and are very closely associated with radial head fractures, even in the absence of overt findings.128 If the fracture is radiographically occult on plain films, MR imaging can confirm the presence of a fracture by demonstrating effusion, marrow oedema and the actual fracture line.
In adults, the anterolateral aspect of the radial head is especially vulnerable to injury because it lacks subchondral bone.129 By contrast, in children, fracture of the radial neck is more common, though the morphological appearance is similar.130 The degree of comminution is important to assess in all fractures of the proximal radius as it is one of the most important factors in the long-term prognosis. When the fracture is not well visualized on plain film radiography, MR imaging may be indicated.131
Fractures of the coronoid process of the ulna are distraction injuries caused by the avulsion of the brachialis muscle from dislocation or hyperextension. They can occur in conjunction with or independently from fractures of the radial head. If seen together, they are likely the result of a posterior dislocation caused by a FOOSH.132 When associated with a sprain of the ulnar collateral ligament, they form the ‘terrible triad of the elbow’, invariably challenging from a management standpoint.133,134
Fractures of the medial and lateral epicondyles are both most commonly avulsion injuries caused by contraction of the flexor or extensor/supinator muscle groups respectively. Direct impact, creating varus or valgus stress, may also be a cause. MR imaging is helpful once again to determine the degree of comminution and damage to the adjacent articular cartilage. Complex fractures will most likely be managed surgically.135,136
Dislocations
The elbow joint is the second most commonly dislocated joint in adults (following the shoulder). In children, it is the commonest site of such injuries and the mechanism of injury is usually traction.78,123,137 This is referred to technically as radial head subluxation, and colloquially as ‘pulled elbow’ or ‘nursemaid’s elbow’ referring to the frequent presentation whereby a parent (or nursemaid) has jerked or pulled a small child’s arm whilst holding hands; the injury is usually inadvertent. It may be reduced successfully in most cases without any requirement for imaging. In adults, a FOOSH or forced hyperextension is the typical cause of this injury and the situation is usually rather more complex.138–141
The ulna and radius can dislocate together or individually. Because of the requirement for pronation and supination, they are closely approximated in all movements. This nature of this closed kinematic chain means that when significant trauma is detected in one area of the chain, the remaining components should be carefully scrutinized to eliminate collateral injury.29,142 Classical examples of this phenomenon include the Monteggia fracture-dislocation (radial head dislocation associated with an ulnar fracture) and the Essex-Lopresti injury (a comminuted, displaced fracture of the radial head with dislocation of the distal radioulnar joint).78
These injuries are usually quite evident both clinically and with conventional radiography. The utility of MR imaging mainly resides in the assessment of the adjacent soft tissue damage, underlying osseous complications and surgical planning (Figures 9.13–9.16). In particular, small fractures and capsular disruptions missed on plain film may be linked to residual instability.125 Other injuries associated with dislocation are contusions at the anterior coronoid process, radial head and posterior capitellum; musculotendinous strains involving the brachialis muscle; ligamentous and capsule sprains; and neurovascular damage.143
Ligamentous trauma
The ulnar and radial collateral ligament complexes, as well as the capsule, can all be well evaluated with MR imaging. Damage to the collateral ligaments is a common, sports-related, chronic stress injury. It may, however, also occur following acute events such as dislocation.136,143
On plain film radiographs, subtle soft tissue densities corresponding to avulsed fragments adjacent to the involved epicondyle and gapping of the joint may be the only sign of injury. Any gapping may be accentuated on stress radiographs.78 By contrast, MR images may demonstrate signs of acute or chronic ligamentous sprain: increased signal in or surrounding the ligament on T2-weighted images, representing oedema or haemorrhage; thickening or thinning of the ligament and waviness, laxity or discontinuity of the fibres (Figure 9.17). Ligamentous ruptures will be demonstrated by discontinuous fibres and abnormalities of the surrounding signal.143–145
Ulnar collateral ligament
Ruptures of the UCL are usually an acute occurrence, whereby the patient experiences sudden pain, which may be associated with a popping sensation. They most often occur during sports involving throwing.145 For most ordinary beings, the treatment will be conservative – the flexor-pronator muscle group will be sufficient to stabilize the elbow. In elite athletes, surgical reconstruction may be attempted in order to allow further pursuit of the sport of choice.80,146
The aetiology of the injury may, however, be chronic, arising from repetitive valgus force – typically from throwing activities – placing a high amount of stress on the UCL. Over time, these stresses lead to repeated microtrauma, inflammatory changes, weakening and eventually rupturing of the ligament. Clinically, this may present as medial elbow instability. By far the most common site for tears of the UCL is the mid-substance of the anterior bundle of the ligament.80 Avulsions of the proximal attachment (3% of cases) or distal attachment (10% of cases) site have also been reported.147,148 Chronic degeneration with thickening of the ligaments over time may lead to radiographically visible calcific changes or heterotopic bone formation, similar to that found in Pellegrini–Stieda disease in the medial collateral ligament of the knee. In patients who have undergone repetitive valgus stress, a characteristic osteophyte may be present at the insertion of the UCL on the coronoid process.80
Radial collateral ligament
Injuries to the radial collateral ligament may occur in acute traumatic events such as a FOOSH, causing hyperextension along with a varus stress, or as a result of chronic epicondylitis, causing lateral epicondylar soft tissue degeneration and tearing of the common extensor tendon.48 Rotational instability may be present but difficult to elicit if the patient is guarding.82 On MR images, as with other ligament tears, there will be discontinuous fibres with adjacent signal irregularities (Figure 9.18). Posterolateral rotatory instability, as seen with lateral ulnar collateral ligament (LUCL) incompetence, will result in a rotary subluxation of the humeroulnar joint and subluxation or dislocation of the radiohumeral joint. This pattern of instability may also be secondary to a surgical lateral extensor release.149
Tendinous injuries
Although uncommon injuries, biceps and triceps tendon tears can be assessed with MR imaging, which can confirm the rupture and distinguish between complete and partial tears as well as excluding differential diagnoses.123,149 Rupture of the biceps tendon typically occurs acutely in middle-aged men. If it occurs distally, it will arise near or at the insertion site on the radial tuberosity.144,150,151 On MR imaging, the low signal intensity of the tendon will be absent on axial images.123,143 The T2-weighted images will show high signal intensity corresponding to oedema in the antecubital fossa (Figure 9.19). Retraction of the tendon fibres may be observed on the sagittal images. The amount of retraction is usually linked to a concomitant injury to the bicipital aponeurosis (lacertus fibrosus).
Tendinopathy and partial tears are also common. In both chronic and acute injury, thinning of the tendon may be seen; however, on occasion, the tendon may also appear thickened. In the acute scenario, this is due to the oedema associated with the intrasubstance damage. By contrast, the thickening seen in chronic injury is caused by accumulated fibrosis, which will have a less intense signal on the fluid-sensitive images. Partial ruptures are also characterized by the presence of high T2-weighted signal intensity, indicating bone marrow oedema in the radial tuberosity; and presence of fluid (high T2 signal intensity) in the interosseous fossa, corresponding to associated bursitis.64,152 Low signal intensity on both T1-weighted and T2-weighted images represents osseous proliferation at the radial tuberosity, which may result from such an injury.151 Differentiation of partial tears from bicipital tendinopathy is difficult as one may predispose to the other. It is important to consider and correlate the clinical presentation to inform the differential diagnosis.
Tears of the triceps tendon, whether complete or partial, are even rarer injuries. Tears may be seen after acute incidents (such as a FOOSH injury) or from chronic, repetitive events related to sports. The MR imaging findings will be similar to those described in the biceps tendon, but will be present in or surrounding the olecranon process, with associated bone marrow changes observed on both axial and sagittal images. Small avulsion fractures may be visualized at the olecranon on MR imaging and also on the lateral plain film views.63,141
Epicondylitis
Epicondylitis of the elbow is a common clinical disorder. It involves partial avulsion of the tendons attaching to the epicondyles of the humerus.150–152 The diagnosis can be made clinically without imaging.3,44 Radiographs are classically normal but may show dystrophic calcification adjacent to the involved epicondyle, particularly if the disorder is chronic. This finding represents calcific changes or heterotopic bone formation in the adjacent tendons.153 MR imaging may, however, demonstrate characteristic findings when the study is performed to rule out concomitant or mimicking injuries, especially in the case where there is inadequate resolution of symptoms despite appropriate care. MR imaging may also assist in surgical planning to evaluate the presence of associated tendinous tears.141,150,151
MR imaging findings will be similar in both medial and lateral epicondylitis and pathology is usually seen best on coronal images, which can demonstrate a range of changes, from a mild thickening of a tendon through to a partial interstitial tendon tear or complete avulsion with tears of the adjacent collateral ligament.142,150,152
The signal intensity within and about the involved epicondyle may be increased on T2-weighted, fat-saturated T2-weighted and inversion recovery sequences, consistent with localized bone and soft tissue oedema (Figure 9.19). Tendons normally display homogeneous low signal intensity on all sequences. In epicondylitis, thickening and increased signal intensity will be seen in the substance of the tendon on T1- and T2-weighted images, most often 1–2 cm below the attachment. Complete tears will be demonstrated by a lack of continuity of the tendon fibres. Paratendinous oedema (on high T2-weighted signal) is also commonly seen.141,151 It is important to be aware of recent therapeutic corticosteroid injections, as they may also cause this appearance. Signal changes in the tendon also seem to be chronic and persist after the regression of the symptoms. Associated abnormalities in signal intensity may be visualized in the surrounding ligaments and muscles, as pathology in the collateral ligaments have common mechanisms of injuries.154
In lateral epicondylitis, the primarily involved structure is the extensor carpi radialis brevis. The signal changes will be more apparent 1–2 cm below the attachment point, in the hypovascular area of the tendon.153,154 The origins of the extensor carpi radialis longus, extensor digitorum and extensor carpi ulnaris may also demonstrate changes.141,155 This condition is also commonly referred to as ‘tennis elbow’; however, most sufferers do not actually play tennis. Any sport requiring the use of a racquet may of course be predisposing, but, realistically, anyone using a hand tool repetitively is at risk (construction workers, tailors, drummers, computer users, etc.). The condition is caused by chronic varus stress where the wrist extensor and supinator muscles are overutilized.27,28,154
Patients will classically experience lateral elbow pain, particularly with resisted wrist extension (Cozen’s sign). Pain may also be present with passive wrist flexion when the elbow is in full extension. Tenderness will likely be elicited upon palpation of the conjoined tendon distal to the lateral epicondyle. If tenderness is present more distally, it may be more indicative of a radial nerve syndrome.155 Chronic, long-standing and severe lateral epicondylitis may lead to strains or tears of the LUCL and, in turn, radial collateral ligament instability.79,134,156
Medially, in ‘golfer’s elbow’ or ‘pitcher’s elbow’, the pronator teres and common flexor tendon are affected.155,157 As opposed to those with its lateral counterpart, medial epicondylitis patients usually participate in sports: golf, baseball, bowling, archery or weightlifting.17–19,143,158 They experience pain primarily on the medial aspect of the elbow and demonstrate symptoms aggravated by wrist flexion and forearm pronation. Elbow extension may also be limited. Tenderness will be elicited distally and anteriorly to the medial epicondyle around the origin of the pronator teres and the flexor carpi ulnaris.3,155 Medial epicondylitis or partial tendon tears may occur after chronic, repetitive valgus stress or acute overload. During a valgus motion, the medial aspect of the elbow is stretched and the lateral aspect is compacted; consequently, in acute cases, it is important to assess the ulnar collateral ligament for signs of tears/strain as well the capitellum for osteochondral injuries and bone contusion.141,151 In the skeletally immature patient, the stress may even lead to complete avulsion of the epicondyle (‘Little-leaguer’s’ elbow).113,121,159
Nerve entrapment
All three major nerves of the upper extremity can be trapped as they pass through the elbow and present clinically as neuropathies that need to be differentiated from more proximal and distal entrapment syndromes. Consideration will also need to be made as to the possibility of ‘double crush’ injuries; positive findings in the elbow do not remove the requirement for a full analysis of the kinematic chain as a whole.54,85,160
Compression of the ulnar nerve in the cubital tunnel (cubital tunnel syndrome) is the second most common neuropathy in the adult population (after carpal tunnel syndrome with median nerve neuropathy).28,52,54,161 Pronator (median nerve) and radial tunnel syndrome are also quite regular clinical presentations.54,55,141 The aetiology is often varied but is mostly associated with chronic overuse processes.4,120 The symptoms are variable and may be similar to those of tendinous injuries, particularly in patients with radial entrapment, which may present as a lateral epicondylitis that has been unresponsive to treatment. Long-term medial epicondylitis may also be associated with median nerve entrapments.54,141
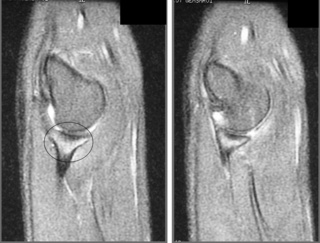
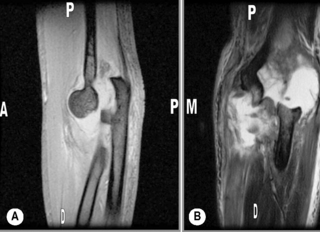
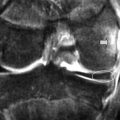
The median, radial and especially the ulnar nerve are surrounded by a layer of fat, which permits good visualization of each nerve on axial sequences.143 Inflammatory changes will be shown as heterogeneous or homogeneous increased signal intensity on T2-weighted sequences within the contours of the nerve. The diameter of the nerve may be increased around the compression site and there may be blurring of the individual fascicles (Figures 9.20–9.22). 63,142
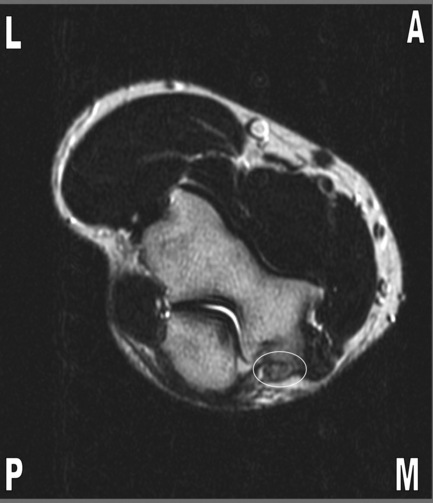
Figure 9.21 • Axial T1-weighted MR imaging of the elbow in the same patient illustrated in Figure 9.20 demonstrating thickening, heterogeneous signal intensity and irregularity of the ulnar nerve (oval) due to ulnar neuropathy.

Figure 9.22 • Coronal T2-weighted MR imaging of the elbow in the same patient illustrated in Figures 9.20 and 9.21, with fat suppression, demonstrating high (bright) signal in the ulnar nerve with associated thickening (oval) due to ulnar neuropathy. P = proximal, D = distal.
The surrounding muscular structures may demonstrate changes as well. It is important to assess the surrounding muscles for the presence of associated morphological changes such as muscle denervation or oedema (increased T2-weighted, fat-saturated T2-weighted and inversion recovery sequences), muscle atrophy and fatty degeneration (reduction in overall muscle belly size and increased T1-weighted signal). Early diagnosis and treatment offer the best prognosis, as these trophic changes may be irreversible after 6 months.63,141,142
Cubital tunnel syndrome or neuropathy is compression of the ulnar nerve in the area of the cubital tunnel retinaculum.69,156 A wide variety of causes can be responsible: developmental causes associated with an accessory muscle like the anconeus epitrochlearis72,157,158 or an aberrant triceps insertion159; a shallow cubital tunnel160; post-traumatic causes associated with malunion or non-union of fractures53,161; muscle hypertrophy162; repeated valgus stress injuries48,148; and medial epicondylitis.26,163 The clinical presentation can vary with the degree of entrapment from mild paraesthesia to severe deformation and muscle atrophy.156
The symptoms will manifest in the fifth digit and the medial aspect of the fourth digit, along the ulnar nerve distribution … exactly the same symptoms as you may have experienced if you have every hit your ‘funny bone’. It is important to elicit the presence of any ulnar nerve signs and symptoms proximal to the wrist, such as paraesthesia or weakness in the flexor carpi ulnaris muscle, as this can differentiate between ‘Tunnel of Guyon’ syndrome and more proximal entrapment of the nerve.156,164
Radial neuropathy is not as frequently seen as ulnar nerve entrapment.28,54 Depending on the compression site, it may present clinically with either sensory and motor dysfunction or a motor deficit alone (posterior interosseous nerve syndrome). There will be findings of denervation in the muscles supplied by the radial nerve and sensory disturbances in the dorsal and radial aspects of the wrist and hand.156,164 If the entrapment occurs distally, in the arcade of Frohse, there will only be muscular problems, as the radial nerve has by that time divided into a main sensory branch and the posterior interosseous branch, which supplies the supinator muscle and all the extensor muscles of the forearm with the exception of the extensor carpi radialis longus, which is supplied by the radial nerve before its bifurcation.68,75,164
In the general population, the median nerve is most often entrapped in the carpal tunnel of the wrist.88 It may, however, be compressed in the elbow region, most commonly in athletes.54,55 This occurs at the level of the pronator muscle and is termed pronator syndrome. It is also possible for the anterior interosseous branch only to be affected.165 The median nerve gives off this major branch after passing between the two origins of the pronator teres, approximately 5 cm inferior to the lateral epicondyle. The anterior interosseous nerve is a strictly motor branch supplying the pronator quadratus, the flexor pollicis longus and the radial half of the flexor digitorum profundus.74,75
Anterior interosseous nerve syndrome is demonstrated clinically as weakness of the thumb and index finger in conjunction with a complaint of proximal forearm pain. Patients with pronator syndrome generally experience an aching pain in the anterior portion of the proximal forearm and intermittent paraesthesia. Weakness or frank sensory loss is unusual.156,164 Sources of entrapment leading to a pronator syndrome are multiple, including the ligament of Struthers,55,84 muscle hypertrophy,166 aberrant muscle origins,167 and soft tissue masses.168 If there are concomitant findings in the median and radial nerve distribution, one should consider cervical radiculopathy or brachial plexitis as differential diagnoses.164
Bursitis
The olecranon and bicipitoradial bursae are not typically seen on MR imaging unless engorged with fluid. Patients will present with an antecubital mass or swelling at the posterior aspect of the elbow, depending on the affected bursa. Inflammatory conditions of the bursa can be imaged with MR and generally produce a high fluid signal intensity in the olecranon or bicipitoradial bursae on T2-weighted images and low signal intensity on T1-weighted images. The appearance of bicipitoradial bursitis, which can be insidious or present after athletic activity, is similar on MR imaging.169,170
MR is not necessary to manage bursitis in most cases; nonetheless, one must keep in mind that bursitis can be more than a reactive process at a site of high frictional stress. Inflammation of the olecranon bursa, for example, is classically seen after trauma, yet may also be present in inflammatory conditions such as rheumatoid arthritis and crystal deposition disorders such as gout.171,172 Acute osteomyelitis in children and chronic osteomyelitis in adults is often associated with infectious bursitis. Performed usually only on cases that are refractory, MR imaging shows hyperintense marrow oedema on T1-weighted and T2-weighted images and cortical destruction.173,174
Articular conditions
Synovial folds or plicae represent a thickened fold of synovial tissue, situated at the lateral aspect of the radiocapitellar joint. They are also referred to as a radiohumeral meniscus or labrum.175,176 Plicae are most commonly seen in the knee joint and are associated with chondromalacia on the adjacent articular surface.177,178 The only plain film finding in the elbow may be sclerotic changes in the radial head and capitellum. As with their main differential diagnosis (loose bodies), they can be asymptomatic, or may cause ‘snapping’ of the elbow, locking and pain in the lateral aspect of the joint line.
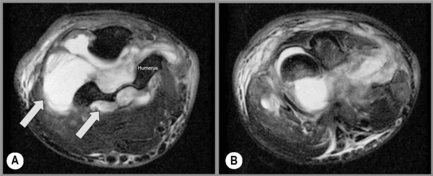
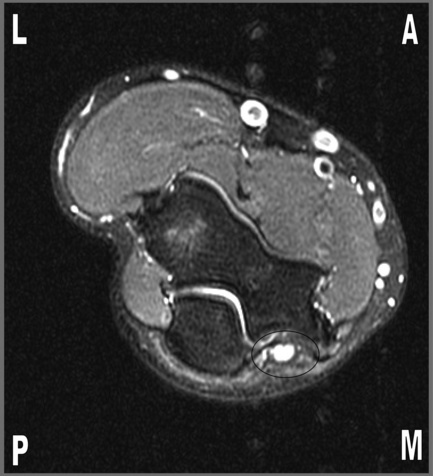
Conditions typically associated with synovial articulations, such as inflammation, degeneration or proliferation, can affect the elbow and can be visualized with MR imaging (Figure 9.23A,B).
Rheumatoid arthritis (RA) is a common, systemic arthritic condition; involvement of the elbow joint is seen in 20% to 50% of rheumatoid patients.144,179,180 The diagnosis is not usually dependent solely on imaging, but rather based on clinical criteria, which also include joint stiffness, presence of nodules and serological markers.113,181 Nevertheless, elbow involvement may cause debilitating pain and joint destruction in this condition, which begins as a proliferative synovitis and rapidly progresses to destruction of the articular cartilage and subchondral bone.182 On plain film, this is demonstrated by a loss of joint space and bony erosions.181 On MR images, thickening of the synovial membrane and associated pannus formation occurs and intra-articular fluid accumulates. An increased signal intensity from the oedematous synovium is seen, with hyperintense joint effusion. In a patient exhibiting clinical signs of rheumatoid arthritis, these are imaging signs that best confirm the diagnosis.144
Erosions, which exhibit decreased signal intensity, are radiologically visible and the pathognomonic nodules show as mixed signal intensity masses in the skin, synovium and tendons. Erosions in the cartilage and subchondral bone as well as any associated bursitis are also well visualized.183 If intravascular contrast is used, the synovium will demonstrate enhancement, especially prominent on fat-saturation sequences. The destruction of both soft tissue structures and bone can lead to severe elbow instability. In late-stage RA, when the joint space is almost completely destroyed, MR may show a decrease in the synovitis.183 Although other imaging modalities such as ultrasound may be used to follow the course of RA, MR imaging is able to evaluate better the subtle alterations to the bone as well as to the tendons that may not be detectable using ultrasound.
Osteoarthritis is seen less commonly in the elbow than in weight-bearing joints, and commonly there is a predisposing factor that has resulted in the degeneration of articular cartilage, such as trauma or arthropathy. Findings are typically evident on plain films.181 MR imaging may be used to evaluate the integrity of the cartilage, identify focal defects or chondromalacia, and further qualify the findings seen on radiography. Osteoarthritis is a long-term complication of instability and impingement.173,184
1 Functional anatomy of the musculoskeletal system. Standring S., editor. Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 39th ed, Edinburgh: Elsevier, 2005.
2 Bates B., Hoekelman R. Interviewing and the health history. In: Bates B., editor. A Guide to Physical Examination. 3rd ed. Philadelphia: JB Lippincott; 1983:1-27.
3 Bates B. The musculoskeletal system. In: Bates B., editor. A Guide to Physical Examination. 3rd ed. Philadelphia: JB Lippincott; 1983:324-370.
4 Weinstein S.M., Herring S.A. Nerve problems and compartment syndromes in the hand, wrist, and forearm. Clin Sports Med. 1992;11(1):161-188.
5 Rojas I.L., Provencher M.T., Bhatia S., et al. Biceps activity during windmill softball pitching: injury implications and comparison with overhand throwing. Am J Sports Med. 2009;37(3):558-565.
6 Davidson P.A., Pink M., Perry J., Jobe F.W. Functional anatomy of the flexor pronator muscle group in relation to the medial collateral ligament of the elbow. Am J Sports Med. 1995;23(2):245-250.
7 Priest J.D., Jones H.H., Nagel D.A. Elbow injuries in highly skilled tennis players. J Sports Med. 1974;2(3):139-149.
8 Priest J.D. Tennis elbow. The syndrome and a study of average players. Minn Med. 1976;59(6):367-371.
9 Carroll R. Tennis elbow: incidence in local league players. Br J Sports Med. 1981;15(4):250-256.
10 Hang Y.S., Peng S.M. An epidemiologic study of upper extremity injury in tennis players with a particular reference to tennis elbow. Taiwan Yi Xue Hui Za Zhi. 1984;83(3):307-316.
11 Kitai E., Itay S., Ruder A., et al. An epidemiological study of lateral epicondylitis (tennis elbow) in amateur male players. Ann Chir Main. 1986;5(2):113-121.
12 Jacobson J.A., Miller B.S., Morag Y. Golf and racquet sports injuries. Semin Musculoskelet Radiol. 2005;9(4):346-359.
13 Hensley L.D., Paup D.C. A survey of badminton injuries. Br J Sports Med. 1979;13(4):156-160.
14 Jorgensen U., Winge S. Injuries in badminton. Sports Med. 1990;10(1):59-64.
15 Parziale J.R., Mallon W.J. Golf injuries and rehabilitation. Phys Med Rehabil Clin N Am. 2006;17(3):589-607.
16 Plancher K.D., Minnich J.M. Sports-specific injuries. Clin Sports Med. 1996;15(2):207-218.
17 Wadsworth L.T. When golf hurts: musculoskeletal problems common to golfers. Curr Sports Med Rep. 2007;6(6):362-365.
18 Wiesler E.R., Lumsden B. Golf injuries of the upper extremity. J Surg Orthop Adv. 2005;14(1):1-7.
19 Loftice J., Fleisig G.S., Zheng N., Andrews J.R. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23(4):519-530. vii–viii
20 Verow P. Squash. Practitioner. 1989;233(1470):876. 878–879
21 Cooney W.P.3rd. Sports injuries to the upper extremity. How to recognize and deal with some common problems. Postgrad Med. 1984;76(4):45-50.
22 Meeuwisse W.H., Sellmer R., Hagel B.E. Rates and risks of injury during intercollegiate basketball. Am J Sports Med. 2003;31(3):379-385.
23 Heming M. Occupational injuries suffered by classical musicians through overuse. Clinical Chiropractic. 2004;7(2):55-66.
24 Klussmann A., Gebhardt H., Liebers F., Rieger M.A. Musculoskeletal symptoms of the upper extremities and the neck: a cross-sectional study on prevalence and symptom-predicting factors at visual display terminal (VDT) workstations. BMC Musculoskelet Disord. 2008;9:96.
25 Eltayeb S., Staal J.B., Kennes J., et al. Prevalence of complaints of arm, neck and shoulder among computer office workers and psychometric evaluation of a risk factor questionnaire. BMC Musculoskelet Disord. 2007;8:68.
26 Pascarelli E.F., Hsu Y.P. Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil. 2001;11(1):1-21.
27 Silverstein B., Viikari-Juntura E., Kalat J. Use of a prevention index to identify industries at high risk for work-related musculoskeletal disorders of the neck, back, and upper extremity in Washington state, 1990–1998. Am J Ind Med. 2002;41(3):149-169.
28 Helliwell P.S., Bennett R.M., Littlejohn G., et al. Towards epidemiological criteria for soft-tissue disorders of the arm. Occup Med (Lond). 2003;53(5):313-319.
29 Young M.F. The physics of anatomy. In: Essential Physics for Muscloskeletal Medicine. Edinburgh: Elsevier; 2009.
30 Hindle A. Function of the upper limb. In: Trew M., Everett T., editors. Human Movement: An Introductory Text. 4th ed. Churchill Livingstone: Edinburgh; 2005:193-202.
31 Schwartz D., Reisdorff E. Fundamentals of skeletal radiology. In: Emergency Radiology. Colombus, OH: McGraw-Hill; 1999:L11-L26.
32 Rowe L., Yochum T. Radiograpic positioning and normal anatomy. In: Yochum T., Rowe L., editors. Essentials of Skeletal Radiology. Baltimore: Williams and Wilkins; 1987:1-93.
33 Kijowski R., De Smet A.A. The role of ultrasound in the evaluation of sports medicine injuries of the upper extremity. Clin Sports Med. 2006;25(3):569-590. viii
34 Balint P., Sturrock R.D. Musculoskeletal ultrasound imaging: a new diagnostic tool for the rheumatologist? Br J Rheumatol. 1997;36(11):1141-1142.
35 Kane D., Grassi W., Sturrock R., Balint P.V. Musculoskeletal ultrasound—a state of the art review in rheumatology. Part 2: Clinical indications for musculoskeletal ultrasound in rheumatology. Rheumatology (Oxford). 2004;43(7):829-838.
36 Yoon J.S., Walker F.O., Cartwright M.S. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve. 2008;38(4):1231-1235.
37 Yoon J.S., Hong S.J., Kim B.J., et al. Ulnar nerve and cubital tunnel ultrasound in ulnar neuropathy at the elbow. Arch Phys Med Rehabil. 2008;89(5):887-889.
38 Yoon J.S., Kim B.J., Kim S.J., et al. Ultrasonographic measurements in cubital tunnel syndrome. Muscle Nerve. 2007;36(6):853-855.
39 Wiesler E.R., Chloros G.D., Cartwright M.S., et al. Ultrasound in the diagnosis of ulnar neuropathy at the cubital tunnel. J Hand Surg [Am]. 2006;31(7):1088-1093.
40 Okamoto M., Abe M., Shirai H., Ueda N. Diagnostic ultrasonography of the ulnar nerve in cubital tunnel syndrome. J Hand Surg [Br]. 2000;25(5):499-502.
41 Park G.Y., Lee S.M., Lee M.Y. Diagnostic value of ultrasonography for clinical medial epicondylitis. Arch Phys Med Rehabil. 2008;89(4):738-742.
42 Tran N., Chow K. Ultrasonography of the elbow. Semin Musculoskelet Radiol. 2007;11(2):105-116.
43 Serafini G., Zadra N. Anaesthesia for MRI in the paediatric patient. Curr Opin Anaesthesiol. 2008;21(4):499-503.
44 Jaramillo D., Laor T. Pediatric musculoskeletal MRI: basic principles to optimize success. Pediatr Radiol. 2008;38(4):379-391.
45 Smidt N., Lewis M., van der Windt D.A., et al. Lateral epicondylitis in general practice: course and prognostic indicators of outcome. J Rheumatol. 2006;33(10):2053-2059.
46 Bohndorf K., Kilcoyne R.F. Traumatic injuries: imaging of peripheral musculoskeletal injuries. Eur Radiol. 2002;12(7):1605-1616.
47 Hoy G., Wood T., Phillips N., et al. When physiology becomes pathology: the role of magnetic resonance imaging in evaluating bone marrow oedema in the humerus in elite tennis players with an upper limb pain syndrome. Br J Sports Med. 2006;40(8):710-713.
48 Thornton R., Riley G.M., Steinbach L.S. Magnetic resonance imaging of sports injuries of the elbow. Top Magn Reson Imaging. 2003;14(1):69-86.
49 Fritz R.C. MR imaging of osteochondral and articular lesions. Magn Reson Imaging Clin N Am. 1997;5(3):579-602.
50 Ercoli C., Boncan R.B., Tallents R.H., Macher D.J. Loose joint bodies of the temporomandibular joint: a case report. Clin Orthod Res. 1998;1(1):62-67.
51 Chan B.K., Bell S.N. Bilateral avascular necrosis of the humeral trochleae after chemotherapy. J Bone Joint Surg Br. 2000;82(5):670-672.
52 Cunningham P.M. MR imaging of trauma: elbow and wrist. Semin Musculoskelet Radiol. 2006;10(4):284-292.
53 Bartels R.H., Verbeek A.L. Risk factors for ulnar nerve compression at the elbow: a case control study. Acta Neurochir (Wien). 2007;149(7):669-674. discussion 74
54 Rich B.C., McKay M.P. The cubital tunnel syndrome: a case report and discussion. J Emerg Med. 2002;23(4):347-350.
55 Bencardino J.T., Rosenberg Z.S. Entrapment neuropathies of the shoulder and elbow in the athlete. Clin Sports Med. 2006;25(3):465-487. vi–vii
56 Bilge T., Yalaman O., Bilge S., et al. Entrapment neuropathy of the median nerve at the level of the ligament of Struthers. Neurosurgery. 1990;27(5):787-789.
57 Rogers M.R., Bergfield T.G., Aulicino P.L. The failed ulnar nerve transposition. Etiology and treatment. Clin Orthop Relat Res. 1991:269:193-200.
58 Merolla G., Staffa G., Paladini P., et al. Endoscopic approach to cubital tunnel syndrome. J Neurosurg Sci. 2008;52(3):93-98.
59 Tanenbaum L.N. Clinical 3T MR imaging: mastering the challenges. Magn Reson Imaging Clin N Am. 2006;14(1):1-15.
60 Wessely M., Hurtgen-Grace K., Grenier J.-M. Elbow MRI. Part 1. Normal imaging appearance of the elbow. Clinical Chiropractic. 2006;9(4):198-205.
61 Teh J. Imaging of the elbow. Imaging. 2007;19:220-233.
62 Nuffield Orthopaedic Centre NHS Trust. MRI Protocols. Available from www.noc.nhs.uk/SerARef/radiology/mriprotocols.htm, 2009. Accessed 28.02.09
63 Wessely M., Grenier J.-M. Elbow MRI. Part 2: The imaging of common disorders affecting the elbow region. Clinical Chiropractic. 2007;10(1):43-49.
64 Brunton L.M., Anderson M.W., Pannunzio M.E., et al. Magnetic resonance imaging of the elbow: update on current techniques and indications. J Hand Surg [Am]. 2006;31(6):1001-1011.
65 Fowler K.A., Chung C.B. Normal MR imaging anatomy of the elbow. Magn Reson Imaging Clin N Am. 2004;12(2):191-206. v
66 Standring S., editor. Gray’s Anatomy – Pectoral girdle and upper limb: General organization and surface anatomy of the upper limb. Edinburgh: Elsevier, 2009. (Section 48)
67 Green J., Silver P. Exploring the limbs. In: An Introduction to Human Anatomy. Oxford: Oxford University Press; 1981:27-51.
68 Standring S., editor. Gray’s Anatomy – Pectoral girdle and upper limb: Elbow. Edinburgh: Elsevier, 2009. (Section 51)
69 Moore K. The upper limb. In Clinically Oriented Anatomy, 2nd ed, Baltimore: Williams and Wilkins; 1985:626-793.
70 O’Driscoll S. Coronoid fracture classification. Available from www.eorif.com/Elbowforearm/images, 2009. Accessed 09.03.09
71 O’Hara J.J., Stone J.H. Ulnar nerve compression at the elbow caused by a prominent medial head of the triceps and an anconeus epitrochlearis muscle. J Hand Surg [Br]. 1996;21(1):133-135.
72 Hsu R.W., Chen C.Y., Shen W.J. Ulnar nerve palsy due to concomitant compression by the anconeus epitrochlearis muscle and a ganglion cyst. Orthopedics. 2004;27(2):227-228.
73 Kim Y.S., Yeh L.R., Trudell D., Resnick D. MR imaging of the major nerves about the elbow: cadaveric study examining the effect of flexion and extension of the elbow and pronation and supination of the forearm. Skeletal Radiol. 1998;27(8):419-426.
74 Green J., Silver P. The blood supply and nerve supply to the upper limb. In: An Introduction to Human Anatomy. Oxford: Oxford University Press; 1981:69-88.
75 Standring S., editor. Gray’s Anatomy – Pectoral girdle and upper limb: Forearm. Edinburgh: Elsevier, 2009. (Section 52)
76 Green J., Silver P. The muscles and joints of the upper limb. In: An Introduction to Human Anatomy. Oxford: Oxford University Press; 1981:89-112.
77 Munshi M., Pretterklieber M.L., Chung C.B., et al. Anterior bundle of ulnar collateral ligament: evaluation of anatomic relationships by using MR imaging, MR arthrography, and gross anatomic and histologic analysis. Radiology. 2004;231(3):797-803.
78 Rowe L., Yochum T. Trauma. In: Yochum T., Rowe L., editors. Essentials of Skeletal Radiology. 2nd ed. Baltimore: Williams and Wilkins; 1996:653-794.
79 Lin F., Kohli N., Perlmutter S., et al. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16(6):795-802.
80 Lynch J.R., Waitayawinyu T., Hanel D.P., Trumble T.E. Medial collateral ligament injury in the overhand-throwing athlete. J Hand Surg [Am]. 2008;33(3):430-437.
81 Berg E.E., DeHoll D. Radiography of the medial elbow ligaments. J Shoulder Elbow Surg. 1997;6(6):528-533.
82 Dunning C.E., Zarzour Z.D., Patterson S.D., et al. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 2001;83-A(12):1823-1828.
83 Dunning C.E., Zarzour Z.D., Patterson S.D., et al Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin Orthop Relat Res. 2001:388:118-124
84 Lee B.P., Teo L.H. Surgical reconstruction for posterolateral rotatory instability of the elbow. J Shoulder Elbow Surg. 2003;12(5):476-479.
85 Sener E., Takka S., Cila E. Supracondylar process syndrome. Arch Orthop Trauma Surg. 1998;117(6–7):418-419.
86 Lordan J., Rauh P., Spinner R.J. The clinical anatomy of the supracondylar spur and the ligament of Struthers. Clin Anat. 2005;18(7):548-551.
87 Siqueira M.G., Martins R.S. The controversial arcade of Struthers. S1. Surg Neurol. 64. suppl 1:2005:17-20, discussion S1:20–21
88 Campbell W.W., Landau M.E. Controversial entrapment neuropathies. Neurosurg Clin N Am. 2008;19(4):597-608. vi–vii
89 Gudmundsen T.E., Ostensen H. Accessory ossicles in the elbow. Acta Orthop Scand. 1987;58(2):130-132.
90 Obermann W.R., Loose H.W. The os supratrochleare dorsale: a normal variant that may cause symptoms. AJR Am J Roentgenol. 1983;141(1):123-127.
91 Ishikawa H., Hirohota K., Kashiwagi D. A case report of patella cubiti. Z Rheumatol. 1976;35(11–12):407-411.
92 Kopuz C., Sancak B., Ozbenli S. On the incidence of third head of biceps brachii in Turkish neonates and adults. Kaibogaku Zasshi. 1999;74(3):301-305.
93 Standring S., editor. Gray’s Anatomy – Pectoral girdle and upper limb: Upper arm. Edinburgh: Elsevier, 2009. (Section 50)
94 Macalister A. Additional observations on muscular anomalies in human anatomy (third series), with a catalogue of the principal muscular variations hitherto published. Trans Roy Ir Acad Sci. 1875;25:1-134.
95 Vollala V.R., Nagabhooshana S., Bhat S.M., et al. Multiple arterial, neural and muscular variations in upper limb of a single cadaver. Rom J Morphol Embryol. 2009;50(1):129-135.
96 Kim K.C., Rhee K.J., Shin H.D. A long head of the biceps tendon confluent with the intra-articular rotator cuff: arthroscopic and MR arthrographic findings. Arch Orthop Trauma Surg. 2009;129(3):311-314.
97 Kim K.C., Rhee K.J., Shin H.D., Kim Y.M. Biceps long head tendon revisited: a case report of split tendon arising from single origin. Arch Orthop Trauma Surg. 2008;128(5):495-498.
98 Schoenleber S.J., Spinner R.J. An unusual variant of the biceps brachii. Clin Anat. 2006;19(8):702-703.
99 Abu-Hijleh M.F. Three-headed biceps brachii muscle associated with duplicated musculocutaneous nerve. Clin Anat. 2005;18(5):376-379.
100 Jacoby S.M., Herman M.J., Morrison W.B., Osterman A.L. Pediatric elbow trauma: an orthopaedic perspective on the importance of radiographic interpretation. Semin Musculoskelet Radiol. 2007;11(1):48-56.
101 De Boeck H. Radiology of the elbow in children. Acta Orthop Belg. 1996;62(suppl 1):34-40.
102 Ansah P., Vogt S., Ueblacker P., et al. Osteochondral transplantation to treat osteochondral lesions in the elbow. J Bone Joint Surg Am. 2007;89(10):2188-2194.
103 Takahara M., Mura N., Sasaki J., et al. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 Pt 1):47-62.
104 Takahara M., Mura N., Sasaki J., et al. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89(6):1205-1214.
105 Mitsunaga M.M., Adishian D.A., Bianco A.J.Jr. Osteochondritis dissecans of the capitellum. J Trauma. 1982;22(1):53-55.
106 Klekamp J., Green N.E., Mencio G.A. Osteochondritis dissecans as a cause of developmental dislocation of the radial head. Clin Orthop Relat Res. 1997:338:36-41
107 Marshall K.W., Marshall D.L., Busch M.T., Williams J.P. Osteochondral lesions of the humeral trochlea in the young athlete. Skeletal Radiol. 2009;38(5):479-491.
108 Kennedy J. What are osteochondral defects? Available from http://www.osteochondraldefects.com, 2009. Accessed 02.03.09
109 Rowe L., Yochum T. Hematological and vascular disorders. In: Yochum T., Rowe L., editors. Essentials of Skeletal Radiology. 2nd ed. Baltimore: Williams and Wilkins; 1996:1243-1326.
110 Kijowski R., De Smet A.A. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34(5):266-271.
111 Beers M., Berkow R. Avascular necrosis. In The Merck Manual, 17th ed, Merck & Co: West Point, PA; 1999:453-454.
112 Peterson R.K., Savoie F.H.3rd, Field L.D. Osteochondritis dissecans of the elbow. Instr Course Lect. 1999;48:393-398.
113 Helms C. Arthritis. In: Fundamentals of Skeletal Radiology. Philadelphia: Elsevier Saunders; 2005:113-140.
114 Ytrehus B., Carlson C.S., Ekman S. Etiology and pathogenesis of osteochondrosis. Vet Pathol. 2007;44(4):429-448.
115 Kobayashi K., Burton K.J., Rodner C., et al. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg. 2004;12(4):246-254.
116 Kaeding C.C., Whitehead R. Musculoskeletal injuries in adolescents. Prim Care. 1998;25(1):211-223.
117 Stoane J.M., Poplausky M.R., Haller J.O., Berdon W.E. Panner’s disease: X-ray, MR imaging findings and review of the literature. Comput Med Imaging Graph. 1995;19(6):473-476.
118 Jawish R., Rigault P., Padovani J.P., et al. Osteochondritis dissecans of the humeral capitellum in children. Eur J Pediatr Surg. 1993;3(2):97-100.
119 De Smet A.A., Fisher D.R., Graf B.K., Lange R.H. Osteochondritis dissecans of the knee: value of MR imaging in determining lesion stability and the presence of articular cartilage defects. Am J Roentgenol. 1990;155(3):549-553.
120 De Smet A.A., Fisher D.R., Burnstein M.I., et al. Value of MR imaging in staging osteochondral lesions of the talus (osteochondritis dissecans): results in 14 patients. Am J Roentgenol. 1990;154(3):555-558.
121 Bradley J.P., Petrie R.S. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med. 2001;20(3):565-590.
122 Pena E., Calvo B., Martinez M.A., Doblare M. Effect of the size and location of osteochondral defects in degenerative arthritis. A finite element simulation. Comput Biol Med. 2007;37(3):376-387.
123 Steinbach L.S., Fritz R.C., Tirman P.F., Uffman M. Magnetic resonance imaging of the elbow. Eur J Radiol. 1997;25(3):223-241.
124 Beingessner D.M., Dunning C.E., Gordon K.D., et al. The effect of radial head fracture size on elbow kinematics and stability. J Orthop Res. 2005;23(1):210-217.
125 Itamura J., Roidis N., Mirzayan R., et al. Radial head fractures: MRI evaluation of associated injuries. J Shoulder Elbow Surg. 2005;14(4):421-424.
126 Tejwani N.C., Mehta H. Fractures of the radial head and neck: current concepts in management. J Am Acad Orthop Surg. 2007;15(7):380-387.
127 Loder R.T. The demographics of equestrian-related injuries in the United States: injury patterns, orthopedic specific injuries, and avenues for injury prevention. J Trauma. 2008;65(2):447-460.
128 O’Dwyer H., O’Sullivan P., Fitzgerald D., et al. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. J Comput Assist Tomogr. 2004;28(4):562-565.
129 Gordon K.D., Duck T.R., King G.J., Johnson J.A. Mechanical properties of subchondral cancellous bone of the radial head. J Orthop Trauma. 2003;17(4):285-289.
130 Landin L.A., Danielsson L.G. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand. 1986;57(4):309-312.
131 Mackenney P.J., McQueen M.M., Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88(9):1944-1951.
132 Cohen M.S. Fractures of the coronoid process. Hand Clin. 2004;20(4):443-453.
133 Zeiders G.J., Patel M.K. Management of unstable elbows following complex fracture-dislocations—the “terrible triad” injury. J Bone Joint Surg Am. 2008;90(suppl 4):75-84.
134 Lindenhovius A.L., Jupiter J.B., Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg [Am]. 2008;33(6):920-926.
135 Loomer R.L. Elbow injuries in athletes. Can J Appl Sport Sci. 1982;7(3):164-166.
136 McKee M.D., Schemitsch E.H., Sala M.J., O’Driscoll S.W. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003;12(4):391-396.
137 Josefsson P.O., Nilsson B.E. Incidence of elbow dislocation. Acta Orthop Scand. 1986;57(6):537-538.
138 Macias C.G., Wiebe R., Bothner J. History and radiographic findings associated with clinically suspected radial head subluxations. Pediatr Emerg Care. 2000;16(1):22-25.
139 Macias C.G. Radial head subluxation. Acad Emerg Med. 2000;7(2):207-208.
140 Schunk J.E. Radial head subluxation: epidemiology and treatment of 87 episodes. Ann Emerg Med. 1990;19(9):1019-1023.
141 Quan L., Marcuse E.K. The epidemiology and treatment of radial head subluxation. Am J Dis Child. 1985;139(12):1194-1197.
142 Helms C. Trauma. In: Fundamentals of Skeletal Radiology. Philadelphia: Elsevier Saunders; 2005:78-112.
143 Kijowski R., Tuite M., Sanford M. Magnetic resonance imaging of the elbow. Part II: Abnormalities of the ligaments, tendons, and nerves. Skeletal Radiol. 2005;34(1):1-18.
144 Melloni P., Valls R. The use of MRI scanning for investigating soft-tissue abnormalities in the elbow. Eur J Radiol. 2005;54(2):303-313.
145 Kooima C.L., Anderson K., Craig J.V., et al. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am J Sports Med. 2004;32(7):1602-1606.
146 O’Holleran J.D., Altchek D.W. The thrower’s elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J. 2006;2(1):83-93.
147 McKee M.D., Schemitsch E.H., Sala M.J., O’Driscoll S.W. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003;12(4):391-396.
148 Richard M.J., Aldridge J.M.3rd, Wiesler E.R., Ruch D.S. Traumatic valgus instability of the elbow: pathoanatomy and results of direct repair. J Bone Joint Surg Am. 2008;90(11):2416-2422.
149 Marti R.K., Kerkhoffs G.M., Maas M., Blankevoort L. Progressive surgical release of a posttraumatic stiff elbow. Technique and outcome after 2–18 years in 46 patients. Acta Orthop Scand. 2002;73(2):144-150.
150 Bauman J.T., Sotereanos D.G., Weiser R.W. Complete rupture of the distal biceps tendon in a woman: case report. J Hand Surg [Am]. 2006;31(5):798-800.
151 Ramsey M.L. Distal biceps tendon injuries: diagnosis and management. J Am Acad Orthop Surg. 1999;7(3):199-207.
152 Durr H.R., Stabler A., Pfahler M., et al Partial rupture of the distal biceps tendon. Clin Orthop Relat Res. 2000:374:195-200
153 Martin C.E., Schweitzer M.E. MR imaging of epicondylitis. Skeletal Radiol. 1998;27(3):133-138.
154 Savnik A., Jensen B., Norregaard J., et al. Magnetic resonance imaging in the evaluation of treatment response of lateral epicondylitis of the elbow. Eur Radiol. 2004;14(6):964-969.
155 Eustace S., Johnston C., O’Neill P., O’Byrne J. The elbow. In: Sports Injuries: Examination, Imaging and Management. Edinburgh: Elsevier Churchill Livingstone; 2007:333-356.
156 Bannister R. Disorders of the nerve roots and peripheral nerves. In Brain and Bannister’s Clinical Neurology, 7th ed, Oxford: Oxford University Press; 1992:420-458.
157 Boero S., Sénès F., Catena N. Pediatric cubital tunnel syndrome by anconeus epitrochlearis: a case report. J Shoulder Elbow Surg. 2009;18(2):e21-e23.
158 Dahners L.E., Wood F.M. Anconeus epitrochlearis, a rare cause of cubital tunnel syndrome: a case report. J Hand Surg [Am]. 1984;9(4):579-580.
159 Matsuura S., Kojima T., Kinoshita Y. Cubital tunnel syndrome caused by abnormal insertion of triceps brachii muscle. J Hand Surg [Br]. 1994;19(1):38-39.
160 Abe M., Ishizu T., Shirai H., et al. Tardy ulnar nerve palsy caused by cubitus varus deformity. J Hand Surg [Am]. 1995;20(1):5-9.
161 Barrios C., Ganoza C., de Pablos J., Canadell J. Posttraumatic ulnar neuropathy versus non-traumatic cubital tunnel syndrome: clinical features and response to surgery. Acta Neurochir (Wien). 1991;110(1–2):44-48.
162 Matsuzaki A. Membranous tissue under the flexor carpi ulnaris muscle as a cause of cubital tunnel syndrome. Hand Surg. 2001;6(2):191-197.
163 Grana W. Medial epicondylitis and cubital tunnel syndrome in the throwing athlete. Clin Sports Med. 2001;20(3):541-548.
164 Lindsay K., Bone I., Callander R. Localised neurological disease and its management. In: Neurology and Neurosurgery Illustrated. Edinburgh: Elsevier; 1991:213-466.
165 Bridgeman C., Naidu S., Kothari M.J. Clinical and electrophysiological presentation of pronator syndrome. Electromyogr Clin Neurophysiol. 2007;47(2):89-92.
166 Ng A.B., Borhan J., Ashton H.R., et al. Radial nerve palsy in an elite bodybuilder. Br J Sports Med. 2003;37(2):185-186.
167 Paraskevas G., Natsis K., Ioannidis O., et al. Accessory muscles in the lower part of the anterior compartment of the arm that may entrap neurovascular elements. Clin Anat. 2008;21(3):246-251.
168 Fitzgerald A., Anderson W., Hooper G. Posterior interosseous nerve palsy due to parosteal lipoma. J Hand Surg [Br]. 2002;27(6):535-537.
169 Siemons W., Kegels L., Van Oyen J., et al. Bicipitoradial bursitis. JBR-BTR. 2007;90(5):456.
170 Blankstein A., Ganel A., Givon U., et al. Ultrasonographic findings in patients with olecranon bursitis. Ultraschall Med. 2006;27(6):568-571.
171 Watrous B.G., Ho G.Jr. Elbow pain. Prim Care. 1988;15(4):725-735.
172 Jin W., Lee J.H., Yang D.M., et al. Olecranon bursitis communicating with an olecranon cyst in rheumatoid arthritis. J Ultrasound Med. 2007;26(6):857-861.
173 Schweitzer M., Morrison W.B. Arthropathies and inflammatory conditions of the elbow. Magn Reson Imaging Clin N Am. 1997;5(3):603-617.
174 Llinas L., Olenginski T.P., Bush D., et al. Osteomyelitis resulting from chronic filamentous fungus olecranon bursitis. J Clin Rheumatol. 2005;11(5):280-282.
175 Ruch D.S., Papadonikolakis A., Campolattaro R.M. The posterolateral plica: a cause of refractory lateral elbow pain. J Shoulder Elbow Surg. 2006;15(3):367-370.
176 Steinert A.F., Goebel S., Rucker A., Barthel T. Snapping elbow caused by hypertrophic synovial plica in the radiohumeral joint: a report of three cases and review of literature. Arch Orthop Trauma Surg. 2010. Mar;130(3):347–351
177 Farkas C., Gaspar L., Jonas Z. The pathological plica in the knee. Acta Chir Hung. 1997;36(1–4):83-85.
178 Boles C.A., Butler J., Lee J.A., et al. Magnetic resonance characteristics of medial plica of the knee: correlation with arthroscopic resection. J Comput Assist Tomogr. 2004;28(3):397-401.
179 Lehtinen J.T., Kaarela K., Ikavalko M., et al. Incidence of elbow involvement in rheumatoid arthritis. A 15 year endpoint study. J Rheumatol. 2001;28(1):70-74.
180 Ehrlich G.E. Incidence of elbow involvement in rheumatoid arthritis. J Rheumatol. 2001;28(7):1739.
181 Rowe L., Yochum T. Arthritic disorders. In: Yochum T., Rowe L., editors. Essentials of Skeletal Radiology. 2nd ed. Baltimore: Williams and Wilkins; 1996:795-974.
182 Beers M., Berkow R. Diffuse connective tissue disease. In The Merck Manual, 17th ed, Merck & Co: West Point, PA; 1999:416-445.
183 Guermazi A., Taouli B., Lynch J.A., Peterfy C.G. Imaging of bone erosion in rheumatoid arthritis. Semin Musculoskelet Radiol. 2004;8(4):269-285.
184 Kato H., Hirayama T., Minami A., et al. Cubital tunnel syndrome associated with medial elbow ganglia and osteoarthritis of the elbow. J Bone Joint Surg Am. 2002;84-A(8):1413-1419.