from clinical reasoning to molecular biology
2.2 Laboratory methods11
Patients present with symptoms, and a clinical examination elicits signs that suggest a diagnosis. Examination of specimens such as blood, urine, faeces and tissue samples in the various pathology laboratories helps confirm this diagnosis and monitor the treatment.
• Diagnosis involves clinical skills and laboratory tests.
• Specialist pathological techniques can aid in diagnosis.
• The autopsy has a place in auditing the quality of diagnosis in addition to determining cause of death.
2.1. Diagnosis
Diagnosis is the act of recognising a disease in an individual patient and is based on clinical history, physical examination and investigation. The ability to integrate knowledge of the classification, epidemiology and mechanisms of disease processes, as discussed in Chapter 1, is essential. Making a diagnosis involves:
• taking a clinical history of symptoms: what the patient has noticed wrong (e.g. cough, breathlessness, pain)
• clinical examination for signs: what the doctor finds wrong on examination (e.g. lumps, rashes, abnormal lung sounds).
The clinician then works through a series of questions:
• Which organ system is most likely to be affected?
• Which category of disease do the signs and symptoms most likely suggest, e.g. inflammation, malignancy or poisoning?
• Do other factors such as race, age, sex, behavioural patterns or occupation of the patient provide clues to the diagnosis?
The diagnostic process involves testing a series of hypotheses based on the clinician’s knowledge of the frequency of occurrence of the symptoms and signs in different disease states and on the probability of these occurring in the population from which the patient comes. A list of possible diagnoses is constructed, known as the differential diagnosis, beginning with the most likely disease and progressing to include diagnoses which are less likely but are important to exclude.
Special investigations are used to refine the list of differential diagnoses by providing evidence consistent with some diagnoses but excluding others. In a sense, they test the hypothesis that a particular disease process is present in a patient. Special investigations can include radiology, isotope scans, and tests of body fluids and tissue in the pathology laboratories. Reaching a diagnosis enables the clinician to start treatment and to give the patient some idea of the outcome of the disease (prognosis).
The clinical laboratory disciplines
As a clinical subject, pathology grew up in side rooms adjacent to hospital wards where simple diagnostic tests could be performed by nurses, medical students and doctors, and in the post-mortem room where the morphological changes associated with disease could be observed at autopsy. As the number and complexity of tests grew, hospitals required centralised laboratories, staffed by dedicated technical and medical personnel.
Nowadays, clinical pathology is divided into a number of disciplines, each with its own specialist practitioners:
• Clinical chemistry or chemical pathology: the investigation of metabolic disturbances by changes in the concentration of substances in body fluids.
• Haematology: the study of diseases of the blood and bone marrow.
• Immunology: the study of diseases of the immune system.
• Medical genetics: the study of the inheritance of disease.
• Microbiology: the detection and characterisation of bacteria, viruses, fungi and parasites.
2.2. Laboratory methods
Histopathology
Histology
Basic histological techniques involve the processing of tissue specimens, so that they can be finely sliced and stained on a glass slide to be examined under the light microscope. Specimens can include biopsies (small pieces of tissue removed to make a diagnosis) and excision specimens (where a surgeon removes the diseased tissue as a therapeutic procedure). The tissue is first fixed in a preservative, usually formalin. It is then processed into paraffin wax, which supports the tissue while it is sliced into thin sections, typically 4–5μm in thickness.
Most histopathology laboratories use the haematoxylin and eosin (H&E) stain routinely. The haematoxylin dye stains basic molecules blue, such as nucleic acids, while the eosin stains acidic molecules red, such as proteins. Pathologists commonly use terms such as basophilic and eosinophilic for materials that take up haematoxylin and eosin, respectively. Other stains may be used in addition to H&E for some specimens to demonstrate a particular substance or structure better than in an H&E section. Some of these special stains are highly specialised and used rarely; others are used commonly in pathology (Table 2).
| Stain | Principle | Examples of diagnostic use |
|---|---|---|
| Reticulin | Silver impregnation of reticulin fibres (predominantly type III collagen) | Demonstration of the architecture of tissues, e.g. lung and liver, by outlining the reticulin network around cells |
| Trichrome | Dye binds to collagen | Demonstration of fibrosis in inflammatory and neoplastic processes |
| Periodic acid–Schiff (PAS) | Reacts with sugars and macromolecules rich in sugar residues | Demonstration of substances such as glycogen, mucin and basement membranes |
| Perls’ | Uses the Prussian blue reaction to demonstrate iron | Demonstration of iron deposits following inflammation or in haemochromatosis |
| Congo red | Dye is taken up by beta-pleated sheets | Demonstration of amyloid |
| Gram’s | Uptake and retention of dyes depends on qualities of bacterial cell walls | Demonstrates bacteria and divides them into two groups: Gram-positive (stain dark blue) and Gram-negative (stain pink-red). |
| Ziehl–Neelsen (ZN) | Stains acid-fast bacilli | Demonstration of mycobacterial infection |
| Giemsa’s | One of the Romanowsky family of stains that uses methylene blue and eosin | A routine stain for blood films and air-dried cytology specimens. Can also be used in tissue sections, for example to demonstrate certain parasites |
| Papanicolaou’s | A mixture of dyes gives good cellular morphology | The routine stain for fixed cytology preparations, e.g. cervical smears |
Sometimes clinicians require a very urgent diagnosis during surgery. If so, small amounts of tissue can be frozen quickly and sectioned in an instrument called a cryostat, and looked at within a few minutes (‘frozen sections’). Another use for frozen sections is to demonstrate fatty material in a specimen, because processing to paraffin wax dissolves any lipid out of the tissue.
It is also possible to look at tissues at a much higher magnification using the electron microscope. This technique, also known as ultrastructural examination, demonstrates cell structures at the level of organelles and smaller. It is relatively expensive and is generally used only in specific circumstances, such as the investigation of glomerular disease in renal biopsies. Viral particles in cells can be seen by electron microscopy.
Cytology
Sometimes it is easier or more efficient to take specimens of cells rather than whole pieces of tissue. Cells can be scraped from the surface (as in cervical smears), aspirated from various parts of the body through a fine needle, or separated from body fluids (such as urine, effusions or cerebrospinal fluid). The cells thus obtained can be placed directly on glass slides and stained to produce a cytological preparation, allowing abnormal cell morphology to be identified. Alternatively, the cells can be used for other techniques such as flow cytometry or detection of viral DNA.
Immunohistochemistry
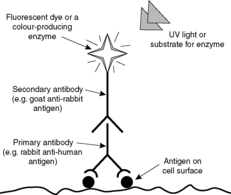
Immunohistochemistry provides the pathologist with a powerful tool for demonstrating and identifying proteins, glycolipids and carbohydrates, which may be normal tissue constituents or produced as a result of a pathological process. Immunohistochemistry is based on the specificity of antibody-antigen binding. Monoclonal antibodies (antibodies having only one antigenic target) or polyclonal antibodies (a group of antibodies having a range of targets) can be made against a range of human antigens (Figure 1 and Ch. 7). Monoclonal antibodies are more specific. The antibodies can be applied to tissue sections or cytology preparations and will bind wherever their antigen is present. The antibody can be tagged either with an enzyme that catalyses a colour reaction or with a fluorescent dye. In this way the antibody and, by implication, the antigen can be visualised. A simple example is given in Figure 2.
Immunohistochemistry has enabled pathologists to learn much about the distribution of tissue antigens in both health and disease, and has increased the accuracy of diagnosis. Examples of diagnostic immunohistochemistry are given in Table 3.
| Antibody | Diagnostic use |
|---|---|
| Chromogranin | This component of neurosecretory granules can be used to locate neuroendocrine cells in tissues. It is also found in neoplasms of neuroendocrine type, e.g. carcinoid tumours and pancreatic endocrine tumours |
| Cytokeratin | The expression of cytokeratin by a tumour may help differentiate between an epithelial and a non-epithelial neoplasm. Sometimes specific cytokeratins can suggest a primary site, e.g. CK20 is typically expressed by carcinomas of the large intestine |
| Desmin | This filamentous protein is found in muscle cells. Its expression in a neoplasm implies muscle differentiation |
| Immunoglobulin | Identification of immunoglobulin in neoplastic plasma cells can aid in the diagnosis of multiple myeloma; identification of immunoglobulin in the tissues can help determine the immune nature of a disease, e.g. immunoglobulin in the renal glomerulus in glomerulonephritis (see Chs 7 and 8) |
| S100 | This protein is present in some cells (e.g. melanocytes, nerve cells and antigen-presenting cells), but not in others. It can be used to help determine the line of differentiation of neoplasms |
Molecular biology techniques
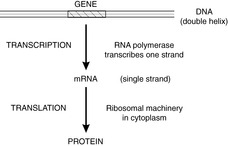
New techniques for looking at chromosomes, genes, DNA, RNA and proteins are being developed continuously. Some are still research techniques, but others have entered diagnostic practice and are described in this section. Familiarity with the structure of DNA and the ‘DNA-RNA-protein’ pathway (Figure 3) will help in understanding the principles of molecular biology.
 |
| Figure 3 |
In situ hybridisation
Molecular techniques can be used to determine whether specific DNA or RNA sequences are present in a specimen. A length of nucleic acid (the probe) with a complementary sequence to the DNA or RNA under study is constructed (see Box 1). The cDNA or cRNA probe is labelled with a radioisotope or a non-radioactive enzyme system and applied to a tissue section. Under the correct conditions the labelled probe will hybridise with its complementary nucleic acid sequence in the tissue. The specimen is then washed, and if the probe has attached itself to the specimen it can be detected by its label. In this way, the locations, numbers or types of cells containing the DNA/RNA can be seen down the microscope. In the relatively new procedure of fluorescent in situ hybridisation (FISH), the probe is attached to a fluorescent marker.
Box 1
• DNA is double stranded
• Bonds between complementary bases hold strands together (cytosine–guanine; adenine–thymine)
• Heat/alkalinise DNA – separation of strands (‘denaturation’) occurs
• Cool separated strands – complementary double strands re-form
• Labelled complementary single-strand DNA can identify a DNA sequence (e.g. a gene) in intact cells or disrupted cell preparations
Polymerase chain reaction (PCR)
This relatively simple technique is now widely used in molecular biology. It allows analysis of DNA or RNA from virtually any tissue specimen. Central to PCR is a chain reaction which amplifies the length of DNA under examination many million-fold. This increases the amount of the sequence to be identified to a level that can be detected easily in the laboratory. The three vital ingredients of the reaction are (Figure 4):
• Two oligonucleotides, usually 15–30 bases long, with sequences matching DNA sequences flanking the DNA fragment of interest. They give the amplification its specificity.
• A heat-stable DNA polymerase (typically Taq polymerase from the thermophilic organism Thermus aquaticus), which can withstand heating and synthesises DNA at high temperatures.
 |
| Figure 4 |
The mixture is heated, dissociating the double-stranded DNA and allowing the single strands to bind to the oligonucleotides. These oligonucleotides then act as primers for the polymerase and a new double-stranded DNA molecule is formed. Twice as much double-stranded DNA is then present and the cycle can be repeated. Each cycle doubles the amount of DNA in the area of interest, so at the end of several cycles (typically between 15 and 30) the area of interest will have been reproduced thousands or millions of times and there will be large amounts of DNA for analysis. The sensitivity of the technique is such that the DNA from a single cell can be amplified. The reaction has numerous applications:
• detection of genetic diseases, e.g. cystic fibrosis
• cross-matching tissues for transplantation (human leucocyte antigen (HLA) subtyping)
• detection of bacteria and viruses
• detection of abnormal genes linked with cancer.
Flow cytometry
Flow cytometers analyse cells as they flow one by one past one or more sensors. The cells are suspended in liquid (the sheath fluid), and as they flow through the machine they are illuminated with light, typically from a laser. From the degree and direction of scatter, information about the physical properties of each cell, such as size and shape, can be deduced. Further information can be obtained by labelling the cells with fluorescent antibodies; the laser causes any labelled cells to fluoresce, so cells with a specific antigen can be identified. Modern machines can analyse several thousand cells every second.
Flow cytometry is a powerful tool; haematologists use it to analyse blood cells, and histopathologists use it to analyse cells from cytological and histological specimens. In the latter case, the cells have to be disaggregated so they form a suspension in the sheath fluid.
DNA microarray analysis
A DNA microarray (DNA chip) is a collection of thousands of microscopic spots of DNA attached to a solid surface such as glass or a silicon chip. The process resembles Southern blotting in that when the DNA to be tested is exposed to the DNA chip, complementary strands will hybridise. The DNA attached to the substrate is called the probe, and the free DNA being tested is called the target. The probe may be a length of cDNA or an oligonucleotide synthesised from nucleic acid bases. Ways in which hybridisation can be detected include fluorescence, chemiluminescence and changes in conductivity in the silicone chip substrate. The result is that thousands of different genes from one sample can be analysed.
Although still essentially an experimental technique, DNA microarrays are expected to have applications in clinical diagnosis. For example:
• microbiological specimens could be screened for the presence of thousands of bacteria simultaneously, without the need for culture
• specific genetic mutations in cancers could be identified, helping accurate classification of the neoplasm and possibly allowing targeted gene therapy
• a potential application in forensic medicine is detection of single nucleotide polymorphisms that could link a sample to an individual person.
Microbiology
Microscopy and bacterial culture
Specimens for microbiological analysis are routinely examined under the microscope. Sometimes, there are enough organisms present for a provisional identification to be made. The Gram stain, Ziehl–Neelsen and Giemsa stains are often used (Table 2).
Culture is performed by inoculating a growth medium such as an agar plate with the specimen and then incubating it under conditions suitable for the growth of pathogenic bacteria. Any bacteria that grow can be isolated and identified by a combination of features, such as their morphology and biochemical profile. The sensitivity of the organism to various antibiotics can also be tested.
Detection of microbial antigens and nucleic acid
The presence of microbial antigens can be detected by using antibodies. For example, enzyme immunoassay uses antibodies fastened to a solid phase, such as the inside of a test tube, to trap antigens in a fluid. If the antigens are captured they can be detected by adding a labelled antibody of the same specificity. If the antigen is present, the labelled antibody will bind to it forming a ‘sandwich’.
Microbiologists use molecular techniques to detect specific DNA or RNA from bacteria and viruses. PCR can be used to amplify microbial DNA so that even a single organism in the specimen can be detected. Although this sensitivity is one of the strengths of PCR, it is also a potential pitfall because contamination of the sample or the presence of clinically insignificant amounts of DNA could produce a false-positive reaction.
Serology
Serology is the detection of specific antibodies in a patient’s blood. If antibodies to an organism are detected it provides indirect evidence of infection. However, the results of these tests require careful interpretation since a positive result could indicate past exposure to the organism rather than current infection.
A commonly used serological method is enzyme immunoassay. The principle is the same as described in the previous section except that the antigen is attached to the solid phase and is used to trap antibody in the fluid being tested.
Cytogenetics
The mainstay of morphological cytogenetics is the karyotype, which consists of the chromosomes numbered and arranged in sequence from largest to smallest. Classically, karyotyping is performed on chromosomes in metaphase obtained by treating cultured cells with colchicine, which disrupts the formation of the mitotic spindle. The chromosomes are stained with Giemsa’s, resulting in a sequence of light and dark bands unique to each chromosome. The latest techniques use chromosomes in prometaphase because the banding pattern is visible more clearly. Changes in the number or structure of chromosomes can be used to diagnose cytogenetic diseases (see Ch. 1).
In comparative genomic hybridisation, changes in the number of copies of a segment of a chromosome can be detected. It is used in cancer cytogenetics and for the assessment of early embryos during in vitro fertilisation procedures. In principle, chromosomes from the patient are broken into small segments and labelled with a fluorochrome. Normal chromosomes act as a control; they are broken into similar segments and labelled with a different fluorochrome. A mixture of these chromosome fragments are hybridised to normal chromosome spreads on a microscope slide. If there is more or less of one segment in the patient’s sample, the ratio of the intensities of the two fluorochromes along the chromosomes in the spreads will change. This finding represents regions of gain or loss of DNA sequences, such as duplications, amplifications or deletions.
2.3. The autopsy
The word autopsy is derived from the Greek word for eye witness, and can be translated as ‘seeing for oneself’. It is the examination of the body after death (post-mortem examination) and can involve histological, microbiological and other techniques in addition to the dissection and naked-eye examination of the organs.
Most countries have statutory procedures for investigating deaths that are suspicious or unnatural. In England and Wales, it is the responsibility of the coroner to investigate such deaths and to order an autopsy if one is required (see Box 2). If the case does not fall under the jurisdiction of the coroner, an autopsy can only be performed by obtaining fully informed consent from the next of kin; such cases are often called ‘hospital autopsies’ to distinguish them from coroners’ autopsies. In the UK there are stringent regulations concerning the retention of tissues and organs at post mortem for further investigations, teaching or research. Other nations have similar regulations in place.
Box 2
A death should be referred to the coroner if:
• the cause of death is unknown
• the deceased was not seen by the certifying doctor either after death or in the 14days before death
• the deceased was not seen by a doctor during their last illness
• the death was violent, unnatural or suspicious
• the death may be due to an accident (whenever it occurred), suicide or an abortion
• the death may be due to self-neglect or neglect by others
• the death may be related to a medical procedure or treatment
• the death occurred during an operation or before recovery from the effects of an anaesthetic
• the death occurred during or shortly after detention in prison or police custody
• the deceased was detained under the Mental Health Act
• the death may be due to an industrial disease or related to the deceased’s employment.
Self-assessment: questions
One best answer questions
2. Which of the following is most suitable for analysing thousands of different genes simultaneously?
a. DNA microarray
b. electron microscopy
c. enzyme immunoassay
d. flow cytometry
e. polymerase chain reaction (PCR)
3. A doctor is examining a patient with high blood pressure. She suspects he may have a phaeochromocytoma (a tumour of the adrenal medulla that secretes adrenaline and noradrenaline) so she wishes to measure the levels of catecholamines in his urine. To which laboratory should she submit the urine specimen?
a. chemical pathology
b. cytogenetics
c. haematology
d. histopathology
e. immunology
True-false questions
1. The following are correctly paired:
a. haematoxylin uptake – eosinophilia
b. DNA polymerase – polymerase chain reaction (PCR)
c. tuberculosis – PAS stain
d. serology – enzyme immunoassay
e. high blood pressure – clinical sign
2. The following statements are correct:
a. immunohistochemistry demonstrates the presence of antigens in tissues
b. western blotting techniques are used to analyse DNA
c. squamous cell carcinoma may produce cytokeratin intermediate filaments
d. frozen sections are a rapid diagnostic technique which can be used intraoperatively
e. in situ hybridisation techniques cannot be used to examine RNA in tissues
3. The following cases should be referred to the coroner under English law:
a. a 90-year-old man falls down the stairs. He makes a good recovery, but a month later dies of subdural haemorrhage
b. a 45-year-old man has a cardiac arrest during a coronary bypass operation and resuscitation is unsuccessful
c. a 90-year-old woman is found dead in bed at her home address. Her doctor is unsure why she died
d. a 22-year-old man is found dead in a hotel room. A note next to the body says he has taken tablets with the intention of killing himself
e. a 50-year-old worker in a nuclear power station dies of leukaemia
Extended matching items questions (EMIs)
EMI 1
Theme: Laboratory procedures
A. Congo red stain
B. cytology
C. electron microscopy
D. karyotyping
E. immunohistochemistry
F. PAS stain
G. Perls stain
H. polymerase chain reaction
I. reticulin stain
Which of the above procedures is a pathologist most likely to use in the following scenarios?
1. A specimen of pleural fluid from a 75-year-old woman with a pleural effusion is sent to the laboratory. The request form states: ‘Lung mass, ?malignant effusion.’
2. A pathologist examining a liver biopsy wants to delineate the architecture of the tissue to see if cirrhosis is present.
3. A pathologist wants to examine the internal structure of the mitochondria.
4. A rectal biopsy is received with a request form stating: ‘Please test for amyloid.’
5. A pathologist examines a tumour and suspects it may be of smooth muscle type. She would like to determine whether it contains proteins typical of smooth muscle cells such as actin and desmin.
6. An infant with multiple congenital abnormalities dies a few hours after birth. The cause of death is unknown and an autopsy is performed. The pathologist suspects trisomy 13 (Patau’s syndrome).
Case history question
Case history 1
1. List the symptoms and signs in this case.
2. Why might the patient have these problems?
3. What factors in the history are likely to predispose to the development of this disease?
Objective structured clinical examination question (OSCE)
OSCE 1
You are the house officer caring for a 65-year-old man who worked as a roofer between the ages of 20 and 32. During this time, he was often exposed to asbestos. He was diagnosed as having malignant mesothelioma of the pleura 9months ago and, despite treatment, died yesterday. His wife has just learnt that the case has been referred to the coroner and that an autopsy has been requested. She does not want an autopsy performed, and has asked to speak to you.
Short note questions
Write short notes on the following:
1. When could electron microscopic examination of tissues be of use diagnostically?
2. Describe the principles of the PCR reaction, and how it is used in diagnostic practice.
Viva question
1. What is the role of the autopsy in modern medicine?
Self-assessment: answers
One best answer
2. a. The purpose of DNA microarrays is to analyse thousands of genes simultaneously. PCR amplifies only a single segment of DNA.
3. a. The chemical pathology laboratory measures the concentration of substances in blood, urine and other body fluids.
True-false answers
1.
a. False. Substances that stain with haematoxylin are basophilic. A substance that stains with eosin is eosinophilic (or acidophilic).
b. True. A heat-stable DNA polymerase is a key component of the PCR reaction.
c. False. Tuberculosis is caused by Mycobacterium tuberculosis, which is an acid-fast bacillus which stains positively with the ZN stain. PAS stain does not demonstrate this particular organism.
d. True. There are many variations on the theme of the enzyme immunoassay. Antibodies can be used to detect antigens and antigens can be used to detect antibodies, depending on how the test is configured. One application is serology, i.e. the detection of antibodies in the blood.
e. True. High blood pressure (hypertension) is a clinical sign. Most patients will not know whether or not their blood pressure is normal unless it is measured, because high blood pressure is typically asymptomatic (without symptoms).
2. a. True. Immunohistochemical techniques exploit specific antigen-antibody binding to identify antigens in tissue sections.
b. False. Western blot analysis is used for identification of peptides/proteins.
c. True. Many cancers produce excessive quantities of certain cell products, which can be identified using histochemical or immunohistochemical techniques. For example, a malignant melanoma, a tumour of the pigment-containing cells of the epidermis (melanocytes) may produce excessive melanin which can be seen in diagnostic sections using a special silver stain (Masson–Fontana) or by immunostaining for S-100, a calcium-binding protein found in melanocytes. Similarly, squamous cancers produce cytokeratins, which are proteins found in most epithelial cells. Thus, cytokeratins are good markers of epithelial differentiation in tumours (see Ch. 12).
d. True. The rapid frozen section is used by surgeons who require urgent confirmation of a diagnosis during surgery. They may alter their surgical procedure on this basis, e.g. knowing whether a tumour is benign or malignant may drastically alter the type of operation performed. Surgeons may also ask the pathologists to perform frozen sections on tissue resection margins during cancer operations, to ensure complete removal of the tumour.
e. False. In situ hybridisation is a very useful technique which enables visualisation of specific DNA or RNA sequences in tissue sections. For example, it can be used to identify viral or bacterial RNA/DNA, such as the Epstein–Barr virus in malignant lymphoid tumours and human papilloma virus sequences in cervical cancer and pre-cancer.
3. a. True. The fall is an accident that represents a possible cause of the intracranial bleeding.
b. True. Death during an operation is a coroner’s case.
c. True. If the cause of death is unknown, the doctor cannot complete a death certificate and the case needs to be referred to the coroner.
d. True. This appears to be suicide.
e. True. This could be an industrial disease.
EMI answers
EMI 1
Theme: Laboratory procedures
1. B. Typically, the specimen will be centrifuged to concentrate the cells in the fluid. Then the cells will be mounted on a glass slide, stained, and examined under the microscope to determine whether any of the cells show features of malignancy.
2. I. A reticulin stain is ideal for this purpose. A trichrome stain might also be of use in this case by demonstrating any fibrosis.
3. C. The electron microscope is required to examine the ultrastructure of cells.
4. A. Congo red is a good stain for amyloid. When the section is examined through crossed polarising filters, amyloid stained with Congo red exhibits apple-green birefringence. This finding increases the specificity of the reaction.
5. E. Immunohistochemistry is often used diagnostically in this way.
Case history answers
Case history 1
1. The patient’s symptoms are chest pain, breathlessness, sweating and nausea on exertion. The signs of his illness elicited by his general practitioner are cold hands, abnormal pulse and heart sounds.
2. This is a very common clinical scenario in the Western world. The most likely pathogenesis is narrowing of the coronary arteries by atherosclerosis (furring of the arteries caused by a lipid-rich deposit in the vessel wall, see Ch. 6). This pathological process restricts the blood supply to the heart, thus compromising its function, particularly when the heart is stressed by the increased demands of exercise. The pain occurs when the oxygen demands of the heart are not matched by the supply of blood.
3. As in many diseases, both genetic and acquired processes have a role in the development of atherosclerosis. Inherited abnormalities of lipid metabolism can lead to early atherosclerosis, and the increased blood cholesterol is likely to be significant in this case. Many of the risk factors for atherosclerosis are acquired and can be controlled by alterations in lifestyle. Cigarette smoking is strongly associated with atherosclerosis, as in this case. Other factors predisposing to this condition are the patient’s age (the incidence of coronary atherosclerosis increases with advancing age) and his sex (the incidence in men is higher than in women of the same age).
OSCE answers
OSCE 1
Comment: You should start by expressing sympathy and then explore the reasons for the patient’s wife’s request to see you. You should find out how much she already understands. You may need to explain that the mesothelioma was due to asbestos exposure during his employment and is therefore an industrial disease. There is often a long time delay between the exposure and the onset of the tumour, as in this case. The relatives cannot refuse the autopsy, since the case comes under the jurisdiction of the coroner and is thus a legal requirement.
You should explain that:
• the procedure will be performed by trained professionals who will be respectful
• the autopsy is designed to investigate fully the circumstances of the death
• it may help to answer any outstanding questions about the progress of the disease and its treatment.
Be prepared to answer questions about retention and disposal of tissue samples; if you don’t know the details, agree to find out. She may wish to talk with a bereavement coordinator, chaplain or other member of the team, and you should be willing to facilitate this. Empathy and sensitivity will obviously be required throughout.
Short note answers
1. In microbiology, electron microscopy has applications in identifying viruses in specimens. It may also be of use in identifying some unusual bacteria and protozoa. In histopathology, it is used routinely in renal biopsies taken for investigation of glomerulonephritis. It can also be used to classify some tumours by identifying ultrastructural components in the cells (for example neurosecretory granules in neuroendocrine neoplasms), but immunohistochemistry has superseded the use of the electron microscope in this field for all but a few specific tumours.
2. Comment: A good answer would start by defining the PCR reaction as a technique which amplifies DNA. RNA can be amplified after conversion to complementary DNA by reverse transcriptase. Describe how repeated DNA strand separation, primer annealing and chain extension by heat-stable DNA polymerase are produced by cycles of heating and cooling. As a result, small amounts of DNA or RNA in the sample which otherwise might be too small to detect can be analysed. Examples of its use are to identify bacteria, viruses and other pathogens; abnormal genes in cancers; and inherited disease genes, such as those involved in muscular dystrophy or cystic fibrosis.
Viva answer
1. Even if a cause of death has been given on a death certificate, an autopsy can:
• detect conditions that were unsuspected during life (still a common occurrence despite the increasing use of modern diagnostic techniques), and thus act as a form of audit
• correlate clinical findings with pathological processes
• identify organs involved in ‘new’ diseases (e.g. HIV)
• be a valuable teaching resource
• provide data for research.
There are circumstances in which an autopsy may be required by law, for example to ascertain the cause of death where it is unknown, or in the investigation of unnatural deaths.